Objectives:
To describe clinical characteristics of fracture patients, including a closer look to hip fracture patients, and determine how epidemiological variables may have influenced on a higher vulnerability to SARS-CoV-2 infection, as the basis for the considerations needed to reintroduce elective surgery during the pandemic.
Design:
Longitudinal prospective cohort study.
Setting:
Level I Trauma Center in the East of Spain.
Patients/Participants:
One hundred forty-four consecutive fracture patients 18 years or older admitted for surgery.
Intervention:
Patients were tested for SARS-CoV-2 with either molecular and/or serological techniques and screened for presentation of COVID-19.
Main Outcome Measurements:
Patients were interviewed and charts reviewed for demographic, epidemiological, clinical, and surgical characteristics.
Results:
We interviewed all patients and tested 137 (95.7%) of them. Three positive patients for SARS-CoV-2 were identified (2.1%). One was asymptomatic and the other 2 required admission due to COVID-19-related symptoms. Mortality for the whole cohort was 13 patients (9%). Significant association was found between infection by SARS-CoV-2 and epidemiological variables including: intimate exposure to respiratory symptomatic patients (P = 0.025) and intimate exposure to SARS-CoV-2-positive patients (P = 0.013). No association was found when crowding above 50 people was tested individually (P = 0.187). When comparing the 2020 and 2019 hip fracture cohorts we found them to be similar, including 30-day mortality. A significant increase in surgical delay from 1.5 to 1.8 days was observed on the 2020 patients (P = 0.034).
Conclusions:
Patients may be treated safely at hospitals if strict recommendations are followed. Both cohorts of hip fracture patients had similar 30-day mortality.
Level of Evidence:
Prognostic Level II. See Instructions for Authors for a complete description of levels of evidence.
Key Words: SARS-CoV-2, COVID-19, hip fractures, fracture outcome, elective surgical procedure, surgery restoration
INTRODUCTION
Since December 2019, a global pandemic has been spreading vigorously. The novel coronavirus known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first notified in the city of Wuhan, Hubei (China). Currently, bats seem to be the origin of SARS-CoV-2,1 although Malayan Pangolins may have been acting as a reservoir.2 SARS-CoV-2 has been catalogued as a global pandemic and is known to have caused 349,095 deaths globally as of May 27, 2020.3
There is already consolidated data on the characteristics of SARS-CoV-2 infection.4–6 Several studies have already emphasized the importance of avoiding transmission7 and its incubation period and basic reproductive number (R0).8,9 In this regard, many countries have opted to enforce a lockdown for their respective populations.
Because of the risk of droplet-based transmission, it is necessary to understand the crowded conditions that can be derived from hospital admissions and the intimate contact with potential asymptomatic health workers to which these patients are exposed.10,11 Understanding the risk of virus transmission to patients within the health care setting may be critical in countries with limited ability to acquire personal protective equipment and limited testing capacity, where only a sample of potential SARS-CoV-2 carriers are tested.
Recent studies have shown that SARS-CoV-2-infected fracture patients who undergo surgery during the incubation period may experience a poor clinical outcome. However, these are small and limited to a predominantly Chinese population12 or have a short follow-up period.13 Information that guides treatment and defines the risks for fracture patients during the pandemic is therefore needed, especially for those whose surgical outcome is time-dependent such as hip fracture patients.14 The challenge is further amplified by the fact that many aspects of musculoskeletal care are not considered essential during a pandemic crisis when resources are limited. The cancellation of elective surgical procedures and a limitation of outpatient visits will create a challenging backlog difficult to manage.15
Given the effects, there is an urgent need to obtain reliable data that may support decision-making regarding restoration of musculoskeletal practice. In this context, we aim to determine how epidemiological variables may have influenced on a higher vulnerability to SARS-CoV-2 infection, as the basis for the considerations needed to reintroduce elective surgery. We consider an effective way to achieve this will be by describing and studying epidemiological circumstances, SARS-CoV-2 infection, complications and mortality on a prospective cohort of surgical fracture patients during the pandemic, including a closer look at hip fracture patients.
MATERIALS AND METHODS
Study Design and Participants
A single-center prospective cohort study was performed for all consecutive patients admitted for surgery of their fractures. Patients were admitted to a Level I Trauma Center within the Spanish National Health System during the period February 1, 2020 to April 15, 2020. This cohort included all hip fracture patients seen, even though some did not undergo surgery as comorbidity or previous conditions discouraged it.
Exclusion criteria included under-aged patients (<18 years old) and those who rejected participation. Patients were given a minimum follow-up of 30 days and interviewed at the end of the follow-up. Informed consent was obtained from all participants.
Hip fracture patients were filtered to meet criteria above 65 years old and compared with a cohort of patients with hip fracture of similar demographic treated during the same period before the pandemic in 2019.
Data Collection and Variables
All study subjects were interviewed at the end of the follow-up using a predesigned survey through outpatient visits and home visits. A blood test to include serological analysis was extracted at this point to all surviving patients. Information about deceased patients together with patients unable to respond to the interview was obtained through their primary caregivers.
At the time of this study there was an absence of a clearly defined protocol for testing with reverse transcription polymerase chain reaction (RT-PCR) and a lack of constant supply. RT-PCR was therefore performed upon patient-based individualized criteria and medical judgment from the surgeon or a third party.
Every patient was surveyed for the presence of COVID-19 symptoms. The survey accounted for signs and symptoms to include fever, cough, dyspnea, sore throat, anosmia/ageusia, headache, diarrhea, and other not specified. Following criteria established by the “Estudio Nacional de sero-Epidemiología de la infección por SARS-CoV-2 en España (ENE-Covid19)” study in Spain,16 we considered untested deceased patients with 3 or more specified symptoms or those with anosmia/ageusia plus another specified symptom to be suspect of SARS-CoV-2 infection if no other source could be identified.
Moreover, the survey also accounted for epidemiological variables that could have potentially influenced infection by SARS-CoV-2 during the study period outside the health care setting. We investigated intimate contact (defined as being less than 2 meters away without mask for more than 5 minutes, couples or cohabitants) with respiratory symptomatic people (cough and/or dyspnea and/or sore throat), intimate contact with SARS-CoV-2 confirmed cases, any travel outside the province, or attendance to events or places where more than 50 people were gathered together (to include living in nursing homes). The fact of being a health worker was also recorded. We individually tested exposure to each epidemiological variable and the combination of them.
Primary data included sociodemographic characteristics, surgical variables (to include surgical delay, length of stay and fractured body part), need for admission and intensive care unit, available RT-PCR results, and serological test results. Laboratory test values and radiological imaging were gathered from medical records. Comorbidity was identified through the American Society of Anesthesiologists score. Mortality was also recorded.
Regarding the hip fracture comparative study for those above 65 years old, 2020 patients were equally surveyed and followed as mentioned whereas the 2019 cohort was reviewed using medical records and no intervention was conducted. Variables recorded included gender, age, surgical delay, length of stay, American Society of Anesthesiologist, and mortality.
Laboratory testing for RT-PCR was done by detecting genes E and RdRp. Serological testing was done for blood extracted through venipuncture with a combination of immunocromatography and Enzyme-Linked ImmunoSorbent Assay (ELISA). Initially, sieving was done by 2 types of immunocromatographies: one detected total antibodies (immunoglobulin M [IgM] and immunoglobulin G [IgG]) and the other, IgM and IgG separately. When a positive test for immunocromatography was detected, it was further confirmed with ELISA.
Statistical Analysis
Microsoft Office Excel (2011; Microsoft, Redmond, WA) and Statistical Package for the Social Sciences (SPSS) software (version 25.0; IBM, Armonk, NY) were used for statistical analysis of primary data.
RESULTS
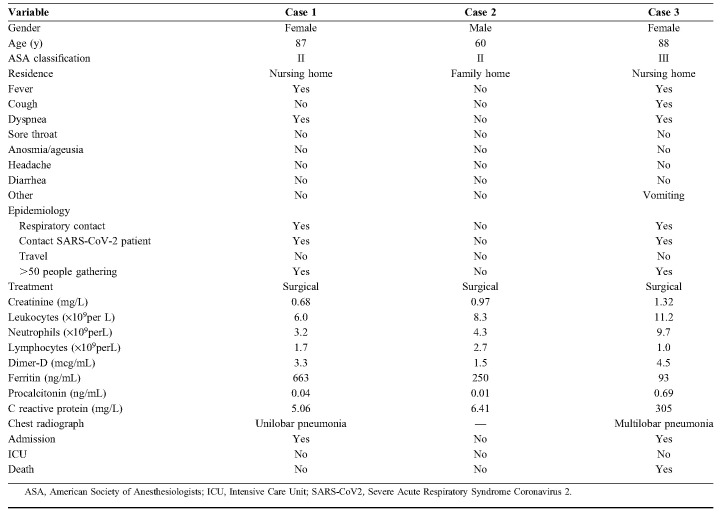
Following our selection criteria, 144 patients were included in our prospective study. Only 5 patients rejected enrollment. Hip fracture patients above 65 years old accounted for 68 of them. Table 1 shows a summary of the main variables collected. The mean age was 70.6 years ranging from 18 to 100 years. Most patients underwent surgery and the most common fractured anatomical area was the hip. The average length of stay was 4.8 days and patients waited an average of 2.9 days until surgery. The mean follow-up for our cohort was 69.7 days.
TABLE 1.
Cohort Characteristics
A total of 137 patients were tested and 7 patients died with no testing. No untested deceased patients matched our symptomatic criteria and were known to die for other reasons. Twenty-one RT-PCR and 134 serological tests were performed. Some patients underwent both testing procedures but had no discrepancy between results.
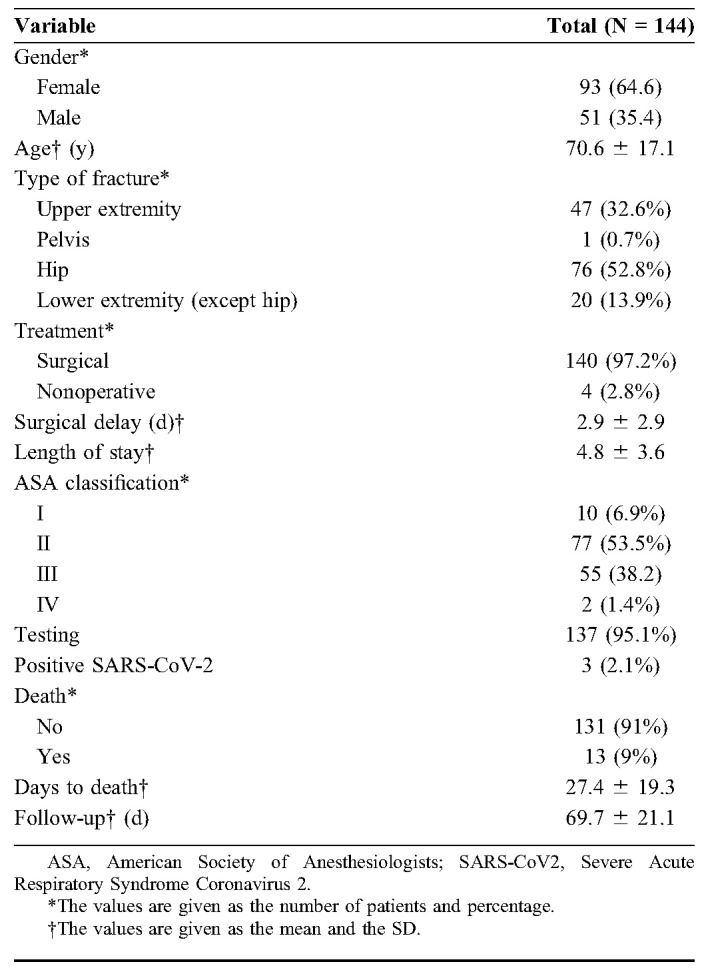
We obtained a sample of 3 positive patients for SARS-CoV-2 (2 through RT-PCR and one through serology). All of them underwent surgical treatment of their fractures (2 hip fractures and one distal tibial fracture). The patient identified through serology remained asymptomatic for the whole follow-up and lived in a family home. The 2 other patients were above 65 years old and lived in nursing homes. Both required admission, were treated accordingly, and none of them received intensive care unit support. One patient died at the hospital and the other recovered after 48 hours of supportive treatment and was discharged to the nursing home. Details of clinical, surgical variables, and outcome of these 3 patients can be seen on Table 2.
TABLE 2.
Demographic and Clinical Presentation of SARS-CoV-2-Positive Patients
Mortality for our whole cohort and follow-up period was 13 patients (9%). Of these, 12 had a hip fracture and were above 65 years old. They represent 17.6% of this subgroup and account for the 7 untested patients.
Within tested patients, mortality reached 6 patients (4.4%) for the whole cohort, and 5 patients (8.2%) for hip fractures above 65 years old.
The one patient left over from the previous data died secondary to leiomyosarcoma.
The mean number of epidemiological exposures as identified by screening was 0.49. Positive SARS-CoV-2 patients had greater (2.0) epidemiological exposure than negative patients (0.46), a fact that tends toward significance (P = 0.062).
Significant association was found between intimate exposure to respiratory symptomatic patients and infection by SARS-CoV-2 (P = 0.025). A similar result could be observed between intimate exposure to confirmed SARS-CoV-2 patients and infection (P = 0.013). No association could be determined between individual gatherings of more than 50 people with infection (P = 0.187), and for travel (P = 0.10) when tested individually. We found positive association of SARS-CoV-2 infection from the combination of several epidemiological variables. Figure 1 presents findings on this respect.
FIGURE 1.
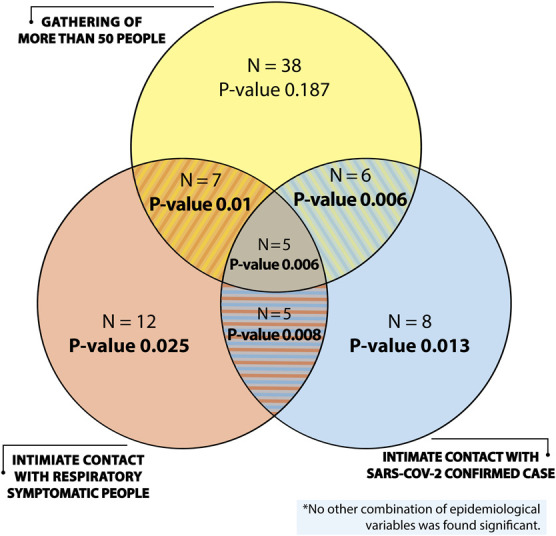
Relationship between epidemiological variables and infection by SARS-CoV-2.
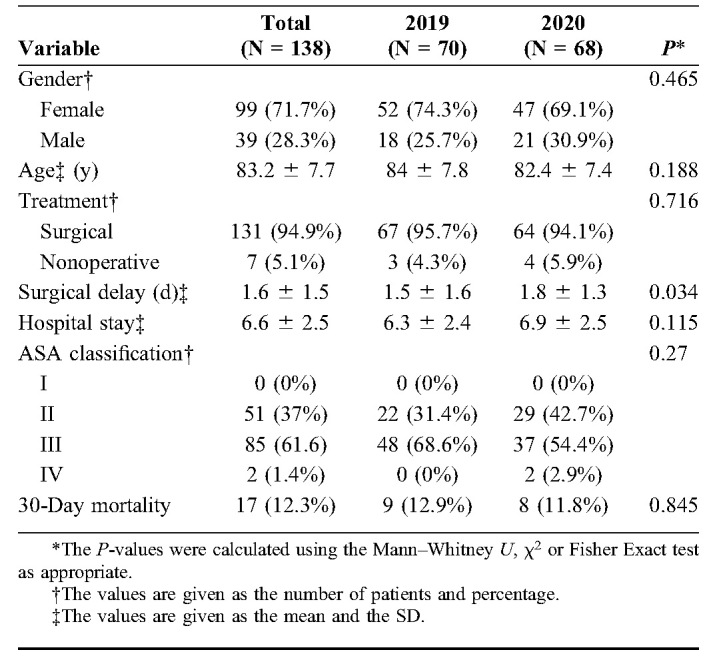
The 2020 hip fracture cohort was then compared with that of 2019. We included the 68 patients for the 2020 cohort and 70 patients for that of 2019. Table 3 shows the variables gathered. The mean ages for the 2020 and the 2019 cohort were 82 and 84 years old respectively. A significant increase in surgical delay from 1.5 days to 1.8 days for the 2020 cohort (P = 0.034) was identified. Both groups had similar comorbidities (P = 0.27) and mortality was found to be similar in both groups after a 30-day follow-up (P = 0.845).
TABLE 3.
Hip Fracture Patients' Characteristics
DISCUSSION
This paper presents prevalence, clinical outcomes, and mortality of 144 fracture patients treated during the pandemic. Our cohort had a 2.1% SARS-CoV-2 infection rate, similar to that from the general population on our community (2.3%).16 Because of clinical particularities of hip fracture patients that may make them more vulnerable, we made a deeper approach in the study of this subgroup. The tracing data on exposure from the screening process helps outline the risks for SARS-CoV-2 infection in surgical patients and may offer relevant considerations for the reintroduction of elective surgery.
Our study had some limitations. First, because of dynamic circumstances during the pandemic, the survey had to be modified during the study period allowing a homogeneous interview to patients only by the end of the follow-up. At this point, answers to surveyed questions may lead to memory bias mainly among older patients. In this sense, accuracy of interviews with primary caregivers may have been less reliable too. It was also difficult for some patients to identify situations that were specifically above 50 people, so we had to turn to examples related to patient lifestyle. Second, due to limited testing capacity during the first pandemic period, RT-PCR from throat swab and serological testing was available to a limited number of patients. Therefore, some patients were lost during the follow-up with no SARS-CoV-2 determination. We tried to overcome this fact using symptom criteria on our statistical analysis. Third, we found differences between the sensitivity (sen) and specificity (spe) on the tests since different suppliers have been used because of lack of a constant supply: RT-PCR (sen > 95% and spe 100%); inmunocromatography (sen 85%–95% and spe 95%–99%); ELISA (sen 85%–99% and spe 95%–100%). Finally, we did not account for other epidemiological variables that may affect mortality rates such as severity of flu season when comparing both hip fracture groups.
A similar 30-day mortality was observed for both hip fractures cohorts treated both before and during the pandemic, even though the 7 untested patients belonged to this group. A difference within surgical delay was observed. However, this does not seem to be clinically significant since it remained under 48 hours.14 This difference can be explained by circumstances inherent to the pandemic period. First, hospitals underwent redistribution of surgical personnel, converting operating rooms into ICU beds to accommodate SARS-CoV-2 patients. Surgical teams were also assigned to backup periods reducing the number of available surgeons. Furthermore, a delay of SARS-CoV-2 test results may have postponed the surgery. It is well known the importance of an early surgery on hip fractures because it is directly related to better outcomes and mortality rates.14 These patients should therefore be taken into consideration when planning resources during a pandemic.
In our prospective cohort, we were able to prove a direct relationship among several epidemiological events that must be kept in consideration for the future. Perhaps, most importantly, we found no association between infection by SARS-CoV-2 and individual gathering of more than 50 people at once. However, we did find association between symptomatic respiratory patients or SARS-CoV-2 confirmed cases with SARS-CoV-2 infection when combined with crowding. Positivity is therefore associated with patient-linked characteristics and we must therefore reinforce the fact of avoiding the concurrence of the combination of any of these 3 factors at the hospital to reintroduce elective surgery safely.
On the one hand, symptomatic respiratory patients should be isolated upon admission because these patients may be a possible source of infection for other healthy patients who may be admitted for other purposes such as surgery. On the other hand, positive SARS-CoV-2 patients must be quickly identified and isolated too. Regarding this, testing should be conducted on all patients undergoing hospital admission, including all surgical patients. Hospitals should work on creating well-defined care circuits upon admission, isolating patients into COVID and non-COVID areas. A way to achieve this may be by creating transition areas where all undiagnosed patients could be accommodated until test results are available and final diagnosis is reached.
Even though these conditions are satisfied, there is always a chance that transmission may occur between patients. In this scenario, health workers may be acting as main vectors on hospital wards11 and the hospital must therefore guarantee the availability of personal protective equipment and testing to them.
Because this is a dynamic situation and testing does not mean immunity against SARS-CoV-2, all patients should be educated on social distancing within the hospital, for example promoting individual accommodation and strict hygiene measures should also be enforced. Furthermore, an effort should also be made to avoid overcrowding by facilitating a constant flow of discharge.
With focus on orthopaedic surgery, several actions can be taken. First, patients should be selected carefully to have a low comorbidity and avoid long stays and complications. Accordingly, surgical techniques that encourage a faster recovery such as fast-track protocols should be implemented.17 With respect to follow-up of surgical orthopaedic patients and with regard to outpatient clinics, attendance to health care centers should be reduced to avoid overcrowding. For that purpose, the use of telemedicine and telerehabilitation18,19 should be considered while SARS-CoV-2 is still around.
In summary, our results support the evidence that fracture patients can be treated safely in a hospital during the ongoing pandemic if strict recommendations are followed. Also, mortality for especially vulnerable patients such as those with hip fractures has remained similar to previous periods, which reinforces this idea of safety. Grouping of SARS-CoV-2-positive and respiratory symptomatic patients into COVID and non-COVID areas may pose a unique opportunity for the reintroduction of elective surgery, although this effect should be studied further.
ACKNOWLEDGMENTS
The authors thank Ainhoa Sánchez Cortés, María Cuenca Torres and Paul Caulfield for assistance with data collection, statistical analysis, and proofreading.
Footnotes
The authors report no conflict of interest.
REFERENCES
- 1.Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang T, Wu Q, Zhang Z. Probable pangolin origin of SARS-CoV-2 associated with the COVID-19 outbreak. Curr Biol. 2020;30:1346–1351.e2. Erratum in: Curr Biol. 2020;30(8):1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report-128. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200527-covid-19-sitrep-128.pdf?sfvrsn=11720c0a_2. Accessed May 28, 2020. [Google Scholar]
- 4.Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Trav Med Infect Dis. 2020;34:101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ong SWX, Tan YK, Chia PY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;323:1610–1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395:689–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rivett L, Sridhar S, Sparkes D, et al. Screening of healthcare workers for SARS-CoV-2 highlights the role of asymptomatic carriage in COVID-19 transmission. Elife. 2020;9:e58728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mi B, Chen L, Xiong Y, et al. Characteristics and early prognosis of COVID-19 infection in fracture patients. J Bone Joint Surg Am. 2020;102:750–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muñoz Vives JM, Jornet-Gibert M, Cámara-Cabrera J, et al. Mortality rates of patients with proximal femoral fracture in a worldwide pandemic: preliminary results of the Spanish HIP-COVID observational study. J Bone Joint Surg Am. 2020;102:e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moja L, Piatti A, Pecoraro V, et al. Timing matters in hip fracture surgery: patients operated within 48 hours have better outcomes: a meta-analysis and meta-regression of over 190,000 patients. PLoS One. 2012;7:e46175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jain A, Jain P, Aggarwal S. SARS-CoV-2 impact on elective orthopaedic surgery: implications for post-pandemic recovery. J Bone Joint Surg Am. 2020;102:e68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Instituto de Salud Carlos III (Spain). Estudio Nacional de sero-Epidemiología de la Infeccion por SARS-CoV-2 en España. Informe preliminar; Available at: https://www.isciii.es/. May 13, 2020. Spanish. https://www.mscbs.gob.es/ciudadanos/ene-covid/docs/ESTUDIO_ENE-COVID19_PRIMERA_RONDA_INFORME_PRELIMINAR.pdf. Accessed May 26, 2020. [Google Scholar]
- 17.Kehlet H, Thienpont E. Fast-track knee arthroplasty—status and future challenges. Knee. 2013;20(suppl 1):S29–S33. [DOI] [PubMed] [Google Scholar]
- 18.Gilat R, Haunschild ED, Tauro T, et al. Recommendation to optimize safety of elective surgical care while limiting the spread of COVID-19: primum non nocere. Arthrosc Sports Med Rehabil. 2020;27:e177–e183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang X, Hunter DJ, Vesentini G, et al. Technology-assisted rehabilitation following total knee or hip replacement for people with osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019;20:506. [DOI] [PMC free article] [PubMed] [Google Scholar]