Supplemental Digital Content is Available in the Text.
Key Words: HIV, COVID-19, SARS-CoV-2, coinfection, antiretroviral treatment, China
Background:
Given the magnitude of the global COVID-19 pandemic, persons living with HIV (PLWH) may become coinfected with SARS-CoV-2.
Setting:
We conducted a survey in Wuhan, China, to characterize the status of coinfected PLWH, their time to clinical improvement, and clinical prognoses.
Methods:
Using a Wuhan shipping service for antiretroviral medications, the Wuhan LGBT Center screened 2900 PLWH shipping addresses and cross-referenced 36 of them to quarantine sites or hospitals, suggesting possible COVID-19 cases. Through telephone calls and WeChat (social media) messaging, we conducted a survey after obtaining online informed consent.
Results:
We had 12 HIV-infected respondents (10 men and 2 women) who also reported COVID-19. The median age was 36 years (interquartile range: 33.0–56.3), mean age 42.4 years, and range 25–66 years of age. Nine of 10 persons on antiretroviral therapy (ART) presented with only mild COVID-19 symptoms. The 10th person on ART was a 56-year-old man who died at home early in the outbreak when health care services were overwhelmed. Two additional cases who had been in intensive care with acute COVID-19 were both men, aged 25 and 37 years; both were ART-naive until this hospitalization. Excluding the deceased man, 6 of 11 coinfected persons reported feeling depressed even after clinical improvements.
Conclusion:
Twelve coinfected persons were identified in Wuhan; 9 of 10 were on long-term ART and had favorable outcomes. Two men identified as having started ART only recently were found to have severe symptoms. Our case series suggests the value of ART for potential mitigation of COVID-19 coinfection.
INTRODUCTION
A group of immunosuppressed persons who might be at higher risk for novel coronavirus (SARS-CoV-2) disease (COVID-19) is persons living with HIV (PLWH) infection. The clinical prognosis of coinfection is unknown but could be alarming given that other chronic infections have proven to be associated with adverse COVID-19 outcomes.1,2 By contrast, PLWH who are taking antiretroviral therapy (ART) may benefit from their ART if the drugs have partially helped the person with immune reconstitution or even have downmodulated SARS-CoV-2 replication. PLWH with excellent HIV control might have milder symptoms or shorter duration of COVID-19 than coinfected persons not taking ART. A variety of COVID-19 clinical presentations have been reported, but the course in PLWH is not yet clear.3–5
Wuhan city, Hubei province, China, was taken by surprise by the COVID-19 pandemic. Free movement of the public was limited during the eventual city lockdown, disrupting the continuity of ART for PLWH in the social distancing period,6 as well as complicating health care information collection and reporting. Creative approaches to effectively distribute ART were developed by community advocates. HIV/CoV-coinfected persons are under tremendous psychological pressures,7 but we nonetheless sought them to assess their clinical courses.
METHODS
Setting and Design
We conducted a survey in Wuhan, the early epicenter of the COVID-19 pandemic, to identify coinfection of HIV and SARS-CoV-2. We used shipping addresses for ART drugs that colocated with quarantine sites or hospital addresses to identify PLWH coinfected with SARS-CoV-2, through the efforts of a collaborating nongovernmental organization, the Wuhan LGBT Center. Ten cases were identified by address linkage and 2 cases came to our attention through social media.
Recruitment
The executive director of the Wuhan LGBT Center (H.H.) initiated a program to improve antiretroviral (ARV) drug supplies by shipping ART during the city-wide lockdown to about 2600 PLWH from January 23, 2020, to March 31, 2020, on behalf of designated HIV/AIDS specialized hospitals.6 By the end of October 2019, there were 5953 PLWH in Wuhan by official statistics such that over half of the known PLWH were engaged by the Wuhan LGBT Center in this endeavor. At the beginning, the team thought that the drug shipments would be needed briefly during the city lockdown, and records were not kept carefully until the first 700 persons were assisted through February 16, 2020. At that time, a careful shipping record system was instituted in the face of a continued urban lockdown for the subsequent 1900 persons receiving ARVs. To identify persons potentially eligible for the survey of coinfected persons, the Wuhan LGBT Center identified 36 persons whose shipping addresses were designated quarantine sites or hospitals. Through telephone contact, 10 persons responded, all of whom were coinfected.
An additional 2 PLWH were identified with COVID-19 disease; both had severe “white lung” requiring intensive care unit (ICU) admission to the Wuhan Jin YinTan Hospital and had not yet been discharged at the time of our survey. Both were recently diagnosed with HIV and had never received ART before their hospital admission. One ICU case sought help for admission because of serious pneumonia at a time of high hospital demand, posting a cry-for-help on social media. One of us (H.H.) saw the post and arranged his admission with the help of Hubei Provincial Centers for Disease Control and Prevention. The second ICU case was the roommate of other case. One individual died before we could interview him; we obtained his history through his well-informed partner; the couple's story was presented in a gay-oriented blog community called Baihualin.
Characteristics of the Case Series Subjects
We collected sociodemographic information, clinical features of HIV/AIDS and COVID-19 infection, comorbidities, and the major concerns of interviewees at the time of the survey, including age, sex, time of confirmed HIV diagnosis, last CD4+ cell count and viral load (VL), ART regimen before admission, presence of fever, and, when applicable, time of first fever, peak temperature, comorbidities, and time of COVID-19 confirmatory diagnosis. We asked subjects (or the partner of the deceased man) as to gastrointestinal symptoms including nausea, abdominal discomfort, diarrhea, and anorexia. We assessed clinical outcomes after definitive clinical outcome on a 7-category ordinal scale, recommended by the World Health Organization: (1) not hospitalized with resumption of normal activities; (2) not hospitalized but unable to resume normal activities; (3) hospitalized, not requiring supplemental oxygen; (4) hospitalized, requiring supplemental oxygen; (5) hospitalized, requiring nasal high-flow oxygen therapy, noninvasive mechanical ventilation, or both; (6) hospitalized, requiring invasive mechanical ventilation, extracorporeal membrane oxygenation, or both; and (7) death.8 For admitted patients, we assessed whether glucocorticoids were used, liver or pancreas damage, rashes, and any clinical trials participation date and time of discharge, whether quarantine was lifted by the time of the survey, whether they knew other coinfected people, what their major concerns were at present, what kind of help they felt that they needed most, and their mobile phone numbers if they wished to have continued contact. We used Wenjuanxing (Changsha Haoxing Information Technology Co., Ltd., China) software for the survey questionnaire.
RESULT
Sociodemographic Characteristics and Comorbidities
We enrolled 12 participants living with HIV and coinfected with COVID-19 in Wuhan. The median age of the participants was 36 years [interquartile range (IQR): 33.0–56.3], range 25–66 years, and the mean age was 42.4 years. Ten were men and 2 were women. Four participants reported comorbidities: 1 with tuberculosis, 2 with hypertension, and 1 with chronic nephritis.
HIV/AIDS Clinical Features
Before outbreak of the COVID-19, the 10 participants identified through address matching reported no immune deficiencies, whereas the 2 identified through social media who were hospitalized were advanced HIV cases who were late to receive ART. One man knew that he was HIV-infected, but he was not on ART until he received it on the COVID-19 hospitalization. His roommate was also admitted with COVID-19, and he was diagnosed with HIV infection only at the time of this COVID-19 hospitalization with a CD4+ cell count of 15/µL (Fig. 1). Both ICU patients had late-stage HIV disease meeting an AIDS surveillance case definition. Among the other 10 participants identified through addresses, 9 had been on ART and had mild COVID-19. The 10th case was a 56-year-old man who died soon after 8 days of fever before he could be admitted to the hospital.
FIGURE 1.
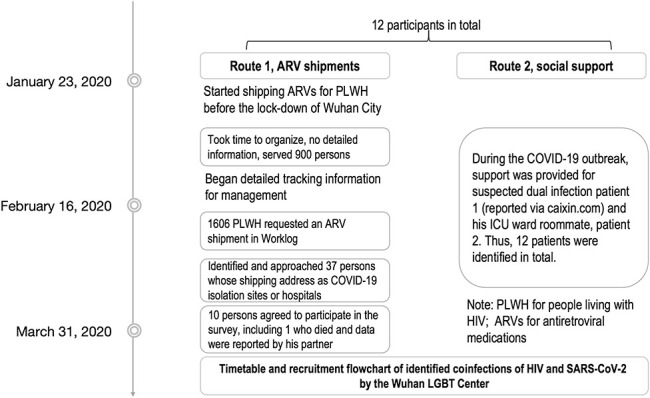
Timetable and recruitment flowchart of 12 identified coinfections of HIV and SARS-CoV-2 by the Wuhan LGBT Center.
The median time of HIV diagnosis to time of the survey was 5.8 years (IQR 4.2–7.5). The most recent CD4+ cell count was 500/μL (IQR 339–745), and the recency of the test was a median of 2 months (IQR 2–4) before the survey. ART regimens for the 10 persons identified in the address matching included 5 on tenofovir disoproxil fumarate (TDF) + efavirenz (EFV) + lamivudine (3TC), 3 on zidovudine (ZDV) + nevirapine (NVP) + 3TC, and 2 on ZDV + EFV + 3TC. The 2 ICU patients identified through social media were placed on TDF + lopinavir/ritonavir (LPV/r) + 3TC on admission. HIV VL was undetectable in 8 of 10 persons on longer-term ART, whereas the other 2 persons did not know their VL but stated that their “doctors said the VL was okay” (Table 1).
TABLE 1.
Sociodemographic Characteristics of the Participants (N = 12)
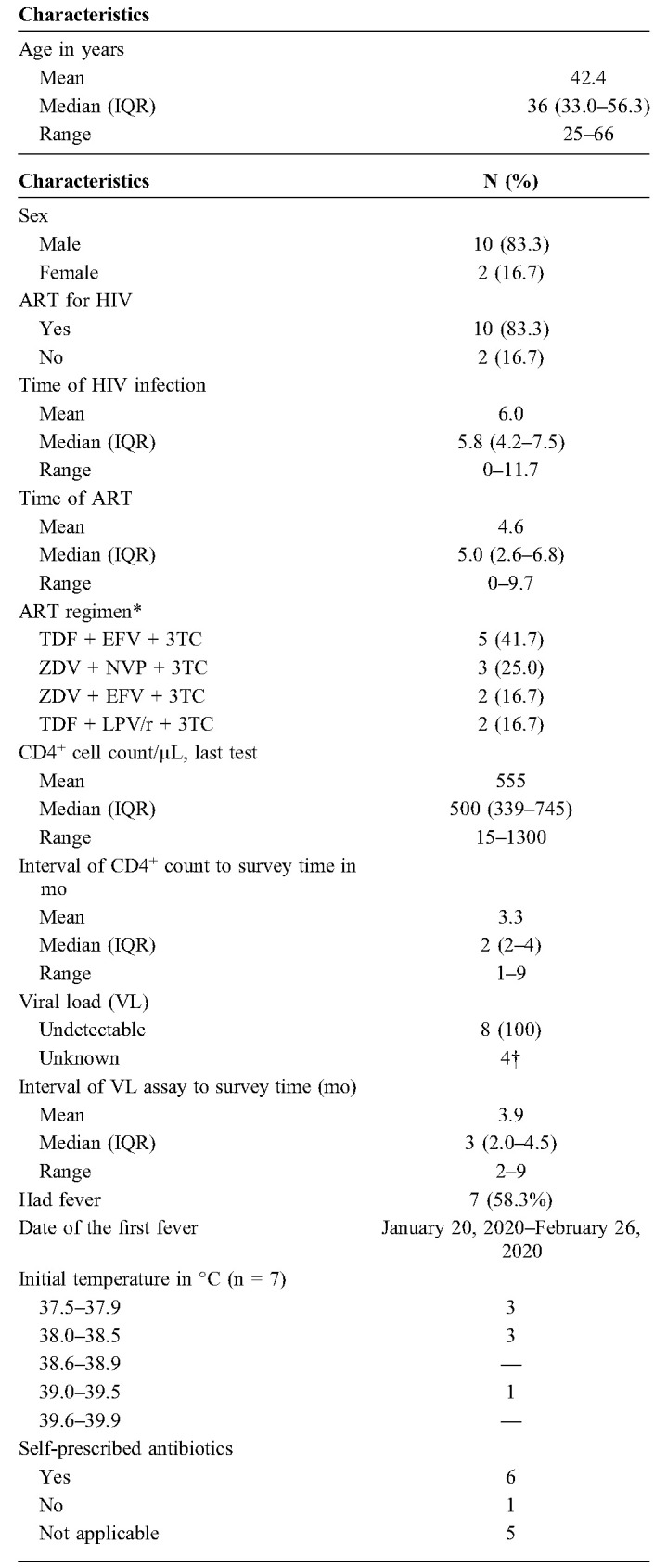
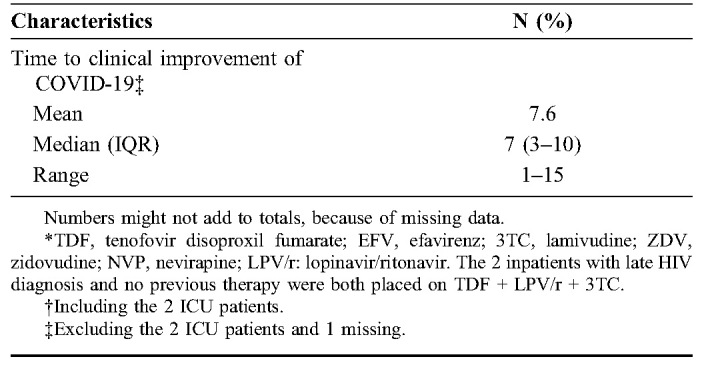
Coinfection With COVID-19
Of the 12 coinfected PLWH, 9 had mild symptoms, 1 56-year-old man died before he could be admitted to the hospital, and 2 were the serious ICU cases with late-diagnosed HIV/AIDS without previous ART. Six reported feeling discomfort of the digestive tract when coinfected with COVID-19, 5 of whom reported anorexia, 4 with nausea, 6 with abdominal discomfort, and 7 with diarrhea. Three were never hospitalized and were able to resume normal activities, 6 were hospitalized without requiring supplemental oxygen, 1 was hospitalized and required supplemental oxygen, 1 was hospitalized requiring high-flow nasal cannula for oxygen therapy, and one died before able to admit. Among hospitalized cases, only 1 received glucocorticoids. The median time to clinical improvement for 10 of 12 patients was 7 days (IQR: 3–10), and the mean time was 7.6 days with a range of (1–15), but these are minimum estimates because we exclude the one man with AIDS who was still hospitalized in the ICU at the time of the survey, and we exclude the patient who died. Two cases reported rashes and 7 had miscellaneous other symptoms. None had participated in clinical trials. The date of discharge varied from February 22, 2020, to March 21, 2020, and 5 cases had completed their time of quarantine by the time of survey. Three people reported they knew other HIV/CoV-coinfected people.
Self-reported Major Concerns
In soliciting what were the 11 survivors' major concerns, 6 reported depression, 7 were worried that their incomes would be affected substantially by COVID-19, 3 were worried about ongoing access to ART, and 5 worried about their families' health status. In open-ended questions as to their needs, 2 reported receiving psychological support and treatment for depression. One person reported lacking money for basic needs and one cited worry about a possible abrupt ART shortage due to work in another city. Three persons left their mobile phone numbers with us for further inquiries. Individual case histories are in the Supplemental Digital Content (see Supplement, http://links.lww.com/QAI/B495).
DISCUSSION
Without a comparison, control, or other counterfactual population, we cannot draw firm inferences about how COVID-19 has afflicted PLWH in Wuhan. One person died before he could be fully evaluated or hospitalized, and 2 persons were seriously ill, both of whom were diagnosed very late with HIV and had no previous ART history. Excluding the deceased patient who did not make it to the hospital, 2 of the 3 sickest patients were also our most immunosuppressed persons. Hence, we believe it plausible that good adherence to ART with consequent viral suppression and partial immune reconstitution was beneficial for the patients, 8 of 10 of whom had less serious illness (1 died and 1 needed a ventilatory support, although he recovered). The fact that all 11 HIV and SARS-CoV-2–coinfected persons who reached the hospital survived was a pleasant surprise. One may also ask whether the vigor of the cytokine storm might be downmodulated in patients with HIV because even ART-adherent patients are still immunosuppressed to some degree. At this early stage of the study, we can only posit hypotheses, relying on cohorts to determine whether our hypothesis is plausible and based on evidence confirmed from larger cohorts with many more coinfected persons.
Advanced age is a well-known predictor for bad prognosis of the COVID-19,9 especially problematic in the time in Wuhan when hospitals suffered from medical resource shortages. Although none of our participants used LPV/r as a previous ARV drug (it was given post–COVID-19 diagnosis to the 2 ICU patients), overuse of LPV/r as a putative COVID-19 therapy in the current epidemic has risked shortages for this now second-line treatment for PLWH in China.10 Both late HIV presenters were young, both had low CD4+ cell counts, severe pneumonia, and prolonged ICU stays. This underscores the benefits of early ART initiation among PLWH. Although our case series provides no insights as to whether ARVs might be used to treat or prevent SARS-CoV-2 infection, previous use for HIV management is likely to have been beneficial with 8 of 10 on ART avoiding serious disease, but 2 of 2 not on ART landing in the ICU with serious COVID-19 (P = 0.09 by the Fisher exact test). Overuse of ARVs for COVID-19 in the absence of evidence should take into consideration the need to ensure continuity of drug availability for PLWH. This issue is similar to the use of hydroxychloroquine for COVID-19 that has made it difficult for some persons to secure the drug for rheumatologic therapy or malaria.
Coinfection with COVID-19 and HIV may have resulted in even more perceived stigmatization than with HIV alone. Persons self-identifying as gay often suffered from depressive ideation even after recovery, perhaps reflecting previous sentiments.11,12 We were told that coinfected persons would rather admit to COVID-19 rather than HIV infection in Wuhan. Health care professionals must address stigmas of being gay, being HIV-infected, and, perhaps, of having yet another viral infection. Addressing the underlying drivers and facilitators of stigma is vital.6,7 Dually infected persons may represent persons of exceptional vulnerability.2
Strengths of our study include the creative assembly of a case series based on the recruiting team (led by H.H.), with renowned community outreach skills as documented by international (eg, CNN) and local (eg, Caixin.com) media. The Wuhan LGBT Center was assisting about half of the city's PLWH during the crisis. The address match was a creative way to identify likely COVID-19 infections among PLWH. Use of health informatics and electronic medical records will simplify the considerable search for coinfected persons, although they will only represent persons whose data are entered into an electronic medical record.
Study limitations include the likely underestimation of the proportion of serious cases among the all presumptive coinfected PLWH because only 28% of potential coinfections (10/36) responded to our outreach; most were in quarantine sites rather than in hospitals. People concerned with revealing their infection status, stigma, or discrimination may avoid participating in a survey. The sampling is from responses to overtures and is not a representative sample of cases. Ascertainment of cases with coinfection does not present any counterfactual comparison we know that we cannot generalize the findings. For example, a hospital worker told us that 16 patients with HIV/CoV were hospitalized, but we could identify only 2. Although the small sample of 12 persons limits generalizability, the case series can help generate hypotheses about dual HIV/CoV infection.
We posit that early detection of HIV and timely, early initiation of ART will best prevent PLWH from acquiring serious COVID-19 disease. If our deceased patient had been admitted to the hospital in a timely fashion, we speculate that he, too, might have survived. Whether persons with well-controlled HIV are paradoxically protected from the extremes of cytokine storms is unknown and worthy of additional study. Assaults on self-esteem experienced by persons in the LGBTQ communities, along with perceived, experienced, and internalized stigma, can increase the likelihood of depression, both before and after COVID-19 infection with dual HIV/CoV infection. Finally, given that an estimated 38 million persons are living with HIV worldwide, HIV/CoV coinfection is likely more common than realized3,13–18 and will have special clinical and psychosocial considerations.
ACKNOWLEDGMENTS
The authors thank the participants for their time and opinions in the postcrisis of fighting against COVID-19.
Footnotes
Y. Hu is supported in part by the National Natural Science Foundation of China (81673232) and Beijing Natural Science Foundation (7202009). S. H. Vermund is supported in part by the National Institutes of Health grant (P30MH062294). The sponsors have no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
The study was approved by the Capital Medical University Ethics Review Board (2020SY004).
Informed participants consent: Obtained.
The authors have no conflicts of interest to disclose.
Y.H. is the principal investigator and conceptualized the study; J.M. and H.H. conducted the survey; Y.H. drafted the manuscript; Y.H. and S.H.V. interpreted findings, edited, and revised the manuscript. All authors had final approval of the submitted and published versions.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jaids.com).
We are happy to share the available data and can upload the anonymized data upon request.
REFERENCES
- 1.Blanco JL, Ambrosioni J, Garcia F, et al. COVID-19 in patients with HIV: clinical case series. Lancet HIV. 2020. doi: 10.1016/S2352-3018(20)30111-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu F, Cao Y, Xu S, et al. Co-infection of SARS-CoV-2 and HIV in a patient in Wuhan city, China. J Med Virol. 2020;92:529–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhao J, Liao X, Wang H, et al. Early virus clearance and delayed antibody response in a case of COVID-19 with a history of co-infection with HIV-1 and HCV. Clin Infect Dis. 2020. doi: 10.1093/cid/ciaa408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323:1574–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang X, Fang J, Zhu Y, et al. Clinical characteristics of non-critically ill patients with novel coronavirus infection (COVID-19) in a Fangcang Hospital. Clin Microbiol Infect. 2020. doi: 10.1016/j.cmi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lily Lee BW. People living with HIV in Wuhan struggle to find medicine during coronavirus outbreak. CNN 2020;CNN health. Available at: https://edition.cnn.com/2020/03/13/health/coronavirus-china-hiv-wuhan-intl-hnk/index.html. Accessed March 13, 2020. [Google Scholar]
- 7.Logie CH, Turan JM. How do we balance tensions between COVID-19 public health responses and stigma mitigation? Learning from HIV research. AIDS Behav. 2020. doi: 10.1007/s10461-020-02856-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cao B, Wang Y, Wen D, et al. A trial of lopinavir-ritonavir in adults hospitalized with severe covid-19. N Engl J Med. 2020;382:1787–1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ashcroft J. Keep older healthcare workers off the covid-19 front line. BMJ 2020;369:m1511. [DOI] [PubMed] [Google Scholar]
- 10.Ford N, Vitoria M, Rangaraj A, et al. Systematic review of the efficacy and safety of antiretroviral drugs against SARS, MERS or COVID-19: initial assessment. J Int AIDS Soc. 2020;23:e25489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang N, Wang S, Qian HZ, et al. Negative associations between general self-efficacy and anxiety/depression among newly HIV-diagnosed men who have sex with men in Beijing, China. AIDS Care. 2019; 31:629–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tao J, Qian HZ, Kipp AM, et al. Effects of depression and anxiety on antiretroviral therapy adherence among newly diagnosed HIV-infected Chinese MSM. AIDS. 2017;31:401–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vizcarra P, Pérez-Elías MJ, Quereda C, et al. Description of COVID-19 in HIV-infected individuals: a single-centre, prospective cohort. Lancet HIV 2020. doi: 10.1016/S2352-3018(20)30164-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang M, Luo L, Bu H, et al. One case of coronavirus disease 2019 (COVID-19) in a patient co-infected by HIV with a low CD4+ T-cell count. Int J Infect Dis. 2020;96:148–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ridgway JP, Farley B, Benoit JL, et al. A case series of five people living with HIV hospitalized with COVID-19 in Chicago, Illinois. AIDS Patient Care STDS. 2020. doi: 10.1089/apc.2020.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suwanwongse K, Shabarek N. Clinical features and outcome of HIV/SARS-CoV-2 co-infected patients in the Bronx, New York City. J Med Virol. 2020. doi: 10.1002/jmv.26077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nakamoto T, Kutsuna S, Yanagawa Y, et al. A case of SARS-CoV-2 infection in an untreated HIV patient in Tokyo, Japan. J Med Virol. 2020. doi: 10.1002/jmv.26102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baluku JB, Mwebaza S, Ingabire G, et al. HIV and SARS-CoV-2 co-infection: a case report from Uganda. J Med Virol. 2020. doi: 10.1002/jmv.26044. [DOI] [PMC free article] [PubMed] [Google Scholar]


