Supplemental Digital Content is available in the text.
Keywords: coronavirus disease, pandemics, stroke
Abstract
Background:
Anecdotal reports suggest fewer patients with stroke symptoms are presenting to hospitals during the coronavirus disease 2019 (COVID-19) pandemic. We quantify trends in stroke code calls and treatments at 3 Connecticut hospitals during the local emergence of COVID-19 and examine patient characteristics and stroke process measures at a Comprehensive Stroke Center (CSC) before and during the pandemic.
Methods:
Stroke code activity was analyzed from January 1 to April 28, 2020, and corresponding dates in 2019. Piecewise linear regression and spline models identified when stroke codes in 2020 began to decline and when they fell below 2019 levels. Patient-level data were analyzed in February versus March and April 2020 at the CSC to identify differences in patient characteristics during the pandemic.
Results:
A total of 822 stroke codes were activated at 3 hospitals from January 1 to April 28, 2020. The number of stroke codes/wk decreased by 12.8/wk from February 18 to March 16 (P=0.0360) with nadir of 39.6% of expected stroke codes called from March 10 to 16 (30% decrease in total stroke codes during the pandemic weeks in 2020 versus 2019). There was no commensurate increase in within-network telestroke utilization. Compared with before the pandemic (n=167), pandemic-epoch stroke code patients at the CSC (n=211) were more likely to have histories of hypertension, dyslipidemia, coronary artery disease, and substance abuse; no or public health insurance; lower median household income; and to live in the CSC city (P<0.05). There was no difference in age, sex, race/ethnicity, stroke severity, time to presentation, door-to-needle/door-to-reperfusion times, or discharge modified Rankin Scale.
Conclusions:
Hospital presentation for stroke-like symptoms decreased during the COVID-19 pandemic, without differences in stroke severity or early outcomes. Individuals living outside of the CSC city were less likely to present for stroke codes at the CSC during the pandemic. Public health initiatives to increase awareness of presenting for non-COVID-19 medical emergencies such as stroke during the pandemic are critical.
See related article, p 2613
Stroke is a medical emergency. Because stroke treatment is time-sensitive, guidelines recommend immediate medical evaluation for patients experiencing symptoms concerning for stroke. However, anecdotal evidence suggests a decrease in emergency evaluation for patients with stroke-like symptoms in the setting of the coronavirus disease 2019 (COVID-19) pandemic in the United States.1
Since the confirmation of the first case of COVID-19 (the disease caused by the virus severe acute respiratory syndrome coronavirus 2) in the United States on January 21, 2020,2 there has been a steep rise in the number of diagnosed cases and attributable deaths.3 To mitigate viral spread, social distancing was implemented to varying degrees across the country. A survey from March 17 to March 20, 2020, demonstrated that up to 72% of US adults were no longer going to public places.4 It is conceivable that one of the public places avoided was the hospital, given the concern for severe acute respiratory syndrome coronavirus 2 exposure.
There is an urgent need to inform the stroke and public health communities about volumes and processes of care during the COVID-19 pandemic. The purpose of this study was to compare the volume of stroke codes before and during COVID-19 local spread across a healthcare system. We also sought to describe demographic and clinical characteristics of patients who presented with acute stroke-like symptoms before and during the pandemic. Finally, we ascertained the association between the onset of the pandemic and acute stroke metrics and outcomes.
We hypothesized that the number and types of patients seeking care, the severity of presenting symptoms, and acute stroke door-to-intervention metrics would differ before and after the date of March 1, 2020. This cutoff date was selected because the first cases of COVID-19 in the neighboring states of New York and Rhode Island were announced on March 1, potentially affecting both public sentiment regarding seeking medical care and acute stroke care procedures in Connecticut due to an impending pandemic.5
Methods
Study Design
This is a retrospective pre- and during-event cohort analysis. This study was approved by the Yale-New Haven Hospital (YNHH) Institutional Review Board, which sanctioned a waiver of informed consent. The data that support the findings of this study are available from the corresponding author upon reasonable request by investigators.
Study Population
Aggregate Analysis Cohort
YNHH is a tertiary care, 1540 bed hospital comprised of 2 campuses in New Haven, Connecticut, including 1 of 2 Comprehensive Stroke Centers (CSC) in the state.6 YNHH provides acute stroke care to patients who present directly to this hospital, video-based guidance to 9 spoke hospitals within its telestroke network, and telephone consultations to numerous regional hospitals on an as-needed basis (Figure 1, generated using publicly available Google Maps API). YNHH’s stroke team tracks stroke codes called for patients in the emergency department (ED), the inpatient setting, and telestroke phone and video consultations. This data set was the source of observations from January 1 to April 28, 2019 and 2020, in this study. Stroke codes from the same time period in 2019 were included to capture local temporal variations which may impact hospital presentation and workflow. At YNHH, an acute neurological change occurring within 24 hours of last known well prompted stroke code activation in both periods.
Figure 1.
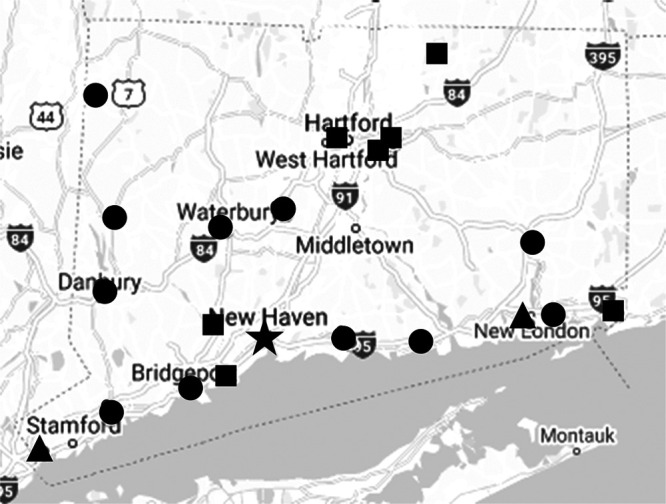
Map showing telestroke hub (Yale-New Haven Hospital, star), Greenwich and Lawrence + Memorial Hospitals (triangles), telestroke spoke hospitals (squares), and telephone consultation hospitals (circles).
To assess the impact of COVID-19 on stroke presentation and care at a site geographically closer to the COVID-19 regional epicenter, New York City, we included 2019 and 2020 aggregate data from a Yale Health affiliate, Greenwich Hospital (GH). GH is a 181-bed Primary Stroke Center that became thrombectomy capable in January 2020 and formally extended its stroke code window to 24 hours on January 6, 2020. Finally, we included 2020 stroke code data from another Yale Health affiliate, Lawrence and Memorial Hospital, a 252-bed Primary Stroke Center located in New London, Connecticut, near Connecticut’s eastern (Rhode Island) border. Lawrence and Memorial Hospital data from 2019 were not included due to a substantial change in data collection practices. All 3 hospitals currently participate in the Get With The Guidelines-Stroke Registry, a quality improvement initiative in which hospitals enter clinical data of all patients hospitalized with a stroke diagnosis.7
Patient-Level Analysis Cohort
To determine patient-level factors influencing stroke presentation and care at our CSC, we defined and analyzed 2 time-based cohorts of patients evaluated at YNHH for whom a stroke code was activated in February (prepandemic cohort) and March 1 to April 28, 2020 (pandemic cohort). We chose February as the prepandemic comparator month since it was most proximal to onset of the pandemic. We confirmed that February was representative of a prepandemic time by comparing patient characteristics between January and February, 2020, which were all similar (Table I in the Data Supplement).
Variables
The following variables were manually extracted from the electronic medical record for the patient-level analysis at YNHH: age, sex, race/ethnicity, household income approximated by median income of patient’s residential zip code,8 New Haven residency by zip code, health insurance status (none or public payer versus private payer), prestroke code antiplatelet or anticoagulation use, comorbidities (hypertension, dyslipidemia, diabetes mellitus, atrial fibrillation/flutter, prior transient ischemic attack or stroke, congestive heart failure, coronary artery disease, chronic obstructive pulmonary disease, malignancy, tobacco use, and substance abuse), arrival method (personal transport, emergency medical services usage, or in-hospital stroke code), and preadmission modified Rankin Scale (mRS). Presenting neurological symptoms (categorized into weakness, numbness, speech difficulty, visual symptoms, altered mental status, or other, with each patient assigned as many symptoms as were relevant to their presentation) and National Institutes of Health Stroke Scale scores were abstracted from the initial neurological evaluation. This study includes computed tomography perfusion data performed at YNHH on those patients deemed clinically appropriate by the treating neurologist, with ischemic core and penumbra volumes extracted from automated RAPID (iSchemaView, Menlo Park, CA) reports. The ultimate diagnosis was resolved to ischemic stroke, transient ischemic attack, intracranial hemorrhage, subarachnoid hemorrhage, or nonstroke based on discharge documentation. Testing for severe acute respiratory syndrome coronavirus 2 during the hospital encounter was documented.
Outcomes
Aggregate Analysis Cohort
For the analysis of aggregate stroke volumes, we electronically extracted and evaluated stroke codes at YNHH, GH, and Lawrence and Memorial Hospital in 2020 during each 7-day time interval from January 1 to April 28, 2020. We analyzed stroke code volumes and treatments (intravenous alteplase or mechanical thrombectomy) at YNHH and GH from January 1 to April 28, 2019 and 2020. As a proxy for acute stroke code activity throughout the region, we assessed telestroke video and phone call volume during these time intervals.
Patient-Level Analysis Cohort
Outcomes included in the patient-level analysis were time metrics (last-known-well-to-ED-arrival time, ED arrival to alteplase administration [door-to-needle time], ED arrival to reperfusion [door-to-reperfusion time]), Thrombolysis in Cerebral Infarction recanalization for thrombectomy patients, length of stay (days), stroke pathogenesis per Trial of ORG 10172 criteria,9 and functional status (mRS) at discharge. For wake-up strokes, last well was considered the time of going to bed if known; undetermined last well times were considered missing and were not imputed. Stroke pathogenesis was extracted from the discharge summary reviewed by the supervising vascular neurology attending physician. Discharge mRS was either explicitly stated in the discharge summary or estimated from inpatient therapy notes, using previously validated methods.10
Statistical Analysis
Statistical analyses were performed using SAS 9.4 (Cary, NC). The threshold for statistical significance was established a priori at a P<0.05.
Aggregate Analysis
The number of stroke codes at the 3 hospitals were analyzed from January 1 to April 28, 2020. By scatterplot visualization, we identified time cut points associated with changes in stroke code volumes. We then confirmed these cut points by piecewise linear regression and spline analyses given the nonlinearity of data (Shapiro-Wilk test P<0.0001). To quantify the change in weekly stroke code volume within each timespan defined by the 2 cut points, 3 separate, piecewise linear regression models were fit. Y intercepts (β0), slopes of the independent variable of calendar week (β1), and the R2 associated with each regression model were noted. A linear spline was fit to ascertain the relationship between calendar week and weekly stroke code volume using 2 cut points as knots. We then calculated the observed/expected percentage of stroke codes called at the CSC after cut point observed in the full cohort. Expected stroke codes (in the absence of possible perturbation by the onset of the pandemic) were defined as the median number of stroke codes from week 1 through the week before the first cut point. We also calculated the cumulative number of stroke codes observed after this point compared the number of codes called during the corresponding weeks in 2019.
A cubic spline model was generated to estimate the number of stroke codes called in January through April 28, 2019 versus 2020 at YNHH and GH. The weeks at which the 2 curves intersected were calculated to determine the calendar week at which the number of stroke codes in 2020 dropped below 2019 levels.
Univariate linear regression models were also generated to discern the relationship between calendar weeks and the number of stroke codes called in the ED, stroke codes called in the inpatient setting, and numbers and rates of alteplase administrations or thrombectomies.
Patient-Level Analysis
Categorical and continuous variables are presented as N (%) and median (interquartile range), respectively. Categorical variables during the 2020 epochs (prepandemic: February 1 to 29; pandemic: March 1 to April 28) were compared by either χ2 tests or Fisher Exact test, depending on the number of observations per cell. Continuous variables were compared using the Kruskal-Wallis test. Missing data were not imputed to preserve the integrity of the dataset. No variable had >10% missing data.
Results
Aggregate Level
A total of 822 stroke codes were called at YNHH, GH, and Lawrence and Memorial Hospital from January 1, 2020 to April 28, 2020. There was a significant decline in weekly stroke code volumes at the 3 hospitals from January to April, 2020, with 2.5 fewer stroke codes called each week (P<0.0001, R2=0.7163; Table II in the Data Supplement). We visually identified week 8 (February 18–24) as an inflection point at which the rate of stroke code volumes decreased and week 12 (March 17–23) when the rate stabilized (Figure 2A). Piecewise linear regression analysis demonstrated a nonsignificant slope from weeks 1 to 7, a slope of −12.8 calls/wk from weeks 8 to 11 (P=0.0296, R2=0.9416), and a nonsignificant slope from weeks 12 to 17, although with a lower β0 of 40.3 stroke codes (Table II in the Data Supplement). A linear spline model generated with knots at 8 and 12 weeks is presented in Figure 2B with associated R2 values of 0.8232. At the CSC, a nadir of 21 stroke codes (39.6% of expected) occurred at week 11 (March 10–16; Table III in the Data Supplement). During the pandemic (from weeks 8 onwards), total stroke codes called decreased by 30.0% compared with corresponding weeks in 2019.
Figure 2.
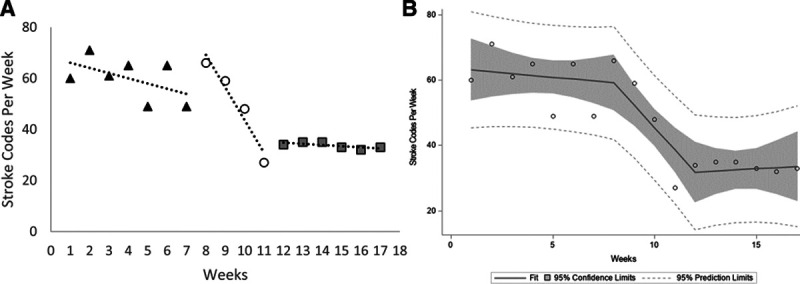
Temporal trends in stroke code calls. A, Piecewise linear regression models from weeks 1–7 (black triangles), weeks 8–11 (unfilled circles), and weeks 12–17 (gray squares). B, Linear spline of weekly stroke codes activated at Yale-New Haven Hospital (YNHH), Greenwich Hospital (GH), and Lawrence and Memorial Hospital (LMH) in 2020.
Between YNHH and GH, there were 786 stroke codes called from January 1 to April 28, 2019, and 756 from January 1 to April 28, 2020. In 2020, for every calendar week, there were on average 2.6 fewer stroke codes called (P<0.0001, R2=0.7085); there was no significant difference across January to April 2019. The cubic spline model for 2019 and 2020 (R2=0.6955) intersected between weeks 9 and 10 (Figure 3). The rate of stroke codes in both ED and inpatient settings also significantly declined. There were no significant associations between calendar week and telestroke consultations, alteplase administration, or thrombectomies (Table II in the Data Supplement).
Figure 3.
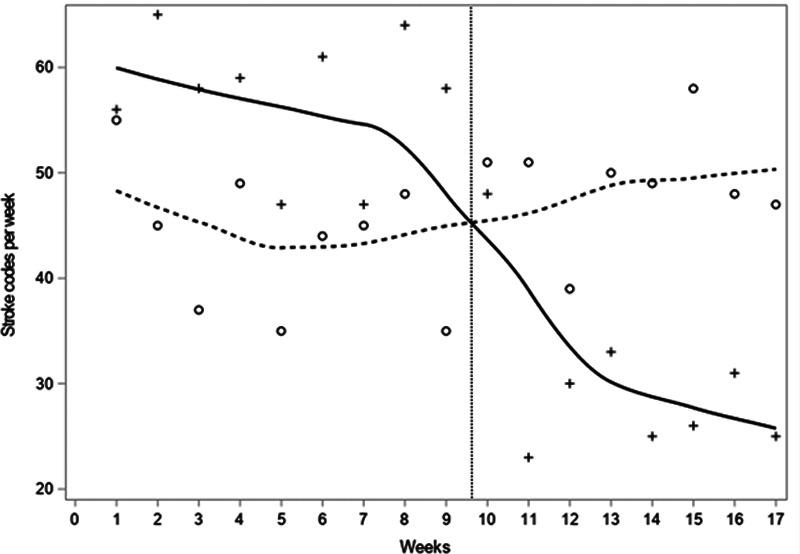
Cubic spline model of weekly stroke codes activated at Yale-New Haven Hospital (YNHH) and Greenwich Hospital (GH) in 2019 (dashed/o) and 2020 (solid/+).
Figure 4 shows the 7-day moving average of daily CSC stroke codes called from March 1 to April 28, 2019 and 2020, with local events superimposed. There was a higher coefficient of variation (compared using Feltz and Miller asymptotic test) in the daily number of stroke codes from March 1 to April 28, 2020 (0.63; 95% CI, 0.51–0.74) compared with March 1 to April 28, 2019 (0.44; 95% CI, 0.36–0.51; P=0.0317). Figure I in the Data Supplement demonstrates the time course of stroke code calls from January 1 to April 28, 2020, by the institution.
Figure 4.
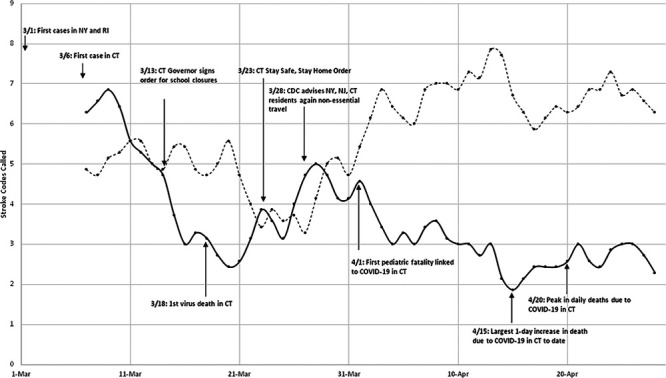
Seven-day moving average of stroke codes activated at Yale-New Haven Hospital (YNHH) in March and April, 2019 (dashed) and 2020 (solid) by calendar day with state, regional, and federal events overlaid. CDC indicates Centers for Disease Control and Prevention; CT, Connecticut; NJ, New Jersey; NY, New York; and RI, Rhode Island.
Patient Level
A total of 378 stroke codes were called at the CSC in 2 epochs: 167 in February 2020 (prepandemic) and 211 from March 1 to April 28, 2020 (pandemic). Pandemic stroke code patients were more likely to have a prior diagnosis of hypertension (P=0.0438), hyperlipidemia (P=0.0149), coronary artery disease (P=0.0433), or substance abuse (P=0.0110), less likely to have private health insurance (P=0.0464), and more likely to live in the CSC city (P<0.0001). There were no significant differences in sex, age, race/ethnicity, premorbid mRS, prestroke antiplatelet or anticoagulation use, histories of diabetes mellitus, atrial fibrillation, prior stroke or transient ischemic attack, congestive heart failure, chronic obstructive pulmonary disease, malignancy, or tobacco use (Table 1).
Table 1.
Patient Characteristics
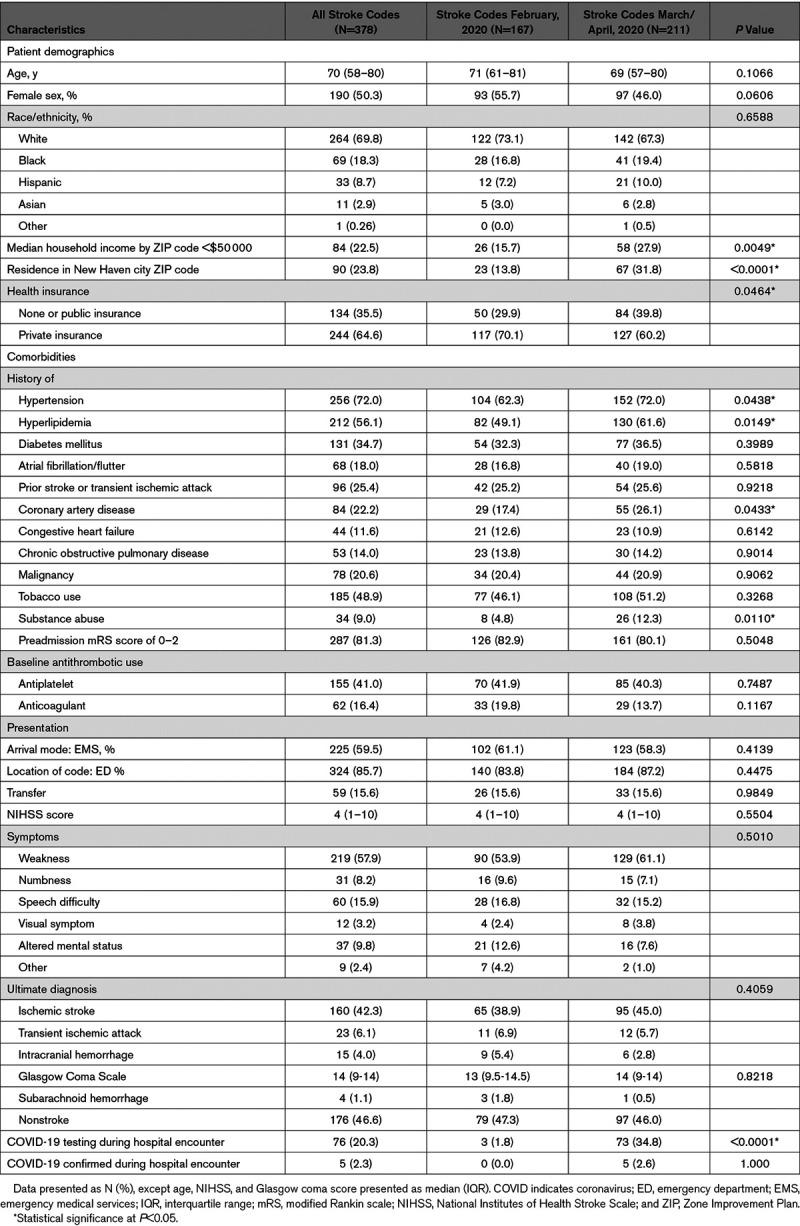
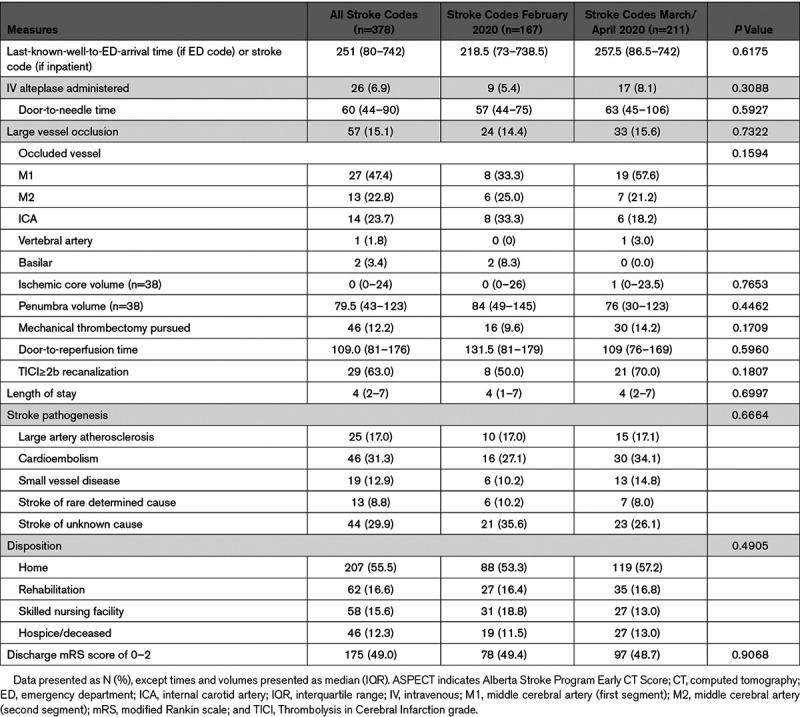
We observed no difference in the proportion of patients presenting by emergency medical services versus walk-in, inpatient versus ED code, transfer status, last well to ED arrival time (if ED code) or stroke code activation time (if inpatient), presenting National Institutes of Health Stroke Scale score, distribution of neurological symptoms, or proportion of stroke codes ultimately diagnosed with stroke. Three percent of the prepandemic cohort was tested for COVID-19 during the index hospital encounter compared with 35% pandemic (P<0.0001), with 5 confirmed COVID-19 cases during the hospital encounter in the pandemic epoch (Table 1). Treatment rates remained similar. Nine patients (5.4%) received intravenous alteplase and 16 (9.6%) underwent mechanical thrombectomy in the prepandemic month versus 17 alteplase (8.1%) and 30 thrombectomy (14.2%) during the 2-month pandemic period (P=0.3088 and 0.1709, respectively). There were no differences in door-to-needle times, door-to-reperfusion times, or rate of Thrombolysis in Cerebral Infarction 2b or greater revascularization and no association between COVID-19 rule-out status and either door-to-needle or door-to-reperfusion times. Radiographic results did not differ between epochs, including ischemic core volume, penumbra volume, and distribution of vessel occlusion among patients with large vessel occlusions.
We observed no significant month-to-month difference in stroke pathogenesis, disposition distribution, median length of stay, or discharge mRS (Table 2).
Table 2.
Process Measures and Outcomes
Discussion
We described hospital presentation for stroke-like symptoms and outcomes of patients in the context of the COVID-19 pandemic. We demonstrated a steep decrease in the rate of stroke code calls from after week 7 (February 11–17) with stabilization but no positive recovery from the decline from weeks 12 to 17 (March 17 to April 28). Stroke code calls in 2020 dipped below 2019 volumes after calendar week 9, corresponding with the March 1 announcement of the first cases of COVID-19 in the neighboring states of New York and Rhode Island. Stroke code calls reached a nadir of 39.6% of expected calls at Week 11 (March 10–16). Our overall 30% decrease in stroke code volumes during the pandemic weeks, relative to 2019, is comparable to that described in recent reports.11,12 We added patient level-data to these observations and found that pandemic-epoch patients were more likely to have histories of hypertension, dyslipidemia, coronary artery disease, and substance abuse, to have no or public health insurance, have lower median household income, and to live in the CSC city. There was no difference in stroke severity or time metrics pre- versus during-pandemic.
All 3 hospitals saw a significant decrease in patients presenting as acute stroke codes during the pandemic, consistent with anecdotes and early data suggesting declines in presentation for non-COVID-19 related medical conditions13–16 including stroke. There is little reason to think that the overall incidence of ischemic stroke decreased during this period. Stroke incidence may increase during humanitarian crises.17,18 COVID-19 may increase stroke risk by mechanisms of hypercoagulability,19 endothelial cell-related vascular inflammation,20,21 systemic inflammation, or complications including myocarditis, heart failure, and dysrhythmias.22,23
There has been speculation that decreases in stroke call volumes may be driven disproportionately by individuals experiencing mild strokes, leading to a self-selection of only more severe stroke patients presenting for emergency care. We found no significant difference in presenting the National Institutes of Health Stroke Scale score or neurological symptoms to support this hypothesis. There was also no narrowing of the distribution of stroke scale scores to suggest that both mild and the most severe strokes were underpresenting. Rather, our data suggest that across the spectrum of stroke severity, patients were less likely to present to the hospital. We also found no differences in age, baseline mRS, or ischemic core or penumbra volumes before and during the pandemic. Although there was no significant increase in the rate of stroke codes undergoing treatment, the absolute number of patients receiving acute treatment were comparable pre- versus during-pandemic. Determination of whether expected treatment opportunities were missed due to lack of emergency presentation warrants further evaluation in a larger cohort.
Patient-level analysis of CSC data demonstrated an increase in stroke code patients living in the CSC city, patients with lower extrapolated income, and patients without private insurance. This may be driven by fewer patients presenting from localities outside of the CSC city during the pandemic, including suburbs and rural communities. Alternatively, socioeconomic factors and insurance status may influence primary care availability, perhaps leading to presentation to the local ED instead. The increased proportion of New Haven residents might indicate that stroke code decreases were driven in part by a redistribution of which hospitals patients present to with stroke symptoms. However, while this is not a population-based study, the YNHH catchment area and telestroke affiliations are broad, and we did not find an increase in telestroke spoke evaluations commensurate with the decrease in hub evaluations. Similarly, a recent study using RAPID software as a surrogate for ischemic stroke code volumes found a decrease in high, medium, and low utilization hospitals, suggesting an overall decrease in acute stroke evaluations.11 Furthermore, even in nonpandemic settings, most strokes occur at home24; thus, individuals spending more time at home during the pandemic would not be expected to cause a large shift in hospital of presentation. Our data ultimately suggest a decrease in overall emergency evaluations for stroke, potentially more marked among patients who live away from CSCs, which are often located in urban, population-dense localities.
A greater proportion of patients in the pandemic epoch had premorbid hypertension, hyperlipidemia, CAD, and substance abuse. The reasons for this are uncertain but may relate to local prevalence in New Haven versus the surrounding areas. It is unlikely to be related to awareness of stroke symptoms, as those with prior stroke or transient ischemic attack were no more likely to present during-pandemic. A nonsignificant trend toward disproportionate declines in women presenting as stroke codes (55.7% prepandemic versus 46.0% during, P=0.0606) is not explained by the sex distribution of New Haven City or county25 and is similar to at least one other report.11 These findings may warrant further evaluation.
Decreases in non-COVID-related emergency medical utilization may be due to public trepidation regarding seeking care at a medical facility. This is supported by a March 28 poll in which 83% of respondents said that they would be either very concerned or moderately concerned if they needed medical treatment right now at a hospital or doctor’s office.26 Undiagnosed acute strokes may be an unintended consequence of social distancing, since typical environments where patients may be seen by others (school, work, and family gatherings) are less available. In the setting of a financial crisis, Americans may be hesitant to seek medical care due to fear of associated costs.27 Early studies suggest an unexpected increase in deaths at home during the current pandemic28; it is conceivable that individuals with large stroke are dying at home, rather than coming to medical attention.
The implications of individuals not seeking emergency medical care during the pandemic may be grave. Fewer patients presenting with acute stroke may translate into missed opportunities for critical, time-sensitive therapy to mitigate stroke mortality and morbidity. Even untreated mild strokes may reflect missed opportunities for secondary prevention measures to offset the risk of a recurrent, potentially more severe stroke.29,30 There is a critical public health imperative to inform individuals that there is a safe pathway through the healthcare system and that they should seek emergency care, even during this ongoing pandemic. During times of social isolation, it is also especially important to maintain routine virtual contact with individuals who may have small social networks and medical comorbidities, such as the elderly living alone. Finally, during a pandemic, it may be valuable to set up telehealth emergency or urgent-care visits to assess patients with acute neurological or other non-COVID medical conditions and guide concerned patients through safe medical care channels.
Stroke time metrics and early outcome measures were preserved during the pandemic, suggesting a robustness in the stroke system to absorb the impact of potential delays secondary to the pandemic. This is notable since stroke systems were actively reconfiguring to minimize COVID-19 exposure by decreasing hospital personnel engaging with patients to the minimum necessary, obtaining collateral from family or caregivers no longer able to accompany patients in the hospital, donning and doffing of personal protective equipment, and sanitization of rooms and equipment. Neither thrombolysis nor thrombectomy was significantly delayed during the pandemic, even when examining patients suspected of having COVID-19.
We acknowledge several limitations. This was a retrospective, pre- and during-analysis and was confined to the constructs of this study design. Patient-level data were only available at our CSC. Piecewise linear regression models are discontinuous and more granular data are needed to further understand the robustness of estimates and relationships between the involved regressions. While there was no significant difference in epoch-related stroke measures and treatment rates, our observational study may not have been powered to detect a subtle difference. A post hoc sample size calculation was performed based on the mean (6.65) and SD (7.46) of National Institutes of Health stroke severity scale in January, 2020, at an α of 0.05 and power of 0.8, with an expected pandemic mean National Institutes of Health stroke severity scale of 9, necessitating 159 patients per cohort to detect a difference. This criterion was reassuringly met in both time cohorts. It is possible that decreases in stroke code volumes were driven by changes in practice patterns with regard to calling stroke codes, rather than patient presentation. However, if this were the case, we might expect a difference in stroke severity or stroke code sensitivity, which were not observed. Individuals seeking medical care after 24 hours would not be expected to be included in our study; however, even if these patients ultimately come to medical attention, we would still be concerned for missed opportunities for acute stroke treatment. The generalizability of our findings is unknown; however, we feel that the data may be useful in understanding patient and hospital behaviors in the setting of this pandemic. GH began performing thrombectomies in January, 2020, extending its stroke code call window to 24 hours at that time. An increase in 2020 stroke code volumes would, therefore, be expected, in contrast there was a significant decrease. Some studies, such as CT perfusion, were used only for selected patients; thus, we would not anticipate their findings to be generalizable to all patients presenting with stroke-like symptoms. We were only able to include early outcome metrics, as of the time of hospital discharge; it is possible that longer follow-up would reveal differences. Our telestroke consultants are not called for all stroke codes at all local hospitals; thus, telestroke numbers may not capture all regional stroke activity. Nonetheless, our study reflects a real-world experience, with trends that may apply more broadly.
Conclusions
We observed a decrease in acute stroke code calls temporally associated with the COVID-19 pandemic. This decrease occurred irrespective of stroke severity, underscoring the need to remind individuals of the importance of seeking emergency medical attention for symptoms concerning for stroke. This may be particularly relevant for those who live further from large hospitals, which are typically located in population-dense areas which patients may be reluctant to approach these during a pandemic. Among those who presented with acute stroke-like symptoms, early time metrics and outcomes were similar before and during the pandemic, indicating that the stroke systems of care were well-preserved. Further studies are needed at a national level to determine whether the patterns observed in this study are generalizable and to identify optimal stroke education and care strategies during this and future pandemics.
Acknowledgments
We acknowledge the stroke coordinators at Greenwich Hospital (Sheryl Feldheim) and Lawrence and Memorial Hospital (Lisa Bedard) for providing us with institutional stroke data.
Sources of Funding
There were no funding sources for this study. Dr Sheth is supported by the National Institutes of Health (NIH; U24NS107136, U24NS107215, R01NR018335, R01NS107215, U01NS106513, and R03NS112859) and the American Heart Association (18TPA34170180 and 17CSA33550004).
Disclosures
Dr Krumholz works under contract with the Centers for Medicare & Medicaid Services to support quality measurement programs; was a recipient of a research grant, through Yale, from Medtronic and the US Food and Drug Administration to develop methods for post-market surveillance of medical devices; was a recipient of a research grant with Medtronic and is the recipient of a research grant from Johnson & Johnson, through Yale University, to support clinical trial data sharing; was a recipient of a research agreement, through Yale University, from the Shenzhen Center for Health Information for work to advance intelligent disease prevention and health promotion; collaborates with the National Center for Cardiovascular Diseases in Beijing; receives payment from the Arnold & Porter Law Firm for work related to the Sanofi clopidogrel litigation, from the Martin/Baughman Law Firm for work related to the Cook Celect IVC filter litigation, and from the Siegfried and Jensen Law Firm for work related to Vioxx litigation; chairs a Cardiac Scientific Advisory Board for UnitedHealth; was a member of the IBM Watson Health Life Sciences Board; is a member of the Advisory Board for Element Science, the Advisory Board for Facebook, and the Physician Advisory Board for Aetna; and is the co-founder of HugoHealth, a personal health information platform, and co-founder of Refactor Health, an enterprise healthcare AI-augmented data management company. Dr Spudich directs a study within the AIDS Clinical Trials Group that receives study medications donated by ViiV Healthcare, Inc. Dr Sheth reports research grant funding from Biogen, Novartis, Bard, Hyperfine, is on the data and safety monitoring board for a study from Zoll, and reports equity in Alva Health. The other authors report no conflicts.
Supplementary Material
Footnotes
Nonstandard Abbreviations and Acronyms
- COVID-19
- coronavirus disease 2019
- CSC
- Comprehensive Stroke Center
- ED
- emergency department
- GH
- Greenwich Hospital
- mRS
- modified Rankin Scale
- YNHH
- Yale-New Haven Hospital
For Sources of Funding and Disclosures, see page 2672 and 2673.
The Data Supplement is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/STR.0000000000000347.
References
- 1.American Heart Association/American Stroke Association Stroke Council Leadership Temporary emergency guidance to US stroke centers during the COVID-19 pandemic. Stroke 2020511910–1912doi: 10.1161/STROKEAHA.120.030023 [DOI] [PubMed] [Google Scholar]
- 2.First Travel-related Case of 2019 Novel Coronavirus Detected in the United States [press release] Centers for Disease Control and Prevention. 2020. January 21, https://www.cdc.gov/media/releases/2020/p0121-novel-coronavirus-travel-case.html. Accessed April 1, 2020
- 3.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 202020533–534doi: 10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murad Y. Most U.S. Adults Practice Some Degree of Social Distancing Amid Coronavirus Spread. Morning Consult. 2020. March 20, https://morningconsult.com/2020/03/20/coronavirus-social-distancing-poll. Accessed April 1, 2020
- 5.Brindley E. Rhode Island, New York announce first coronavirus cases. Hartford Courant. 2020 https://www.courant.com/breaking-news/hc-br-coronavirus-case-rhode-island-20200301-qf7w5gtxybel7bhmlid77iaw24-story.html. Accessed March 30, 2020. [Google Scholar]
- 6.American Hospital Directory. https://www.ahd.com. 2018. Accessed April 1, 2020.
- 7.Schwamm LH, Fonarow GC, Reeves MJ, Pan W, Frankel MR, Smith EE, Ellrodt G, Cannon CP, Liang L, Peterson E, et al. Get With the Guidelines-Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation 2009119107–115doi: 10.1161/CIRCULATIONAHA.108.783688 [DOI] [PubMed] [Google Scholar]
- 8.Income by ZIP Code. Income Statistics for Connecticut Zip Codes. 2018 https://www.incomebyzipcode.com/connecticut. Accessed March 30, 2020.
- 9.Adams HP, Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE., 3rd. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 19932435–41doi: 10.1161/01.str.24.1.35 [DOI] [PubMed] [Google Scholar]
- 10.Zhang W, Coote S, Frost T, Dewey HM, Choi PM. Reliability of the acutely estimated premorbid modified Rankin scale for stroke treatment decision making. J Stroke Cerebrovasc Dis 2019281022–1026doi: 10.1016/j.jstrokecerebrovasdis.2018.12.026 [DOI] [PubMed] [Google Scholar]
- 11.Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of covid-19 on stroke evaluation in the United States. N Engl J Med. 2020:NEJMc2014816. doi: 10.1056/NEJMc2014816. doi: 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thornton J. Stroke: “striking reductions” are seen in number of people with symptoms seeking help [published online April 6, 2020]. BMJ. 2020;369:m1406. doi: 10.1136/bmj.m1406. doi: 10.1136/bmj.m1406. https://www.bmj.com/content/369/bmj.m1406. [DOI] [PubMed] [Google Scholar]
- 13.Woods A. Los Angeles residents are putting off hospital visits over coronavirus fears. New York Post 2020. April 21, https://nypost.com/2020/04/21/la-residents-putting-off-hospital-visits-over-coronavirus-fears. Accessed April 21, 2020 [Google Scholar]
- 14.Bernstein L, Stead SF. Patients with heart attacks, strokes and even appendicitis vanish from hospitals. Washington Post 2020. April 19, https://www.washingtonpost.com/health/patients-with-heart-attacks-strokes-and-even-appendicitis-vanish-from-hospitals/2020/04/19/9ca3ef24-7eb4-11ea-9040-68981f488eed_story.html. Accessed April 20, 2020 [Google Scholar]
- 15.Krumholz H. Where Have All the Heart Attacks Gone? New York Times. Published April 6, 2020. Updated May 14, 2020. https://www.nytimes.com/2020/04/06/well/live/coronavirus-doctors-hospitals-emergency-care-heart-attack-stroke.html. Accessed April 7, 2020. [Google Scholar]
- 16.Garcia S A, M, Meraj P, Schmidt C, Garberich R, Jaffer F, Dixon S, Rade J, Tannenbaum M, Chambers J, Huang P, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020752871–2872doi: 10.1016/j.jacc.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hayman KG, Sharma D, Wardlow RD, Singh S. Burden of cardiovascular morbidity and mortality following humanitarian emergencies: a systematic literature review. Prehosp Disaster Med 20153080–88doi: 10.1017/S1049023X14001356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Swerdel JN, Janevic TM, Cosgrove NM, Kostis JB; Myocardial Infarction Data Acquisition System (MIDAS 24) Study Group The effect of Hurricane Sandy on cardiovascular events in New Jersey. J Am Heart Assoc 20143e001354.doi: 10.1161/JAHA.114.001354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thachil J TN, Gando S, Falanga A, Cattaneo M, Levi M, Clark C, Iba T. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost 2020181023–1026doi: 10.1111/jth.14810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zinkernagel A MM, Schuepbach R, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020395102341417–1418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paniz-Mondolfi A, Bryce C, Grimes Z, Gordon RE, Reidy J, Lednicky J, Sordillo EM, Fowkes M. Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). J Med Virol 202092699–702doi: 10.1002/jmv.25915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020191145–147doi: 10.1016/j.thromres.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Long B, Brady WJ, Koyfman A, Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med 2020381504–1507doi: 10.1016/j.ajem.2020.04.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feng EJ, Orencia AJ, Whisnant JP. Outcome and pathogenesis of stroke is conditioned by place of stroke occurrence. J Stroke Cerebrovasc Dis 199333–8doi: 10.1016/S1052-3057(10)80126-0 [DOI] [PubMed] [Google Scholar]
- 25.U.S. Census Bureau. United States Census Bureau; 2019. U.S. Census Bureau Quick Facts: New Haven County, Connecticut. https://www.census.gov/quickfacts/newhavencountyconnecticut. Accessed March 20, 2020. [Google Scholar]
- 26.Saad L. Gallup; 2020. Gallup’s Data Brief on COVID-19. https://news.gallup.com/opinion/gallup/307667/gallup-covid-data-brief-no.aspx. Accessed April 8, 2020. [Google Scholar]
- 27.Witters D. Gallup; 2020. In U.S., 14% with likely COVID-19 to avoid care due to cost. https://news.gallup.com/poll/309224/avoid-care-likely-covid-due-cost.aspx. Accessed April 30, 2020. [Google Scholar]
- 28.Brown E, Ba Tran A, Thebault R. Excess U.S. deaths hit estimated 37,100 in pandemic’s early days, far more than previously known. Washington Post. 2020 https://www.washingtonpost.com/investigations/2020/05/02/excess-deaths-during-covid-19/?arc404=true. Accessed May 3, 2020. [Google Scholar]
- 29.Nedeltchev K, Baumann C, Haefeli T, Georgiadis D, Arnold M, Baumgartner RW. Organized inpatient (stroke unit) care in very old patients. Neurol Res 200931885–891doi: 10.1179/174313209X382502 [DOI] [PubMed] [Google Scholar]
- 30.Khatri P, Conaway MR, Johnston KC; Acute Stroke Accurate Prediction Study (ASAP) Investigators Ninety-day outcome rates of a prospective cohort of consecutive patients with mild ischemic stroke. Stroke 201243560–562doi: 10.1161/STROKEAHA.110.593897 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


