Summary:
The Virtual Fracture Clinic (VFC) has proved beneficial in reducing footfall within the hospital setting, improving the cost of running a trauma service, while satisfying the majority of referred patients. The mandatory upscaling of telemedicine use, specifically the enhancement of the VFC, amidst the COVID-19 pandemic, was analyzed. The remit of the VFC within our hospital was expanded so as to include all referred ambulatory trauma. Outcomes of our VFC review over the 6-week period following the introduction of the national Irish COVID-19–related restrictions were gathered. These outcomes were analyzed and compared with the corresponding 6-week period from 2019. A 77.2% increase in the VFC referral volume was observed throughout the COVID-19–related period. Patients were directly discharged in 55.2% of cases in 2020, as opposed to 47.8% in 2019 (P = 0.044); referred directly for physiotherapy in 32.9% of cases in 2020, as opposed to 28.9% in 2019 (P = 0.173); and referred to a fracture clinic in 11.9% of cases in 2020, as opposed to 23.7% in 2019 (P < 0.001). Also, 3.0% of patients returned to the clinic after discharge in 2020, compared with 4.4% in 2019 (P = 0.237); 4.5% of patients were referred for surgery in 2020, as opposed to 2.2% in 2019 (P = 0.105). The VFC proved to be an efficient tool in managing ambulatory trauma throughout the pandemic. Upscaling the VFC to include all ambulatory trauma is a safe, effective method in reducing clinic attendances and hospital footfall, whilst ensuring that high care standards are maintained.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
Key Words: virtual fracture clinic, practice management, service provision, quality improvement, fracture clinic, COVID-19
INTRODUCTION
Innovative practice changes have rapidly developed throughout the COVID-19 pandemic, which has served as a catalyst for accelerated change.1,2 It is hoped that these developments will ultimately improve the care of patients with musculoskeletal ailments, as progress is made toward providing a comprehensive trauma and elective orthopaedic service once social distancing restrictions are lifted.
The Glasgow Royal Infirmary produced the Virtual Fracture Clinic (VFC) pathway in 2011, whereby suitable patients could be safely managed remotely by an orthopaedic surgeon.3 Following plain film radiograph review, patients could be booked to attend a fracture clinic, attend for physiotherapy, or were discharged directly from the emergency department (ED). Treatment included that of a removable strapping, splint, or boot, as well as an information leaflet, which included the necessary contact information should any concerns arise. Two-thirds of patients meeting the Glasgow criteria may be managed virtually, which has the benefits of reducing footfall within the hospital setting, significantly improving the costs associated with running a trauma service, while satisfying up to 97% of all referred patients.4,5
Our previous experience with virtual clinics has been a huge boon in our service provision during the period of national measures implemented to limit the spread of COVID-19. “Social distancing” has become a widespread practice, and it is a vital public health initiative to reduce exposure and curtail viral spread.6 Within our department, we have expanded the remit of our VFC to include all referred ambulatory trauma, minimizing footfall within the hospital and reducing exposure of our vulnerable cohort of patients. A disproportionately high mortality rate is linked to the frequency of outpatient attendances amidst the recent pandemic.7
We examined our department's experience in the mandatory upscaling of telemedicine use for ambulatory trauma, specifically our enhancement of the VFC in light of the current crisis, describing its effect on our delivery of care in a safe, socially distanced manner.
METHODS
The Midlands Regional Hospital Tullamore (MRHT) VFC database was audited to identify all patients who were referred during the 6-week period following the introduction of the National Irish COVID-19–related restrictions. We assessed the corresponding 6-week period from 2019 as a comparison group.
MRHT is a regional Irish trauma center, covering a population of more than 400,000 people, comprising 3 EDs.8 One ED is located at our institution, whereas 2 other district hospitals serve as outside referral units. Our unit was an early advocate for telemedicine incorporation and was established as Ireland's pilot VFC site in 2016.4 Referrals to the VFC include all injuries that can be managed with a removable splint, boot, or shoe, so as to facilitate self-removal following treatment completion. Since the first Irish COVID-19 case was reported, our VFC has expanded to include all ambulatory trauma cases referred to the unit from all ED sources.
All referrals were reviewed on the following working day by an orthopaedic surgeon, an orthopaedic nurse specialist, and an extended scope physiotherapist (ESP) in the scheduled VFC. Cases requiring surgery were booked directly to the trauma ward, making use of the day-of-surgery-admission (DOSA) pathway. Patients necessitating early clinical review were booked to attend either a general fracture clinic or a subspecialty trauma clinic within that coming week. Stable injury patterns, requiring early physiotherapy, were booked directly to attend the ESP clinic. Virtual physiotherapy sessions began throughout the study period, making use of video conferencing software. Patients suitable for direct discharge had an injury-specific information leaflet posted to their address, outlining when to remove their splint, demonstrated their prescribed rehabilitation program, and highlighted the necessary contact information. Each patient subsequently received a phone call, so as to have the above explained in detail.
Outcomes of our VFC review over the 6-week period following the introduction of the national Irish COVID-19–related restrictions on the March 20, 2020, were gathered. These outcomes were analyzed and compared with the corresponding 6-week period from 2019. The referral volume from outside institutions, as well as the number of patients who were discharged, referred to an ESP clinic, referred to the fracture clinic, and referred for surgery were noted for both years. The number of patients opting to return to the fracture clinic, following discharge was also compared between both periods.
Chi-square testing was used to compare the data between both periods. Statistical analysis was performed using IBM SPSS version 26 (IBM Corp Released 2019; IBM SPSS Statistics for Mac, Version 22.0. Armonk, NY: IBM Corp).
RESULTS
In the 6 weeks that followed the introduction of national COVID-19–related restrictions in early 2020, 404 patients were referred to the VFC. Throughout the corresponding 6-week period in 2019, 228 patients were referred, signifying a 77.2% increase in referred patient volume in 2020.
The proportion of referrals originating from outside institutions increased by 21.1% between the 2 time intervals—35.1% in 2020 from 14.0% in 2019 (P < 0.001).
Shown in Table 1 and Figure 1 are the outcomes of the VFC referrals for both the 2020 and 2019 on a 6-week period. Patients were discharged from the VFC following x-ray review in 55.2% of cases in 2020, as opposed to 47.8% in 2019, which showed statistical significance (P = 0.044). Patients were referred directly to the physiotherapy clinic from the VFC in 32.9% of cases in 2020, as opposed to 28.9% in 2019, which did not show statistical significance (P = 0.173); 11.9% of patients were brought to a fracture clinic in 2020, as opposed to 23.7% in 2019, which showed statistical significance (P < 0.001).
TABLE 1.
Data Comparison Between the 6-Week Time Periods of 2020 and 2019
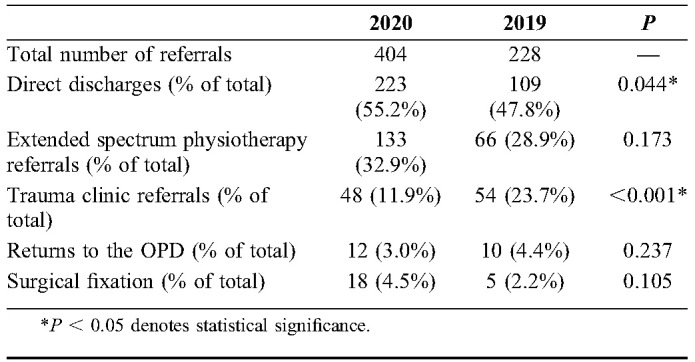
| 2020 | 2019 | P | |
| Total number of referrals | 404 | 228 | — |
| Direct discharges (% of total) | 223 (55.2%) | 109 (47.8%) | 0.044* |
| Extended spectrum physiotherapy referrals (% of total) | 133 (32.9%) | 66 (28.9%) | 0.173 |
| Trauma clinic referrals (% of total) | 48 (11.9%) | 54 (23.7%) | <0.001* |
| Returns to the OPD (% of total) | 12 (3.0%) | 10 (4.4%) | 0.237 |
| Surgical fixation (% of total) | 18 (4.5%) | 5 (2.2%) | 0.105 |
P < 0.05 denotes statistical significance.
FIGURE 1.
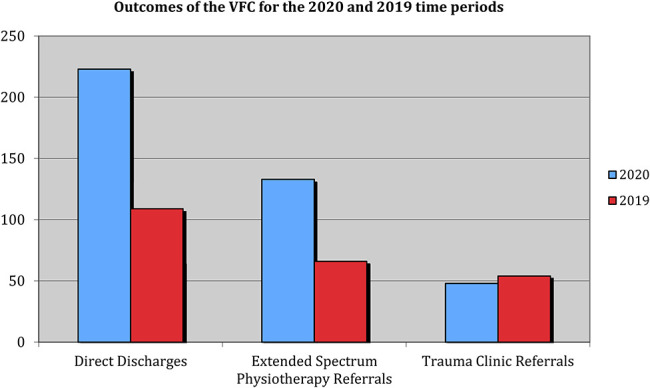
Outcomes of the VFC for the 2020 and 2019 periods.
Twelve patients returned to the clinic for subsequent review following discharge in 2020, which equated to 3.0% of all COVID-19–related VFC referrals. Ten patients re-presented to the clinic over the 2019 comparison period, which signified a return rate of 4.4%; χ2 testing showed this not to be a statistically significant difference (P = 0.237).
Of the total VFC referrals in 2020, 18 patients (4.5%) required surgery, as opposed to 5 patients (2.2%) in 2019. The observed increase in the proportion of cases requiring surgical intervention was not found to be statistically significant (P = 0.105).
DISCUSSION
The number of patients reviewed in the VFC increased by 77.2%, from 228 patients during the 6-week period in 2019, to 404 patients in 2020. Three scheduled virtual sessions were conducted each week throughout 2019; however, this was increased to 5 weekly sessions in 2020, so as to accommodate for the anticipated surge in referral volume. “Social distancing” throughout the community has proven to be a vital measure in reducing the spread of COVID-19.9,10 Virtualizing the fracture clinic, thereby minimizing footfall, has served as a social distancing measure within the hospital setting. Protocolized care pathways, derived from the Glasgow VFC criteria, have been shown to enhance patient flow via the reduction of waiting times for both patients and their family members presenting to the ED with musculoskeletal trauma.5 Throughout Irish fracture clinics, the doctor–patient interaction period has narrowed by a factor of 65% during the COVID-19 period.11 Clinic attendances within our trauma unit reduced from a mean of 68 to fewer than 10 patients in the 4 weeks following the introduction of national measures, in an effort to “flatten the curve.”12 Increasing the volume of virtual referrals within our institution has served as an effective, pragmatic tool in reducing the exposure risk for both patients and staff.
Expansion of the TAC took 2 forms. First, all ambulatory trauma was deemed suitable for virtual review, in light of measures taken to reduce footfall within the hospital. Fractures of the hip and long bones continued to undergo admission for surgical fixation via the on-call orthopaedic team. Patients requiring clinical review were directed to the necessary subspecialty clinic, so as to expedite expert opinions on the most appropriate management plan. Moulded casts, where applicable, were applied by the on-call orthopaedic team in the ED, so as to prevent interval fracture displacement necessitating surgical intervention. Plaster of paris backslabs were converted to casts via the daily fracture clinic, in a dedicated afternoon nurse-led casting session. Repeat x-rays, post cast application, were reviewed thereafter by the orthopaedic team on call, where necessary.5,13
Second, the COVID-19 pandemic saw the VFC expand from one on-site ED referring stable injuries, to 3 affiliated EDs referring all trauma presentations. Midlands Regional Hospital Portlaoise had engaged with the VFC process since August 2018, but Midlands Regional Hospital Mullingar began to refer patients virtually after the 2019 study period. Throughout the studied 2020 COVID-19–related period, the ED of both neighboring hospitals in Mullingar and Portlaoise were referring patients to the VFC, which would account for an independent increase in referral volume. Secondary imaging, when required following VFC review, was arranged within either referring unit. Virtual follow-up was facilitated remotely, via the National Integrated Medical Imaging System (NIMIS),14 which expedited further reductions in the volume of patients physically presenting to the fracture clinic in the weeks that followed.
Upscaling the VFC by 77.2% was shown to be a safe intervention. There was no significant difference in the rates of patients returning to clinic, or patients referred for surgery, between the 2 periods. Less than 3% of all referrals re-presented to the clinic with queries in 2020 following discharge, a decrease from 4.4% in 2019. Of patients reviewed during the 2020 timeframe, 4.5% required surgical intervention, as opposed to 2.2% during 2019.
Neither the difference in rate of clinic returns nor the rate of surgical intervention were statistically significant between the 2 studied periods, thus implying an equivalence between the upscaled and routine VFC processes in terms of safety and reproducibility. Throughout COVID-19, patient queries were more likely to have been dealt with via phone calls, virtual reviews, and additional physiotherapy sessions. The reduction in return rate may in part be attributed to patient anxiety caused by the risk of COVID-19 exposure by way of a hospital visit. Patients reviewed by the ED team who required surgical intervention were referred either to the on-call orthopaedic team or sent directly to the fracture clinic for review, throughout 2019. The VFC was not previously seen as an appropriate destination for patients likely requiring operative fixation. A higher proportion of all trauma presentations, including those likely requiring fixation, have been referred to the VFC throughout the pandemic so as to facilitate patient flow through the ED. Although the overall surgical volume decreased throughout 2020, the proportion of injuries requiring surgery presenting to the VFC did marginally increase. Borderline surgical cases were more likely to have been managed conservatively, in light of published guidelines, as well as the findings of notable pragmatic, multicenter, randomized control trials.15–17 Anecdotally, when given the choice between operative and conservative management options, patients were often found to favor the latter throughout 2020.
Each of the 144 VFC patients referred to the extended spectrum physiotherapist throughout the COVID-19 pandemic were managed virtually via telehealth, which consisted of phone, video call, and email consultations. The use of telehealth has been shown to increase exercise adherence for a variety of musculoskeletal conditions18 and has reported high levels of patient satisfaction.19 Our prompt adaptation from the physical to “virtual” interaction with our patients was expedited by having an existing “OrthoLive” hub available on site in MRHT to easily access our online telehealth communications. Onward referral of patients continued to those community physiotherapy sites conducting telehealth consultations. Of the 10 patients re-presenting to the clinic over the 2019 period, 2 were re-referred from physiotherapy. This compares with 1 patient re-referral from physiotherapy of the 12 re-attending trauma clinics during the COVID-19 period in 2020.
Although 2 periods of 6 weeks were assessed, the range of injury patterns seen throughout the 2020 group was more varied. The 2019 study group consistently contained fractures managed with removable splints, in line with the established VFC protocols. The COVID-19 pandemic inspired the virtual management of musculoskeletal trauma. Guidelines on trauma management varied throughout the pandemic, due to the high turnover of recommendations amidst evolving public health advice. As such, the weekly volume of referrals to the VFC increased successively throughout the pandemic-related study period. The rate of surgical intervention did not increase in proportion to the enlarging volume of referrals. The VFC was a consultant-led outpatient session, and thus it was used as a means to standardize the management of trauma within the unit, as protocols developed throughout the 6-week period.
This is the first study to focus on the safety of upscaling the use of VFCs to include all ambulatory trauma in light of the COVID-19 pandemic. Maximizing the use of telemedicine in the outpatient setting is a safe, reliable means to reduce footfall within hospitals and minimize nosocomial disease spread. Trauma units operating without a VFC should consider establishing a similar pathway, so as to reduce the number of clinic attendees, while maintaining care standards and boosting patient satisfaction levels amidst recent anxiety.20–22 VFCs have proven to be a cost-saving intervention4,22,23 and have allowed for the generation of additional resources at this vital juncture. Upscaling the use of virtual clinics has undoubtedly served as an effective weapon in the fight against COVID-19.
CONCLUSIONS
The VFC is an efficient tool in managing ambulatory trauma throughout a pandemic. Upscaling the VFC to include all ambulatory trauma is a safe, effective method in reducing clinic attendances and hospital footfall, whilst ensuring that high care standards are maintained.
Footnotes
The authors report no conflict of interest.
REFERENCES
- 1.Reilly MFO, Merghani KM, Sheehan EC. Virtualised care and COVID-19. Ir J Med Sci. 2020. doi: 10.1007/s11845-11020-02269-11845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haddad FS. COVID-19 and orthopaedic and trauma surgery. Bone Joint J. 2020;102-B:545–546. [DOI] [PubMed] [Google Scholar]
- 3.Jenkins PJ, Gilmour A, Murray O, et al. The Glasgow fracture pathway: a virtual clinic. BJJ News. 2014:22–24. [Google Scholar]
- 4.O'Reilly M, Breathnach O, Conlon B, et al. Trauma assessment clinic: virtually a safe and smarter way of managing trauma care in Ireland. Injury. 2019;50:898–902. [DOI] [PubMed] [Google Scholar]
- 5.Vardy J, Jenkins PJ, Clark K, et al. Effect of a redesigned fracture management pathway and virtual fracture clinic on ED performance. BMJ Open. 2014;4:e005282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stein R. COVID-19 and rationally layered social distancing. Int J Clin Pract. 2020;6:e13501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisher D, Heymann D. The novel coronavirus outbreak causing COVID-19. BMC Med. 2020;18:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Census 2016. Ireland: Central Statistics Office; 2017. [Google Scholar]
- 9.Lewnard JA, Lo NC. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect Dis. 2020;20:631–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koo JR, Cook AR, Park M. Interventions to mitigate early spread of COVID-19 in Singapore: a modelling study. Lancet Infect Dis. 2020;20:678–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheridan G, Boran S, Taylor C, et al. Pandemic adaptive measures in a major trauma center: coping with COVID-19. J Patient Saf. 2020;16:177–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feeley I, McAleese T, Clesham K, et al. Foot and ankle service adaptation in response to COVID-19 and beyond. Ann Med Surg. 2020;54:62–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaudhry S, DelSole EM, Egol KA. Post-splinting radiographs of minimally displaced fractures: good medicine or medicolegal protection? J Bone Joint Surg Am. 2012;94:e128. [DOI] [PubMed] [Google Scholar]
- 14.O'Reilly MF, Breathnach OP, Mohamed KM, et al. The national integrated medical imaging system [NIMIS]-friend, Not Nimesis! Ir. J Med Sci. 2019;188:365–369. [DOI] [PubMed] [Google Scholar]
- 15.Rangan A, Handoll H, Brealey S, et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. JAMA. 2015;313:1037–1047. [DOI] [PubMed] [Google Scholar]
- 16.Griffin D, Parsons N, Shaw E, et al. Operative versus non-operative treatment for closed, displaced, intra-articular fractures of the calcaneus: randomised controlled trial. BMJ. 2014;349:g4483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.BOA Trauma Committee; BOAST—Management of Patients with Urgent Orthopaedic Conditions and Trauma during the Coronavirus Pandemic. Available at: https://www.boa.ac.uk/resources/covid-19-boasts-combined.html. Accessed May 29, 2020. [Google Scholar]
- 18.Bennell K, Marshall C, Dobson F, et al. Does a web-based exercise programming system improve home exercise adherence for people with musculoskeletal conditions?: a randomized controlled trial. Am J Phys Med Rehabil. 2019;98:850–858. [DOI] [PubMed] [Google Scholar]
- 19.Moffet H, Tousignant M, Nadeau S, et al. Patient satisfaction with in-home telerehabilitation after total knee arthroplasty: results from a randomized controlled trial. Telemed Ehealth. 2017;23:80–87. [DOI] [PubMed] [Google Scholar]
- 20.Williams SC, Hollins D, Barden-Marshall S, et al. Improving the quality of patient care: patient satisfaction with a nurse-led fracture clinic service. Ann R Coll Surg Engl. 2003;85:115–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jayaram PR, Bhattacharyya R, Jenkins PJ, et al. A new virtual patient pathway for the management of radial head and neck fractures. J Shoulder Elbow Surg. 2014;23:297–301. [DOI] [PubMed] [Google Scholar]
- 22.Mackenzie SP, Carter TH, Jefferies JG, et al. Discharged but not dissatisfied: outcomes and satisfaction of patients discharged from the edinburgh trauma triage clinic. Bone Joint J. 2018;100-B:959–965. [DOI] [PubMed] [Google Scholar]
- 23.Anderson GH, Jenkins PJ, McDonald DA, et al. Cost comparison of orthopaedic fracture pathways using discrete event simulation in a Glasgow hospital. BMJ Open. 2017;7:e014509. [DOI] [PMC free article] [PubMed] [Google Scholar]


