Abstract
Objectives
The following primary objectives of this study were to: (1) establish baselines of prevalence and causes of medical errors experienced by Iowans in medical settings, (2) determine whether Iowa patients were informed of the errors by the responsible healthcare providers, (3) understand reasons why Iowans who experienced medical errors did or did not report the errors, and (4) discover how Iowans view mandatory reporting of medical errors.
Methods
A total of 1010 Iowa adults took part in a telephone survey in summer 2017. Interviews were completed via random landlines and random digit dialing of cell phone numbers.
Results
Nearly one fifth of surveyed Iowa adults (18.8%) reported being involved in a medical error in their own care or in the care of someone close to them, and yet only four in 10 (39.1%) were notified of the error by the responsible provider. Most Iowans strongly agree that Iowa hospitals (79.5%), physicians (74.1%), and nursing homes (82.2%) should be required to report all medical errors to the patient and to a state agency.
Conclusions
A significant proportion of Iowans will experience a medical error. They also desire full transparency from healthcare providers with respect to medical errors, including notifying the patient when an error occurs and mandating that providers report errors to a state-based agency. Iowa regulators should carefully assess and initiate stringent regulatory guidelines for mandatory reporting of medical errors.
Key Words: medical errors, patient safety, culture of safety, incident reports, survey, Iowa, preventable adverse events
Medical Errors in Iowa: Prevalence and Patients' Perspectives. In the United States, the number of patients harmed by hospitals, clinics, and nursing homes due to medical errors (also called preventable adverse events) is largely unknown. Many medical errors are never reported voluntarily.1 Because the Institute of Medicine's (IOM) report on medical errors2 was released nearly 20 years ago, the progress in reducing preventable harm has been slow and limited.3 A 1997 National Patient Safety Foundation (NPSF) report found that as many as 42% of respondents reported that they, or a close friend or relative, had experienced a medical mistake,4 with the same result (42%) in a similar 2002 study.5 When the data were collected again in 2017, the NPSF found that although improvements in some areas of patient safety have been made, the same percentage (41%) of Americans reported that they had experienced a medical error either personally or secondhand.6 The lack of transparency and sluggish response to the problem of medical errors has led some to list the preventable harm due to medical errors as a national public health crisis.7
Quantifying the magnitude of the medical error problem is an essential first step toward solving these safety issues. However, the United States does not have a bona fide national strategy to assess medical errors. Although the United States has safety and collaborative bodies that advance patient safety initiatives such as the Centers for Medicare and Medicaid Services, there is no independent central coordination group, similar to the Federal Aviation Administration, to align all of the organizations involved in patient safety for reporting and investigative purposes. Because of this lack of centralized oversight, hospitals and clinicians around the country do not report medical errors accurately and consistently.8 Krause et al.9 indicated “The only way patient safety as a whole can be presently evaluated in the United States is by resource-intensive studies that sample provider records and count the number of adverse events.” Determining progress with regard to medical errors requires a baseline from which to compare future results. Currently, we do not have the data to serve as that baseline.
Specific Objectives
Iowa is a largely racially homogeneous Midwestern, US state with a population of 3.1 million. Before this study, the prevalence of medical errors in Iowa was largely unknown. The Iowa Patient Safety Study was designed to establish a current baseline of patient-reported medical errors in Iowa. Patient's reports of medical errors are important, in that patients have the capacity to serve as “vigilant partners” in their own safety and have been identified as an important aspect of safety improvement strategies.10
The following key objectives of this study were to: (1) establish initial baselines of prevalence and causes of medical errors experienced by Iowans in medical settings, (2) determine whether Iowa patients were informed of the errors by the responsible healthcare providers, (3) understand reasons why Iowans who experienced medical errors did or did not report the errors, and (4) discover how Iowans view mandatory reporting of medical errors by medical providers.
METHODS
Survey Development
Permission was granted from researchers at the Harvard Opinion Research Program (HORP), Harvard School of Public Health (HSPH) to adapt the 2014 survey instrument used in The Public's Views on Medical Error in Massachusetts.11 The authors developed two additional questions to the HSPH instrument, which addressed (1) the degree to which the error had financial consequences and (2) the type of medical insurance the injured party had when the error occurred. Data collection and analysis were conducted by Data Point Research, Inc.
Sampling Procedure
Of 7256 Iowans contacted, 1010 Iowans fully completed the survey. From May 11 to June 6, 2017, a telephone-based data collection survey was completed using 451 interviews on numbers called via a random selection of landlines within Iowa's area codes. A further 559 interviews were completed using random-digit dialing of cell phone numbers issued in Iowa.
All responses, including medical error experiences, were self-reported. Similar studies used self-report approaches to successfully examine medical errors, including errors that had not been identified by existing healthcare incidence reporting systems,12 and evidence suggests that respondents are able to report their own safety information effectively and reliably.13–19
Analyses
Weighting
Poststratification weights were calculated to align sample characteristics of the study with the overall population characteristics of Iowans with regard to both sex and age category. In particular, the participant totals for sex (male or female) within each age group category (18–29, 30–49, 50–64, ≥65 years) were converted into proportions of the total sample. The same proportions were also calculated for sex and age category from the entire population of Iowa based on Census data (American Community Survey, 2015). Finally, weights were computed that adjusted the sample proportions to match the population proportions, and these weights were applied to each subject's data given their sex and age.
Analyses
Survey items are reported as the percentage of respondents selecting each response option, of all valid responses for each item. Percentages were computed using weighted data to better represent the population of Iowans at large. Survey results for items using a Likert-type rating scale were computed as the average rating for all respondents who provided a valid response, again using weighted data.
RESULTS
Medical Errors
Overall, 39.3% of Iowans reported knowing what the term “medical error” means, whereas slightly fewer (32.9%) of Iowans reported never having heard of the term “medical error,” and 26.8% report having heard of the term but were not sure of what it means. Given the varied level of familiarity, the term “medical errors” was defined for all respondents in the survey instrument as: “Sometimes when people receive medical care, mistakes are made. These mistakes sometimes result in no harm; sometimes they may result in additional or prolonged treatment, disability or death. These types of mistakes are called medical errors.”
Study participants were then asked about their personal experiences with medical errors. Critically, 18.8% of respondents reported that they, or someone close to them, had experienced a medical error in the last 5 years. Of those who reported experiencing a medical error, most were medical mistakes made in the care of someone close to the respondent (57.3% of those reporting a medical error, 10.9% of all respondents), rather than in the care of the respondent themselves (34.5% of those reporting a medical error; 7.9% of all respondents).
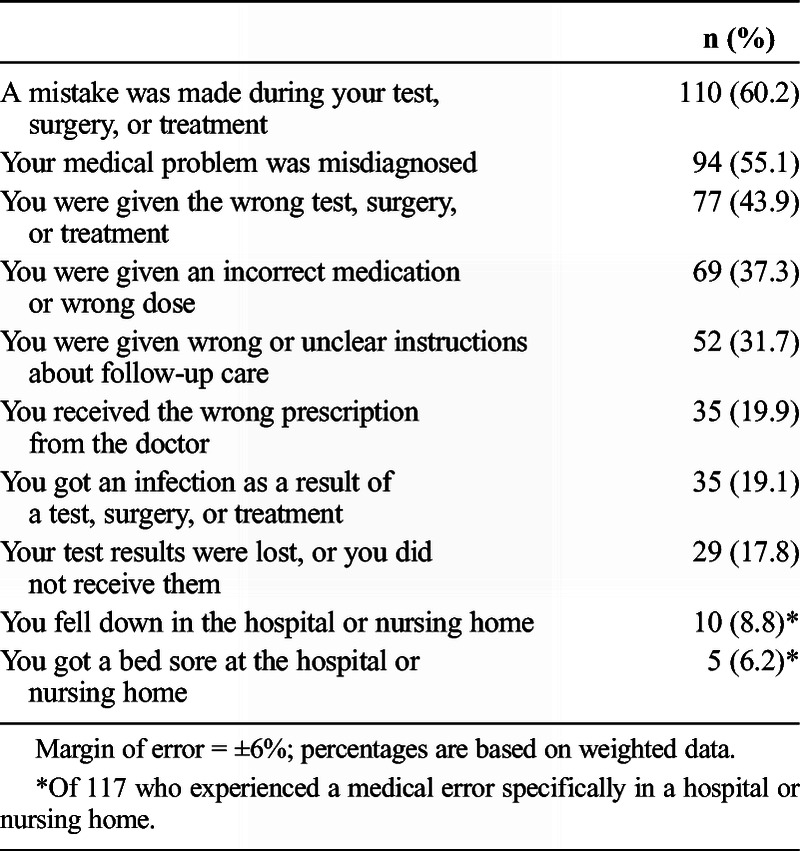
The most common type of medical error was a mistake during a medical test, surgery, or treatment (60.2%), followed closely by a misdiagnosis (55.1%). Just less than half of respondents who experienced a medical error reported being given the wrong test (43.9%) and 37.3% reported that they were given wrong medication or the wrong dose (Table 1). Twice as many medical errors were reported to have occurred at a hospital (58.5%) than at a doctor's office (29.5%). Despite varied types and locations of errors, most respondents (59.5%) reported that the medical error had serious health consequences, whereas only 22.9% reported minor health consequences and 17.2% reported no consequences. Additional health consequences often create additional financial burdens. Almost one-third (32.1%) of respondents reported that they experienced “serious” financial consequences from the medical mishap.
TABLE 1.
Medical Errors Experienced (n = 180 Respondents Who Experienced a Medical Error)
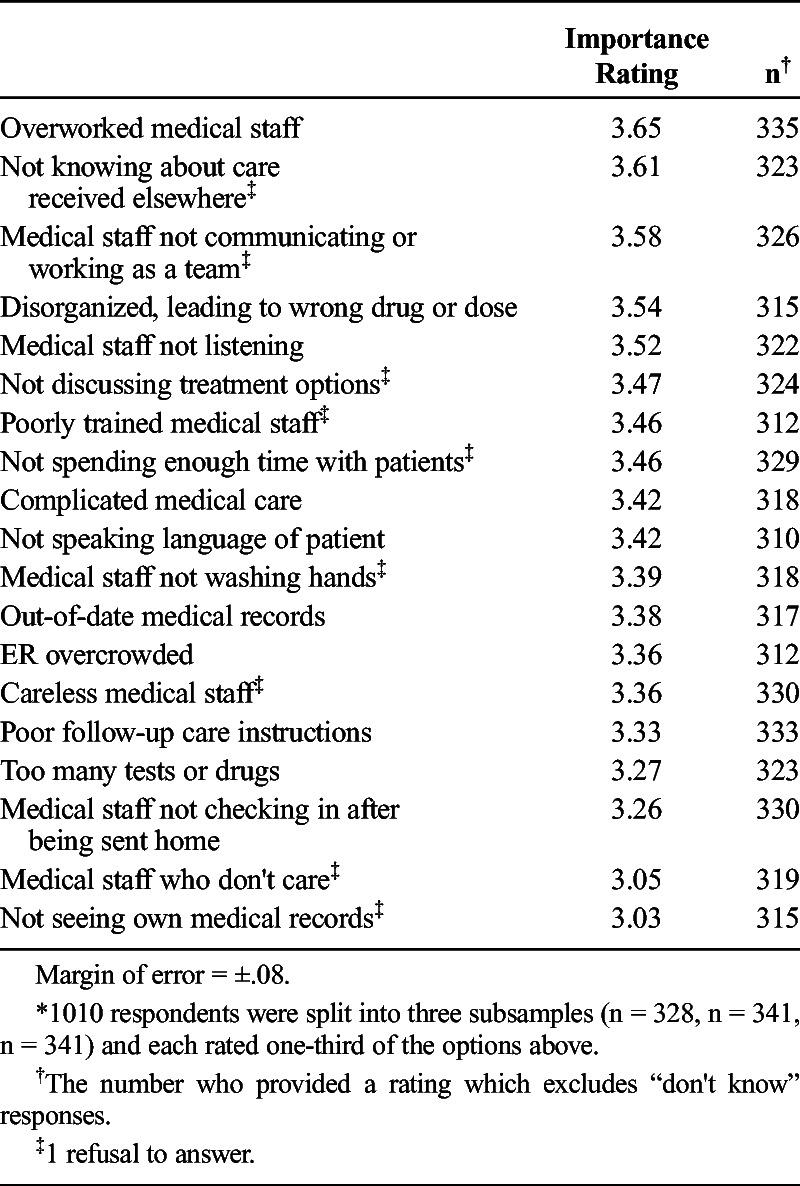
Respondents were asked to rate the importance of several potential causes contributing to medical errors (1 = not at all important, 4 = very important) (Table 2). The three most important reasons were that medical staff were overworked (3.65), staff did not know about care the patient received elsewhere (3.61), and the medical staff not working as a team (3.58). The two items rated least important in their contribution to medical errors were not seeing their own medical records (3.03), and medical staff who do not care about their work (3.05).
TABLE 2.
Average Importance Ratings of Beliefs Regarding Potential Causes of Medical Errors (1 = Not Important at All, 4 = Very Important) (N = 1010 Respondents Who Completed the Survey)*
Reporting Medical Errors
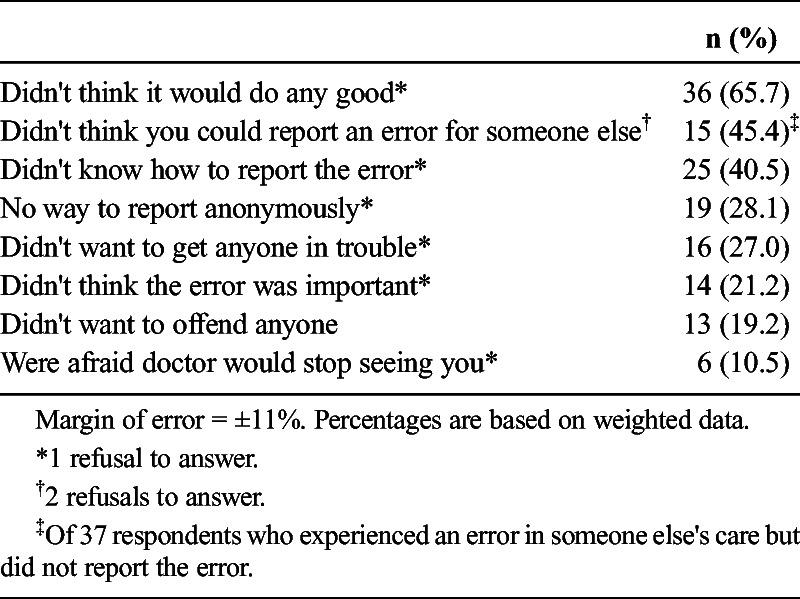
Only 39.1% of those who reported experiencing a medical error were informed by medical staff that a medical error had occurred. However, patients reported their medical error 61.5% of the time, most often to the medical staff where the error occurred (78.8%) (Table 3). Most (88.9%) of those who informed staff of the error did so to prevent further errors happening to other patients, suggesting altruistic reasons for reporting rather than financial or litigious ones (Table 4). For those who decided not to report the error, 65.7% stated that they did not think that it would do any good. A lack of knowledge of who could report the error (45.4%) or how to report the error (40.5%) were also important reasons errors were not reported (Table 5).
TABLE 3.
To Whom the Medical Error Was Reported? (n = 69 Respondents Who Experienced and Reported a Medical Error)
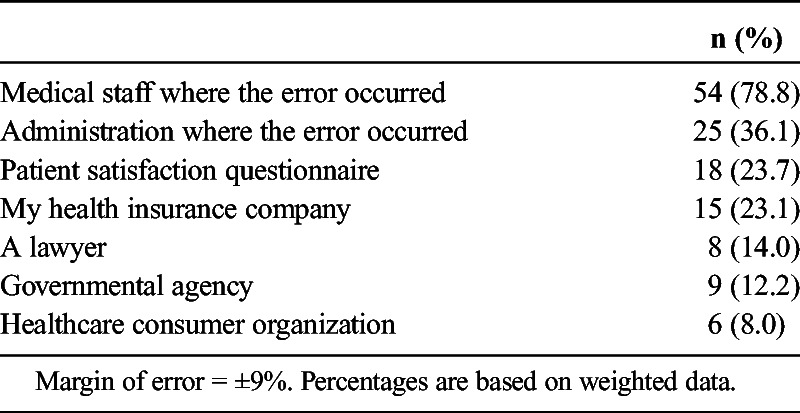
TABLE 4.
Reasons the Medical Error Was Reported (n = 69 Respondents Who Experienced and Reported a Medical Error)
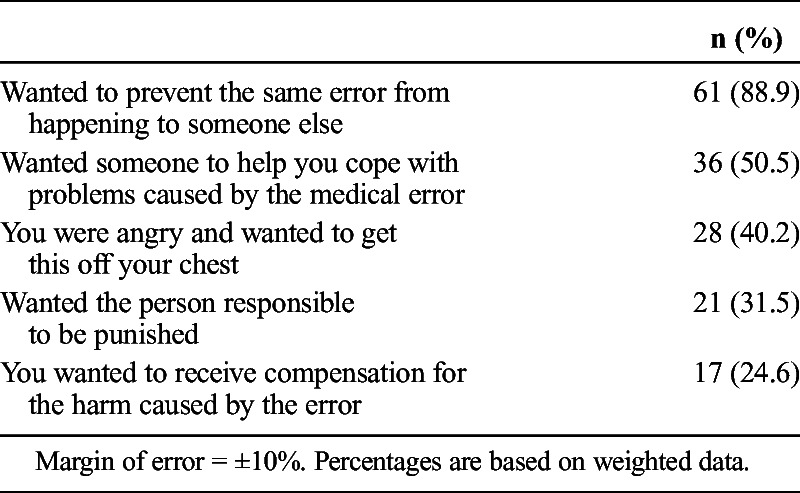
TABLE 5.
Reasons the Medical Error Was Not Reported (n = 58 Respondents Who Experienced a Medical Error but Did Not Report It)
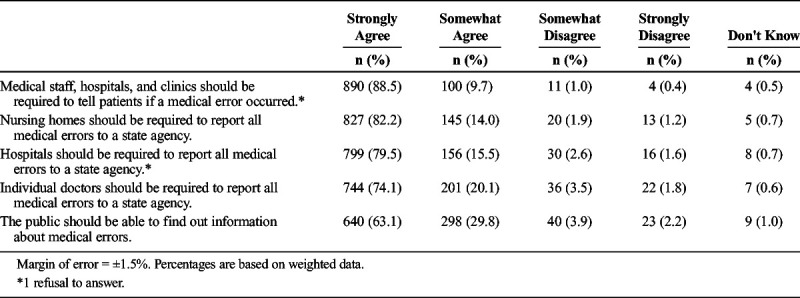
Beliefs About Regulatory Requirements for Reporting Medical Errors
Table 6 shows the agreement with several statements regarding reporting requirements for medical clinics and staff. Most respondents (88.5%) strongly agree that all providers should tell patients if a medical error occurred in their treatment. In addition, most strongly agree that nursing homes (82.2%), hospitals (79.5%), and doctors (74.1%) should be required to report all medical errors to a state agency. Moreover, 63.1% strongly agree that this information should be made available to the general public.
TABLE 6.
Agreement With Reporting Requirements (N = 1010 Respondents Who Completed the Survey)
DISCUSSION
This study is noteworthy because they are derived from one of only a few state-specific studies performed in the United States and it provides critical baseline data from which to gauge future progress with regard to reducing medical errors. The most important result is that 18.8% of Iowans have experienced a medical error in the last five years. By comparison, Massachusetts found that 23% of residents reported medical errors in 2014.10 A national study in 2017 similarly found that 23% of Americans experienced a medical error, according to e-mail of Patricia McTiernan, Director of Program Communications, IHI/NPSF.
The impacts of a medical error on patient health are multifaceted, in that a medical error potentially compounds the complexity and severity of the original medical issue while slowing recovery and increasing emotional burdens on patients and their families.20 Our results suggest that in addition to a slowed recovery, the additional medical treatments due to a medical harm can also have a significant financial burden. These additional costs of a medical harm not only are for the patient but also become part of the financial burden to the health care provider and health care system as a whole. When estimating the economic impact, using quality-adjusted life years of those who die from medical harm, the cost has been estimated as high as nearly US $1 trillion per year.21
Although previous studies show that medical errors and adverse events happen anywhere that medical care is given, the current results demonstrate that the sheer volume of medical procedures performed in hospitals provides an important reason to focus on hospitals when addressing medical errors as they are the location of 58.5% of medical errors. Similarly, Massachusetts residents reported that 75% of medical errors happened within hospitals, whereas 18% occurred as a medical error in a doctor's office or clinic.10
Several of the medical errors reported here are related to poor communication within and between health care providers. The inability to share information effectively stems from a myriad of incompatible electronic health record systems that are not fundamentally equipped to allow for effective communication between providers. Moreover, poor training and coordination protocol make it difficult for well-meaning medical professionals to operate effectively and efficiently. The results suggest that Iowan's perceive these issues and believe that medical errors are caused mainly by poor staff communication and the belief that medical staff do not know about previous care patients received elsewhere. In addition, the long hours in a stressful environment and the requirement for medical professionals to remain current on the vast volume of medical literature published annually serve as a serious challenge adding to stress and practitioner burnout that may lead to medical errors.22 Again, Iowans clearly sense this issue in their care by reporting an “overworked medical staff” as one of the main three reasons for medical errors. Interestingly, Iowans also believe that medical staff do generally care about their work and their patients but that the health care workers are forced to work within poor systems of care that lead to mistakes.
Largely due to fears of litigation and the financial consequences of tarnished reputations, full disclosure from providers occurs infrequently. Although only 39.1% of surveyed Iowans who experienced a medical error were informed by the medical staff that an error had occurred, this finding is higher than both the Massachusetts and IHI & NPSF studies of 30% and 32%, respectively.5,10 Other national studies suggest that physicians disclose medical errors to patients only 25% to 30% of the time even when they are ethically required to do so,23 and physicians and hospitals do not disclose medical errors unless forced.24 This lack of disclosure is often assumed to be tied to US medical malpractice laws. However, research in other countries, such as New Zealand, suggests that even when the legal system does not allow patients to sue for medical harm, doctors were just as unlikely to inform patients when a medical error occurred.25
Because a lack of reporting does not seem to be due to minimizing legal repercussions, the other possibility is that medical professionals simply do not realize how important the reporting of medical errors is to the patient and the community at large. If this is the case, one solution would be to require training for physicians and staff to ethically report medical errors to their patients—in addition to other continuing education requirements.
In 2015, Iowa adopted the Communication and Optimal Resolution statute §135P, commonly referred to as the “Candor” law, that was initiated by the Iowa provider community to provide legal protection before committing to engage with harmed patients. The Candor statue protects physicians, advanced registered nurse practitioners, physician assistants, and podiatrists who opt to engage their patients in frank and confidential discussions after an adverse outcome, without risk of information shared in these discussions later being used against the provider in court.26 Recently, expansions to the Candor statute were signed into Iowa law in 2017, applying caps on noneconomic damages to US $250,000 (with some exceptions), and expanding Candor protections to include all members of the healthcare team.27 Although such reforms attempt to encourage a higher-level of communication between the provider and patient as a result of a medical error, these programs are routinely designed to serve as an added legal protection to the provider but may not necessarily benefit the patient. Because of the recency of the Candor statute implementation, the full impact of this statute is not reflected in the findings of this study. Thus, the current results serve as an effective “pre-Candor” baseline from which to compare the effects “post-Candor” to assess the statute's effectiveness in the future.
Iowans who experienced a medical error believe that reporting errors is critical to error prevention. The overwhelming reason given by Iowans who reported errors was to prevent the same error from happening to someone else. Despite an anecdotally held belief that medical errors are reported by patients primarily to receive some form of compensation for the harm, only one-quarter of those who reported said that they did so to receive compensation, which coincides with a recent national study.5 Receiving a sincere apology from the medical provider that acknowledges an error, its consequences, and admits responsibility for causing harm can decrease blame and anger and increase trust while improving relationships.28 A simple apology helps diffuse and settle the risk of medical malpractice lawsuits.29 As of 2014, 36 states have provisions regarding medical professionals making apologies or sympathetic gestures.30
Notably, many survey respondents who did not report the medical error they experienced simply thought it would not do any good. The sense that one person cannot have an impact on a large medical organization is not unique to healthcare, but the impact of this belief is likely to be worse health outcomes and increased healthcare costs in general. Many others elected to not report errors because they did not feel empowered to report on behalf of someone else or simply did not know how to report the error. These findings suggest that patients may benefit from having easy access to information that provides basic information about patient rights, including how and why to report a medical error.
The survey finds that 88.5% Iowans, whether they experienced a medical error or not, believe that the provider community should be required to tell patients whether a medical error is made during their treatment. At least three-quarters of Iowans “strongly agree” that hospitals, physicians, and nursing homes should be required to report all medical errors to a state agency. These findings provide impetus for Iowa policymakers to pursue a state mandate for healthcare providers to report medical errors to a state-based agency.
Not all errors are the same, and different errors can generate very different outcomes for a patient. However, whether a particular medical error generates a harmful outcome was not addressed in the current study for two reasons. First, we sought to replicate the Harvard questionnaire because it was used in Massachusetts to allow the Iowa results to be effectively compared with other states that have used the same questionnaire. Because the questions in the original Harvard survey do not ask about or differentiate between different types of outcomes, we are limited to the inferences that can be made with the questions as written. Second, and more importantly, we believe that all errors regardless of the outcome are important indicators of a possible system failure within a medical organization, and when they go unaddressed, may later develop again with more harmful or even fatal consequences. Outcomes from medical errors are indiscriminate results, some being innocuous, whereas others can be severely harmful to the patient. However, if a particular medical error does not result in a serious or potentially harmful event, it does not negate the fact that it was still an error. In other industries, reporting both errors and near misses has proven to be instrumental in improving safety and quality.31 The healthcare industry should not be immune from benefiting from robust reporting of medical errors, because this critical data will allow healthcare organizations and regulatory agencies to evaluate causes and revise and create processes to reduce the risk of errors in the future. This information can help medical organizations more clearly understand the root causes of what exactly happened, regardless of the outcome of the error, and identify the combination of factors that caused the error or near miss to occur. Doing so will allow organizations to determine the frequency of the problem and predict whether this could happen again. An error is an error, regardless of the outcome.
Although there is no nationwide mandatory reporting system for state governments to collect standardized “adverse medical events” resulting in death and serious harm, as of 2015, 28 states and the District of Columbia have variations of authorized adverse event (medical error) reporting systems for healthcare providers.32 However, even mandatory reporting almost certainly leads to undercounting and underreporting due to insufficient enforcement provisions included in these mandatory reporting laws. To serve as a counter balance to insufficient provider reporting, Iowa and other states may consider implementing an independent, statewide random-sampling survey process of patients who recently received care from providers. From this, states and providers may gain critical insight about the prevalence of medical errors to allow for future improvements. Medical providers are missing crucial feedback and learning opportunities when errors are not reported and discussed. Current patient satisfaction surveys seldom address medical error problems, and this approach would require a more intense focus on medical safety issues and outcomes. One possible logical survey process to use would be the existing provider-endorsed questionnaire known as the Hospital Consumer Assessment of Healthcare Providers and Systems. Although the standard Hospital Consumer Assessment of Healthcare Providers and Systems survey does not include questions relating to medical errors, states might mandate these questions to be included by its hospitals.
CONCLUSIONS
The results of this study are significant because they represent findings of one of few state-specific studies performed in the United States and can provide guidance to local healthcare leaders, policymakers, and researchers regarding initiatives to measure and improve patient safety. Iowans desire full transparency with respect to medical errors from healthcare providers both in terms of notifying the patient when an error occurs and in terms of mandating that providers report the error to a state-based agency.
Reducing medical errors first requires an understanding of the problem through the transparent reporting of medical errors by medical providers. There is no singular method to promote full transparency from the provider community. However, implementing mandatory provider reporting, enforcement provisions, and creation of a centralized repository for patients to report medical errors may all constitute part of a useful approach to understanding medical errors. In addition, Iowa and other states may benefit from developing an on-going, independent, random-sampling process to survey patients who recently received care to provide insight into the prevalence of medical errors, confirm provider reports of medical error rates, and provide systematic feedback to providers to reduce future medical errors.
ACKNOWLEDGMENTS
The authors thank Harvard School of Public Health for the use of their instrument.
Footnotes
The authors disclose no conflict of interest.
Research costs for Iowa Patient Safety Study was entirely underwritten by D.P.L., principal at Heartland Health Research Institute.
REFERENCES
- 1.Wolf ZR, Hughes RG. Error reporting and disclosure. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality (US); 2008. Apr. Chapter 35. Available at: https://www.ncbi.nlm.nih.gov/books/NBK2652/. [PubMed] [Google Scholar]
- 2.Institute of Medicine. To Err Is Human. Washington, DC: National Academy Press; 1999. [Google Scholar]
- 3.Pronovost PJ Cleeman JI Wright D, et al. . Fifteen years after To Err Is Human: a success story to learn from. BMJ Qual Saf. 2016;25:396–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Louis Harris & Associates. 1997. Public Opinion of Patient Safety Issues Research Findings. Rochester, NY: Louis Harris. [Google Scholar]
- 5.Blendon R DesRoches C Brodie M, et al. . Views of practicing physicians and the public on medical errors. N Engl J Med. 2002;347:1933–1940. [DOI] [PubMed] [Google Scholar]
- 6.NORC at the University of Chicago and IHI/NPSF Lucian Leape Institute. 2017. Americans' Experiences with Medical Errors and Views on Patient Safety. Cambridge, MA: Institute for Healthcare Improvement and NORC at the University of Chicago; 2017. [Google Scholar]
- 7.Institute of Medicine (IOM) Committee on Quality of Health Care in America: Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, DC; National Academy Press; 2000. [PubMed] [Google Scholar]
- 8.Department of Health and Human Services: Office of Inspector General (January, 2012). Hospital Incident Reporting Systems Do Not Capture Most Patient Harm. Washington, DC: Daniel R. Levinson; OEI-06-09-00091. [Google Scholar]
- 9.Krause T Bell K Pronovost P, et al. . Measurement as a performance driver: the case for a national measurement system to improve patient safety. J Patient Saf. 2017. doi: 10.1097/PTS.0000000000000315. [DOI] [PubMed] [Google Scholar]
- 10.Hibbard JH Peters E Slovic P, et al. . Can patients be part of the solution? Views on their role in preventing medical errors. Med Care Res Rev. 2005;62:601–616. [DOI] [PubMed] [Google Scholar]
- 11.Harvard School of Public Health. The Public's Views on Medical Error in Massachusetts, Commissioned by the Betsy Lehman Center for Patient Safety and Medical Error Reduction. Boston, MA: Center for Health Information and Analysis, Health Policy Commission; 2014. [Google Scholar]
- 12.Levtzion-Korach O Franel A Alcalai H, et al. . Integrating incident data from five reporting systems to assess patient safety: making sense of the elephant. Jt Comm J Qual Patient Saf. 2010;36:402–410. [DOI] [PubMed] [Google Scholar]
- 13.Basch E Artz D Dulko D, et al. . Patient online self-reporting of toxicity symptoms during chemotherapy. J Clin Oncol. 2005;23:3552–3561. [DOI] [PubMed] [Google Scholar]
- 14.Kuzel AJ Woolf SH Gilchrist VJ, et al. . Patient reports of preventable problems and harms in primary health care. Ann Fam Med. 2004;2:333–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weingart SN Gandhi TK Seger AC, et al. . Patient-reported medication symptoms in primary care. Arch Intern Med. 2005;165:234–240. [DOI] [PubMed] [Google Scholar]
- 16.Weingart SN Pagovich O Sands DZ, et al. . What can hospitalized patients tell us about adverse events? Learning from patient-reported incidents. J Gen Intern Med. 2005;20:830–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weingart SN Pagovich O Sands DZ, et al. . Patient-reported service quality on a medicine unit. International J Qual Health Care. 2006;18:95–101. [DOI] [PubMed] [Google Scholar]
- 18.Weingart SN Price J Duncombe D, et al. . Patient-reported safety and quality of care in outpatient oncology. Jt Comm J Qual Patient Saf. 2007;33:83–94. [DOI] [PubMed] [Google Scholar]
- 19.Zhu J Stuver SO Epstein AM, et al. . Can we rely on patients' reports of adverse events? Med Care. 2011;49:948–955. [DOI] [PubMed] [Google Scholar]
- 20.Stangierski A Warmuz-Stangierska I Ruchała M, et al. . Medical errors - not only patients' problem. Arch Med Sci. 2012;8:569–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Andel C Davidow SL Hollander M, et al. . The economics of health care quality and medical errors. J Health Care Finance. 2012;39:39–50. [PubMed] [Google Scholar]
- 22.Soldaini L Cohan A Yates A, et al. . 2015. Retrieving medical literature for clinical decision support. In: Hanbury A, Kazai G, Rauber A, Fuhr N. (eds) Advances in Information Retrieval. ECIR 2015. Lecture Notes in Computer Science, vol 9022 Cham, Switzerland; Springer. [Google Scholar]
- 23.Wu AW Boyle DJ Wallace G, et al. . Disclosure of adverse events in the United States and Canada: an update, and a proposed framework for improvement. J Public Health Res. 2013;2:e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gallagher TH Waterman AD Garbutt JM, et al. . US and Canadian physician's attitudes and experiences regarding disclosing errors to patients. Arch Intern Med. 2006;166:1605–1611. [DOI] [PubMed] [Google Scholar]
- 25.Gallagher TH Waterman AD Garbutt JM, et al. . US and Canadian physicians' attitudes and experiences regarding disclosing errors to patients. Arch Intern Med. 2006;166:1605–1611. [DOI] [PubMed] [Google Scholar]
- 26.Adverse Health Care Incidents - Communications - Confidentiality, Iowa Code 2016, Chapter 135P (2015 & Supp. 2017).
- 27.Ibid.
- 28.Robbennolt JK. Apologies and medical error. Clin Orthop Relat Res. 2009;467:376–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Banja JD. Does medical error disclosure violate the medical malpractice insurance cooperation clause? In: Henriksen K Battles JB Marks ES, et al., editors. Advances in patient safety: from research to implementation: Vol. 3. Implementation issues. Challenges and Lessons Learned. Rockville, MD: Agency for Healthcare Research and Quality; 2005. pp. 371–81. AHRQ Publication No. 05-0021–3. [PubMed] [Google Scholar]
- 30.National Conference of State Legislatures. Available at: http://www.ncsl.org/research/financial-services-and-commerce/medical-professional-apologies-statutes.aspx. Accessed January 21, 2014.
- 31.Barach P, Small SD. Reporting and preventing medical mishaps: lessons from non-medical near-miss reporting system. BMJ. 2000;320:759–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hanlon C Sheedy K Kniffin T, et al. . 2014 Guide to State Adverse Event Reporting Systems. Portland, ME: National Academy for State Health Policy; 2015. [Google Scholar]


