Abstract
The objective of this study was to determine the feasibility and effectiveness of translating films, and whether the use of narrative is an effective vehicle for producing changes in knowledge, attitudes, and behaviors regarding cervical cancer compared with a nonnarrative film. A randomized controlled telephone trial surveyed the effectiveness of two films our team produced among a sample of 300 monolingual Spanish-speaking women, ages 25 to 45, who were of Mexican origin. Participants were recruited using random digit dialing (RDD) procedures from 2013 to 2014 in Los Angeles County and were randomly selected to view either a narrative or nonnarrative film. Data were collected by phone at baseline, 2 weeks, and 6 months after viewing. On average, participants arrived in the USA 25 years ago. The majority reported having less than high school education and limited English proficiency. Compared with their nonnarrative counterparts, women who received the cervical cancer–related information in the narrative film showed a significantly greater increase in new knowledge (p = 0.01) and in supportive attitudes about Pap tests expense (p = 0.05). Importantly, at 6 months, although not statistically significant, women who viewed the narrative film were also more likely to have had or scheduled a Pap test (62% vs 42%). Narratives are a useful and underutilized tool to communicate information about cancer prevention. These findings have important implications for the delivery of health education among Spanish-speaking, low-literacy immigrant women, and for the reduction of cancer-related disparities.
Keywords: Cervical cancer screening, Health communication, Latinas, Spanish speaking
Introduction
In the USA, cervical cancer is the second leading cause of cancer death for women between the ages of 20 to 39 years [1]. The cervical cancer burden in Los Angeles County follows the national trend where Latina women have higher incidence rates compared with non-Hispanic whites and Asian/Pacific islander women [2, 3]. Latinos now number 57.5 million [4], and about a third report speaking Spanish at home and that they are English proficient [5]. While English proficiency appears to be on the rise, foreign-born Hispanics report much lower rates at just 35%. Although the longer an individual is in the USA, even if foreign born, the higher one would expect in terms of language proficiency in English, and acculturation. However, research [6] has shown that it is not always the case, as some groups are slower to acculturate than others [7]. Latinos with limited English proficiency are a population with greater risk for poor health outcomes and access to care [8].
Despite documented health care disparities by cultural and language barriers, there is a lack of assessment for effective health communication interventions that target Spanish-speaking populations. In recent years, there has been an increase in adapting and validating psychometric measurements and written materials for interventions but less has been written about the translation and adaption of health communication interventions [9]. The purpose of this study was to evaluate a culturally and linguistically appropriate, Spanish language narrative (storytelling) and nonnarrative film delivered to Mexican immigrant women with limited English proficiency. Specific aims were to (1) evaluate whether translating a film from English into Spanish was effective in changing knowledge, attitudes, and behavior and (2) compare the effectiveness of the narrative and nonnarrative film.
The current study builds upon existing research by this team examining the effectiveness of two existing films that were culturally tailored and originally produced in English for a Mexican-American audience [10, 11]. We used rigorous techniques to develop and translate both films into Spanish. The films contained the same cervical cancer–related facts; however, one was delivered in a narrative/story telling format and the other in a nonnarrative format. Based on previous studies with English-speaking populations [10], we hypothesize that both films will show change from pre-test to follow-up but the change will be larger among the narrative group than among the nonnarrative group.
Methods
Procedure
The Spanish language films were translated and developed by a multidisciplinary team of investigators at the University of Southern California. Two 11-min films had previously been implemented and tested in English: a fictional narrative (Tamale Lesson/Conversando entre Tamales) and a more traditional nonnarrative film (It’s Time/Es Tiempo) [11]. Both films contained the same type and amount of information, promoting the benefits of early vaccination against the human papillomavirus (HPV) and of the utilization of Pap tests. The development of the films was a multi-stage process that included formative groups (focus groups), reactions to script, reaction to rough cut, and feedback on final version of the films.
The translation into Spanish used a combination of dubbing, remixing, and/or voice over techniques to accommodate low-literacy Latinas with limited English proficiency. Showing the Spanish version films to bilingual women who also saw the English version assessed face validity of the translated films. These women felt the quality of the films was not degraded through the professional dubbing.
The narrative film centered on a Mexican-American family, the Romero family, preparing for the youngest daughter’s (Rosita’s) quinceañera or 15th birthday celebration. The story began with the preparation of tamales for the birthday celebration, where the eldest daughter of the family, Lupita, reveals to her sister, Connie, that she had an abnormal Pap test and has been diagnosed with the human papillomavirus infection (HPV). As the story unfolded, Lupita shares key facts about HPV, its relation to cervical cancer, and the importance of Pap tests in detecting cervical cancer. The older women in the film acknowledge the potential benefits of getting tested. The film concludes with Connie, Connie’s mother, and a family friend (Petra) going to the local clinic to get a Pap test.
The nonnarrative film was nonfictional, took a more traditional approach of disseminating information through the use of charts and figures to provide evidence, and doctors and patients talking about the disease, risk factors, and the importance and process of getting a Pap test. Both films were targeted towards and featured Latina women.
Participants
Participants were recruited to participate in a series of three phone interviews using a random digit dialing procedure. Inclusion criteria included (1) women must have had no pre-existing cervical cancer; (2) were between the ages of 25 and 45; (3) self-identified as fluent in Spanish; (4) self-identified as being of Mexican origin; and (5) residing in Los Angeles County. Three hundred women were randomized, a total of 187 women completed the post-test survey, and 140 women completed the surveys at three points in time, of which 109 were included in this study (see Fig. 1). For analysis, we excluded participants who were born in the USA because it has been found that foreign-born and US-born Hispanics show differences of opinion on some key issues [12]. Thus, given the sensitivity of our topic about the human papillomavirus (HPV) and of the utilization of Pap tests, our target participants were foreign-born women.
Fig. 1.
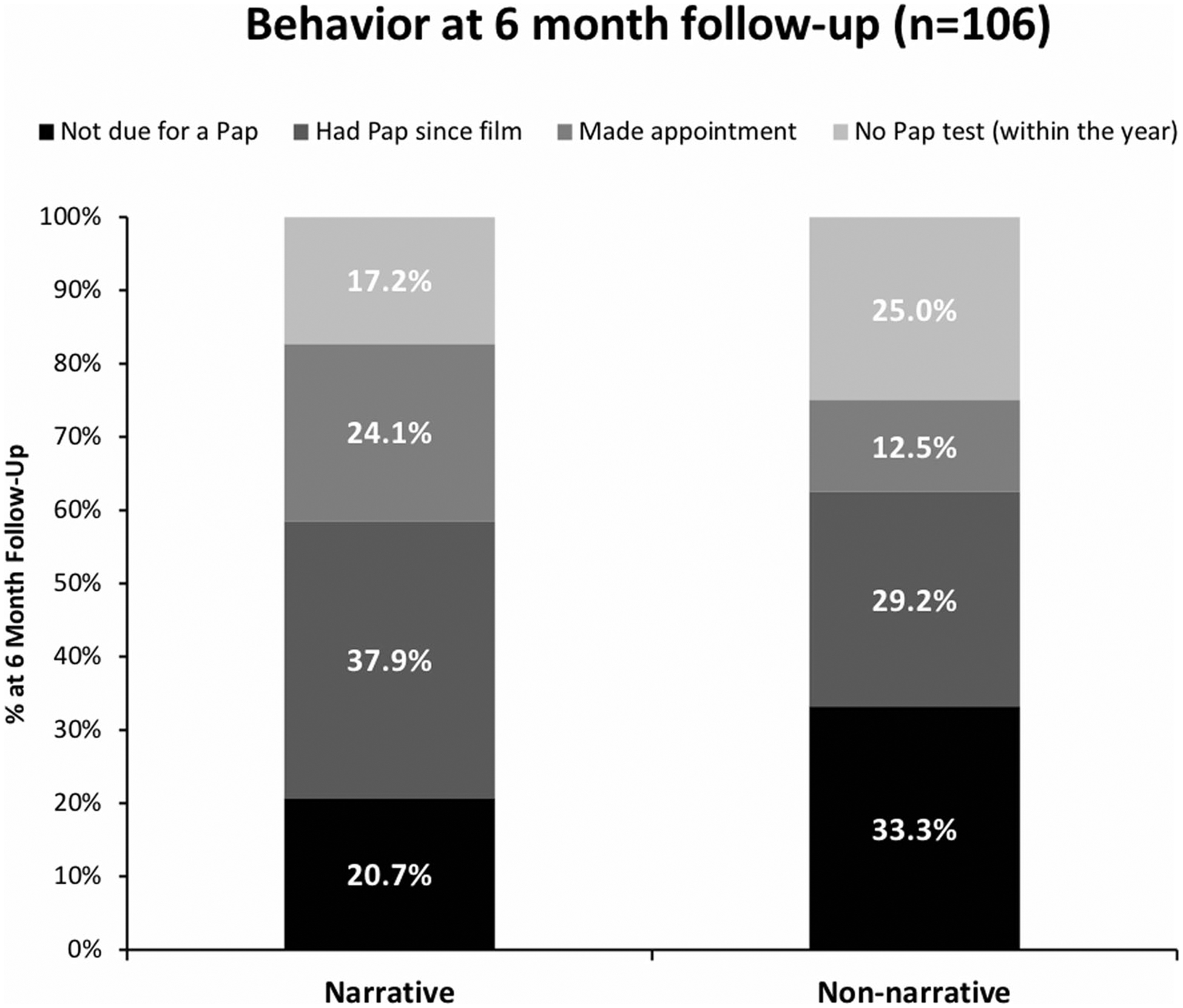
Behavior at 6 months follow-up (n = 106)
Intervention
After providing written informed consent and completing the baseline survey, participants were randomly assigned to one of two experimental conditions: half of the participants were assigned to view the narrative film (Tamale Lesson/Conversando entre Tamales), and the other half were assigned to view the nonnarrative film (It’s Time/Es Tiempo). Both films contained the same type and amount of information, about cervical cancer prevention, the HPV vaccine, and early detection via regular screenings. Participants were surveyed two more times at 2 weeks (post-test) and 6 months after (follow-up) viewing either film.
Outcomes
Knowledge
Knowledge was assessed at pre-test, post-test, and follow-up surveys with a series of eight open-ended questions. Example questions include “Does a woman need a Pap test if she is not sexually active?” and “What, if anything, can prevent females from contracting the Human Papilloma Virus?” Participants’ answers were categorized as correct or incorrect. Then, the results were summed to create separate count knowledge scores for pre-test, post-test, and follow-up.
Attitude towards Pap Test
Attitude towards Pap test was assessed using a series of 10-point Likert-type scales anchored at “1 = not at all” and “10 = extremely.” Specifically, participants were asked four questions that measured how embarrassing, physically painful, important, and expensive Pap tests were. Higher numbers indicated more supportive attitudes towards Pap tests.
Behavioral Intentions
At pre-test, participants were asked, “When did you have your most recent Pap test?” Participants who reported within the previous 6 months were categorized as not due for a Pap test. At both the post-test and follow-up, participants were asked “Since you saw the film, did you make an appointment for a Pap test?” Response options included yes, no, or do not know. Making an appointment for a Pap test is a measure of behavioral intention and has been found to be an acceptable predictor for cervical cancer screening behavior among Latinas [13]. Behavioral intention was measured in addition to behavior change as some women may have delays in making an appointment.
Behavior
At post-test and follow-up, participants were also asked “Since you saw the film, have you had a Pap test?” Participants’ responses included yes, no, or do not know.
Data Analysis
We conducted statistical analyses using SPSS version 24 (IBM, Armonk, NY) [14] with an alpha set at 0.05. Chi-square test for categorical variables was conducted to describe the demographic- and health-related outcomes including the behavioral intentions and behavior of participants. At baseline, the reported mean scores of knowledge and attitudes were different among women randomized to each group; thus, we examined if there was a change in the mean scores of cervical cancer–related knowledge and attitudes towards Pap tests at post-test and follow-up with analysis of covariance, controlling for pre-test mean scores.
Results
Characteristics of Participants
There were no statistical differences in baseline characteristics of income, marital status, number of years in the USA, health care coverage, and self-reported health status among the women who completed all three surveys and those who were lost to attrition. However, we did find some statistical differences in baseline characteristics that assessed women’s educational level (X2 = 8.71 (3), p = 0.03) and English proficiency (speaking X2 = 5.08 (1), p = 0.02; reading X2 = 6.71 (1), p = 0.01; and writing X2 = 7.20 (1), p = 0.01). Women who were less educated and had limited English-speaking abilities, and limited reading, and writing proficiency in English, were more likely to complete all three surveys. Additionally, there were no statistical differences in baseline characteristics of education, income, marital status, health care coverage, self-reported health status, and English proficiency among the women who were assigned to the narrative film rather than nonnarrative film. On average, women who were assigned to watch the narrative film reported longer length in the USA (26.6 vs 23.3; p = 0.005) compared with women who were assigned to the nonnarrative film.
Among the 109 women who completed all three surveys, the majority had less than high school education, were married or reported living with a partner, and having incomes less than 20,000 dollars. In terms of health characteristics, the majority of women reported having some health care coverage and having good health status. On average, women had arrived to the USA over 23 years ago and the vast majority reported not speaking, writing, or reading English very well or at all well (see Table 1).
Table 1.
Demographic and health-related characteristics for foreign born at baseline by experimental condition (narrative or nonnarrative film) (n = 222)
| Characteristics | Experimental condition | p value | |
|---|---|---|---|
| Narrative (n = 128) N (%) or M (SD) | Nonnarrative (n = 104) N (%) or M (SD) | ||
| Education | |||
| < High school | 58 (49.6%) | 52 (50.0%) | 0.964 |
| High school | 36 (30.8%) | 33 (31.7%) | |
| Some college degree | 23 (19.7%) | 19 (18.3%) | |
| Income, $ | |||
| < 20,000 | 42 (39.6%) | 41 (43.6%) | 0.770 |
| 20,000 to < 40,000 | 39 (36.8%) | 32 (34.0%) | |
| 40,000 to < 60,000 | 16 (15.1%) | 16 (17.0%) | |
| ≥ 60,000 | 9 (8.5%) | 5 (5.3%) | |
| Marital status | |||
| Married/living with partner | 88 (75.2%) | 86 (82.7%) | 0.313 |
| Separated/divorced/widowed | 16 (13.7%) | 8 (7.7%) | |
| Never married (single) | 13 (11.1%) | 10 (9.6%) | |
| Health care coverage | |||
| Yes | 92 (78.6%) | 71 (68.3%) | 0.080 |
| No | 25 (21.4%) | 33 (31.7%) | |
| Health status | |||
| Very poor or poor | 1 (0.9%) | 2 (1.9%) | 0.417 |
| Fair | 16 (13.9%) | 13 (12.5%) | |
| Good | 36 (31.3%) | 44 (42.3%) | |
| Very good | 24 (20.9%) | 15 (14.4%) | |
| Excellent | 38 (33.0%) | 30 (28.8%) | |
| Number of years in USA | 26.59 (9.08) | 23.25 (8.27) | 0.005 |
| English speaking proficiency | |||
| Very well/well | 36 (31.6%) | 28 (27.2%) | 0.478 |
| Not very well/not at all well | 78 (68.4%) | 75 (72.8%) | |
| English reading proficiency | |||
| Very well/Well | 41 (35.3%) | 37 (35.9%) | 0.929 |
| Not very well/Not at all well | 75 (64.7%) | 66 (64.1%) | |
| English writing proficiency | |||
| Very well/well | 37 (32.2%) | 31 (29.8%) | 0.705 |
| Not very well/not at all well | 78 (67.8%) | 73 (70.2%) | |
Bolded is significant at p<0.05
n varies based on missing responses; percentages are based on valid percent
Change in Knowledge, Attitudes, and Behavior
Both films produced an increase in cervical cancer–related knowledge at post-test and follow-up. Table 2 shows the mean score of knowledge and Pap test attitudes. According to ANCOVA with baseline knowledge entered as a covariate, compared with their nonnarrative counterparts, women who received the cervical cancer–related information in the narrative film showed significantly greater knowledge at post-test (on average of 0.66 more facts) (F(1, 107) = 6.58; p = 0.01; η2 = 0.058; reported effect sizes were partial η2). However, at follow-up, the main effect of the film was not significant (F(1, 107) = 0.04 p = 0.84).
Table 2.
Mean knowledge and Pap test attitudes condition (narrative or nonnarrative film)
| Variable | Narrative (n = 61), mean(SD) | Nonnarrative (n = 48), mean (SD) | p value |
|---|---|---|---|
| Knowledge | |||
| Pre-test | 2.92 (1.33) | 2.77 (1.22) | 0.554 |
| Post-test | 5.10 (1.45) | 4.44 (1.15) | 0.011 |
| Follow-up | 5.38 (1.27) | 5.29 (1.17) | 0.718 |
| Pap test attitudes: embarrassing | |||
| Pre-test | 4.28 (3.46) | 5.79 (3.54) | 0.027 |
| Post-test | 4.70 (3.25) | 5.42 (3.83) | 0.307 |
| Follow-up | 5.08 (3.36) | 5.71 (3.27) | 0.330 |
| Pap test attitudes: physically painful | |||
| Pre-test | 6.48 (2.96) | 7.06 (2.89) | 0.301 |
| Post-test | 6.59 (2.85) | 6.40 (3.23) | 0.739 |
| Follow-up | 7.13 (2.66) | 7.23 (2.72) | 0.850 |
| Pap test attitudes: importance | |||
| Pre-test | 9.85 (0.81) | 9.90 (0.47) | 0.743 |
| Post-test | 9.97 (0.18) | 9.98 (0.14) | 0.708 |
| Follow-up | 9.98 (0.13) | 9.94 (0.25) | 0.240 |
| Pap test attitudes: expensive | |||
| Pre-test | 8.25 (2.82) | 8.13 (2.79) | 0.847 |
| Post-test | 8.50 (2.74) | 8.02 (3.13) | 0.412 |
| Follow-up | 9.19 (1.98) | 8.74 (2.49) | 0.324 |
Bolded are significant at p<0.05
While both films led to change in attitudes towards getting a Pap test, there was only a statistically significant difference in overall attitudes towards how expensive Pap test were. With baseline attitudes entered as a covariate in ANCOVA, women who viewed the narrative film showed significantly more supportive attitudes towards “how expensive Pap test were” at follow-up (F(1, 82) = 4.12; p = 0.05; η2 = 0.048) which was not seen at post-test (F(1, 82) = 0.10; p = 0.76; η2 = 0.001). There was no significant difference in attitudes towards how embarrassing, how physically painful, and how important Pap test were by film condition. Moreover, there was no main effect of film condition with respect to the importance of Pap test as women in both films rated Pap test as extremely important at post-test (F(1, 107) = 0.15; p = 0.70; η2= 0.001; narrative women mean = 9.97 vs nonnarrative women mean = 9.98) and at follow-up (F(1, 107) = 1.81; p = 0.18; η2 = 0.017; narrative women mean = 9.98 vs nonnarrative women mean = 9.94).
At baseline, there was no statistical difference in Pap test status. The majority of women reported not having had a Pap test within the previous 6 months (narrative n = 46 (79%) and nonnarrative n = 32 (67%); p = 0.14). Of those women that had not had a Pap test, there was no statistical difference in behavioral intentions at 2 weeks based on the film condition; however, there were trends that the narrative film had a greater effect. Importantly, at 6 months, although not statistically significant, women who viewed the narrative film were more likely to have had or scheduled a Pap test (n = 36, (62%) vs n = 20 (42%); p = 0.13) (see Fig. 1).
Discussion
The goal of this study was to examine the effectiveness of the translation and adaption of health communication interventions to Spanish-speaking Mexican-American women to promote the benefits of the utilization of Pap tests. We successfully contacted and recruited 300 women into this study, of those 46.6% completed all three waves. As found in our previous study among English-speaking women [10], the Spanish language narrative film produced a greater retention rate than the nonnarrative film. We also found a statistically significant difference in education level and English proficiency among participants who completed all three surveys, which suggests that these women were engaged and perhaps had higher motivation to participate in our study than women who had proficient English skills and had higher levels of education.
Both films were successful interventions when assessed 2 weeks and 6 months after viewing. Our results supported our hypothesis that both films would show a change from pre-test to follow-up, but the change will be larger among the narrative group than among the nonnarrative group. Women in the narrative group had a significantly greater increase in knowledge related to cervical cancer. Women who viewed the narrative film were also more likely than those who viewed the nonnarrative to have decrease in attitudes towards how expensive Pap test was which might have contributed to change in their screening practices. Our study also found that women who viewed the narrative film were more likely than those who viewed the nonnarrative to have made an appointment or had a Pap at the 6-month follow-up. Although these differences were not statistically significant this is likely due to sample size. Taken together, this study suggests that a narrative format that considers cultural values and involves the community is a useful tool to present information about cervical cancer screening regarding efficacy and cost.
Interestingly, our findings also showed that viewing the nonnarrative film also led to more supportive attitudes towards how embarrassing a Pap test was which might suggest different needs for Spanish-speaking Mexican women. It may be beneficial, therefore, to include a scenario that depicts an interactive story line of a women’s medical visit to get a Pap test. Latino cultural values of confianza (i.e., trust) and respeto (i.e., respect) could be incorporated to influence women’s perception about their doctors and increase their self-efficacy about navigating the healthcare system.
Two important findings potentially relevant to future health communication interventions were identified. The most interesting of our findings were those related to the success of both interventions with a new sample of women who were monolingual Spanish speakers. This study replicated many of the results from the English-speaking audience on the effects of the narrative and nonnarrative formats. Although our findings did not reach statistical difference for main effect on the different aspects of attitudes towards Pap test, the results presented in Table 2 suggest that attitudes towards how embarrassing a Pap test is something that future interventions can focus on to potentially modify screening behaviors. Additionally, our findings strongly suggest that it is possible to translate the language of health education material (films) without the loss of efficacy when the original materials were already culturally appropriate. The fact that we can use voice over techniques on existing media rather than re-filming health communication interventions means we can reach new audiences that speak different languages at a drastically reduced cost. Furthermore, the film and study were specifically designed for Mexican-American women. Future studies should focus on evaluating if these interventions would be efficacious among other Latina subgroups living in the USA and throughout Latin America are warranted, given that the burden of cervical cancer varies by country of origin.
Our study has some limitations. The first of these limitations concerns the question assessing “getting a Pap test” which has been found to have social desirability effects, especially in Spanish language questionnaires [15]. The second limitation of this study pertains to all measures being self-reported. Future research should partner with local clinics and/or organizations to obtain clinical information to follow-up and verify screening behaviors. A third limitation would be our sample size. Finally, future studies should explore the association of an individual’s response with sociodemographic factors (such as length of time in the USA or other health practices).
Conclusion
This study contributes substantially to a better understanding of how to both facilitate and maintain behavior change. Our results suggest that a narrative format may be a useful tool for eliminating cervical cancer health disparities in highly vulnerable populations, and a preferred tool over nonnarrative formats, especially among less acculturated Spanish-speaking women. These findings have implications for the delivery of cancer information to the public, and overall health education delivery methods, especially among vulnerable, Spanish language populations, helping to save lives.
Funding
This study was supported by the National Cancer Institute (NCI), through a Transformative Research Award (TR01), awarded to the University of Southern California (RO1CA144052: (Murphy/ Baezconde-Garbanati). This project was possible also in part by support from the SC Clinical and Translation Science Institute at USC (CTSI) award number UL1TR000130 (Baezconde-Garbanati/Murphy), and the Norris Comprehensive Cancer Center (NCCC) (NCI - P30CA014089).
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
Research Involving Human Participants All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s13187-019-01521-6) contains supplementary material, which is available to authorized users.
References
- 1.Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68(1):7–30 [DOI] [PubMed] [Google Scholar]
- 2.Los Angeles County Department of Public Health OoWsH. Health indicators for women in Los Angeles County: highlighting disparities by ehtnicity and povery level. 2017
- 3.CDC. Cervical Cancer Rates by race and ethnicity. https://www.cdc.gov/cancer/cervical/statistics/race.htm. Accessed September 2017
- 4.Bureau UC. Facts for features: Hispanic heritage month 2017. 2017; https://www.census.gov/newsroom/facts-for-features/2017/hispanic-heritage.html. Accessed 5 July 2018
- 5.Flores A How the U.S. Hispanic population is changing. 2017; http://www.pewresearch.org/fact-tank/2017/09/18/how-the-u-s-hispanic-population-is-changing/. Accessed July 5, 2018
- 6.Batalova JZaJ. The limited English proficient population in the United States. 2015; https://www.migrationpolicy.org/article/limited-english-proficient-population-united-states. Accessed 10 June 2018
- 7.Jens Manuel Krogstad RSaMHL. English proficiency on the rise among Latinos. U.S. Born Driving Language Changes 2015; http://www.pewhispanic.org/2015/05/12/english-proficiency-on-the-rise-among-latinos/. Accessed 10 June 2018 [Google Scholar]
- 8.Sentell T, Braun K (2012) Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ ethnic groups in California. J Health Commun 17(Suppl 3):82–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ko LK, Reuland D, Jolles M, Clay R, Pignone M (2014) Cultural and linguistic adaptation of a multimedia colorectal cancer screening decision aid for Spanish-speaking Latinos. J Health Commun 19(2):192–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murphy ST, Frank LB, Chatterjee JS, Moran MB, Zhao N, Amezola de Herrera P, Baezconde-Garbanati LA (2015) Comparing the relative efficacy of narrative vs nonnarrative health messages in reducing health disparities using a randomized trial. Am J Public Health 105(10):2117–2123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baezconde-Garbanati LA, Chatterjee JS, Frank LB, Murphy ST, Moran MB, Werth LN, Zhao N, Amezola de Herrera P, Mayer D, Kagan J, O’Brien D (2014) Tamale lesson: a case study of a narrative health communication intervention. J Commun Healthc 7(2): 82–92 [Google Scholar]
- 12.Brown A (2015) The unique challenges of surveying U.S. In: Latinos
- 13.Roncancio AM, Ward KK, Sanchez IA, Cano MA, Byrd TL, Vernon SW, Fernandez-Esquer ME, Fernandez ME (2015) Using the theory of planned behavior to understand cervical cancer screening among Latinas. Health Educ Behav 42(5):621–626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.IBM SPSS for Windows (2018) Version 24.0 [computer program]. IBM Corp, Armonk [Google Scholar]
- 15.Marín G, Marín BV Research with Hispanic populations In: Research with Hispanic populations. Sage Publications, Inc, Thousand Oaks: ix, 130-ix, 130 [Google Scholar]


