Abstract
Objectives
In this literature review, we discuss 2 system-level, nurse-targeted patient safety practices (PSPs) that aim to reduce medication errors associated with infusion pumps, including smart pumps. One practice focuses on implementing structured process changes and redesigning workflows to improve efficiencies with pump use. The other focuses on investing in initial and ongoing staff training on the correct use, maintenance, and monitoring of infusion pumps.
Methods
Two databases were searched for “infusion pumps” and related synonyms, along with relevant terms for each PSP. Articles were excluded if outcomes were not directly relevant to the PSP addressed in this review, the article was out of scope, or study design was insufficiently described.
Results
Limited research was found on best practices for reducing errors and improving infusion pump use through workflow and process changes, as well as education and training. Four studies reported medication administration errors, procedural errors, or deviations from hospital policy as clinical outcomes of workflow or process changes. Mixed results were found examining process outcomes related to pump handling. Education on the correct use of smart pumps was found to decrease medication errors and adverse drug events, and 2 studies found an increase in nurses’ adherence to using the medication safety software library as a result of education.
Conclusions
Standardization of process and integration of technology and workflows were found as facilitators. Type and content of education provided were identified as facilitators, whereas time and energy constraints on nurse educators can be barriers to implementing large hospital-wide education programs.
Key Words: evidence review, patient safety practice, infusion pump, smart pump, workflow, process change, training, education, medication error
Infusion pumps, widely used medical devices, are used to administer fluids such as nutrients or medications to patients. In comparison to manual administration of fluids, infusion pumps provide the advantage of controlled administration—the ability to deliver fluids in small volumes or at precisely programed rates or intervals. Most infusion pumps deliver medications intravenously; however, subcutaneous, arterial, and epidural infusions are also occasionally used. Many newer infusion pumps are equipped with predetermined clinical guidelines, hospital-defined drug libraries with dosing parameters, and dose error reduction systems. These “smart pumps” are designed to address the programming errors that traditional pumps are susceptible to by notifying a user when there is a risk of an adverse drug interaction or when the pump’s parameters are set outside of specified safety limits for the medication being administered. Alerts generated by smart pumps include clinical advisories, soft stops, and hard stops. Clinical advisories provide information about medications within the administering facility’s drug library, including prompts for correct administration, which are programed into the pump by the facility or larger organization. Soft stops notify users that a selected dose is outside of the anticipated range for a specific medication. These alerts can be overridden without changing the pump’s settings. Hard stops alert users that a dose is out of the institution’s determined range and prohibit the infusion from being administered unless the pump is reprogramed.1
As infusion pump technology continues to evolve, use of smart pumps in hospitals has increased. A report by the American Society of Health-System Pharmacists found that in 2013, 72.9% of all U.S. hospitals were using smart infusion pumps, compared with just 44% in 2007.2 Along with this increase, many national organizations have identified implementing smart pumps as a key patient safety tool. The Institute for Safe Medication Practices strongly supports the use of smart pump safety features, and in 2006, the Institute of Medicine identified adoption of smart pumps as a strategy hospitals can use to help reduce the frequency and severity of medication errors.3
Despite the growing support for the use of smart pumps as a safety strategy, the literature shows varying results for the effect they have on reducing medication errors. User error, inadequate use of safety technology, incorrect programming, and equipment failures can still occur, significantly impacting patient safety. For example, one study found that despite use of smart pumps, 67% of the infusions evaluated involved one or more discrepancies.
The infusion pump, along with its failures and user errors, can have significant implications for patient safety because of its ubiquitous nature and frequent use to administer critical fluids. Infusion-associated medication errors are mistakes related to ordering, transcribing, dispensing, administering, or monitoring drugs.4 From 2005 to 2009, the U.S. Food and Drug Administration (FDA) received approximately 56,000 reports of adverse events related to the use of infusion pumps, and manufacturers conducted 87 infusion pump recalls.5 Fourteen of these recalls were categorized as class 1, in which there is a reasonable probability that use of the recalled device will cause serious adverse health consequences or death. Although many of the events reported to the FDA were related to deficiencies in device design and engineering, user errors also occurred. One study found that almost half of all infusion-associated medication errors were attributed to deviations in following procedures and documentation requirements.4
Intravenous (IV) infusions in particular pose risks to patient safety due to their complexity and the multiple steps required in their administration. Studies have found that IV infusion is associated with 54% of all adverse drug events, 56% of medication errors, and 61% of serious and life-threatening errors.6 In addition, IV medications are twice as likely to be involved in errors that cause harms when compared with medications delivered via other routes.7
In this literature review, we discuss 2 system-level patient safety practices (PSPs) that aim to reduce medication errors associated with infusion pumps, including smart pumps. One practice focuses on implementing structured process changes and redesigning workflows to improve efficiencies with pump use. The other focuses on investing in initial and ongoing staff training on the correct use, maintenance, and monitoring of infusion pumps. Both practices largely target nurses, as they are often on the front lines of medication administration and pump management; however, system processes and education can also include other clinicians, administrators, and hospital leadership.
Established workflows are often used in clinical practice to accomplish patient care goals. In the context of infusion pumps, workflow may include having a staff handoff procedure for shift changes or requiring 2 nurses to validate orders, doses, and pump programming for high-alert medications. Studies have shown that infusion pumps can contribute to inefficiencies and lead to errors. This is largely due to time consuming, indirect patient care tasks associated with infusion pumps such as searching for available pumps, priming tubing, manual pump programming, responding to false or unnecessary pump alarms, and managing tangled tubing.8 Inadequate workflows for these tasks can impede communication and cause unnecessary rework, delays, or gaps in care, all of which impact patient safety.9 Organizations must also consider how new technology, such as smart pumps, affects workflow, and is best implemented to drive toward safer use processes. Successful implementation often requires organizational commitment, a shared vision, an understanding of the risks and strengths of current processes, and a unified design that includes all systems and stakeholders.10
The literature shows that inadequate training is often associated with knowledge and rule-based mistakes when using infusion pumps.11 These medication errors can occur when staff are inexperienced, including being unfamiliar with the medication, environment, procedure, or equipment. In addition, lack of training can lead to overriding of smart pump safety features erroneously. Although smart pumps can be a beneficial tool to reduce medication errors attributed to manual programming, using the embedded drug libraries and dose error reduction systems is not mandatory. The literature shows that nurses commonly bypass the safety features because the drug library parameters are not customized for their patient population, it takes too much time to program the pumps, and there are too many alarms.12 To prevent overriding safety features and programming errors, some hospitals invest in initial and ongoing staff training on the correct use, maintenance, and monitoring of smart pumps. The FDA recommends providing training and educational activities for all employees designed to promote the safe use of infusion pumps, including drug library usage, as a risk reduction strategy for facility administrators and managers.13 Hospitals may also implement standard procedures for pump management and provide education on the use of the standardized protocols.
METHODS
This literature review was conducted as part of the Making Healthcare Safer III Report. Initial literature searches for PSPs in the infusion pump harm area were conducted, focusing on systematic reviews and guidelines. Results of these searches were reviewed by harm-area task leads to identify PSPs, iterate on searches as needed, and refine lists of potential PSPs. A project technical expert panel and advisory group were engaged via a survey to prioritize PSPs for inclusion in the Making Healthcare Safer III Report. These survey results, along with refined recommendations for PSP inclusion, were submitted to the Agency for Healthcare Research and Quality for review. After several rounds of review with the Agency for Healthcare Research and Quality, 2 infusion pumps’ PSPs were selected: (1) structured process change and workflow redesign and (2) staff education and training.
Two databases (CINAHL and PubMed/MEDLINE) were searched for “infusion pumps,” “smart pumps,” and related synonyms, as well as “workflow,” “workflow redesign,” “process change,” “product recalls and withdrawals,” and other similar terms for structured process change and workflow redesign and “in-service,” “staff education,” and “staff training,” for staff education and training. Articles included were published in the past 10 years from 2008 to 2018.
The initial search for structured process change and workflow redesign yielded 168 results. Once duplicates were removed and additional relevant articles from select other sources were added, a total of 163 articles were screened for inclusion, and full-text articles were retrieved. Of those, 9 were selected for inclusion in this review. Articles were excluded if the outcomes were not directly relevant to the PSP addressed in this review. See Figure 1 for the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram.
FIGURE 1.
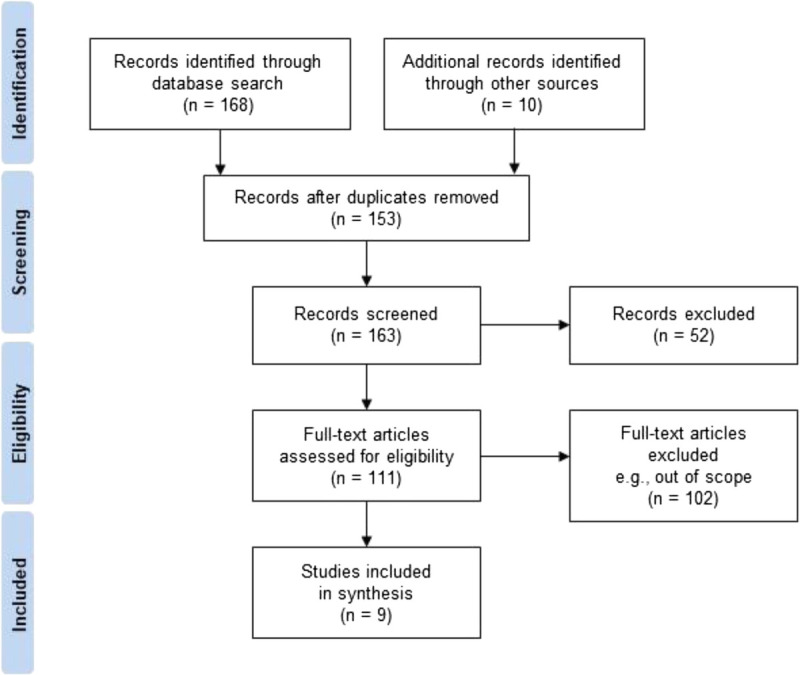
The PRISMA flow diagram for literature review of structured process change and workflow redesign as a PSP for infusion pump use. Adapted from Moher et al.14
The initial search for staff education and training yielded 104 results. Once duplicates were removed and additional relevant articles from select other sources were added, a total of 107 articles were screened for inclusion and full-text articles were retrieved. Of those, 12 were selected for inclusion in this review. Articles were excluded if the outcomes were not directly relevant to the PSP addressed in this review, the article was out of scope, or study design was insufficiently described. See Figure 2 for PRISMA diagram.
FIGURE 2.
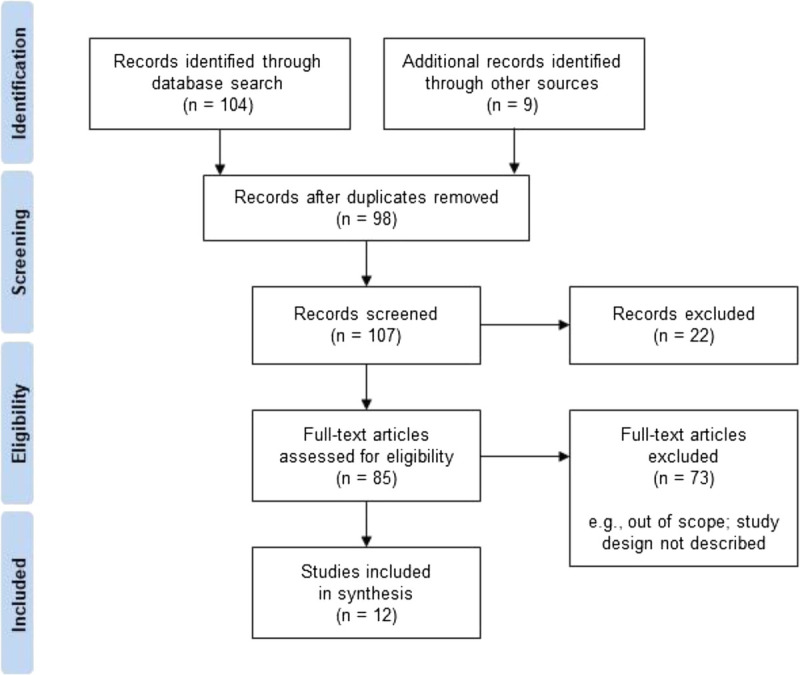
The PRISMA flow diagram for literature review of staff education and training as a PSP for infusion pump use. Adapted from Moher et al.14
RESULTS
Structured Process Change and Workflow Redesign
Of the 9 studies included in this review, 4 were observational studies, 2 were case studies, 1 was semistructured interviews, 1 was a perspective point prevalence study, and 1 was an online survey. Most studies took place in a hospital setting, and 4 took place outside of the United States. The included studies primarily examined medication errors and deviations from hospital policy as outcomes of process changes. However, because nearly half of the studies were observational, it is difficult to draw conclusions about the impact of implemented process changes.
Four of the 9 studies reported clinical outcomes, including medication administration errors, procedural errors, or deviations from hospital policy as outcomes of workflow or process changes. Deviations from hospital policy may indicate that the established processes do not align with the natural workflow of the clinic and that a workflow change is needed to better align current practice with new infusion pump technology.
Russell et al15 observed a pediatric intensive care unit before and after workflow changes as a result of expansion and implementation of a bidirectional interface between computerized physician order entry (CPOE) and the pharmacy system. The researchers compared the discrepancies between medication orders and infusion pump settings and found that the overall discrepancy rate for medications did not significantly change but the type of discrepancy did. For example, they reported that the proportion of unauthorized medications decreased from 60% to 4%; however, the rate of omitted medications and the errors associated with dosage significantly increased.15 In addition, Wiseman et al16 conducted a pre/post observational study in Australia and found that as a result of implementing a requirement for clinical pharmacist annotation on medication charts, medication administration errors dropped from 16.6% to 8.1%. Subsequent adoption of smart pump technology led the error rate to further decrease to 3.9%.16
Two observational studies did not measure the impact of a process change or workflow redesign on errors but did report types and frequency of errors related to an existing medication administration process. Schnock et al17 measured policy violations to assess IV medication administration process and found that the most frequent types of infusion errors were IV labeling (60%) and tubing change policies (35%). Similarly, Lyons et al18 observed 16 National Health Services trusts and found that 47.9% of all infusions had at least one procedural or documentation error of which noncompliance with hospital labeling requirements was the most common.
Two studies also looked at process outcomes related to pump handling. Degraff19 reported that in response to a shortage of IV pumps and staff members hoarding pumps, a hospital implemented a new procedure for cleaning and restocking pumps. This process change resulted in decreasing the steps for pump handling from 26 to 8.19 The results of process change were more mixed in a study by Chaturvedi et al,20 in which a hospital integrated its electronic health records (EHRs), CPOE, smart pumps, and barcode-assisted medication administration (BCMA) and engaged in multiple efforts to standardize workflows. The integrated system significantly reduced the amount of time required by nurses to program medications; however, nurses reported that their overall workload did not decrease and that there was an increase in the number of computer steps required to administer medications.20
Biltoft and Finneman7 measured cost savings of integrating smart pumps with EHR integration after determining the study hospital was losing revenue because of lack of sufficient documentation to support the billed charges or missing documentation, specifically stop times, in the medication administration record for outpatient infusions. The researchers found that implementation of the integrated smart pump-EHR provided accurate start and stop times, which reduced both mean lost charges for infusions from 11.9% to 7.4% and lost revenue from U.S. $980,000 to $610,000.7
Staff Education and Training
Of the 12 studies included in this review, 5 were performance or quality improvement initiatives. Other study designs included a longitudinal study, observational study, snapshot audit, and a randomized control trial. Ten of the 12 studies took place in a hospital setting, 2 of which were pediatric hospitals. Two studies took place in a simulation laboratory used for training. Three of the studies took place outside the United States. To evaluate the impact of implementing staff education and training on the correct use, maintenance, and monitoring of infusion pumps, the studies measured clinical outcomes as well as process outcomes related to compliance and use of safety features.
Of the 12 studies, 4 reported clinical outcomes for the impact of investing in education on the correct use, maintenance, and monitoring of smart pumps. Measured clinical outcomes included the number of medication errors, severe harms averted, and adverse drug events.
A study by Ferguson et al21 examined implementation of mandatory training for 4 months on the proper usage of patient-controlled analgesia pumps for all registered nurses (RNs) who use the pumps. The study found that the number of pumps errors reported for 3 months significantly decreased from 8 before the intervention to 1 after the intervention, addressing the primary cause of medication errors in the 22-unit hospital.21 van der Sluijs et al22 used a lean approach based on feedback and training to implement a fixed, dedicated moment of time to double check medications and a standard operating procedure for changing syringe pumps. The implementation was communicated to clinical staff through lessons and instructions, and the authors found that for 18 months, the overall percentage of medication errors (the percentage of syringes used with a medication error) dropped from 17.7% to 2.3%.22 In addition, Giuliano6 measured the impact of user training in a simulation laboratory on the frequency of programming use error among 3 models of IV smart pumps and found that use errors decreased from 30% to 7%, 17% to 3%, and 8% to 1%. Giuliano6 also found that programming time was significantly shorter after user training.
One study measured different clinical outcomes of proper infusion pump usage: the number of severe harms averted and adverse drug events. Orto et al23 sought to increase compliance with use of the smart pump specifications by assigning nurse champions to conduct monthly educational sessions with RN staff both individually and in groups to ensure that they were using the smart pumps and their drug library parameters. The authors found that the aggregate number of severe harms averted (defined as high risk drugs being programed by the nurse 2.5 times or greater than recommended) per 1000 infusion starts for 6 months decreased from 0.68 preintervention to 0.44 postintervention, indicating there were fewer episodes of severe infusion harms. In addition, the number of adverse drug events more severe than level 2—defined as events that reach the patient and require intervention and monitoring—decreased from 4 to 1 from preimplementation to postintervention.23
Studies examining the impact of implementing education and training on proper usage of infusion pumps measure compliance with pump technology protocols and adherence to using safety software. In a study by Gavriloff,24 researchers implemented staff education focusing on the correct use of the safety software and the benefits of preventing medication errors as part of a multicomponent intervention. The goal of the education program was to improve nurses’ adherence to using the medication safety software drug library created by the organization. Just 1 month after it was implemented, the adherence rate had increased from 25% at baseline to 68%. The adherence rate further increased to 85% after the chief nursing office sent a follow-up communication encouraging nurses to use the medication safety software.24 In addition, Orto et al23 measured compliance with use of the drug library in smart pumps in a hospital where not using the drug library constituted noncompliance with hospital policy. They found that after implementation of a nurse-led smart pump champions program, compliance among RNs significantly increased from 85% to 92%. These gains were sustained after intervention with a compliance of 92.9% and 93.3% at 3 and 6 months, respectively.23
One study examined the impact of an education intervention on the use of smart pump safety features. In a preintervention survey, Herring et al25 found that 88.6% of nurses who responded reported agreeing or strongly agreeing that training and education were adequate and 82.8% agreed or strongly agreed that they knew how to use the drug library. However, 44% of the open response comments requested additional training on the safety features. After implementing an education program that included a mandatory active learning practical skills laboratory and an optional education presentation that reviewed evidence of improved patient safety when smart pump safety features are fully used, the authors found that use of the pump mode with all safety features enabled increased from 5.5% to 30.5%.25
Of the 12 studies, only one study measured cost outcomes; Orto et al23 calculated potential cost avoidance, defined as costs that would have been incurred if the severe harms had not been averted. The study found the costs avoided because severe harms were averted came to U.S. $367,500 at the end of the intervention period compared with U.S. $612,500 6 months before the intervention. The lower cost is associated with lower numbers for severe harms averted due to the use of smart pumps.23
DISCUSSION
Use of infusion pumps, and increasingly smart pumps, has become standard practice in hospitals to administer critical fluids to patients. However, there is still limited research on best practices for reducing errors and improving infusion pump use through workflow and process changes as well as education and training. This limitation may be due to difficultly conducting randomized studies for process changes or education interventions. In addition, the studies included in this review analyzed interventions specific to the needs of the hospital or infusion pump system, so these may not be generalizable. This section reviews some of the common facilitators and barriers related to implementing PSPs to improve infusion pump use.
Facilitators
Standardization and streamlining of processes and workflows were identified as main facilitators of optimal infusion pump use across multiple studies. For example, Degraff19 found that a hospital was able to significantly improve utilization of IV infusion pumps by streamlining its workflow for cleaning and restocking pumps. Biltoft and Finneman7 streamlined nursing workflows by reconfiguring rooms so that infusion pumps and EHR computers could be accessed at the same time, which led to more accurate infusion documentation. In addition, Schnock et al17 note that by reviewing existing policies, the study team recognized the benefits of using standardized tubing labels to indicate when a nurse should change tubing. Finally, Chaturvedi et al20 found that hospital leaders viewed standardization of nursing workflow as extremely beneficial because it was perceived to reduce the frequency of nursing workarounds that could cause patient harm.
The included studies also highlighted the importance of integrating technology and workflows. Pinkney et al26 noted that implementation of smart pumps should be viewed as part of a larger safety initiative rather than just a technology upgrade and that to be successful, implementation should focus on design of workflows. For example, they found that implementing design-oriented solutions that constrain users to follow the preferred workflow, such as defaulting users into using the drug library, helps ensure users use the safety features.26 Similarly, Chaturvedi et al20 concluded that implementation of an IV clinical integration system is not only a technology intervention but requires workflow changes to be successful.
In addition, engaging multiple members of the care team in workflow redesign is an important facilitator. For example, Wiseman et al16 found that clinical pharmacists play a key role in reducing error rates and should be consulted when configuring workflows. Russell et al15 found that after the pediatric intensive care unit was relocated and expanded, pharmacist and dietician presence on rounds increased, resulting in greater collaboration between them and those responsible for ordering medications. This collaboration helped reduce the number of reorders.15
The type and content of education provided were identified as important facilitators to successful implementation. For example, Herring et al25 found that education from the device manufacturer alone may be insufficient and that implementing a hands-on training targeting identified obstacles was essential to increasing use of safety features. Similarly, Nemeth et al27 found that to be most successful, the training program should include opportunities for participants to apply learning through discussing case examples. They also found that training should provide information about the most relevant smart pump’s functions and the potential challenges nurses may encounter to using them. Virtual training systems have also been shown to facilitate learning, although the results are mixed.27 In a study by Luctkar-Flude et al,28 participants who completed an online virtual IV pump learning module reported that the module enhanced their knowledge of programming; however, most students did not feel it increased their ability to program certain types of infusions. Quattromani et al29 compared use of a traditional training method with a faculty member to use of an interactive smart pump training app and found no significant difference in outcomes related to medical knowledge, performance, or learner confidence.
In addition to the type of training, the choice of trainer can be a facilitator. For example, Orto el al23 implemented a nurse champion-led group to improve smart pump compliance because of the success their hospital had in the past with this type of intervention. Finally, Gavriloff24 found that training that focuses on “why” smart pumps are used instead of just “how” to use smart pumps is important to increase adherence. By understanding the safety software, nurses are able to provide ongoing evaluation on needed revisions and refinements.24
Barriers
Lyons et al18 noted that in some cases, procedural deviations are not representative of inadequate care practices but rather demonstrate a poor fit between hospital policy and everyday practice. If workflows do not align with new technology, or policies are implemented that are not compatible with current workflows, then errors or workarounds can occur that impact patient safety. For example, Lyons et al18 found that staff reported deliberate deviations that would benefit patients but conflicted with official rules and formal procedures, such as giving patients fluids that had not yet been prescribed because a doctor was unavailable.18 Schnock et al17 found that information such as infusion start time that was necessary to document on paper labels was no longer needed after implementation of CPOE, eMAR, and BCMA, because it was automatically entered into the system. This example illustrates that when new technology is implemented, processes such as documentation workflows must be reevaluated for relevance.17 Furthermore, Russell et al15 noted that before implementation of a bidirectional interface between CPOE and the pharmacy system, if a provider requested a new urgent medication, the pharmacist could deliver the medication but would be unable to reconcile the order; thus, it appeared as an unauthorized medication. In this case, implementing the new system rectified the misalignment between technology and the established workflow by allowing pharmacists to immediately reconcile verbal orders from physicians.15
Constrained hospital resources were identified as a barrier across both PSPs. Lacovides et al30 noted that when implementing infusion pump technology, organizations need to ensure that adequate infrastructure and resources are available and that the affected staff believe that the change is worth the time and money required. Furthermore, Ferguson et al21 note that establishing hospital-wide education programs can be a significant undertaking for staff development departments and that the time and energy constraints on nurse educators should be carefully considered and planned. Carayon et al31 highlight the importance of planning by noting that a lack of attention devoted to the implementation planning process resulted in nurses reporting more negative perceptions of usefulness of information and clarity of training materials 6 weeks and 1 year after implementation. In addition, limited knowledge transfer was identified as a barrier to staff training. For example, Lee32 found that when nurses move to different wards, they are often exposed to new devices on which they have not been trained. In addition, Ferguson et al21 note that after nurses are trained, they may not retain competency on use of a particular type of smart pump if they commonly use multiple types of pumps or if they infrequently use any pumps.
Finally, staff buy-in and resistance to culture change were also identified as potential barriers. Chaturvedi et al20 reported challenges gaining buy-in from nurses to adopt workflow changes and noted that frontline staff often expressed concerns regarding the patient safety implications of workflow changes. Subramanyam et al33 found that despite educating nurses on the use of standardize pump programming, the nurses were resistant to a culture change from the old processes to a new 2-person verification process. Orto et al23 noted that they implemented a nurse-led program focusing on promoting compliance, partnering with pharmacists, and supporting manual audits to help create a culture of safety.
CONCLUSIONS
There is strong evidence describing the frequency and type of medication and procedural errors associated with infusion pump use; however, there is limited research on workflow and process changes that can be implemented to address those errors. There is also limited evidence on best practices for education and training on the proper usage of smart pumps. More research is needed to understand why nurses commonly bypass smart pump safety technology and best practices for reducing medication errors.
Footnotes
The authors disclose no conflict of interest.
This work was funded by the Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services (Contract HHSP233201500013I; HHSP23337002T).
REFERENCES
- 1.Institute for Safe Medication Practices Proceedings from the ISMP Summit on the Use of Smart Infusion Pumps: Guidelines for Safe Implementation and Use. Philadelphia, PA: Institute for Safe Medication Practices; 2009. [Google Scholar]
- 2.Fox BI, Pedersen CA, Gumpper KF. ASHP national survey on informatics: assessment of the adoption and use of pharmacy informatics in US hospitals-2013 Am J Health Syst Pharm. 2015;72:636–655. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine; Aspden P Wolcott J Bootman JL, et al., eds. In: Preventing Medication Errors. Washington, DC: The National Academies Press; 2007:480. [Google Scholar]
- 4.Wolf ZR. Strategies to reduce patient harm from infusion-associated medication errors: a scoping review. J Infus Nurs. 2018;36:58–65. [DOI] [PubMed] [Google Scholar]
- 5.U.S. Food & Drug Administration Infusion Pumps. 2018. Available at: https://www.fda.gov/medical-devices/general-hospital-devices-and-supplies/infusion-pumps. Accessed March 10, 2020.
- 6.Giuliano KK. IV smart pumps: the impact of a simplified user interface on clinical use. Biomed Instrum Technol. 2015;suppl:13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Biltoft J, Finneman L. Clinical and financial effects of smart pump-electronic medical record interoperability at a hospital in a regional health system. Am J Health Syst Pharm. 2018;75:1064–1068. [DOI] [PubMed] [Google Scholar]
- 8.Weinger MB, Kline A. Reflections on the current state of infusion therapy. Biomed Instrum Technol. 2016;50:253–262. [DOI] [PubMed] [Google Scholar]
- 9.Cain C, Haque S. Organizational workflow and its impact on work quality. In: Hughes R, ed. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality; 2018. [PubMed] [Google Scholar]
- 10.Troiano D Morrison J Federico F, et al. Safely automating the medication use process. Not as easy as it looks. J Healthc Inf Manag. 2009;23:17–23. [PubMed] [Google Scholar]
- 11.Keers RN Williams SD Cooke J, et al. Causes of medication administration errors in hospitals: a systematic review of quantitative and qualitative evidence. Drug Saf. 2013;36:1045–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCartney P. Evidence for practice with smart infusion pumps. MCN Am J Matern Child Nurs. 2014;39:270. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Food & Drug Administration Infusion Pump Risk Reduction Strategies for Facility Administrators and Managers. 2018. Available at: https://www.fda.gov/medical-devices/infusion-pumps/infusion-pump-risk-reduction-strategies-facility-administrators-and-managers. Accessed March 10, 2020.
- 14.Moher D Liberati A Tetzlaff J, et al. The PRISMA Group . Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Russell RA Triscari D Murkowski K, et al. Impact of computerized order entry to pharmacy interface on order-infusion pump discrepancies. J Drug Deliv. 2015;2015:686598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wiseman ML Poole S Ahlin A, et al. Reducing intravenous infusion errors: an observational study of 16 866 patients over five years. J Pharm Pract Res. 2018;48:49–55. [Google Scholar]
- 17.Schnock KO Dykes PC Albert J, et al. The frequency of intravenous medication administration errors related to smart infusion pumps: a multihospital observational study. BMJ Qual Saf. 2017;26:131–140. [DOI] [PubMed] [Google Scholar]
- 18.Lyons I Furniss D Blandford A, et al. Errors and discrepancies in the administration of intravenous infusions: a mixed methods multihospital observational study. BMJ Qual Saf. 2018;27:892–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Degraff B. As medical devices proliferate, asset management is key. Biomed Instrum Technol. 2013;47:123–127. [DOI] [PubMed] [Google Scholar]
- 20.Chaturvedi RR Etchegaray JM Raaen L, et al. Technology isn’t the half of it: integrating electronic health records and infusion pumps in a large hospital. Jt Comm J Qual Patient Saf. 2019;45:649–661. [DOI] [PubMed] [Google Scholar]
- 21.Ferguson R, Williams ML, Beard B. Combining quality improvement and staff development efforts to decrease patient-controlled analgesia pump errors. J Nurses Staff Dev. 2010;26:E1–E4. [DOI] [PubMed] [Google Scholar]
- 22.van der Sluijs AF van Slobbe-Bijlsma ER Goossens A, et al. Reducing errors in the administration of medication with infusion pumps in the intensive care department: a lean approach. SAGE Open Med. 2019;7:2050312118822629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Orto V Hendrix CC Griffith B, et al. Implementation of a smart pump champions program to decrease potential patient harm. J Nurs Care Qual. 2015;30:138–143. [DOI] [PubMed] [Google Scholar]
- 24.Gavriloff C. A performance improvement plan to increase nurse adherence to use of medication safety software. J Pediatr Nurs. 2012;27:375–382. [DOI] [PubMed] [Google Scholar]
- 25.Herring H Ripley TL Farmer KC, et al. An intervention to increase safety feature use on smart pumps: a quality improvement initiative. J Pharm Technol. 2012;28:119–123. [Google Scholar]
- 26.Pinkney S Trbovich P Fan M, et al. Do smart pumps actually reduce medication errors? Biomed Instrum Technol. 2010;44(s1):64–69. [Google Scholar]
- 27.Nemeth CP Brown J Crandall B, et al. The mixed blessings of smart infusion devices and health care IT. Mil Med. 2014;179(suppl 8):4–10. [DOI] [PubMed] [Google Scholar]
- 28.Luctkar-Flude M, Pulling C, Larocque M. Ending infusion confusion: evaluating a virtual intravenous pump educational module. Clin Simul Nurs. 2012;8:e39–e48. [Google Scholar]
- 29.Quattromani E Hassler M Rogers N, et al. Smart pump app for infusion pump training. Clin Simul Nurs. 2018;17:28–37. [Google Scholar]
- 30.Iacovides I Blandford A Cox A, et al. Infusion device standardisation and dose error reduction software. Br J Nurs. 2014;23:S16, S18, S20 passim. [DOI] [PubMed] [Google Scholar]
- 31.Carayon P, Hundt AS, Wetterneck TB. Nurses’ acceptance of smart IV pump technology. Int J Med Inform. 2010;79:401–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee P. A team approach to identify and manage risk in infusion therapy. Br J Nurs. 2010;19:S12–S18. [Google Scholar]
- 33.Subramanyam R Mahmoud M Buck D, et al. Infusion medication error reduction by two-person verification: a quality improvement initiative. Pediatrics. 2016;138 pii: e20154413. [DOI] [PubMed] [Google Scholar]


