Abstract
Introduction
Efforts to improve teamwork in health care have received considerable attention. The current systematic review was conducted to identify recent studies that implemented practices to improve teamwork and were associated with positive improvements on the job.
Methods
Electronic searches of 2 databases (i.e., CINAHL and MEDLINE) were conducted to identify relevant articles published between 2008 and 2018.
Results
Twenty articles were selected for inclusion in this review. The studies most often used quasiexperimental designs and interventions were applied in a variety of hospital settings including labor and delivery, operating rooms, and emergency departments. Across studies, measures assessing teamwork skills on the job were most often collected and showed sustained improvements up to 12 months. Moreover, evidence of improved clinical processes (e.g., compliance with guidelines and efficiency) and increased patient safety (e.g., reduction in adverse events) was found in both studies of team training interventions, as well as in those that introduced performance support tools (e.g., checklist).
Conclusions
The results of the current review are consistent with previous research and add to the evidence base on the practices to improve teamwork within hospital settings. Although efforts to improve teamwork have spread to other health care settings such as office-based care, published studies are lagging behind.
Key Words: teamwork, team training, performance support tools, quality improvement, patient safety
Failures in communication and teamwork have been identified as contributing factors in approximately 68% of adverse events.1 As such, considerable effort has been made to improve teamwork within health care settings through the use of team training programs and performance support tools. According to Weaver et al,2 “team-training is defined as a constellation of content (i.e., specific knowledge, skills, and attitudes that underlie targeted teamwork competencies), tools (i.e., team task analysis, performance measures) and delivery methods (i.e., information, demonstration and practice-based learning methods) that together form an instruction strategy” (p. 360). Some of the earliest health care team training programs were based on crew resource management (CRM), an established and validated strategy within the aviation community. Subsequently, the Veteran’s Health Administration introduced its own team training program called medical team training (MTT). Similarly, the Agency for Healthcare Quality and Research partnered with the Department of Defense to develop a team training program specifically designed for health care providers called Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS). Studies of health care team training have demonstrated positive improvements in reactions, learning, transfer, and results using Kirkpatrick’s3,4 multilevel evaluation framework.5–8 These programs often introduce performance support tools (e.g., checklists) to increase the likelihood that knowledge, skills, and attitudes (KSAs) developed in training are transferred on to the job, reinforced, and integrated into daily practice. However, recent efforts to summarize the impact of teamwork interventions in health care have limited their focus to the delivery of team training and have excluded studies of the support tools implemented to enhance teamwork after training.2,8
The purpose of this review is to report data on the current practices to improve teamwork. In so doing, we attempt to synthesize studies on the effectiveness of team training, as well as on the implementation of performance support tools to foster teamwork on-the-job. Furthermore, because the primary goal of any teamwork intervention is to improve performance in the work environment, the current review focuses specifically on presenting data associated with (1) the transfer of/sustained improvement in teamwork KSAs onto the job; (2) sustained improvements in clinical processes in the work environment; and (3) improved patient outcomes.
METHODS
Electronic searches of CINAHL and MEDLINE databases were conducted to identify studies published between 2008 and 2018 that implemented practices to improve teamwork. Search terms included “teamwork,” “communication,” “team performance,” “team training,” and related synonyms, as well as terms like “training intervention” and “quality improvement.” Based on previous research, specific team training programs such as “TeamSTEPPS,” “VA Medical Team Training,” and “Crew Resource Management,” as well as specific tools such as “Checklist” were also searched.8 Searches also included the term “healthcare,” with no attempt to include or exclude any particular health care setting (e.g., primary care and long-term care).
RESULTS
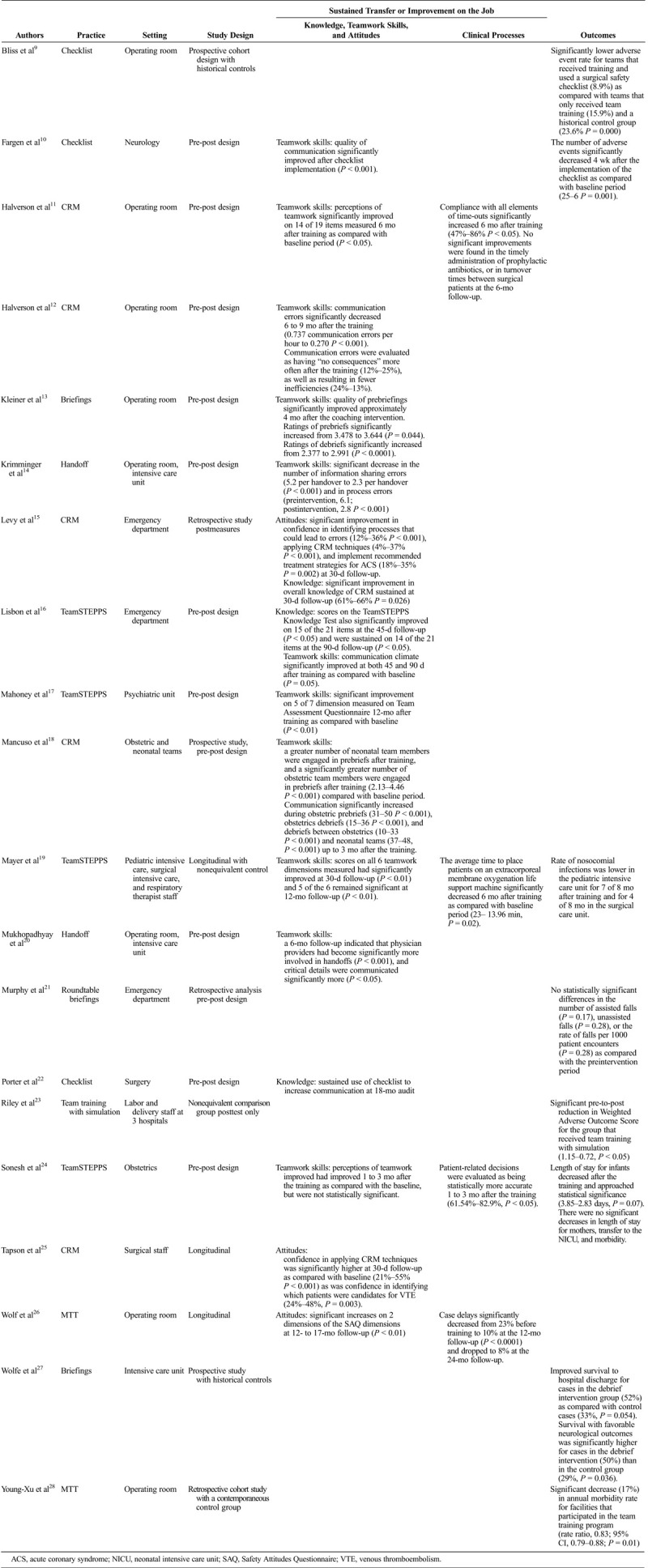
Of the 1760 articles identified, 1231 abstracts were screened by the first author for inclusion and 126 full-text articles were retrieved. Of those, 20 were selected for inclusion in this review. Articles were excluded if the study was descriptive/qualitative in nature, primary goal was not to improve teamwork, study did not evaluate a practice/method to enhance teamwork, study design was insufficiently described, study was conducted with medical or nursing students, or the study was conducted outside the United States. Descriptions of the studies included are outlined in Table 1. Most studies incorporated a quasiexperimental design with premeasure and postmeasure (75%), with 5 studies using a control or comparison group.
TABLE 1.
Study Characteristics and Research Findings
Team Training Programs
Team training programs generally follow a workshop format that includes a didactic lecture, demonstration of both positive and negative examples of teamwork, hands-on practice using teamwork skills (e.g., in role play or simulation exercises), and feedback regarding the effectiveness of teamwork skills demonstrated by participants.
Transfer of KSAs on the Job
Consistent with Kirkpatrick’s transfer level criteria, 10 studies in the review provide evidence of improved team KSAs on the job a minimum of 30 days after team training initiatives, 4 demonstrate improvement on clinical processes, and 3 support an increase in patient safety.
Attitudes
Three studies provided support for sustained improvements on attitudinal measures. Two of the 3 demonstrated that trainees were significantly more confident in applying the CRM techniques learned during training and implement recommended treatment strategies 30 days after team training efforts.15,25 One study found that safety attitudes had improved at a 12- to 17-month follow-up as compared with the baseline period, with significant improvement noted on 2 of the dimensions assessed (P < 0.01).26
Knowledge
Two studies measured sustained changes in knowledge associated with team training. Levy et al15 reported that overall knowledge of CRM had significantly increased at 30-day follow-up (61%–66%, P = 0.026), whereas Lisbon et al16 documented longer maintenance of knowledge, as significant improvements were noted on 14 of 21 TeamSTEPPS Knowledge Test items 90 days after training (P < 0.05).
Although a limited number of studies documented longer-term effects on participant’s attitudes after team training efforts and successful retention (and application) of knowledge on the job, these data add to the existing evidence base from earlier studies.
Skills and Processes
Most studies (i.e., 7/10) in the review assessed whether team training was associated with the transfer of important teamwork skills into the work environment. Three team training studies focused on enhancing communication on the job. For example, one study16 of CRM reported that open communication (i.e., speaking up, discussing errors) was significantly supported up to 90 days after training in comparison to the baseline period (P < 0.05). Another study18 observed significant improvements in communication during prebriefs and debriefs up to 3 months after team training (P < 0.0001). The third reported communication errors in the operating room had significantly decreased 6 to 9 months after the delivery of team training (P < 0.001) and were more frequently evaluated as having “no consequences,” as well as resulting in fewer inefficiencies.12
Four studies assessed whether team training led to improvements on multiple teamwork behaviors on the job. Mayer et al19 reported that perceptions of teamwork significantly improved on the 6 dimensions measured 30 days after the training (P < 0.01) and remained significant on 5 of the 6 dimensions at a 12-month follow-up (P < 0.01). Halverson et al11 also reported that significant improvements on 14 of 19 teamwork dimensions were sustained at 6 months (P < 0.05), and significant improvements on the 5 of 7 teamwork dimensions were sustained in a study conducted in a psychiatric unit by Mahoney et al.17 Only one study reported that perceptions of teamwork improved on the job after team training, but failed to find significant improvements over the baseline period.24
In addition to enhanced teamwork behaviors, 4 studies in the review found that team training had a positive impact on clinical processes relevant to their respective settings. For example, Sonesh et al24 found that patient-related decisions were significantly more accurate 1 to 3 months after TeamSTEPPS training (61.54%–82.9%, P < 0.05), whereas TeamSTEPPS training was associated with a significant decrease in the average time to place patients on an extracorporeal membrane oxygenation life support machine 6 months after training in another study.19 Another study reported that staff compliance with all elements of time-outs had significantly improved 6 months after CRM training (47%–86%, P < 0.05).11 Finally, significant reductions in surgical case delays were sustained 12 months after MTT training (P < 0.0001).26
Patient Outcomes
Three studies of team training initiatives demonstrated improved patient outcomes, which align with the results-level criteria in Kirkpatrick’s evaluation framework. For instance, TeamSTEPPS training delivered to all pediatric intensive care unit, surgical intensive care unit, and respiratory therapist staff was associated with a reduction in the rate of nosocomial infections in the pediatric intensive care unit for 7 of 8 postintervention months and for 4 of 8 postintervention months in the surgical care unit.19 In a study of obstetric clinicians, TeamSTEPPS training was associated with decreased length of stay for infants (from 3.85 to 2.83 days, P = 0.07) over the course of the study.24 Finally, a study of the Veterans Affairs’ MTT program reported a significant decrease (17%) in the observed annual morbidity rate for the facilities that had participated in MTT (rate ratio, 0.83; 95% confidence interval [CI], 0.79–0.88; P = 0.01), whereas the facilities that had not participated in MTT observed a decrease of 6%, which was not statistically significant (rate ratio, 0.94; 95% CI, 0.86–1.05; P = 0.11).28
Simulation
Simulation is another method commonly used to improve teamwork skills either in conjunction with classroom training or by itself. Simulation provides teams with realistic scenarios that they may face, either routinely or in emergencies, and allows teams to practice important teamwork skills.
Only one study was identified that measured transfer from the simulation intervention onto the job.23 The authors found that the group who received the full intervention (condensed TeamSTEPPS training coupled with 11 simulation exercises over the course of 12 months) significantly decreased their weighted adverse outcome score from 1.15 to 0.72 (P < 0.05) over the study period. The weighted adverse outcome score for the group that received only the condensed TeamSTEPPS training remained stable (1.46–1.45, not significant), and the control group’s adverse outcome score increased over the study period from 1.05 to 1.50. Thus, the simulation exercises seem to have been integral to the improvements observed in outcomes.
Tools to Support Teamwork on the Job
Improvements in Skills and Processes
There are a variety of tools available to foster and reinforce teamwork in health care settings. Three studies in the review implemented briefings, 2 implemented handoffs, and 3 used a checklist. Because these tools were introduced within the actual work setting, sustained changes in processes on the job, rather than transfer, will be detailed in this section.
For example, Kleiner et al13 found that teams coached in how to conduct quality surgical prebriefs and debriefs showed sustained improvement in briefing communication. After the coaching intervention, the quality of prebriefs significantly increased from 3.478 to 3.644 (P = 0.044) indicating greater use of a standardized checklist, an increase in team member introductions, greater discussion of contingency plans, and the opportunity for team members to ask questions. Similarly, the quality of debriefs significantly increased from 2.377 to 2.991 (P < 0.0001), signifying greater use of a standard checklist, greater discussion of went well and what did not go well, and that team members were thanked.
Two studies demonstrated process improvements by implementing handoffs. One study found that their handoff implementation was associated with greater participation among team members at handoff (P < 0.001) and increased information sharing–related surgical procedures (P < 0.05).20 Another study supported the efficacy of a structure handover process between the operating room and intensive care unit, where the structured handover was associated with a significant decrease in both the number of process errors (6.1–2.8, P < 0.001) and information sharing errors 6 months after the intervention (5.2 per handover to 2.3 per handover, P < 0.001).14
A final study implemented a preprocedural checklist to increase communication in operating room.22 Compliance significantly increased to 96% immediately after the introduction of the preprocedural checklist was sustained at an 18-month audit, where compliance remained at 96%. Similarly, team member self-introductions also remained high as they occurred 94% of the time immediately after the intervention continued to increase slightly at the 18-month audit (97%, P < 0.0001).
Patient Outcomes
Four studies of performance tools collected measures related to Kirkpatrick’s results-level criteria. Two studies measured the impact of briefings on patient outcomes. A study of resuscitation teams reported improvement in survival to hospital discharge for cases in the debrief intervention group as compared with a control group (52% for debriefed cases versus 33% for control cases, P = 0.054).27 Survival with favorable neurologic outcomes significantly increased for the cases in the debrief intervention group as well (50% for debrief cases versus 29% for control cases, P = 0.036).
Another study assessed the efficacy of roundtable debriefing on patient fall rates in the emergency department.21 Although the patient fall rates did decline somewhat in the postintervention period, there were no statistically significant differences in the number of assisted falls (P = 0.17), unassisted falls (P = 0.28), and the rate of falls per 1000 patient encounters (P = 0.28) as compared with the preintervention period.
The effectiveness of checklists to improve adverse events was also examined in 2 studies. A decrease in the overall number of adverse events was reported by Fargen et al10 after the implementation of a checklist. Additional evidence was provided by Bliss et al9 where they reported that the use of a surgical safety checklist was associated with significantly lower adverse event rates (8.9%) as compared with the performance of a historical control group (23.6%) and a group that had received team training with no checklist (15.9%). Thus, the cohort that received team training and used the checklist had the lowest rate of adverse events.
DISCUSSION AND CONCLUSIONS
Efforts to enhance teamwork have been immensely popular in health care. By 2015, it had been estimated that well over 10,000 individuals had participated in the TeamSTEPPS Master Trainer Workshop.29 In sharing their insights of 10 years of TeamSTEPPS work, Baker et al30 recognized its immense spread, not only in the United States, where it is estimated that approximately 35% of all health care workers have been exposed to TeamSTEPPS in some form, but also around the world. Moreover, previous research has demonstrated that programs such as TeamSTEPPS, CRM, and MTT can positively impact the transfer of teamwork skills, clinical processes, and patient safety (e.g., Weaver et al,2 Hughes et al8).
Most studies in the current review were conducted in a hospital setting and focused on improving teamwork among frontline staff. Studies varied in their approach, with some relying on team training programs to improve teamwork and some implementing tools aimed at enhancing teamwork directly in their work settings. In some instances, a teamwork intervention that had been successfully implemented in at least one unit or clinical area at a given institution was extended and tested in another.18,21 In other cases, the study reviewed served as a jumping off point for the institution, with plans to introduce the training and/or tools in additional clinical areas in the future (e.g., Halverson et al11).
In terms of team training programs, training was most often delivered to a specific unit (e.g., obstetrics and intensive care unit), although some studies did conduct training at the hospital level (e.g., Levy et al15). Posttraining measures were collected anywhere from 30 days to 17 months after the training. Consistent with previous research, positive improvements were demonstrated on a variety of team KSAs, clinical processes, and patient outcome measures.2,8 Only one study was identified that assessed whether simulation led to improved performance on the job, finding positive results consistent with previous research.7,8
The studies in the current review also begin to expand upon research conducted on team training by also examining support tools (e.g., briefings, checklists, and handoffs), which are often implemented after training programs to foster and enhance teamwork on the job. These tools were introduced in a mixture of units/departments including surgical units, intensive care units, emergency departments, and perinatal units. Across studies, these low-cost tools demonstrated positive impacts on the processes and clinical outcomes measured, with sustained improvements reported 6 to 18 months after implementation.
As cautioned by Rosen et al,31 introducing tools such as checklists and briefings may seem to require less time or fewer resources to implement than team training programs. Although implementing these tools may not require time off the job, time and due diligence are needed to educate staff on why the selected tool is being implemented, how the tool should be used, and how the tool fits into established workflows. Once implemented, new protocols sometimes require greater time and participation by the entire team to ensure all elements are covered. For example, increases in the length of handoffs were reported by Krimminger et al,14 whereas a checklist introduced in another study required that more members of the operating room team take an active role in completing the items on the checklist.22 Although this may have led to some resistance and dissatisfaction, the new protocols also led to more engaged teams, greater information being exchanged, and fewer errors in the studies reviewed.
The importance of leadership involvement and project champions was stressed across studies regardless of the specific practice used to improve teamwork.11,17,22,26 Leadership support is needed to not only help get a practice off the ground but also ensure that there is compliance over time. For example, leaders may be involved in endorsing and promoting training programs, as well as participating in (or being present during) team training workshops. In the case of implementing performance support tools on the job, leadership support can signal that support tools are critical to quality and safety of care rather than merely an additional administrative task.31 In addition, leadership can provide reinforcement when staff use the tools as intended and help ensure that their use is sustained over time.
The studies reviewed used multiple methods of measurement including surveys and observational data. Furthermore, these data were collected at the individual level (in the case of survey data) and at the team level (in the case of observational data). Collectively, the studies reviewed provide support for team training interventions and performance support tools for improving teamwork, sustaining those improvements on the job, and positively influencing clinical and patient outcomes.
Future Research
Results from the 20 studies in the current review add to the existing evidence base demonstrating that team training programs can positively impact the transfer of teamwork skills, improve clinical processes, and increase patient safety.2,8 In addition, performance support tools such as briefings, handoffs, and checklists can also help to foster critical teamwork skills on the job. Although specific settings were not included in the search strategy to identify articles, nearly all of the studies reviewed were conducted within hospital settings. However, efforts to improve teamwork have also been introduced in other health care settings such as primary care, ambulatory settings, and long-term care. Although work may be underway in these settings, there is a lack of published, quantitative studies to add to the evidence base (especially related to the impact on patient outcomes), and thus, this is an area requiring further research.
Specific tools to sustain performance on the job (e.g., checklists) have received less attention when synthesizing the literature on teamwork interventions in health care. As evidenced by the studies in the current review, team training and support tools have been implemented in a variety of inpatient settings. The breadth of departments and specialty areas in which studies have been conducted helps demonstrate the importance of teamwork, as well as the applicability of team training and tools. However, this breadth also makes it more difficult to draw conclusions about what team intervention is most effective in specific settings. In addition, some studies included small sample sizes. Further studies are needed to help understand which teamwork interventions have the greatest impact in different health care environments including those outside inpatient hospital settings.
Lastly, limitations to the current review should be noted. First, 2 databases were searched to identify articles, although additional studies may have been identified through databases such as PsycINFO. Second, only one individual reviewed the abstracts and full-text articles for inclusion in the current review. Having 2 independent reviewers would have strengthened the reliability of the overall review. Third, the current review focused on collecting evidence from studies that were conducted in the United States. However, numerous studies of teamwork and team training have been conducted abroad and provide additional evidence that team training programs such as CRM and TeamSTEPPS enhance team KSAs as well as patient outcomes. Finally, studies where improving teamwork was not the primary focus were also excluded. Although this made it easier to attribute desirable results to the teamwork intervention used, future efforts may wish to include studies where improving teamwork was a secondary objective.
Footnotes
The authors disclose no conflict of interest.
Sources of Support: This work was funded by the Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services (contract nos. HHSP233201500013I and HHSP23337002T).
REFERENCES
- 1.The Joint Commission National patient safety goals effective January 1, 2014: Hospital accreditation program.
- 2.Weaver SJ, Dy SM, Rosen MA. Team-training in healthcare: a narrative synthesis of the literature. BMJ Qual Saf. 2014;23:359–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kirkpatrick DL. How to start an objective evaluation of your training program. J Am Soc Train Dir. 1956;10:18–22. [Google Scholar]
- 4.Kirkpatrick DL. Great ideas revisited: revisiting Kirkpatrick’s four-level model. Train Dev. 1996;50:54–59. [Google Scholar]
- 5.Grogan EL Stiles RA France DJ, et al. The impact of aviation-based teamwork training on the attitudes of health-care professionals. J Am Coll Surg. 2004;199:843–848. [DOI] [PubMed] [Google Scholar]
- 6.Nielsen PE Goldman MB Mann S, et al. Effects of teamwork training on adverse outcomes and process of care in labor and delivery: a randomized controlled trial. Obstet Gynecol. 2007;109:48–55. [DOI] [PubMed] [Google Scholar]
- 7.Boet S Bould MD Fung L, et al. Transfer of learning and patient outcome in simulated crisis resource management: a systematic review. Can J Anaesth. 2014;61:571–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hughes AM Gregory ME Joseph DL, et al. Saving lives: a meta-analysis of team training in healthcare. J Appl Psychol. 2016;101:1266–1304. [DOI] [PubMed] [Google Scholar]
- 9.Bliss LA Ross-Richardson CB Sanzari LJ, et al. Thirty-day outcomes support implementation of a surgical safety checklist. J Am Coll Surg. 2012;215:766–776. [DOI] [PubMed] [Google Scholar]
- 10.Fargen KM Velat GJ Lawson MF, et al. Enhanced staff communication and reduced near-miss errors with a neurointerventional procedural checklist. Journal of Neurointerventional Surgery. 2013;5:497–500. [DOI] [PubMed] [Google Scholar]
- 11.Halverson AL Andersson JL Anderson K, et al. Surgical team training: the Northwestern Memorial Hospital experience. Arch Surg. 2009;144:107–112. [DOI] [PubMed] [Google Scholar]
- 12.Halverson AL Casey JT Andersson J, et al. Communication failure in the operating room. Surgery. 2011;149:305–310. [DOI] [PubMed] [Google Scholar]
- 13.Kleiner C Link T Maynard MT, et al. Coaching to improve the quality of communication during briefings and debriefings. AORN J. 2014;100:358–368. [DOI] [PubMed] [Google Scholar]
- 14.Krimminger D Sona C Thomas-Horton E, et al. A multidisciplinary QI initiative to improve OR-ICU handovers. Am J Nurs. 2018;118:48–59. [DOI] [PubMed] [Google Scholar]
- 15.Levy PD Dancy JN Stowell SA, et al. Lessons in flying: crew resource management as a quality improvement method for acute coronary syndromes care. Crit Pathw Cardiol. 2014;13:36–42. [DOI] [PubMed] [Google Scholar]
- 16.Lisbon D Allin D Cleek C, et al. Improved knowledge, attitudes, and behaviors after implementation of TeamSTEPPS training in an academic emergency department: a pilot report. Am J Med Qual. 2016;31:86–90. [DOI] [PubMed] [Google Scholar]
- 17.Mahoney JS Ellis TE Garland G, et al. Supporting a psychiatric hospital culture of safety. J Am Psychiatr Nurses Assoc. 2012;18:299–306. [DOI] [PubMed] [Google Scholar]
- 18.Mancuso MP Dziadkowiec O Kleiner C, et al. Crew resource management for obstetric and neonatal teams to improve communication during cesarean births. J Obstet Gynecol Neonatal Nurs. 2016;45:502–514. [DOI] [PubMed] [Google Scholar]
- 19.Mayer CM Cluff L Lin WT, et al. Evaluating efforts to optimize TeamSTEPPS implementation in surgical and pediatric intensive care units. Jt Comm J Qual Patient Saf. 2011;37:365–374. [DOI] [PubMed] [Google Scholar]
- 20.Mukhopadhyay D Wiggins-Dohlvik KC MrDutt MM, et al. Implementation of a standardized handoff protocol for post-operative admissions to the surgical intensive care unit. Am J Surg. 2018;215:28–36. [DOI] [PubMed] [Google Scholar]
- 21.Murphy LM Murphy SO Hastings MA, et al. Are interprofessional roundtable debriefings useful in decreasing ED fall rates? Findings from a quality-improvement project. J Emerg Nurs. 2015;41:375–380. [DOI] [PubMed] [Google Scholar]
- 22.Porter AJ Narimasu JY Mulroy MF, et al. Sustainable, effective implementation of a surgical preprocedural checklist: an “attestation” format for all operating team members. Jt Comm J Qual Patient Saf. 2014;40:3–9. [DOI] [PubMed] [Google Scholar]
- 23.Riley W Davis S Miller K, et al. Didactic and simulation nontechnical skills team training to improve perinatal patient outcomes in a community hospital. Jt Comm J Qual Patient Saf. 2011;37:357–364. [DOI] [PubMed] [Google Scholar]
- 24.Sonesh SC Gregory ME Hughes AM, et al. Team training in obstetrics: a multi-level evaluation. Fam Syst Health. 2015;33:250–261. [DOI] [PubMed] [Google Scholar]
- 25.Tapson VF, Karcher RB, Weeks R. Crew resource management and VTE prophylaxis in surgery: a quality improvement initiative. Am J Med Qual. 2011;26:423–432. [DOI] [PubMed] [Google Scholar]
- 26.Wolf FA, Way LW, Stewart L. The efficacy of medical team training: improved team performance and decreased operating room delays: a detailed analysis of 4863 cases. Ann Surg. 2010;252:477–483. [DOI] [PubMed] [Google Scholar]
- 27.Wolfe H Zebuhr C Topjian AA, et al. Interdisciplinary ICU cardiac arrest debriefing improves survival outcomes. Crit Care Med. 2014;42:1688–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Young-Xu Y Neily J Mills PD, et al. Association between implementation of a medical team training program and surgical morbidity. Arch Surg. 2011;146:1368–1373. [DOI] [PubMed] [Google Scholar]
- 29.Global Diffusion of Healthcare Group Global diffusion of healthcare innovation study: Accelerating the journey. 2015. Available at: https://www.wish.org.qa/wp-content/uploads/2018/01/WISH_GHDI_Report_2.pdf. Accessed November 27, 2019.
- 30.Baker DP, Battles JB, King HB. New insights about team training from a decade of TeamSTEPPS. In: Patient Safety Network. Rockville, MD: Agency for Healthcare and Quality; 2017. [Google Scholar]
- 31.Rosen MA DiazGranados D Dietz AS, et al. Teamwork in healthcare: key discoveries enabling safer, higher-quality care. Am Psychol. 2018;73:433–450. [DOI] [PMC free article] [PubMed] [Google Scholar]


