Abstract
COVID-19 infection is associated with increased risk of acute kidney injury, but the imaging changes of the kidneys are not fully investigated yet. We report the computed tomography findings in a 17-year-old male who developed severe reversible renal impairment. Those findings are similar to the changes observed in patients with vasculitis and can be contributed to the thromboembolic manifestations associated with corona virus infection.
Keywords: COVID-19, Kidney, Renal, Imaging, CT, Injury
Background
Acute kidney injury is a known complication of COVID-19 infection. However, the imaging findings of the kidneys have rarely been reported. We report the radiological changes involving the kidneys in a patient with COVID-19 infection and the proposed mechanisms for their development.
Case report
A 17-year-old male with morbid obesity (body mass index 47.16) but otherwise no past medical history presented with 4 days history of fever, shortness of breaths, productive cough and pleuritic chest pain. The patient was referred from a private hospital with acute respiratory distress as the oxygen saturation was 55% in room air associated with tachypnea (respiratory rate, 50 breaths/min) and tachycardia (pulse rate, 135 beats/min). His temperature was 38.5°C and blood pressure was 138/87 mmHg. The physical examination was unremarkable.
Laboratory findings revealed leukocytosis (WBC count of 21.9 × 109/L), hemoglobin of 151 g/L, sodium 129 mmol/L, blood urea nitrogen 4.2 mmol/L, creatinine 65 µmol/L, serum lactate dehydrogenase (LDH) 453 U/L, creatine kinase > 42,670 U/L, lactic acid 4.41 mmol/L, and D-dimer 5.19 mg/L. The liver function tests were also significantly elevated, alanine aminotransferase (ALT) of 407 U/L and aspartate aminotransferase (AST) of 430 U/L
A chest X-ray showed diffuse bilateral coarse reticular infiltrates.
The patient was placed on BiPAP and was admitted to the ICU. A nasopharyngeal swab was performed and COVID-19 infection was confirmed. On the following day, his clinical condition worsened and he was intubated. He also developed acute kidney injury that required the initiation of hemodialysis. The serum creatinine level raised significantly from 53 to 270 µmol/L and was continuously elevating until it reached 1147 µmol/L (Fig. 4). Continuous renal replacement therapy was initiated followed by hemodialysis. It started as short sessions of daily hemodialysis that lasted for 3 days and then was adjusted to be three times a week in sessions of three and a half hours each. After 3 more days, it was again adjusted to be four times a week in sessions of four hours each. It was performed through a right internal jugular temporary catheter using a dialysis solution with a bicarbonate concentration of 38 mmol/L, potassium 2 mmol/L, calcium 1.5 mmol/L and sodium 135 mmol/L. The dialyzer membrane was FX 80, dialysis temperature 36.5 C, dialysate flow 500 ml/min and blood flow between 250 and 300 ml/min. A heparin bolus of 1000 IU was administered at the start of every session followed by a maintenance infusion of 500 IU/hr.
Fig. 4.
Serial trend of creatinine level over time.
A computed tomography (CT) scan of the chest, abdomen and pelvis was obtained. The chest CT showed bilateral peripheral lower-lobe predominant ground glass opacities, classical for COVID-19 infection but no pulmonary embolism (Fig. 1). The abdominal CT revealed bulky kidneys with bilateral peripheral focal areas of decreased attenuation (Fig. 2). A trans-esophageal echocardiography was normal without signs of infective endocarditis.
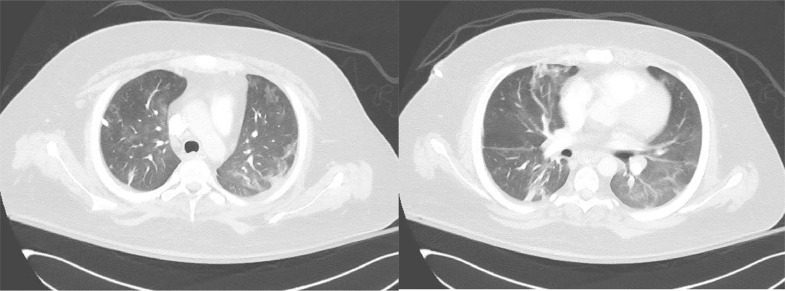
Fig. 1.
CT chest showing bilateral peripheral ground glass opacities.
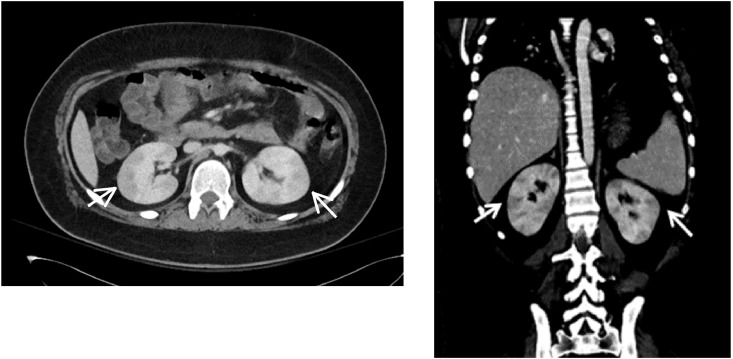
Fig. 2.
Abdominal CT showing bulky kidneys with bilateral peripheral geographic hypodense areas (small white arrows).
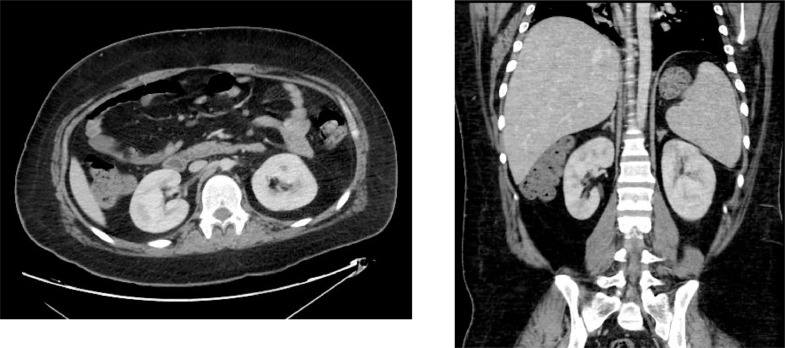
After 7 weeks of fluctuating hospital course with supportive treatment, the patient's clinical status gradually improved. He was extubated with maintained oxygen saturation on room air. The renal impairment was resolved with cessation of hemodialysis. The serum creatinine level dropped gradually until it normalized (Fig. 4). Liver function tests as well as the inflammatory markers were normalized and the repeated throat swabs were negative. The last chest X-ray was almost normal. A repeated CT scan of the abdomen and pelvis was carried out and revealed significant improvement of the bilateral kidney changes (Fig. 3). The patient was discharged home and continued to do well.
Fig. 3.
Follow-up abdominal CT showing almost complete resolution of the bilateral kidney hypodense striations.
Discussion
With the emergence of coronavirus disease 2019 pandemic, several studies were carried out to explore the imaging findings in patients with COVID-19. The chest imaging findings were thoroughly evaluated in the recent reports; however, few studies were published regarding the abdominal findings. Of those, the most reported abdominal imaging findings were related to the gastrointestinal tract. At the time of writing, Only 3 case reports described the kidney changes associated with COVID-19 infection [[1], [2], [3], [4]].
The kidney changes in our patient were similar to the previously reported findings in the form of multiple bilateral low attenuation defects and infarctions. Those changes are similar to the findings observed in patients with vasculitis and are likely related to vasculopathy as proposed in the recent literature.
All the reported cases in addition to our patient developed reversible acute renal impairment that gradually improved after treatment. Our patient and only one of the previously reported patients required temporary hemodialysis.
There are multiple proposed mechanisms for the development of vasculopathy, hypercoagulability and acute kidney injury in patients with COVID-19 infection. They may include direct cytopathic effects of the virus on endothelial cells and kidneys, cytokine storm, hypotension leading to renal hypoperfusion or renal medullary hypoxia [[5], [6], [7]].
Conclusion
COVID-19 infection affecting the kidneys can manifest radiologically as bilateral peripheral low perfusion changes similar to the findings observed in patients with vasculitis and can be contributed to vasculopathy and thromboembolic manifestations associated with corona virus infection.
Declaration of Competing Interest
None.
Contributor Information
Samah Faqeeh, Email: samah.faqeeh@gmail.com.
Raad Madkhali, Email: madkhalira@ngha.med.sa.
References
- 1.Xu JJ, Samaha D, Mondhe S, Massicotte-Azarniouch D, Knoll G, Ruzicka M. Renal infarct in a COVID-19–positive kidney–pancreas transplant recipient. Am J Transplant. 2020;00:1–4. doi: 10.1111/ajt.16089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Post A, den Deurwaarder ESG, Bakker SJL, Haas R, Meurs M, Gansevoort R. Kidney infarction in patients with COVID-19. Am J Kidney Dis. 2020 doi: 10.1053/j.ajkd.2020.05.004. S0272-6386(20)30723-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lushina N, Kuo JS, Shaikh HA. Pulmonary, cerebral, and renal thromboembolic disease associated with COVID-19 infection. Radiology. 2020 doi: 10.1148/radiol.2020201623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhayana R, Som A, Li MD, Carey DE, Anderson MA, Blake MA. Abdominal imaging findings in COVID-19: preliminary observations. Radiology. 2020 doi: 10.1148/radiol.2020201908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Behzada S, Aghaghazvinib L, Radmardb A, Gholamrezanezhadc A. Extrapulmonary manifestations of COVID-19: radiologic and clinical overview. Clinical Imaging. 2020;66:35–41. doi: 10.1016/j.clinimag.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mondal R, Lahiri D, Deb S, Bandyopadhyay D, Shome G, Sarkar S. COVID-19: are we dealing with a multisystem vasculopathy in disguise of a viral infection? J Thromb Thrombolysis. 2020:1–13. doi: 10.1007/s11239-020-02210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olson MC, Lubner MG, Menias CO, Mellnick VM, Gettle LM, Kim DH. RadioGraphics update: venous thrombosis and hypercoagulability in the abdomen and pelvis-findings in COVID-19. Radiographics. 2020 doi: 10.1148/rg.2020200119. [DOI] [PMC free article] [PubMed] [Google Scholar]