Abstract
Background
Stay-at-home orders (lockdowns) have been deployed globally to control COVID-19 transmission, and might impair economic conditions and mental health, and exacerbate risk of food insecurity and intimate partner violence. The effect of lockdowns in low-income and middle-income countries must be understood to ensure safe deployment of these interventions in less affluent settings. We aimed to determine the immediate impact of COVID-19 lockdown orders on women and their families in rural Bangladesh.
Methods
An interrupted time series was used to compare data collected from families in Rupganj upazila, rural Bangladesh (randomly selected from participants in a randomised controlled trial), on income, food security, and mental health a median of 1 year and 2 years before the COVID-19 pandemic to data collected during the lockdown. We also assessed women's experiences of intimate partner violence during the pandemic.
Results
Between May 19 and June 18, 2020, we randomly selected and invited the mothers of 3016 children to participate in the study, 2424 of whom provided consent. 2414 (99·9%, 95% CI 99·6–99·9) of 2417 mothers were aware of, and adhering to, the stay-at-home advice. 2321 (96·0%, 95·2–96·7) of 2417 mothers reported a reduction in paid work for the family. Median monthly family income fell from US$212 at baseline to $59 during lockdown, and the proportion of families earning less than $1·90 per day rose from five (0·2%, 0·0–0·5) of 2422 to 992 (47·3%, 45·2–49·5) of 2096 (p<0·0001 comparing baseline with lockdown period). Before the pandemic, 136 (5·6%, 4·7–6·6) of 2420 and 65 (2·7%, 2·1–3·4) of 2420 families experienced moderate and severe food insecurity, respectively. This increased to 881 (36·5%, 34·5–38·4) of 2417 and 371 (15·3%, 13·9–16·8) of 2417 during the lockdown; the number of families experiencing any level of food insecurity increased by 51·7% (48·1–55·4; p<0·0001). Mothers' depression and anxiety symptoms increased during the lockdown. Among women experiencing emotional or moderate physical violence, over half reported it had increased since the lockdown.
Interpretation
COVID-19 lockdowns present significant economic, psychosocial, and physical risks to the wellbeing of women and their families across economic strata in rural Bangladesh. Beyond supporting only the most socioeconomically deprived, support is needed for all affected families.
Funding
National Health and Medical Research Council, Australia.
Introduction
Stay-at-home (lockdown) orders have been deployed across high-income, middle-income, and low-income countries as a non-pharmaceutical public health intervention to control COVID-19 transmission.1 By April, 2020, up to 2·6 billion people worldwide were living in areas under some form of stay-at-home order or lockdown.2 After confirmation of the first cases of COVID-19 on March 8, 2020, Bangladesh issued an order on March 26, mandating closure of all government and private offices, schools and universities, agriculture and industrial activities, and domestic air, road, and rail travel, and advising the population to remain at home unless completing essential tasks.3 Dhaka and neighbouring districts (particularly Narayanganj) have had the highest number of cases. The lockdown order remained in place until May 30, 2020, after which restricted movement of people was permitted. However, cases of COVID-19 continued to rise in the second week of June, and localised lockdowns in areas of highest transmission were reinstated.
Research in context.
Evidence before this study
We searched PubMed from inception to July 18, 2020, using the terms “(COVID-19 OR SARS-CoV2) AND (domestic violence OR intimate partner violence OR food insecurity OR economic OR mental health OR depression OR anxiety) AND (LMIC OR low income country OR poverty OR middle income country OR Bangladesh OR India OR Pakistan OR Asia OR Africa OR Latin America)”. A small study in one town of Sierra Leone showed ubiquitous economic inactivity, increased symptoms of depression and anxiety, and concerns about food insecurity. Apart from this study, we did not identify others measuring psychological, economic, food security, or intimate partner violence outcomes using a direct field study. We did identify one study from Bangladesh in the non-academic literature. We identified several studies assessing impacts of COVID-19 and lockdowns on socioeconomic and mental health outcomes in low-income countries using online tools to gather data and sampling through social media to access participants. These studies consistently showed a high prevalence of symptoms of anxiety and depression. However, these study designs might suffer from selection bias and do not access the rural poor.
Added value of this study
We directly measured the impact of lockdown on rural families living in a lower-middle-income country, and compared parameters to pre-lockdown baselines. We randomly sampled from a cohort of families previously enrolled in a community randomised controlled trial, which itself had a low screen failure rate and was representative of the underlying community. Our interrupted time series data demonstrate marked reductions in income, increases in food insecurity (including moderate and severe food insecurity), and deteriorations in mental health. Further, our data indicate an increase in anxiety, and document experiences of intimate partner violence.
Implications of all the available evidence
Stay-at-home orders to ameliorate transmission of COVID-19 exert a substantial economic and social cost to family welfare, family nutritional status, and to women's mental wellbeing and safety. If future lockdowns are required to control transmission of COVID-19 or another pathogen, a comprehensive public health response must underwrite economic circumstances and incorporate solutions that ensure the wellbeing of families and, in particular, women.
Home confinement of families and the inability to continue employment raised concerns about effects on economic circumstances, mental health, and intimate partner violence.4 Quarantine (eg, the 2003 severe acute respiratory syndrome epidemic) has been previously associated with substantial and wide-ranging adverse mental health effects, including depression, anxiety,5 and post-traumatic stress disorder.6 In the absence of a vaccine, COVID-19 might become an established infection, and physical distancing and intermittent lockdowns are potentially recurring public health tools for controlling transmission.7
The immediate impact of lockdowns on individuals and families in low-income and middle-income countries (LMICs) is not well understood. In these settings, safety nets to protect incomes and livelihoods might be scarce or absent, compromising access to essentials, especially food.8 The pandemic and associated lockdown might especially impair mental health in affected LMIC settings.9 Reports published to date indicate that economic or psychological stress induced by COVID-19 has exacerbated the incidence of depression and suicide in South Asia.10, 11 Furthermore, confinement of women at home with their partners coupled with substantial financial and emotional stress might increase the risk of intimate partner violence.12
Although Bangladesh has achieved substantial macroeconomic growth over the past decade, about 15 million of its 160 million people still live in extreme poverty, on less than US$1·90 per day.13 More than 60% of the Bangladeshi population live in rural areas.14 Understanding the broad impact of stay-at-home orders on family and particularly women's wellbeing in LMICs and especially in rural communities, where capacity to endure impacts of confinement might be limited, is important to the steering of COVID-19 control efforts. Such information might be crucial for policy makers deciding on the implementation of lockdowns, and for government and non-government organisations involved in the economic and psychosocial protection of families.
In a rural Bangladeshi setting with a high incidence of COVID-19, we aimed to evaluate the immediate effects of at least 8 weeks of stay-at-home orders on family economic outcomes and food security, and on women's mental health and experiences of intimate partner violence, and compare this to their situation before the pandemic.
Methods
Study design and participants
We used an interrupted time-series design among mothers (or female guardians) of children enrolled in the Benefits and risks of iron interventions in children (BRISC) trial—a randomised controlled trial of preventive iron supplementation or placebo given to infants aged 8 months (ACTRN12617000660381) with a primary outcome of child cognitive development after 3 months of intervention. The BRISC trial was set in Rupganj upazila (county) of Narayanganj district, a rural area about 35 km northeast of Dhaka, which covers about 235 km2 and comprises about 82 000 households. Residents work in agriculture, the garment industry, and other industrial activities.
Recruitment to the BRISC trial was based on a house-to-house census enumeration of all infants living within the study area, followed by screening of children for eligibility. The trial enumerated 4065 children, screened 3933 children, and enrolled its target of 3300 children (84% of those screened). Singleton children without a diagnosed blood disorder or severe anaemia (Hb <80 g/L) were eligible when they were aged 8 months; households needed to have an available guardian, low drinking water iron content, and no plans for long-term departure from the study site over the forthcoming 12 months (appendix 2 p 2).15 Trial follow-up occurred up to 12 months post randomisation. At recruitment to the trial (between July 6, 2017 and Feb 20, 2019), mothers or guardians provided data on income, family food security, and maternal depression as a component of the baseline questionnaire. At study endline (12 months post randomisation) questions on food security and depression were repeated. The trial closed on Feb 10, 2020, and remains blinded as of August 2020.16 Like all of Bangladesh, Rupganj Upazila entered lockdown from March 26 to May 30, 2020; rising COVID-19 transmission locally resulted in lockdown being reinstated on June 10.17 We did the COVID-19 impact study over a 1-month period, from May 19 to June 18, 2020, inclusive.
Participants in the COVID-19 impact study were mothers of children enrolled in the BRISC trial. We randomly selected children who had been enrolled in BRISC, and contacted their mother by telephone to complete a questionnaire. All 3300 BRISC participants provided at least one mobile phone number during the screening phase of the BRISC study. The questionnaire (appendix 2 p 3) included modules assessing awareness and adherence to stay-at-home orders. Questions on income, food security, and symptoms of depression used during the BRISC trial were repeated. Questions on anxiety and experiences of intimate partner violence were asked for the first time. Food security was assessed using the Household Food Insecurity Access Scale (HFIAS), consisting of a set of items that assess anxiety and uncertainty about household food supply, insufficient food quality, and insufficient food intake over the previous 30 days.18 The HFIAS has been shown to appropriately distinguish food insecure from food-secure households and to detect changes in food security conditions of a population over time.19 Symptoms of depression were measured using a questionnaire based on the shortened version of the Centre for Epidemiologic Studies-Depression Scale20 that was a component of the family care indicators developed by UNICEF and previously used in Bangladesh.21 The six-question tool assessed the frequency of six depressive symptoms in the previous week. Higher scores indicate a higher frequency of depressive symptoms.22 Anxiety was assessed during lockdown only, and was measured using the Generalised Anxiety Disorder (GAD-7) tool,23 which has been previously successfully deployed in Bangladesh.24 The tool assessed the frequency of seven symptoms of anxiety over the past 2 weeks. A GAD-7 score of between 5 and 9, between 10 and 14, and above 14 was considered representative of mild, moderate, and severe anxiety, respectively.23 Intimate partner violence questions were based on the WHO multicountry survey tool,25 and specifically addressed emotional, physical, and sexual violence by the woman's husband since the last days of March 2020. This tool has been validated and previously used in Bangladesh.26 For all parameters, we also specifically asked participants whether outcomes had changed since the onset of stay-at-home orders (ie, last days of March 2020).
The questionnaire was developed, translated into Bangla and reverse translated, piloted in 77 women, and optimised to ensure all questions were understood by participants and were culturally appropriate. Questionnaires were administered over mobile telephone by trained research assistants who had previously been doing fieldwork for the trial, were familiar with the participants, and were trained for the current study by video conference. Participants were not compensated for their time in this study, although they had been compensated during the main trial at each visit (baseline, midline, endline). Women were warned before commencement of the intimate partner violence module and encouraged to seek privacy; they could decline to answer any module. If a woman had asked for help, we would have provided her information on how to contact available local services. Several non-governmental and government services provide shelter and physical and mental health consultation to women facing domestic violence. Only women living with their husbands were invited to continue to the intimate partner violence module.
Responses were recorded in an Android-based electronic questionnaire, which was synchronised with the server after each interview. Inter-interviewer and intra-interviewer agreement and reliability of measurements was confirmed by repeating a proportion of the interviews (appendix 2 p 21).
All work was approved by the institutional ethical review boards at the International Center for Diarrhoeal Diseases Research, Bangladesh, and Melbourne Health (2016.269). Participants recorded verbal informed consent before enrolment in the study.
Statistical analysis
Justification of the sample size of the BRISC trial is described elsewhere.15 The COVID-19 impact study aimed to enrol all mothers of BRISC participants during a discrete timepoint (1 month) of the lockdown. With the resulting sample size of 2424 participants, the maximum half-width of a two-sided 95% CI around a proportion was 2%. The analyses included mothers who provided informed consent for the survey. Descriptive statistics of all collected and derived variables were provided, whereby binary and categorical variables were summarised using frequencies and percentages, and continuous data using mean (SD) or median (IQR) if skewed. In addition, exact 95% CIs were provided for prevalence outcomes. To evaluate the immediate effect of the lockdown, regression models were used to compare repeated outcomes collected at baseline and lockdown and segmented regression models for outcome data collected during baseline, endline, and lockdown. Monthly income and maternal depression were positively skewed and analysed using a median regression model, and earning less than $1·90 per day and food insecurity were analysed using a generalised linear model with binomial distribution and identity link, while accounting for clustering within participant. Subgroup analyses by the father's occupation were done by adding this subgroup as well as interaction terms to the models. Summaries and analyses used all non-missing data. All statistical tests and 95% CIs were two-sided; no adjustment for multiple testing was made. Analyses were done and tables created using Stata, version 15.1. Figures were obtained using RStudio, version 1.2.1335.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Between May 19 and June 18, 2020, we randomly selected and approached the mothers of 3016 children, of whom 2424 (80%) participated. Of the 592 mothers who did not participate, 407 (68·7%) could not be located, 96 (16·2%) refused to participate, 11 (1·9%) had died, six (1·0%) were too busy, 15 (2·5%) would not provide consent, and 57 (9·6%) were not the mother of the child that previously participated in BRISC (appendix 2 p 10). Baseline and endline measures during the BRISC trial were taken a median of 708 days and 347 days before the COVID-19 assessment, respectively. Participants recruited for this analysis were representative of those enrolled in the overall BRISC trial (appendix 2 p 12). The study population had an identical prevalence of stunting, but tended to own more assets than national estimates (appendix 2 p 14).
Characteristics of the families collected at baseline are summarised in table 1 , along with information on awareness and adherence to the lockdown. Almost all (2414 [99·9%, 95% CI 99·6–99·9] of 2417) women were aware of the stay-at-home advice, and 2411 (99·8%, 99·5–99·9) of 2417 were at least partially adhering, with 1828 (75·6%, 73·8–77·3) leaving the home less often than previously. The mother was the member of the family most likely to leave the home: the main reasons for leaving the house were shopping for necessities (2153 [89·1%, 87·8–90·3] of 2417) or to do paid work (1204 [49·8%, 47·8–51·8] of 2417; table 1).
Table 1.
Cohort characteristics and responses to lockdown
| Total (N=2424) | ||
|---|---|---|
| Characteristics at baseline | ||
| Number of children <5 years living in household* | 2 (1–3) | |
| Monthly family income (Bangladeshi Taka)* | 18 000 (12 000–25 000) | |
| Number of children stunted | 502 (20·7%) | |
| Number of children underweight* | 192 (7·9%) | |
| Mother's age, years† | 24·1 (4·8) | |
| Mother's body-mass index, kg/m2‡ | 24·1 (4·2) | |
| Mother's educational status* | ||
| No education | 96 (4·0%) | |
| 1–8 years | 1242 (51·3%) | |
| 9–12 years | 996 (41·1%) | |
| >12 years | 88 (3·6%) | |
| Mother's main occupation† | ||
| Unemployed | 2357 (97·3%) | |
| Unskilled job | 22 (0·9%) | |
| Skilled job | 43 (1·8%) | |
| Father's age, years† | 31·1 (5·9) | |
| Father's educational status† | ||
| No education | 204 (8·4%) | |
| 1–8 years | 1265 (52·2%) | |
| 9–12 years | 809 (33·4%) | |
| >12 years | 144 (5·9%) | |
| Father's main occupation§ | ||
| Unemployed | 24 (1·0%) | |
| Unskilled job | 451 (18·6%) | |
| Skilled job | 1830 (75·6%) | |
| Other | 115 (4·8%) | |
| Lockdown | ||
| Family aware of stay-at-home order¶ | ||
| No | 3 (0·1%) | |
| Yes | 2414 (99·9%) | |
| Family adhering to stay-at-home order¶ | ||
| No | 6 (0·2%) | |
| Yes, sometimes | 717 (29·7%) | |
| Yes, completely | 1694 (70·1%) | |
| Member of family most often leaving the home¶ | ||
| Child's mother | 2023 (83·7%) | |
| Child's father | 130 (5·4%) | |
| Child's brother or sister | 11 (0·5%) | |
| Others | 253 (10·5%) | |
| Frequency of leaving the house¶ | ||
| Never | 9 (0·4%) | |
| Less than once a week | 104 (4·3%) | |
| Once a week | 476 (19·7%) | |
| 2–3 times a week | 912 (37·7%) | |
| Almost every day | 916 (37·9%) | |
| Change in frequency of leaving house since COVID-19¶ | ||
| More than before | 208 (8·6%) | |
| Same | 381 (15·8%) | |
| Less than before | 1828 (75·6%) | |
| Reason for leaving the house (more than one reason possible)¶ | ||
| NA (not going out) | 3 (0·1%) | |
| Recreation or playing | 15 (0·6%) | |
| Shopping necessities | 2153 (89·1%) | |
| Working or job | 1204 (49·8%) | |
| Home garden or farm | 57 (2·4%) | |
| Other | 85 (3·5%) | |
| Perception of lockdown‖ | ||
| Very frustrating | 1290 (53·5%) | |
| Sometimes frustrating | 575 (23·9%) | |
| I have accepted the situation | 459 (19·0%) | |
| I am enjoying the lockdown | 86 (3·6%) | |
Data are median (IQR), n (%), or mean (SD). Unskilled job describes manual unskilled work (eg, housemaid, garment worker involved in unskilled tasks, labourer, farmer, fisherman, or rickshaw puller). Skilled job describes skilled employment (eg, garment worker, cook, construction work, driving, tailor, craftsman, carpentry, government or non-government clerical work, health service providers including primary health workers, pharmacists, doctor, or teacher). NA=not applicable.
Defined as weight for age Z score of less than −2.
n=2422.
n=2419.
n=2420.
n=2417.
n=2410.
A reduction in work for the father or other family members was reported by 2321 (96·0%, 95% CI 95·2 to 96·8) of 2417 families, with 945 (39·1%, 37·1 to 41·1), 453 (18·7%, 17·2 to 20·4), and 639 (26·4%, 24·7 to 28·2) reporting income had reduced completely, by about three quarters, or by about half, respectively. Median monthly income fell from Bangladesh Taka 18 000 (IQR 12 000 to 25 000; US$212 [conversion June 22, 2020]) at baseline to 5000 (0 to 10 000; $59) during lockdown (−13 000, −14 509 to −11 491; p<0·0001 comparing baseline to lockdown period; table 2 ; appendix 2 p 15.
Table 2.
Impact of pandemic and lockdown on income and food security
| BRISC baseline | BRISC endline | COVID-19 impact study (May–June 2020) | Estimate* | p value† | |||
|---|---|---|---|---|---|---|---|
| Income‡ | |||||||
| Monthly family income§ | 18 000 (12 000 to 25 000) | NA | 5000 (0 to 10 000) | −13 000 (−14 509 to −11 491) | <0·0001 | ||
| Monthly family income§ by father's occupation | |||||||
| Unemployed | 15 000 (11 000 to 23 500) | NA | 0 (0 to 5000) | −15 000 (−15 226 to −14 774) | <0·0001 | ||
| Unskilled job | 14 000 (10 000 to 18 000) | NA | 4000 (0 to 7000) | −10 000 (−10 089 to −9911) | <0·0001 | ||
| Skilled job | 20 000 (15 000 to 25 000) | NA | 5000 (0 to 10 000) | −15 000 (−18 526 to −11 474) | <0·0001 | ||
| Other | 30 000 (20 000 to 40 000) | NA | 5000 (0 to 15 000) | −25 000 (−28 892 to −21 108) | <0·0001 | ||
| Income equivalent <US$1·90/day | 5 (0·2%) | NA | 992 (47·3%) | 47·1% (45·0 to 49·3) | <0·0001 | ||
| Income equivalent <US$1·90/day by father's occupation | |||||||
| Unemployed | 1/24 (4·2%) | NA | 12/18 (66·7%) | 62·5% (36·9 to 88·1) | <0·0001 | ||
| Unskilled job | 2/451 (0·4%) | NA | 199/388 (51·3%) | 50·8% (45·9 to 55·8) | <0·0001 | ||
| Skilled job | 2/1830 (0·1%) | NA | 737/1592 (46·3%) | 46·2% (43·7 to 48·6) | <0·0001 | ||
| Other | 0/115 (0) | NA | 43/94 (45·7%) | 45·7% (35·7 to 55·8) | <0·0001 | ||
| Food security¶ | |||||||
| Household food insecurity access category | 51·7% (48·1 to 55·4) | <0·0001 | |||||
| Food secure | 1952 (80·7%) | 1743 (81·5%) | 739 (30·6%) | .. | .. | ||
| Mildly food insecure | 267 (11·0%) | 153 (7·2%) | 426 (17·6%) | .. | .. | ||
| Moderately food insecure | 136 (5·6%) | 181 (8·5%) | 881 (36·5%) | .. | .. | ||
| Severely food insecure | 65 (2·7%) | 62 (2·9%) | 371 (15·3%) | .. | .. | ||
| Household food insecurity access category by father's occupation | .. | .. | |||||
| Unemployed | 53·8% (15·6 to 92·0) | 0·0058 | |||||
| Food secure | 15/24 (62·5%) | 16/21 (72·7%) | 7/22 (29·2%) | .. | .. | ||
| Mildly food insecure | 6/24 (25·0%) | 2/21 (9·1%) | 3/22 (12·5%) | .. | .. | ||
| Moderately food insecure | 3/24 (12·5%) | 2/21 (9·1%) | 9/22 (37·5%) | .. | .. | ||
| Severely food insecure | 0/24 (0) | 2/21 (9·1%) | 5/22 (20·8%) | .. | .. | ||
| Unskilled job | 63·1% (53·6 to 72·5) | <0·0001 | |||||
| Food secure | 284/450 (63·1%) | 291/396 (74·4%) | 102/391 (22·7%) | .. | .. | ||
| Mildly food insecure | 99/450 (22·0%) | 38/396 (9·7%) | 75/391 (16·7%) | .. | .. | ||
| Moderately food insecure | 38/450 (8·4%) | 45/396 (11·5%) | 186/391 (41·3%) | .. | .. | ||
| Severely food insecure | 29/450 (6·4%) | 17/396 (4·3%) | 87/391 (19·3%) | .. | .. | ||
| Skilled job | 50·0% (45·9 to 54·2) | <0·0001 | |||||
| Food secure | 1544/1829 (84·4%) | 1341/1642 (82·9%) | 573/1617 (31·4%) | .. | .. | ||
| Mildly food insecure | 158/1829 (8·6%) | 108/1642 (6·7%) | 323/1617 (17·7%) | .. | .. | ||
| Moderately food insecure | 92/1829 (5·0%) | 126/1642 (7·8%) | 661/1617 (36·2%) | .. | .. | ||
| Severely food insecure | 35/1829 (1·9%) | 42/1642 (2·6%) | 268/1617 (14·7%) | .. | .. | ||
| Other | 33·1% (19·8 to 46·3) | <0·0001 | |||||
| Food secure | 107/115 (93·0%) | 92/108 (87·6%) | 56/105 (49·1%) | .. | .. | ||
| Mildly food insecure | 4/115 (3·5%) | 5/108 (4·8%) | 24/105 (21·1%) | .. | .. | ||
| Moderately food insecure | 3/115 (2·6%) | 7/108 (6·7%) | 24/105 (21·1%) | .. | .. | ||
| Severely food insecure | 1/115 (0·9%) | 1/108 (1·0%) | 10/105 (8·8%) | .. | .. | ||
Data are median (IQR), n (%), n/n (%), or estimate (95% CI). Unskilled job describes manual unskilled work (eg, housemaid, garment worker involved in unskilled tasks, labourer, farmer, fisherman, or rickshaw puller). Skilled job describes skilled employment (eg, garment worker, cook, construction work, driving, tailor, craftsman, carpentry, government or non-government clerical work, health service providers including primary health workers, pharmacists, doctor, or teacher). A daily income of US$1·90 was defined as corresponding to a monthly income of 58 Bangladeshi Taka (June 22, 2020, conversion). BRISC=Benefits and risks of iron interventions in children trial. NA=not applicable.
For income, the estimate is the difference between COVID-19 impact study and BRISC baseline. For food insecurity (ie, mildly, moderately, or severely food insecure), the estimate is the level change during lockdown from BRISC baseline to endline in food insecurity as per the interrupted time series analyses (appendix p 14).
The p value for interaction with father's occupation is p<0·0001 for monthly family income, p=0·24 for income equivalent under US$1·90/day, and p=0·0037 for food insecurity.
BRISC baseline n=2422; COVID impact study n=2096.
Bangladeshi Taka.
BRISC baseline n=2420; BRISC endline n=2139; COVID impact study n=2417.
Families reported they were managing financially through combinations of using present income (1411 [61·5%, 95% CI 59·5–63·5] of 2293), using savings (1070 [46·7%, 44·6–48·7] of 2293), procuring a loan (747 [32·6%, 30·7–34·5] of 2293), or accessing government (264 [11·5%, 10·2–12·9] of 2293), or other sources of relief (446 [19·5%, 17·8–21·1] of 2293). Overall, 1300 (53·8%, 51·8–55·8) of 2417 respondents considered their families very unstable financially, and a further 888 (36·7%, 34·8–38·7) of 2417 considered their finances somewhat unstable (appendix 2 p 15). At baseline, five (0·2%, 0·0–0·5) of 2422 families were earning less than $1·90 per day, and during the lockdown this number increased to 992 (47·3%, 45·2–49·5) of 2096 (p<0·0001 comparing baseline with lockdown period). Median income among individuals holding a skilled job fell from 20 000 to 5000; and for those holding an unskilled job from 14 000 to 4000. 737 (46·3%, 95% CI 43·8–48·8) of 1592 families where the father held a skilled job were earning less than $1·90 per day, while 199 (51·3%, 46·2–56·4) of 388 families where the father was holding an unskilled job were now earning less than $1·90 per day (table 2).
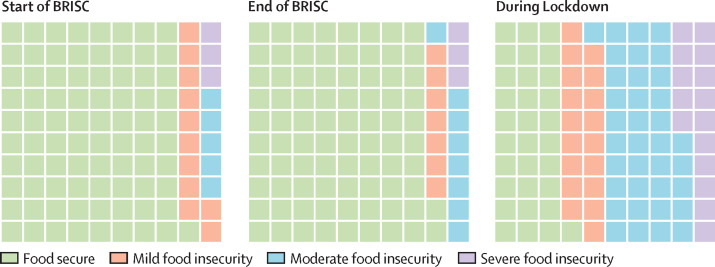
The impact of the pandemic and lockdown on food security are shown in figure 1 and table 2. Household food insecurity was prevalent, and this had increased from the BRISC timepoints. At baseline, of 2420 families, 1952 (80·7%, 95% CI 79·0–82·2) were food secure, and 267 (11·0%, 9·8–12·3), 136 (5·6%, 4·7–6·6), and 65 (2·7%, 2·1–3·4) experienced mild, moderate, and severe food insecurity, respectively; this food insecurity was stable 1 year later, at the trial endline assessment. However, during lockdown, of 2417 families, only 739 (30·6%, 28·7–32·5) remained food secure, and mild, moderate, and severe forms of food insecurity had increased to 426 (17·6%, 16·1–19·2%), 881 (36·5%, 34·5–38·4), and 371 (15·3%, 13·9–16·8), respectively. Between baseline and endline, there was no significant trend in the proportion of families who reported food insecurity (p=0·43), but there was a significant increase to 51·7% (48·1–55·4; p<0·0001; appendix 2 p 16) during lockdown. Subgroup analyses showed that although increased food insecurity was more prevalent among families with a father in an unskilled job, compared with a skilled job, impacts on income and food insecurity were profound across the population, irrespective of the father's occupation (table 2).
Figure 1.
Food security at BRISC trial baseline and endline, and during COVID-19 lockdown in families in Rupganj upazila, Bangladesh
Each square represents 1% of the survey sample. BRISC=Benefits and risks of iron interventions in children trial.
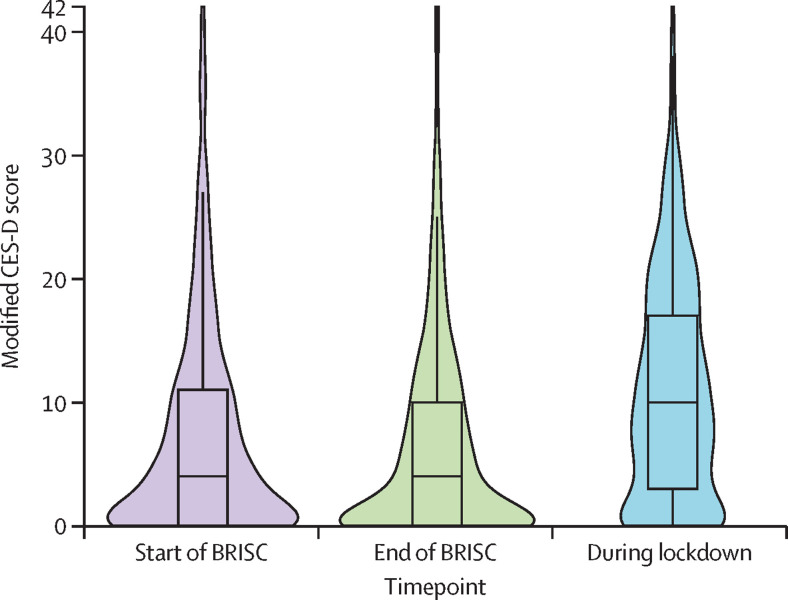
Maternal mental health deteriorated during the lockdown (appendix 2 p 18). Whereas symptoms of depression were stable between trial baseline (median 4, IQR 0–11) and endline (4, 0–10; p=1·00), symptoms increased during lockdown (10, 3–17; 6-point increase, 5·6–6·4; p<0·0001; figure 2 ; appendix 2 p 16). Anxiety was only measured during lockdown. The median GAD-7 score was 3·0 (1·0–7·0), and 620 (25·7%, 95% CI 24·0–27·5) of 2410 women reported a GAD-7 score consistent with mild anxiety, 293 (12·2%, 10·9–13·5) of 2410 reported a score consistent with moderate anxiety, and 32 (1·3%, 0·9–1·9) of 2410 reported severe anxiety. 1657 (68·8%, 66·9–70·6) of 2410 women reported anxiety symptoms had changed since the onset of lockdown; 1639 (98·9%, 98·3–99·4) of 1657 reported their anxiety had increased.
Figure 2.
CES-D scores at BRISC trial baseline and endline, and during COVID-19 lockdown
Violin plot showing median (IQR), together with kernel density plot to show frequency of data. CES-D=Centre for Epidemiologic Studies-Depression Scale. BRISC=Benefits and risks of iron interventions in children trial.
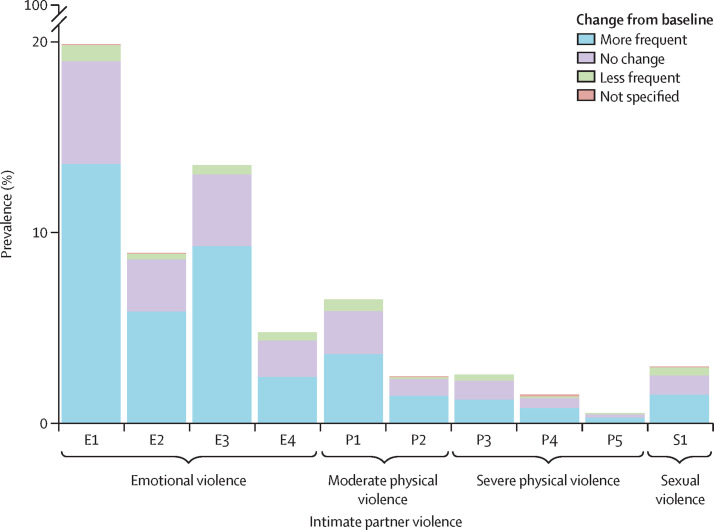
2174 women living with their husbands shared information about intimate partner violence during the lockdown. As shown in figure 3 and the appendix 2 (p 19), forms of emotional, physical, and sexual violence increased. Emotional violence included insults (reported by 19·9% [95% CI 18·2–21·6]; 290 [68·4%] of 424 reported an increase), humiliation (reported by 8·9% [7·8–10·2]; 126 [66·0%] of 191 reported an increase), and intimidation (reported by 13·5% [12·1–15·0]; 200 [68·7%] of 291 reported an increase). Physical violence (eg, being slapped or having something thrown at them) was reported by 6·5% (5·5–7·6; 76 [56%] of 135 reported an increase). Sexual violence was less common (3·0%, 2·3–3·8), but of those affected, 33 (50·8%) of 65 reported it had increased since the lockdown.
Figure 3.
Intimate partner violence during COVID-19 lockdown
Prevalence of intimate partner violence during COVID-19 lockdown, and reported change (more frequent, no change, or less frequent) from before the pandemic. Participants could report multiple forms of violence. Data are presented as prevalence of emotional violence (being insulted [E1], humiliated [E2], intimidated [E3], or threatened [E4]), physical violence (being slapped or having something thrown [P1]; being pushed or having their hair pulled [P2]; hit with a fist [P3]; kicked, dragged, beaten, choked, or burned [P4]; or threatened with or having a weapon used [P5]), or sexual violence (physically forced to have sexual intercourse [S1]).
Discussion
A stay-at-home order, lasting more than 2 months, in a rural South Asian setting has inflicted an enormous economic and psychosocial burden on women and their families. Reductions in employment have led to almost half the population entering extreme poverty, with markedly increased food insecurity. The lockdown has also increased symptoms of depression and anxiety, and exposed more women to intimate partner violence.
Stay-at-home orders to control community transmission of COVID-19 have been a critical public health measure in China, Europe, the USA, and other middle-income and high-income settings.1, 27 The macroeconomic cost of this intervention has been evident. However, the situation appears precarious in LMICs. In our study population, extreme poverty was rare before the lockdown; however, the pandemic and subsequent lockdown has seen the income of about half of families fall below $1·90 per day. This is associated with a concerning reduction in food security and increase in moderate and severe food insecurity. Severe food insecurity is defined when a household reduces the size and number of meals, runs out of food, or when members go to bed hungry or go a whole day and night without eating because of lack of access to food.18 The marked increase in such severe food insecurity in our study population shows the impact of economic pressure on food access,8 although other factors, including effects of the pandemic on food supply chains, might also contribute. Our findings are consistent with reductions in household income and food security seen in a cross-sectional telephone survey of families in urban and rural families across Bangladesh done earlier in the lockdown.28 Ultimately, the increase in food insecurity might impair nutritional outcomes in mothers and children.29 Our data provide primary evidence to support models that the pandemic will have a catastrophic effect on food security worldwide—eg, the World Food Programme estimates that food insecurity could double, to 265 million people, worldwide because of the pandemic;30 our findings suggest the impact could be even greater in some settings. We did not expect to find the levels of food insecurity we observed during this assessment, and during the lockdown we did not have immediate means of directly providing compensation. However, we are now planning to follow up this population as a cohort, and will budget to provide compensation to participants for future visits as well as retrospectively for the interview reported in this manuscript.
The population included in our study is broadly similar to the overall Bangladeshi population. 44·7% of our study population had a partial or completed secondary education; for Bangladesh overall, 52·2% had a similar educational attainment. In our group, stunting prevalence at age 8 months was identical to the national prevalence.31 Nevertheless, it is plausible that the relative proximity to Dhaka might have influenced the severity of the pandemic, lockdown, and its impact in our population, and that the effects differ further from the capital. Notably, Rupganj upazila is in Narayanganj subdistrict, which has among the highest incidence of COVID-19 outside Dhaka (appendix 2 p 11);32 this might have influenced psychological responses to the pandemic and adherence to the lockdown.
Our data provide crucial preliminary insights into experiences and impacts of the pandemic and lockdown in Bangladesh, and South Asia more broadly. Bangladesh is similar to other South Asian countries, including India, Nepal, and Pakistan: the 2019 human development index global ranking for these countries was 135th, 129th, 147th, and 152nd, respectively;33 in 2018, life expectancy for these countries was 72·3 years, 69·4 years, 70·5 years, and 67·1 years, respectively; gross domestic product per capita was $1203, $2100, $817, and $1197, respectively; and the rural population comprised 63·4%, 66%, 80·3%, and 63·3%, respectively.34 These countries have each imposed various forms of lockdown to mitigate transmission of COVID-19. To the extent our data are generalisable, we can predict that lockdowns have affected family economic status and wellbeing across the entire region.
The increase in intimate partner violence might represent a combination of predisposing and precipitating factors. In Bangladesh, 55·0% of women in rural areas and 48·7% in urban areas report having experienced physical or sexual violence from their husband.35 The most common reasons perceived by women were unprovoked violence, or violence provoked by a financial crisis; men cited disobedience by their wives as the leading cause.35 Precipitating factors in men during the pandemic might include the stress of losing work and income, which might arouse anxiety and also cause loss of occupational identity, humiliation, increases in depressed mood, and a feeling of powerlessness about the situation. These feelings might alter perpetrators' threshold to anger, which is directed to their wives and children. Our data provide an initial population estimate of the impact of COVID-19 and lockdown on intimate partner violence in the LMIC context.
Several studies have estimated effects of the COVID-19 pandemic on mental health. Media reports have linked fear of infection and economic stress due to COVID-19 to suicides across South Asia.11 Online surveys of Indians36 and Bangladeshis37 using social media and email-based sampling have shown reductions in wellbeing, and linked financial stressors, food insecurity, and fear of infection to increased stress.38 However, such studies are susceptible to selection bias and might not be generalisable to the population,39 and online surveys are unsuitable for capturing responses from less affluent, especially rural, populations in LMICs. Our study uses a representative sample and direct collection of data from participants by interviewers familiar with the interviewee, and had a high enrolment rate and low rate of missing data, which ensures generalisability to the underlying population.
Our study has several limitations. A geographically wider study might have ensured a broader sample of the country, but would have precluded longitudinal follow-up from the pre-COVID-19 situation, which is a strength of our analysis. Although our study setting is broadly similar to other LMIC settings, generalisability to urban settings (eg, slums) might be limited. We contacted our participants by telephone. Face-to-face interactions might have ensured more authentic responses, but fieldwork would be unsafe for both participants and researchers during the pandemic. Our questionnaire used modules that have been previously used in other community and field studies in Bangladesh. Additional modules addressing other considerations including women's empowerment, or using qualitative research methods to further understand experiences under lockdown would be of value in future studies. The severity of the impact raises the likelihood that detriments might be prolonged, and it will be essential to continue to monitor the cohort.
Two specific interventions appear important in ameliorating the impact of lockdown on family outcomes. First, it is essential to deliver welfare or other forms of social support to underwrite family income for affected families across economic strata,40 and not just those initially considered low income.41 In Bangladesh, the government has offered social security to 8 million people (socioeconomically deprived, older people, widows, and lactating mothers), and staple foods and cash support to poorer families.42 However, only 12% of our sample received government support and, despite this programme, we still observed increased food insecurity, including severe food insecurity. The lockdown is impacting not just the socioeconomically deprived, but also families of skilled workers. Support must therefore be broad, and reach all families experiencing a reduction in income, even if they were not below the poverty line at baseline. Second, local community services to protect the safety of women must be strengthened and supported, health workers could be trained in identification and intervention in cases of domestic violence, and it is crucial that services remain accessible to women even during lockdown.43
Acknowledgments
Acknowledgments
The work was conducted at the International Center for Diarrhoeal Diseases Research, Bangladesh. We thank all the participants in this study for their contribution during this difficult time. We thank the International Center for Diarrhoeal Diseases Research, Bangladesh, field team for contacting the participants and collecting the data. This work was supported by the Australian National Health and Medical Research Council (grant numbers GNT1103262, GNT1159151 and GNT1158696). The International Center for Diarrhoeal Diseases Research, Bangladesh, is also grateful to the Governments of Bangladesh, Canada, Sweden, and the UK for providing core or unrestricted support.
Contributors
JDH, MIH, SJH, and S-RP conceived the study. JDH, MIH, SJH, B-AB, SG-M, SB, and S-RP designed the study. JDH, MIH, SJH, SMMUT, SS, FT, MSAB, and SFM led data collection. AJB and SB did the statistical analyses. S-RP, JDH, JF, AJB, and SB wrote the first draft of the Article. All authors critically reviewed the Article and approved the final draft.
Declaration of interests
S-RP reports grants from the Australian National Health and Medical Research Council during the conduct of this study. The other authors declare no competing interests.
Supplementary Materials
References
- 1.Flaxman S, Mishra S, Gandy A. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020 doi: 10.1038/s41586-020-2405-7. published online June 8. [DOI] [PubMed] [Google Scholar]
- 2.Hoof EV. Lockdown is the world's biggest psychological experiment—and we will pay the price. 2020. https://www.weforum.org/agenda/2020/04/this-is-the-psychological-side-of-the-covid-19-pandemic-that-were-ignoring/
- 3.Government of Bangladesh Cabinet Fighting with coronavirus: press briefing of Cabinet Secretary. 2020. https://cabinet.gov.bd/sites/default/files/files/cabinet.portal.gov.bd/notices/9abbd38f_f012_401c_a172_4654fc2ffada/corona%20press%20briefing.pdf
- 4.Chandan JS, Taylor J, Bradbury-Jones C, Nirantharakumar K, Kane E, Bandyopadhyay S. COVID-19: a public health approach to manage domestic violence is needed. Lancet Public Health. 2020;5:e309. doi: 10.1016/S2468-2667(20)30112-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brooks SK, Webster RK, Smith LE. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10:1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368:860–868. doi: 10.1126/science.abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Global Nutrition Report. The 2020 Global Nutrition Report in the context of Covid-19. 2020. https://globalnutritionreport.org/reports/2020-global-nutrition-report/2020-global-nutrition-report-context-covid-19/
- 9.De Sousa A, Mohandas E, Javed A. Psychological interventions during COVID-19: challenges for low and middle income countries. Asian J Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dsouza DD, Quadros S, Hyderabadwala ZJ, Mamun MA. Aggregated COVID-19 suicide incidences in India: fear of COVID-19 infection is the prominent causative factor. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhuiyan AKMI, Sakib N, Pakpour AH, Griffiths MD, Mamun MA. COVID-19-related suicides in Bangladesh due to lockdown and economic factors: case study evidence from media reports. Int J Ment Health Addict. 2020 doi: 10.1007/s11469-020-00307-y. published online May 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boman JH, 4th, Gallupe O. Has COVID-19 changed crime? Crime rates in the United States during the pandemic. Am J Crim Justice. 2020;45:1–9. doi: 10.1007/s12103-020-09551-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Bank Country Profile: Bangladesh. 2018. https://databank.worldbank.org/views/reports/reportwidget.aspx?Report_Name=CountryProfile&Id=b450fd57&tbar=y&dd=y&inf=n&zm=n&country=BGD
- 14.World Bank 3.1 World Development Indicators: rural environment and land use. 2017. http://wdi.worldbank.org/table/3.1
- 15.Hasan MI, Hossain SJ, Braat S. Benefits and risks of Iron interventions in children (BRISC): protocol for a three-arm parallel-group randomised controlled field trial in Bangladesh. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2017-018325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Braat S, Larson L, Simpson JA. The benefits and risks of iron interventions in children (BRISC) trial: statistical analysis plan. F1000 Res. 2020;9:427. doi: 10.12688/f1000research.23383.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anon Lockdown lifted from three areas in Narayanganj—Rupganj union will be put under lockdown. The Business Standard. June 10, 2020 [Google Scholar]
- 18.Coates J, Swindale A, Bilinsky P. Food and Nutrition Technical Assistance; Washington, DC: 2007. Household Food Insecurity Access Scale (HFIAS) for measurement of food access: indicator guide. [Google Scholar]
- 19.Devereux S, Tavener-Smith L. Seasonal food insecurity among farm workers in the northern cape, South Africa. Nutrients. 2019;11 doi: 10.3390/nu11071535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolf AW, De Andraca I, Lozoff B. Maternal depression in three Latin American samples. Soc Psychiatry Psychiatr Epidemiol. 2002;37:169–176. doi: 10.1007/s001270200011. [DOI] [PubMed] [Google Scholar]
- 21.Hamadani JD, Mehrin SF, Tofail F. Integrating an early childhood development programme into Bangladeshi primary health-care services: an open-label, cluster-randomised controlled trial. Lancet Glob Health. 2019;7:e366–e375. doi: 10.1016/S2214-109X(18)30535-7. [DOI] [PubMed] [Google Scholar]
- 22.Nahar B, Hossain I, Hamadani JD, Ahmed T, Grantham-McGregor S, Persson LA. Effect of a food supplementation and psychosocial stimulation trial for severely malnourished children on the level of maternal depressive symptoms in Bangladesh. Child Care Health Dev. 2015;41:483–493. doi: 10.1111/cch.12176. [DOI] [PubMed] [Google Scholar]
- 23.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 24.Islam S, Akter R, Sikder T, Griffiths MD. Prevalence and factors associated with depression and anxiety among first-year university students in Bangladesh: a cross-sectional study. Int J Ment Health Addict. 2020 doi: 10.1007/s11469-020-00242-y. published online March 2. [DOI] [Google Scholar]
- 25.García-Moreno C, Jansen HAFM, Ellsberg M, Heise L, Watts C. World Health Organization; Geneva: 2005. WHO multi-country study on women's health and domestic violence against women—initial results on prevalence, health outcomes and women's responses. [Google Scholar]
- 26.Azziz-Baumgartner E, Homaira N, Hamadani JD. The prevalence and impact of intimate partner violence on maternal distress in a community of low-income Bangladeshi and displaced ethnic Bihari mothers: Dhaka, 2008–2009. Violence Against Women. 2014;20:59–73. doi: 10.1177/1077801213520579. [DOI] [PubMed] [Google Scholar]
- 27.Hsiang S, Allen D, Annan-Phan S. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature. 2020 doi: 10.1038/s41586-020-2404-8. published online June 8. [DOI] [PubMed] [Google Scholar]
- 28.Rahman HZ, Matin I. BRAC Institute of Governance and Development, Power and Participation Research Centre; Dhaka: 2020. Livelihoods, coping, and support during COVID-19 crisis. [Google Scholar]
- 29.The Lancet Global Health. Food insecurity will be the sting in the tail of COVID-19. Lancet Glob Health; 8: e737. [DOI] [PMC free article] [PubMed]
- 30.World Food Programme COVID-19 will double number of people facing food crises unless swift action is taken. 2020. https://www.wfp.org/news/covid-19-will-double-number-people-facing-food-crises-unless-swift-action-taken
- 31.National Institute of Population Research and Training and ICF . NIPORT and ICF; Maryland, USA: 2019. Bangladesh demographic and health survey 2017–18: key indicators. Dhaka, Bangladesh, and Rockville. [Google Scholar]
- 32.Bangladesh WHO. COVID-19 morbidity and mortality weekly update (MMWU) number 18. 2020. https://www.who.int/docs/default-source/searo/bangladesh/covid-19-who-bangladesh-situation-reports/who-covid-19-update-18-20200629.pdf?sfvrsn=6ef8ba08_2
- 33.UNDP Human Development Index Ranking. 2020. http://hdr.undp.org/en/content/2019-human-development-index-ranking
- 34.Bank W. Databank: World Development Indicators. 2020. https://databank.worldbank.org/reports.aspx?source=2&country=PAK,IND,BGD,LKA,NPL,AFG
- 35.National Institute of Population Research and Training (NIPORT) MaA, and Macro International . National Institute of Population Research and Training, Mitra and Associates, and Macro International; Dhaka, Bangladesh and Calverton, Maryland, USA: 2009. Bangladesh Demographic and Health Survey 2007. [Google Scholar]
- 36.Varshney M, Parel JT, Raizada N, Sarin SK. Initial psychological impact of COVID-19 and its correlates in Indian community: an online (FEEL-COVID) survey. PLoS One. 2020;15 doi: 10.1371/journal.pone.0233874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ali M, Ashan GU, Khan HR, Hossain A. Mental wellbeing in the Bangladeshi healthy population during nationwide lockdown over COVID-19. An online cross-sectional study. medRxiv. 2020 doi: 10.1101/2020.05.14.20102210. published online May 18. (preprint) [DOI] [Google Scholar]
- 38.Islam SMD, Bodrud-Doza M, Khan RM, Haque MA, Mamun MA. Exploring COVID-19 stress and its factors in Bangladesh: a perception-based study. Heliyon. 2020;6 doi: 10.1016/j.heliyon.2020.e04399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pierce M, McManus S, Jessop C. Says who? The significance of sampling in mental health surveys during COVID-19. Lancet Psychiatry. 2020;7:567–568. doi: 10.1016/S2215-0366(20)30237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bruckner M, Mollerus R. UN/DESA Policy Brief number 66: COVID-19 and the least developed countries. 2020. https://www.un.org/development/desa/dpad/publication/un-desa-policy-brief-66-covid-19-and-the-least-developed-countries/
- 41.Arndt C, Davies R, Gabriela S. COVID-19 lockdowns, income distribution, and food security: an analysis for South Africa. Glob Food Secur. 2020;26 doi: 10.1016/j.gfs.2020.100410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anon Tk26.5cr disbursed under social safety net programmes. Dhaka Tribune. June 9, 2020 [Google Scholar]
- 43.WHO Violence and Disasters. 2005. https://www.who.int/violence_injury_prevention/publications/violence/violence_disasters.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.