Highlights
-
•
Peak spread of COVID-19 occurred at an average temperature of 26 °C and a humidity of 55%.
-
•
Highest number of cases were clustered within the average temperature range 26 °C–28 °C and within the humidity range 55%–65%.
-
•
High temperature and high humidity significantly reduce the transmission of COVID-19, respectively.
Keywords: COVID-19, Coronavirus, Temperature, Humidity, Bangladesh
Abstract
This study aimed to determine the association between average temperature and humidity with COVID-19 pandemic in Bangladesh. This study included 9,455 confirmed cases during the observation period (March 08, 2020 to May 03, 2020). The peak spread of COVID-19 occurred at an average temperature of 26 °C. We find, under a linear regression framework, high temperature and high humidity significantly reduce the transmission of COVID-19, respectively. It indicates that the arrival of summer and rainy season in Bangladesh can effectively reduce the transmission of the COVID-19. However, it is unlikely that the COVID-19 pandemic diminishes by summer since Bangladesh still have a high coronavirus transmission. Therefore, other public health interventions such as social distancing are still important for blocking the COVID-19 transmission.
1. Introduction
Coronavirus disease 2019 (COVID-19), caused by the novel coronavirus,1 has become a serious public health problem globally. As of May 03, 2020, more than 3.5 million confirmed cases and over 0.25 million deaths have been reported worldwide.2 COVID-19 is rapidly spreading in many of the western and temperate countries like Italy, France, Germany, Spain, USA, and the UK, where the range of temperature are between 3 °C and 17 °C, most similar to Wuhan China.3 However, the growth rate of conformed cases is apparently slower in Asian tropical countries (such as Indonesia, Malaysia, Vietnam, Singapore, Thailand, etc.,)2 most of which are low- and middle-income countries (LMICs) with weaker detection and response capacity and have not implemented drastic quarantine measures.4 Therefore, the question arises: do warmer and humid weather slow the spread of COVID-19 in tropical countries?
Bangladesh is situated in the tropical monsoon region. Since March 8, 2020, when the first confirmed cases of COVID-19 detected, as of May 03, 2020, 9,455 have tested positive for COVID-19 in this country.5 Going by insights relating to the number of infections, the problem with COVID-19 in Bangladesh sems less severe, despite the size of its population (163 million) and the greater number of cases that other countries are hooking with. Despite the fact that this country has the highest population density and is not capable of doing regular testing, this slower spread of COVID-19, might be an impact of tropical weather (characterized by high temperature, heavy rainfall, often excessive humidity).
Therefore, there has been a lot of debate as to whether warming temperatures with the beginning of spring and summer would lead to reduced transmission in tropical countries like Bangladesh, as is observed for many viral respiratory infections.6 in tropical regions where the vast majority of LMICs are located, this will also have consequences for the risk of spread. Higher temperatures have been demonstrated to be safe against the broadcast of the severe acute respiratory syndrome (SARS) in 2002–2003,7 possibly due to the decreased survival of the SARS-CoV on surfaces at higher temperatures.8 Reduced aerosol spread at higher temperatures is another possible mechanism, as observed for human influenza viruses.9 Also, there is good experimental and epidemiological evidence that patients may have a decline in respiratory function during certain meteorological events.10 , 11
There is also some evidence that COVID-19 cases have particularly clustered around cooler, drier regions.12 , 13 However, there is still a lack of evidence, because some studies found no association of COVID-19 transmission with temperature.14 , 15 This motivated us to start a meteorological investigation to determine the influence of weather on COVID-19 outbreak. This study has investigated the relationship between meteorological factors, especially the average temperature and humidity and the daily number of probable COVID-19 patients in Bangladesh.
2. Methods
2.1. Data sources
Nationwide data on clinically diagnosed COVID-19 cases during the period of March 08 to May 03, 2020, was abstracted from the daily reports of the Institute of Epidemiology, Disease Control and Research (IEDCR), Dhaka, Bangladesh.5 Under IEDCR, 35 laboratories perform COVID-19 testing in all of Bangladesh using rt-PCR based testing. IEDCR tested the first cases on March 04 and found the confirmed patients on 8 Mach 2020. The first COVID-19 death case was identified on March 18, 2020. Because testing strategies could impact the number of reported cases; therefore, the reported number of tests performed daily were also collected from the IEDCR between March 08 to May 03. At the same time, data on daily temperature average (°C) and humidity (%) of Dhaka city were obtained from the Bangladesh Meteorological Department (BMD), Dhaka, Bangladesh.
2.2. Statistical analyses
Descriptive statistics included means ± standard deviations (±SD) for daily confirmed cases, reported number of tests, and meteorological variables were provided. To assess, if an association exist between average temperature and humidity with daily conformed cases of COVID-19, a multiple linear regression model was fitted in the following form: : y= β0+β1Xi1++β2Xi2++β3Xi3 +ε; i = 1.2…..56; in which y is the number of daily confirmed COVID-19 cases, and X1, X2, and X3 are average daily temperature, humidity, and reported number of tests on a daily basis. STATA Version 15.0 (Stata Corp, College Station, TX) was used for all analyses.
3. Results
Table 1 summarizes the descriptive statistics for the daily COVID-19 confirmed cases, reported number of tests, and meteorological variables, respectively. This study included 9,455 confirmed cases during the observation period (March 08, 2020, to May 03, 2020). The average number of daily confirmed cases and the number of tests were168.63 and 1724.40. The metrological data showed the lowest average temperature of 23 °C (with the highest average temperature of 31.5 °C), and the lowest humidity of 48% (with the highest humidity of 81%).
Table 1.
Descriptive statistics of daily confirmed cases, reported number of tests and meteorological variables: March 08 to May 03, 2020.
| Variables | Mean (±SD) | Lowest | Highest |
|---|---|---|---|
| Daily confirmed cases | 168.63 (±215.949) | 0 | 665 |
| Daily reported number of tests | 1724.40 (±1798.79) | 24 | 5,827 |
| Temperature average (°C) | 27.55 (±2.18) | 23 | 31.5 |
| Humidity (%) | 63.70 (±9.12) | 48 | 81 |
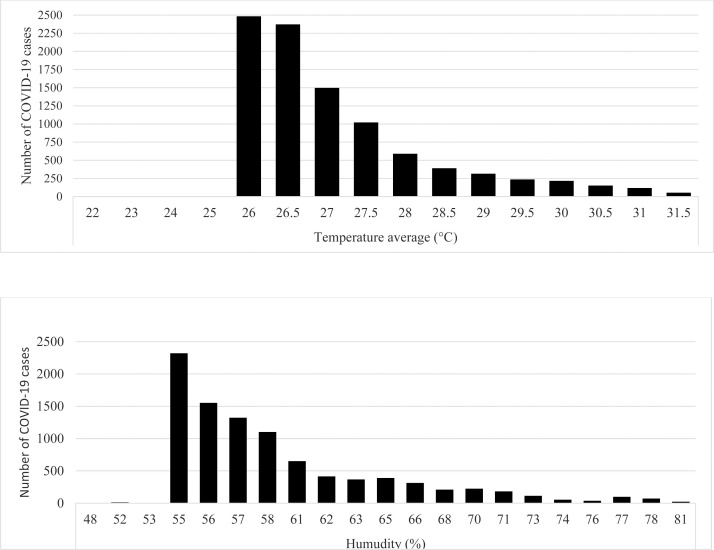
Fig. 1 shows the number of COVID-19 cases by the amount of temperature average (°C) and by the amount of humidity (%). The peak spread of COVID-19 occurred at an average temperature of 26 °C, and a humidity of 55% then gradually decreases as the temperature and humidity rise. Based on tertile splits, the highest number of cases were clustered within the average temperature range 26 °C – 28 °C (84.2%) and within the humidity range 55%-65% (82%).
Fig. 1.
(a) Cases of the COVID-19 by the amount of temperature average (°C), (b) Cases of the COVID-19 by the amount of humidity (%), in Bangladesh from March 08 to May 03, 2020.
Table 2 shows the multiple linear regression model of the association between average temperature and humidity with daily confirmed COVID-19 cases. Significantly, for every unit increase in average temperature and humidity, a -11.76 and -8.79 unit decrease in daily conformed cases is predicted, holding all other variables constant.
Table 2.
Multiple linear regression model of the association between average temperature and humidity with daily confirmed COVID-19 cases: March 08 to May 03, 2020.
| Weather variables | Coefficient of regression (β)1 | SE | t-value | P-value |
|---|---|---|---|---|
| Temperature average (°C) | −11.76 | 5.51 | −2.134 | 0.038 |
| Humidity | −8.79 | 2.98 | −2.95 | 0.005 |
Model was adjusted by reported number of tests.
4. Discussion
In this paper, we find that warm and humid weather may curb the spread of the coronavirus infections (COVID-19). This finding is consistent with the evidence that high temperature and high humidity reduce the transmission of influenza,16 , 17 which can be explained by some possible reasons: First, the influenza virus is more stable at cold temperature, and respiratory droplets stay airborne in dry air longer.18 Second, cold and dry weather also can weaken the immunity of hosts' and make them more vulnerable to the virus.19 Third, higher humidity helps prevent infection in another way by keeping the membranes in the nose and throat moist, which enables them to capture dirt, bacteria, and viruses before they reach the lungs. These mechanisms may also refer to COVID-19 transmission. The findings are also consistent with the evidence that high temperatures and high relative humidity minimizes SARS8 , 13and COVID-1912 , 13 coronavirus viability.
Moreover, more than four-fifths (84.2%) of the total cases were clustered within the average temperature range 26 °C–28 °C so that we can guess that average temperature 26 °C–28 °C may be the optimal temperature for COVID-19 prevalence in Bangladesh. Our findings are in line with a previous study,13 which found that the optimum environmental temperature related to SARS cases was from 16 °C to 28 °C based on data from Hong Kong, Guangzhou, Beijing, and Taiyuan. Another laboratory study found that coronavirus on smooth surfaces was stable for over five days when the temperature at 22 °C – 25 °C, and virus viability was rapidly lost at higher temperatures (e.g., 38 °C).8
However, some limitations should be considered. First, we used the COVID-19 cases for the country as a whole, while weather data from Dhaka District were reported. However, evidence has shown that temperature variation among various districts in Bangladesh exists little. In addition, approximately 73% of confirmed cases were from the district of Dhaka. Therefore, we can assume that it cannot bias our results. Second, although in the multivariate linear regression model, we have adjusted the confounder reported number of tests, however, there are several unknowns including how the virus is mutating and evolving, case fertility ratio, reproductive numbers, and direct versus indirect transmission, population mobility, and population endurance. Future studies are needed to be investigated considering these factors. Third, because there was a lack of patient information. Finally, although the government has established an excellent disease surveillance system, under-reporting may still occur and could affect our main findings, especially at the beginning of the COVID-19 outbreak.
5. Conclusions
Although our paper suggests that, high temperature and relative humidity reduce the transmission of COVID-19, therefore, the arrival of summer and rainy season in Bangladesh can effectively reduce the transmission of the COVID-19; however, it is unlikely that the COVID-19 pandemic diminishes by summer since Bangladesh still have a high coronavirus transmission. Therefore, other public health interventions, such as social distancing are still crucial for blocking COVID-19 transmission. Further laboratory studies are required to determine the underlying mechanisms.
Contribution
SHE and MR: design of the study; MR: Analysis the data; MR: Write the first draft; SHE and MR: Approved and revised the final draft.
Ethical considerations
Because this study uses the public data, therefore, there is no need for informed consent
Funding
None.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgements
We sincerely thanks to Institute of Epidemiology, Disease Control and Research and Meteorological Department of Bangladesh for their assistance on data collection.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.envsci.2020.08.012.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Worldometers, 2020. https://www.worldometers.info/coronavirus/ (Accessed on 23 April 2020).
- 3.Bukhari Q., Jameel Y. 2020. Will coronavirus pandemic diminish by summer? Available at SSRN: https://ssrn.com/abstract=3556998 or https://doi.org/10.2139/ssrn.3556998 Massachusetts Institute of Technology (MIT) [Google Scholar]
- 4.World Health Organization . 2020. Coronavirus disease 2019 (COVID-19) Situation Report - 50. Geneva. [Google Scholar]
- 5.IRDRC; Dhaka: 2020. Institute of Epidemiology, Disease Control and Research. Covid-19 Status Bangladesh. [Google Scholar]
- 6.Imai C., Brooks W.A., Chung Y. Tropical influenza and weather variability among children in an urban low-income population in Bangladesh. Glob Health Action. 2014;7:24413. doi: 10.3402/gha.v7.24413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin K., Fong D.Y.T., Zhu B., Karlberg J. Environmental factors on the SARS epidemic: air temperature, passage of time and multiplicative effect of hospital infection. Epidemiol Infect. 2006;134:223–230. doi: 10.1017/S0950268805005054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan K.H., Peiris J.S.M., Lam S.Y. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv Virol. 2011;2011 doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lowen A.C., Mubareka S., Steel J. Influenza virus transmission is dependent on relative humidity and t emperature. PLOS Pathog. 2007;3 doi: 10.1371/journal.ppat.0030151. e151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marshall R.J., Scraag R., Bourke P. An analysis of the seasonal variation of coronary heart disease and respiratort disease mortality in New Zealand. Int J Epidemiol. 1988;17:325–331. doi: 10.1093/ije/17.2.325. [DOI] [PubMed] [Google Scholar]
- 11.Donaldson G.C., Keatinge W.R. Early increases in ischaemic heart disease mortality dissociated from, and later changes associated with, respiratory mortality, after cold weather in south-east England. J Epidemiol Community Health. 1997;51:643–648. doi: 10.1136/jech.51.6.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang J. High temperature and high humidity reduce the transmission of COVID-19. SSRN Electronic Journal. 2020 doi: 10.2139/ssrn.3551767. [DOI] [Google Scholar]
- 13.Tan J. An initial investigation of the association between the SARS outbreak and weather: with the view of the environmental temperature and its variation. J. Epidemiol. Community Health. 2005;59 doi: 10.1136/jech.2004.020180. 186–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yao Y., Pan J., Liu Z. No association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur Respir J. 2020 doi: 10.1183/13993003.00517-2020. pii: 2000517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shaman J., Kohn M. Absolute humidity modulates influenza survival, transmission, and seasonality. Proc. Natl. Acad. Sci. USA. 2009;106:3243–3248. doi: 10.1073/pnas.0806852106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lowen A.C., Steel J., Mubareka S. High temperature (30oC) blocks aerosol but not contact transmission of influenza virus. J. Virol. 2018;82:5650–5652. doi: 10.1128/JVI.00325-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lowen A.C., Steel J., Mubareka S. Roles of humidity and temperature in shaping influenza seasonality. J. Virol. 2014;88:7692–7695. doi: 10.1128/JVI.03544-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kudo E., Song E., Yockey L.J. Low ambient humidity impairs barrier function and innate resistance against influenza infection. Proc. Natl. Acad. Sci. USA. 2019;116:10905–10910. doi: 10.1073/pnas.1902840116. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.