Abstract
Introduction
Hip dislocation rates in patients with combined total hip arthroplasty (THA) and spinal deformity fixation are significantly higher than those of THA alone. Nevertheless, there are no treatment recommendations for patients who undergo THA and require a spine deformity correction later.
Methods
Twenty-eight patients underwent spinal fixation surgery for adult spinal deformity. Sagittal spinopelvic alignment was analyzed on lateral radiographs taken preoperatively and postoperatively in the sitting and standing positions. Univariate linear regression analysis was conducted to identify the factors affecting the pelvic inclination in the sitting position after spinal fixation. Multiple regression analysis was conducted to determine the most efficient combination of radiographic parameters for predicting postoperative pelvic inclination while sitting.
Results
There were significantly weak associations between postoperative sacral slope (SS) in the sitting position and the following factors: the number of vertebral levels fused (β = 0.30, p = 0.003); the presence of sacral fixation (β = 0.22, p = 0.01); the presence of sacroiliac joint fixation (β = 0.24, p = 0.008); and preoperative SS while standing and sitting (β = 0.21, p = 0.01 and β = 0.34, p = 0.001). Postoperative lumbar lordosis (LL) while standing was strongly associated with postoperative SS in the sitting position (β = 0.67, p <.0001). The combination of postoperative LL in the standing position and preoperative SS in the sitting position was the best fit, and the adjusted R-squared was 0.82.
Conclusions
We devised a prediction formula for pelvic inclination while sitting after spinal fixation that has high predictability: postoperative SS while sitting = 11.7+ (0.4 × postoperative planned LL while standing) + (0.16 × preoperative SS while sitting). This study could be the basis for treatment recommendations for patients who have undergone THA and require a spine deformity correction later.
Keywords: hip-spine syndrome, total hip arthroplasty, dislocation, spinal fixation surgery, postoperative prediction formula
Introduction
Since the concept of hip-spine syndrome was proposed in 19831), it has been our common understanding that hip joint lesions and spinal lesions are related. For severe spinal lesions, spinal fixation and correction of spinal deformities are performed, and for hip osteoarthritis, total hip arthroplasty (THA) is often performed. There have been reports of repeated hip dislocation after spinal surgery2). King et al. surveyed more than 17,000 patients who underwent spinal fusion after THA and reported a significantly increased risk of dislocation compared to that of THA alone3).
Spinal fixation impedes pelvic rollback motion when shifting from the standing to sitting position4). It is thought that, as a result, impingement between the anterior edge of the cup and the femoral stem occurs and causes posterior dislocation2).
Because most of the anterior impingement occurs at the time of posture change from the sitting position, it is important to grasp the pelvic inclination in the sitting position; nevertheless, details regarding pelvic inclination while sitting after spinal fixation in adult spinal deformity (ASD) have not been clarified. Therefore, the purpose of this study was to identify the factors affecting pelvic inclination while sitting after ASD surgery and to determine the goodness of fit of a new formula for predicting postoperative pelvic inclination with preoperative spinopelvic parameters.
Materials and Methods
This study was approved by the institutional review board. In this retrospective study, patients with ASD treated with initial lumbar fixation surgery at our hospital between December 2015 and January 2019 were reviewed. The inclusion criteria were as follows: 1) patients underwent spinal fixation surgery for ASD; 2) complete preoperative and postoperative long-cassette lateral radiographs of the spine and pelvis while sitting and standing; and 3) no evidence of hip or hamstring contractures. Back pain and deformity were major indications for surgery in ASD. Patients with a history of surgery for spinal or pelvic trauma, infections, or tumors were excluded. Patients with histories of previous hip surgeries were also excluded. The contracture of the hamstrings is defined as sensing pain when the leg is at an angle less than 70° in the straight leg raise test. Hip contracture is defined as pain at less than 90° of flexion, 15° or less of abduction, 10° or less of external rotation, or 20° or more of flexion contracture. Informed consent was obtained from all subjects.
Spinal fixation was carried out by the same institutional spine team. Preoperative long-cassette lateral radiographs of the spine and pelvis of the patient's upper limbs on the knees while sitting were obtained. In all cases, these radiographs were re-acquired within 1 year after surgery. The sitting position was an upright posture with the head and trunk vertical on the same stool without a seat back. In this sitting position, the lower legs were bent about 90° at the hips, and knees and feet were on the ground. Long-cassette lateral radiographs of the spine and pelvis in the standing position were obtained with the patient's hands on the clavicles.
To quantify the sagittal spinopelvic alignment in the sitting position, the following radiographic parameters were measured on the lateral radiographs using Centricity Enterprise Web (v3.0; GE Healthcare, Barrington, USA): lumbar lordosis (LL) while standing and sitting; sacral slope (SS) while standing and sitting; and pelvic incidence (PI) while standing. All radiographic data collection was performed by an experienced independent board-certified orthopedic surgeon (D.N., 15 years) who was not involved in the treatment of the patients.
Statistical analysis
All statistical analyses were performed using JMP 14.1 statistical software (SAS Institute Inc., North Carolina, USA). Continuous variables are expressed as mean ± standard deviation. The preoperative and postoperative data were compared using the paired t-test. Univariate linear regression analysis using the ordinary least squares was performed to identify the factors affecting the pelvic inclination in the sitting position after spinal fixation. Multiple regression analysis was performed to determine the most efficient combination of radiographic parameters for predicting postoperative pelvic inclination in the sitting position.
Results
Four male and 24 female ASD patients were included in the study. Their average age was 71.7 years (range 58-82 years). The average number of levels fused was 7.5 segments (3-12).
LL while standing improved significantly from 2.7° ± 20.9° before surgery to 32.9° ± 13.7° after surgery. The mean value of preoperative SS while sitting was 8.5° ± 12.7°, and the postoperative value was 26.3° ± 8.0° after surgery. The baseline demographic characteristics and spinal-pelvic parameters are summarized in Table 1. Univariate analysis with a p-value of less than 0.05 demonstrated no significant relationship between postoperative SS while sitting and the following factors: age, gender, and preoperative LL while standing and sitting (Table 2). A significantly weak association was demonstrated between postoperative SS in the sitting position and the following factors: the number of vertebral levels fused (β = 0.30, p = 0.003); the presence of sacral fixation (β = 0.22, p = 0.01); the presence of sacroiliac joint fixation (β = 0.24, p = 0.008); and preoperative SS while standing and sitting (β = 0.21, p = 0.01 and β = 0.34, p = 0.001). Preoperative PI while standing was associated moderately with postoperative SS in the sitting position (β = 0.55, p <.0001). Postoperative LL while standing was strongly associated with postoperative SS in the sitting position (β = 0.67, p <.0001).
Table 1.
Baseline Demographic Characteristics and Spinal-Pelvic Parameters.
| Mean | SD | Max | Min | |
|---|---|---|---|---|
| Sex (M:F) | 4:24 | |||
| Age | 71.7 | 6.5 | 82 | 58 |
| Number of levels fused | 7.5 | 3.2 | 12 | 3 |
| Presence of sacral fixation (%) | 67.9 | |||
| Presence of sacroiliac joint fixation (%) | 50.0 | |||
| Preoperative LL while standing | 2.7 | 20.9 | 35 | −30 |
| Postoperative LL while standing | 32.9 | 13.7 | 64 | 4 |
| Preoperative SS while sitting | 8.5 | 12.7 | 31 | −17 |
| Preoperative PI-LL | 48.3 | 18.7 | 96.8 | 16 |
| Postoperative PI-LL | 18.0 | 13.2 | 41 | −16 |
SD: standard deviation; Max: maximum; Min: minimum; LL: lumbar lordosis; SS: sacral slope; PI: pelvic incidence
Table 2.
Univariate Analysis for Postoperative SS while Sitting.
| Variable | β | P-value |
|---|---|---|
| Age | 0.12 | 0.08 |
| Sex | 0.03 | 0.41 |
| Number of vertebral levels fused | 0.30 | 0.003 |
| Presence of sacral fixation | 0.22 | 0.01 |
| Presence of sacroiliac joint fixation | 0.24 | 0.008 |
| Preoperative LL while standing | 0.08 | 0.14 |
| Preoperative LL while sitting | 0.07 | 0.18 |
| Preoperative SS while standing | 0.21 | 0.01 |
| Preoperative SS while sitting | 0.34 | 0.001 |
| Preoperative PI while standing | 0.55 | <0.0001 |
| Postoperative LL while standing | 0.67 | <0.0001 |
β: standardized beta coefficient; LL: lumbar lordosis; SS: sacral slope; PI: pelvic incidence
Of these radiographic parameters, only postoperative LL while standing is a parameter for which spinal surgeons can intervene. Under conditions including postoperative LL while standing, combinations with these significant factors for predicting postoperative SS in the sitting position were examined using multiple regression analysis (Table 3). The combination of postoperative LL in the standing position and preoperative SS while sitting was the best fit, and their adjusted R-squared indicating how well the formula fits was 0.82. On the basis of the regression formula, we created the following prediction formula:
Table 3.
Fitting of Combinations with Postoperative LL in Standing Using Multiple Regression Analysis for Predicting Postoperative SS while Sitting.
| Variable | Adjusted R-square |
P-value |
|---|---|---|
| Number of vertebral levels fused | −0.07 | 0.90 |
| Presence of sacral fixation | 0.003 | 0.37 |
| Presence of sacroiliac joint fixation | 0.04 | 0.22 |
| Preoperative SS while standing | 0.36 | 0.0016 |
| Preoperative SS while sitting | 0.82 | <0.0001 |
| Preoperative PI while standing | −0.09 | 0.94 |
LL: lumbar lordosis; SS: sacral slope; PI: pelvic incidence
Postoperative SS while sitting = 11.7+ (0.4 × postoperative planned LL while standing) + (0.16 × preoperative SS while sitting). The achievement rate within a targeted error range between the predicted value and the measured value was 46.4% within 3° error, 71.4% within 5° error, and 96.4% within 7° error.
Discussion
We devised a prediction formula for pelvic inclination while sitting after spinal fixation that has high predictability. Details regarding pelvic inclination while sitting after spinal fixation in ASD were clarified for the first time.
In recent years, an increasing number of patients undergoing both spinal fusion and hip arthroplasty have been reported. Malkani et al. reported a 293% increase in the number of patients with lumbar spinal fusion (LSF) undergoing THA between 2002 and 2014. The sequence of surgical intervention for concomitant lumbar and hip pathology requiring LSF and THA, respectively, significantly impacts the fate of the THA performed5). A survey including more than 17,000 patients who underwent spinal fusion after THA reported a significantly increased risk of dislocation compared to that of THA alone3).
Most of the anterior impingement occurs in the sitting position. In fact, hip precautions prescribed to prevent hip dislocation emphasize the sitting position6,7). Hip precautions encourage patients to avoid bending the hip past 90°, twisting their leg in or out, and crossing their legs. Patients are also encouraged to sit with their hips higher than their knees. Hip precautions may also include avoiding riding in a car or sitting in any low seat.
After spinal fixation, pelvic rollback motion while sitting is prevented, and spinopelvic motion is compensated by hip joint alone. Therefore, it is more important to attain pelvic inclination in the sitting position. Postoperative changes in sagittal spinopelvic alignment in the sitting position was reported in adolescents with idiopathic thoracic scoliosis8). However, there is no such report after spinal fixation in ASD.
Sultan et al. presented an algorithm regarding how to surgically address patients who simultaneously require THA and ASD correction9). In their straightforward algorithm, surgical management is prioritized according to the more symptomatic region.
For patients who had a spine deformity corrected and then required a THA later, Phan et al. proposed treatment recommendations on the basis of spinal flexibility and balance for ideal cup positioning10). Nevertheless, for patients who had a THA and require a spine deformity correction later, there are no treatment recommendations.
Malkani et al. found that patients with prior LSF undergoing THA are at significantly higher risk of dislocation and subsequent revision compared with those with THA first followed by delayed LSF5). This suggests that there is a possibility that the number of patients with THA first followed by later LSF would increase in the future. There is a growing need to provide treatment recommendations for these patients. This study could be the basis for such recommendations.
This study has made it possible to predict the postoperative SS while sitting when LSF is performed on the basis of a target value such as PI-LL < 10°. By combining the results of this study and a three-dimensional (3D) range of motion (ROM) simulation system, it becomes possible to simulate flexion in the sitting position. The 3D ROM simulation enables precise detection of impingement and indicates each angle in three directions. Fig. 1 is an example of the 3D ROM simulation, in which the flexion angle decreases with correction of pelvic inclination. Nevertheless, this is insufficient for an accurate evaluation of the risk of THA dislocation for ASD patients with LSF.
Figure 1.
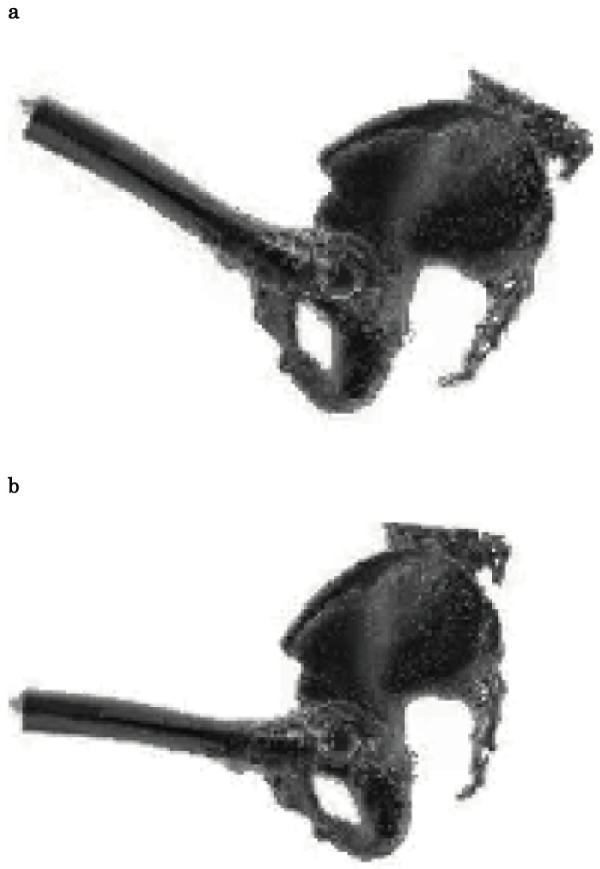
Three-dimensional ROM simulation [ZedHip® software (LEXI Co., Ltd., Tokyo, Japan) ]. SS while sitting was 16°. Anterior impingement occurred in the left hip joint at 122° flexion, 10° adduction, and 10° internal rotation (a). Postoperative SS while sitting was predicted to be 41°. Anterior impingement occurred at 100° flexion, 10° adduction, and 10° internal rotation at that time (b).
While studying 3D joint kinematics during activities of daily living (squatting, kneeling, and sitting cross-legged), the ranges of hip motion required to perform these activities in healthy subjects were revealed11,12). Nevertheless, the range of hip motion required in patients undergoing LSF remains unknown. Once this becomes clear, we can understand the risk of THA dislocation in daily activities for patients with LSF. This would lead to the identification of correct target values of LL that should be recommended as well as the necessity of cup revision.
There are several limitations to this study. First, this was a single-center study and therefore may be subject to selection bias. For this reason, we instituted strict inclusion and exclusion criteria. Multi-center studies are needed to validate our findings. Second, the sitting posture with the trunk vertical used at the time of radiographs requires an effort to maintain a neutral sitting position. This posture may be very different from the comfortable sitting posture with only a minimal trunk muscular effort used in daily life.
In conclusion, the prediction formula for pelvic inclination in the sitting position after spinal fixation devised in this study has high predictability and should be considered useful. The prediction formula is as follows: postoperative SS while sitting = 11.7 + (0.4 × postoperative planned LL while standing) + (0.16 × preoperative SS while sitting).
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Author Contributions: Daisuke Nishiyama designed the study and wrote the initial draft of the manuscript. Takuhei Kozaki contributed to analysis and interpretation of data and assisted in the preparation of the manuscript. All other authors have contributed to data collection and interpretation and critically reviewed the manuscript. All authors read and approved the final manuscript.
Informed Consent: Informed consent was obtained by all participants in this study.
Acknowledgement
We would like to thank Editage (www.editage.com) for English language editing.
References
- 1.Offierski CM, MacNab I. Hip-spine syndrome. Spine. 1983;8(3):316-21. [DOI] [PubMed] [Google Scholar]
- 2.Furuhashi H, Togawa D, Koyama H, et al. Repeated posterior dislocation of total hip arthroplasty after spinal corrective long fusion with pelvic fixation. Eur Spine J. 2017;26(Suppl 1):100-6. [DOI] [PubMed] [Google Scholar]
- 3.King CA, Landy DC, Martell JM, et al. Time to dislocation analysis of lumbar spine fusion following total hip arthroplasty: Breaking up a happy home. J Arthroplasty. 2018;33(12):3768-72. [DOI] [PubMed] [Google Scholar]
- 4.Lazennec JY, Brusson A, Rousseau MA. Hip-spine relations and sagittal balance clinical consequences. Eur Spine J. 2011;20 Suppl 5:686-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malkani AL, Himschoot KJ, Ong KL, et al. Does timing of primary total hip arthroplasty prior to or after lumbar spine fusion have an effect on dislocation and revision rates? J Arthroplasty. 2019;34(5):907-11. [DOI] [PubMed] [Google Scholar]
- 6.Barnsley L, Barnsley L, Page R. Are hip precautions necessary post total hip arthroplasty? A systematic review. Geriatr Orthop Surg Rehabil. 2015;6(3):230-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tran P, Fraval A. Total hip replacement. Recovery and rehabilitation: Western Health; 2013 [cited 2019 Nov 29]. Available from: http://www.orthoanswer.org/hip/total-hip-replacement/recovery.html.
- 8.Zhu W, Liu Z, Sha S, et al. Postoperative changes in sagittal spinopelvic alignment in sitting position in adolescents with idiopathic thoracic scoliosis treated with posterior fusion: an initial analysis. J Neurosurg Pediatr. 2018;22(1):74-80. [DOI] [PubMed] [Google Scholar]
- 9.Sultan AA, Khlopas A, Piuzzi NS, et al. The impact of spino-pelvic alignment on total hip arthroplasty outcomes: a critical analysis of current evidence. J Arthroplasty. 2018;33(5):1606-16. [DOI] [PubMed] [Google Scholar]
- 10.Phan D, Bederman SS, Schwarzkopf R. The influence of sagittal spinal deformity on anteversion of the acetabular component in total hip arthroplasty. Bone Joint J. 2015;97-B(8):1017-23. [DOI] [PubMed] [Google Scholar]
- 11.Hemmerich A, Brown H, Smith S, et al. Hip, knee, and ankle kinematics of high range of motion activities of daily living. J Orthop Res. 2006;24(4):770-81. [DOI] [PubMed] [Google Scholar]
- 12.Zhou H, Liu A, Wang D, et al. Kinematics of lower limbs of healthy Chinese people sitting cross-legged. Prosthet Orthot Int. 2013;37(5):369-74. [DOI] [PubMed] [Google Scholar]


