Abstract
Introduction
We have developed the single or double endplates penetrating screw (SEPS/DEPS) technique, which is a novel percutaneous pedicle screw (PPS) insertion technique suitable for osteoporotic vertebral body fracture (OVF) patients with diffuse idiopathic skeletal hyperostosis (DISH). This study aims to compare the effectiveness of this SEPS/DEPS technique with the conventional pedicle screw technique.
Methods
The screw is inserted upward from the outer caudal side of the pedicle toward the inner cranial side. Vertebrae affected with DISH were inserted with screws using the SEPS/DEPS technique, whereas non-fused vertebrae were inserted with screws using the conventional PPS technique. Twelve OVF patients with DISH were included in this study; three with SEPS/DEPS technique only and nine with a hybrid of both the DEPS and the conventional PPS techniques. As a control group, 12 OVF patients with DISH treated by conventional PPS. The rates of implant failures and of surgical complications were compared between the SEPS/DEPS group and the control group. The insertion torque was measured and compared between DEPS and conventional PPS in three hybrid patients.
Results
In the SEPS/DEPS group, 70 screws were inserted with the SEPS/DEPS technique and 56 screws were inserted with the conventional PPS technique. In the control group, 116 screws were inserted using the conventional PPS and the PS techniques. The loosening of screws was significantly less in screws inserted with the SEPS/DEPS technique (0/70 screws, 0%) than with screws inserted with the conventional technique (12/116 screws, 10.3%). The average insertion torque of DEPS was 2.25 Nm, which was 134% higher than that of conventional PPS which was 1.64 Nm (p = 0.04).
Conclusions
This novel SEPS/DEPS technique has a higher insertion torque compared with the conventional PPS techniques and demonstrated itself to be an effective option for patients with concomitant bone fragility due to DISH.
Keywords: osteoporotic vertebral body fracture (OVF), diffuse idiopathic skeletal hyperostosis (DISH), percutaneous pedicle screw (PPS), minimally invasive spine stabilization (MISt), single endplate penetrating screw (SEPS) technique, double endplates penetrating screw (DEPS) technique
Introduction
In patients with diffuse idiopathic skeletal hyperostosis (DISH), vertebral instability caused by pseudoarthrosis after osteoporotic vertebral body fracture (OVF) may be difficult to heal because of the long lever arms at the cranial and caudal sides of the affected vertebra. Moreover, the complication and mortality rates after spinal fracture in patients with DISH are significantly higher than in patients with a normal spine1). Therefore, surgical treatment is necessary for these patients. Among various spinal fixation methods, minimally invasive spine stabilization using a percutaneous pedicle screw (PPS) is often used because of less surgical invasion and lower complication rates than using conventional open procedures2-4). However, rigid fixation is not easily accomplished because of concomitant bone fragility. As the mobility of vertebral body diminishes in DISH, its bone mineral density may decrease because of stress shielding, which results in a higher risk of vertebral fracture. We have developed the single or double endplates penetrating screw (SEPS/DEPS) technique, which is a novel PPS insertion technique, and have utilized it for patients with DISH. This study aims to introduce this novel SEPS/DEPS technique and to evaluate its effectiveness for DISH patients by comparing it with the conventional PPS technique.
Material and Methods
SEPS/DEPS technique
The SEPS or DEPS technique is a modification of the penetrating S1 endplate screw (PES) technique reported by Matsukawa et al.7). The screw is inserted upward from the outer caudal side of the pedicle toward the inner cranial side (Fig. 1). The skin incision should be made 20 mm caudal to that of the conventional PPS position and should be made vertically to facilitate the adjustment of the sagittal probe angle. The probe is inserted from 7:00 toward 1:00 for the left pedicle and from 5:00 toward 11:00 for the right pedicle. The tip of the probe should reach to the upper endplate in the lateral view before touching the inner edge of the pedicle in the A-P view. The probe should penetrate the upper endplate of the vertebral body and the lower endplate of the adjacent cranial vertebral body. As it might be difficult to penetrate double endplates because of the sagittal pedicle angle at lumbar spine level, only a single endplate is penetrated and this is referred to as the single endplate penetrating screw (SEPS) technique. A guidewire is then inserted, followed by a pedicle screw as in the conventional PPS technique (Fig. 2). We often use 50-55 mm-long screws for female patients and 55-60 mm-long screws for male patients, depending on the preoperative measurements based on the reconstructed sagittal CT view.
Figure 1.
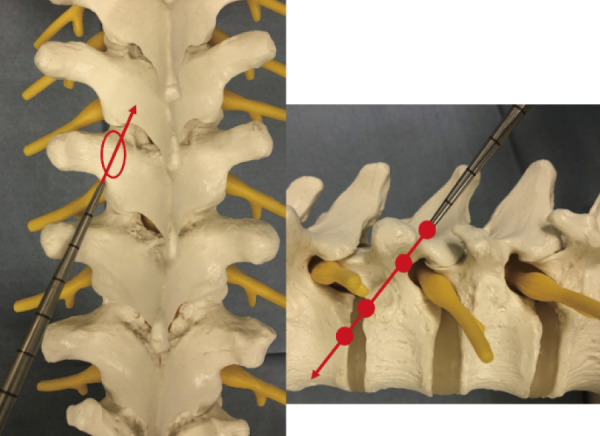
Trajectory of DEPS technique.
oval; pedicle
filled circle; strong fixation point
arrow; direction of insertion
The screw is inserted upward from the outer caudal side of the pedicle toward the inner cranial side.
Figure 2.

Intraoperative fluoroscopy. A-P view (Left), Lateral view (Right).
1; Left pedicle; insert the probe; 7:00→1:00 direction
Right pedicle; insert the probe; 5:00→11:00 direction
2; The tip of probe should reach to the upper endplate in the lateral view before touching the inner edge of the pedicle in the A-P view.
3, 4; Penetrate the lower endplate of the cranial adjacent vertebral body.
5; Insert the guidewire.
6; Insert the pedicle screw in the same way as in conventional PPS.
As the double endplates penetrating screws extend to the adjacent vertebral body, this technique was applied only to vertebral bodies, which had fused due to DISH, whereas the conventional PPS technique was applied to unfused vertebral bodies to maintain mobility.
For patients with DISH in both cranial and caudal vertebrae, the DEPS technique was applied to both sides. However, for patients with DISH in only cranial vertebra, the DEPS technique was applied only to cranial vertebra, and, at the same time, the conventional PPS technique was applied to caudal vertebra (Hybrid technique) (Fig. 3).
Figure 3.

Our treatment strategy of vertebral fracture.
1; Patients with DISH at both cranial and caudal vertebrae; SEPS or DEPS technique to cranial and caudal vertebrae (all SEPS or DEPS technique).
2; Patients with DISH at only cranial vertebrae; DEPS technique to cranial vertebrae and conventional PPS to caudal vertebrae (Hybrid technique).
Materials
In the first study, we retrospectively evaluated the patients who underwent surgery for DISH-related OVF. DISH was defined as ossification along the anterolateral aspect of at least four contiguous vertebral bodies8). Twelve patients with DISH-related OVF who were treated using the SEPS/DEPS technique were included (four males and eight females). The average age was 83.3 years (61 to 94 years old), and the average follow-up period was 22.3 months (9 to 30 months) (Table 1). For the control group, 12 patients with DISH-related OVF treated by conventional PPS (seven patients) and pedicle screw (PS) (five patients) were used (eight males and four females). The average age was 78.0 years (75 to 92 years old), and the average follow-up period was 27.8 months (8 to 72 months) (Table 2). Radiological parameters including the level of affected vertebral body, the range of DISH, the number of instrumented segments, the grade of SEPS/DEPS perforation, and the implant failure rate were evaluated. Screw perforation was graded using Raley's grade, Grade 0: screw within the cortex of the pedicle; Grade 1: perforation ≦2 mm; Grade 2: perforation >2 mm, complication (−); and Grade 3: perforation >2 mm, complication (+)9). The rate of implant failure was compared between the SEPS/DEPS technique group and the control group using the χ2 test.
Table 1.
Patients Demographics in SEPS/DEPS Technique Group.
| Case | Sex Age (years) | Affected vertebrae | DISH range | Hybrid or All S/DEPS | Number of instrumented segments | Instrumented vertebrae | Applied S/DEPS technique | Applied Conventional PPS technique | S/DEPS screw perforation | Implant failure/ revision surgery | Follow up Period (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M 92 |
L1 | T8-L1 | Hybrid | 5 | T10-L3 | T12 DEPS | T10 11 L1 2 3 |
Grade0 | none | 30 |
| 2 | F 81 |
T11 | C6-L1 | Hybrid | 6 | T8-L2 | L1 DEPS | T8 9 10 12 L2 |
Grade0 | none | 29 |
| 3 | F 94 |
T12 | T8-T12 | Hybrid | 4 | T10-L2 | T10 11 DEPS | T12 L1 2 |
Grade0 | none | 26 |
| 4 | F 61 |
L1 | T3-L1 | Hybrid | 5 | T10-L3 | T11 12 DEPS | T10 L2 3 |
Grade0 | L2 3 loosening removal | 27 |
| 5 | F 89 |
L1 | T3-L1 | Hybrid | 5 | T11-L3 | T11 12 DEPS | L1 2 3 | Grade1×1 | none | 24 |
| 6 | F 81 |
T11 | T7-11 | Hybrid | 4 | T9-L1 | T9 10 DEPS | T11 12 L1 |
Grade0 | none | 23 |
| 7 | F 91 |
L1 | T3-S1 | All S/DEPS | 6 | T10-L4 | T10 11 12 DEPS L2 3 4 SEPS | none | Grade0 | none | 23 |
| 8 | M 90 |
T12 | T2-12 | Hybrid | 4 | T10-L2 | T10 11 DEPS | T12 L1 2 |
Grade0 | L2 back out removal | 17 |
| 9 | F 69 |
L1 | T5-L4 | Hybrid | 6 | T10-L4 | T10 11 12 DEPS L3 4 SEPS |
L2 | Grade0 | none | 22 |
| 10 | M 81 |
L1 | T5-S1 | All S/DEPS | 5 | T11-L3 | T11 12 DEPS L2 3 SEPS |
none | Grade1×2 | none | 15 |
| 11 | M 85 |
L1 | T4-T12 | Hybrid | 5 | T11-L3 | T11 12 DEPS | L2 3 | Grade0 | none | 9 |
| 12 | F 85 |
T12 | T5-L4 | All S/DEPS | 6 | T9-L3 | T9 10 11 DEPS L1 2 3 SEPS |
none | Grade1×1 | none | 12 |
| average | 83.3 | 5.1 | 22.3 |
Table 2.
Patients Demographics in Control Group.
| Case | Sex Age (years) | Affected vertebrae | DISH range | Number of instrumented segments | Instrumented vertebrae | PPS/open technique | Implant failure/ revision surgery |
Follow up Period (months) |
|---|---|---|---|---|---|---|---|---|
| 1 | F 76 |
T12 | T5-L2 | 3 | Th10-L1 | PPS | L1 back out | 52 |
| 2 | F 81 |
T11 | T5-11 | 3 | Th9-12 | PPS | none | 24 |
| 3 | M 77 |
T12 | T8-L2 | 4 | Th10-L2 | PPS | none | 30 |
| 4 | M 75 |
T11 12 | T5-L5 | 7 | Th8-L3 | PPS | none | 31 |
| 5 | M 78 |
T11 | T3-L5 | 6 | T8-L2 | open | none | 9 |
| 6 | M 65 |
T7 8 | T6-L1 | 5 | T5-10 | open | none | 24 |
| 7 | F 84 |
T11 | T3-L3 | 6 | T8-L2 | PPS | none | 8 |
| 8 | M 92 |
T11 L1 2 | T5-T12 | 6 | T9-L3 | PPS | T9 10 11 loosening removal | 11 |
| 9 | M 75 |
L1 | T8-L1 | 4 | T11-L3 | PPS | none | 12 |
| 10 | M 75 |
T12 | T7-T12 | 4 | T10-L2 | open | L2 loosening | 12 |
| 11 | M 75 |
T12 | T7-T12 | 4 | T10-L2 | open | L2 loosening | 48 |
| 12 | F 83 |
T11 | T5-L4 | 4 | T9-L1 | open | none | 72 |
| average | 78 | 4.7 | 27.8 |
In the second study, we prospectively measured the insertion torque in three patients to whom the Hybrid technique had been applied, and it was compared between that of the DEPS technique and that of the conventional PPS technique using the Mann-Whitney U test (Table 3).
Table 3.
Demographics of Hybrid Technique Patients with the Insertion Torque Measurement.
| Case | Sex Age (years) | Diagnosis | Affected vertebrae | DISH range | Instrumented vertebrae | Applied DEPS technique | Applied Conventional PPS technique |
|---|---|---|---|---|---|---|---|
| 1 | M 90 |
osteoporotic vertebral body fracture | T12 | T2-12 | T10-L2 | T10 11 | T12 L1 2 |
| 2 | F 69 |
osteoporotic vertebral body fracture | L1 | T5-L4 | T10-L4 | T10 11 12 L3 4 | L2 |
| 3 | M 75 |
pyogenic spondylitis | L1 2 | T4-L1 | T11-L4 | T11 12 | L3 4 |
The insertion torque was measured with a screwdriver connected with a torque meter (HTG2-5N, Imada) during screw insertion. All screws showed a steady increase in torque toward the end of the insertion, and the maximum insertion torque was measured in the last phase7).
Results
In the first study, the affected vertebral bodies in the SEPS/DEPS technique group were at T11 in two patients, T12 in three patients, and L1 in seven patients. DISH was extended from the cervical spine to the lumbar spine in all the patients. The number of instrumented segments was 5.1 (4-6) in the SEPS/DEPS technique group (Table 1). In the control group, the affected vertebral bodies were at T11 in four patients, T12 in four patients, L1 in one patient, both T7 and T8 in one patient, both T11 and T12 in one patient, and T11, L1, and L2 in one patient. DISH was extended from the thoracic spine to the lumbar spine in all the patients. The number of instrumented segments was 4.7 (3-7) (Table 2).
Screws were inserted into two or three vertebral bodies both at the cranial and caudal sides using either method because the affected vertebra was severely unstable due to long lever arm associated with DISH. Seventy screws were inserted using the SEPS/DEPS technique, and 116 screws were inserted using the conventional PPS and PS techniques in the control group. There were four screws with Grade1 perforation in the SEPS/DEPS technique group (Table 1). No perioperative complications related to the surgery were observed in either group.
No screw loosening was observed in the SEPS/DEPS technique group (0%), whereas 12 screws loosened in the control group (10.3%), which showed a statistically significant difference (p = 0.005) (Table 4). Revision surgery was required because of screw loosening in three patients: two patients with conventional PPS in the SEPS/DEPS technique group (Hybrid technique) and one patient in the control group. No revision surgery was required in the SEPS/ DEPS technique group. Two patients required removal of a part of PPS, and the other patient required removal of all PPS and had Balloon Kyphoplasty performed to the distal adjacent segmental fracture (Table 1, 2).
Table 4.
Comparison of Implant Failure Rate between SEPS/DEPS Group and Control Group.
| SEPS and DEPS technique group |
Control group |
|
|---|---|---|
| Implant failure (+) | 0 | 12 |
| Implant failure (−) | 70 | 104 |
In the second study, the insertion torque was measured in 28 screws: 18 screws with the DEPS technique and 10 screws with the conventional PPS technique (Table 4). The diameter of PSs in DEPS was 5.5 mm in six screws and 6.5 mm in 12 screws, whereas the diameter was 7.5 mm in all screws using the PPS technique. The average insertion torque of the DEPS technique was 2.25 Nm, and that of the conventional PPS technique was 1.64 Nm (p = 0.04). Therefore, the DEPS technique achieved a 134% higher average insertion torque than using the conventional PPS technique (Fig. 4).
Figure 4.
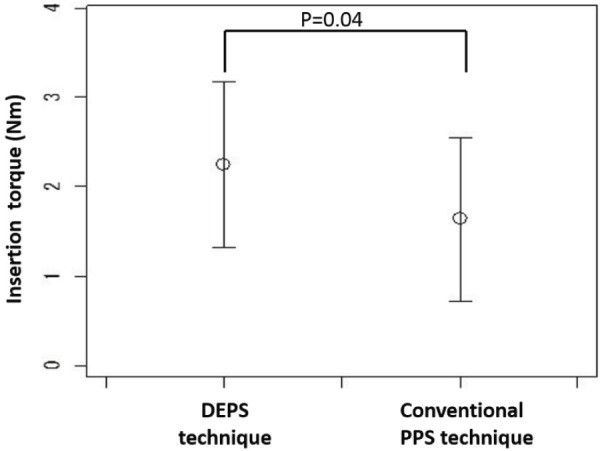
Comparison of insertion torque (DEPS technique vs. Conventional PPS technique).
The DEPS technique had a 134% higher average insertion torque than the conventional PPS technique (p=0.04).
Illustrative case (case 15)
An 85 year-old female was admitted to our hospital because of severe back pain and lower extremity paralysis after the failure of conservative treatment at a nearby hospital. Radiography showed a compression fracture at T12 and an ankylosed spine from the upper thoracic spine to L4. CT and MRI revealed that the fracture at T12 was a reverse Chance-type fracture. Posterior fusion was performed using the DEPS technique at T9, T10, and T11 and using the SEPS technique at L1, L2, and L3. She was able to sit up a few days afterward, and bony union was verified 3 months after the surgery (Fig. 5).
Figure 5.

①; Lateral radiograph of the spine showing the T12 fracture and ankylosed spine.
②, ③; Sagittal view of CT imaging showing the ankylosed spine from the upper thoracic spine to L4 and reverse Chance-type fracture at T12.
④; Sagittal view of MRI (T2) showing the diffuse high signal intensity area in T12, L1 vertebral body and posterior element of T12.
⑤; Coronal and lateral radiograph after the surgery. DEPS technique was applied to T9, T10, T11, and SEPS technique was applied to L 1, L2, and L3.
⑥, ⑦; Sagittal and 3-D reconstructed CT imaging after the surgery.
Discussion
DISH is a non-inflammatory disease whereby the spinal longitudinal ligaments and entheses become ossified over time resulting in the decreased mobility of the affected segment10). The diagnosis can be made when flowing ossification of the anterior longitudinal ligament is present on spine radiographs over at least four consecutive levels8). This condition is associated with osteoporosis as a result of chronic inflammation and disuse atrophy11). In DISH patients, minor trauma can cause serious spinal fractures that carry a high risk of delayed and surgical complications. As with fracture in long bone, the long lever arm formed by the ossified spine increases the mechanical stress at the fracture1,5,6). Paxisons et al. reported that bone quality is an important factor that influences the stability of posterior thoracic implant and that fixation strength in osteoporotic patients was only one-fourth of the value measured in vertebrae with good bone quality12). Caron et al. evaluated the surgical results of spine fracture in patients with ankylosing spinal disorders and suggested that posterior segmental fixation extending a minimum of three levels above and below the injured vertebra resulted in reliable fracture healing13). These studies suggest that it is difficult to obtain rigid fixation to osteoporotic bone and to determine the appropriate fixation method in DISH patients.
To resolve these issues, we have developed the SEPS/DEPS technique, which is a novel PPS insertion technique suitable for patients with DISH.
The DEPS technique is a modification of the PES technique reported by Matsukawa et al. The PES technique was demonstrated to have a 141% higher average insertion torque than the traditional technique and the endplate offered the best screw fixation, which was confirmed by the higher insertion torque despite the shorter screw length7).
The screw used in the DEPS technique is a type of transvertebral screw that was first reported by Abdu et al. for high-grade spondylolisthesis in adults14). Minamide et al. reported the biomechanical results of transdiscal L5-S1 screws for the fixation of isthmic spondylolisthesis. They reported that transdiscal L5-S1 fixation produced a 1.6-1.8 times stiffer construct than traditional PS fixation in a cadaveric model of simulated L5-S1 spondylolisthesis15). Several other studies have reported on screws that penetrate the adjacent vertebra. Nottmeier et al. reported on the transvertebral PS placement in the thoracic spine with the aid of 3-D image guidance16). Rodriguez-Martinez et al. reported the biomechanical results of transvertebral screw fixation for thoracic spine. They reported that transvertebral screw fixation had good fixation force similar to the traditional PS fixation, and it can be a viable therapeutic option for fixation in a salvage procedure, if PS insertion is not possible17). Sandquist et al. reported on the multilevel stabilization screw technique for decreasing the incidence of proximal junctional failure in long segmental instrumented fusions for adult degenerative scoliosis18). These reports suggested that transvertebral screws are a useful device to obtain favorable surgical outcomes. As a result, we have developed this unique SEPS/DEPS technique designed particularly for DISH patients. Another advantage of this innovative technique in comparison with previous conventional techniques is that SEPS/DEPS is a percutaneous method and utilizes fluoroscopy, not 3-D image guidance. Therefore, this technique is less invasive and can be performed at medium-sized hospitals that do not have 3-D image guidance. Our comparative study between the SEPS/DEPS technique group and the control group demonstrated a more successful radiological outcome with a lower implant failure rate in the SEPS/DEPS technique group. Okada et al. have reported on screw loosening in conventional PPS for vertebral fractures associated with DISH. Although no screw loosening was observed postoperatively, there was 12.5% of screw loosening intraoperatively3). In our study, no screw loosening intraoperatively and postoperatively was observed using the SEPS/DEPS technique. Furthermore, the safety of this method was confirmed by the absence of critical screw perforation or complications related to SEPS/DEPS insertion. Revision surgery was required in two patients in the SEPS/DEPS technique group, but these were due to screws inserted using the conventional PPS method in the Hybrid technique, and none was required in the SEPS/DEPS technique group.
To obtain more accurate comparisons, we measured and evaluated the insertional torque of two different methods applied to three patients who had been treated with both DEPS and conventional PPS (Hybrid technique). The DEPS technique showed a 134% higher average insertion torque in spite of the smaller diameter of the screw than with the conventional PPS technique. There are several potential reasons for the higher insertion torque in DEPS. Firstly, based on the idea that the PES technique was demonstrated to have a 141% higher average insertion torque than the traditional technique, the screws used in the DEPS technique penetrated double endplates in a similar way as in the PES technique7). Secondly, the trajectory of DEPS technique screws passes the caudal half of the pedicle, which has the highest bone density in the pedicle and has a 44% higher load to failure during PS compression testing19) (Fig. 1). We believe that these reasons for the higher insertion torque explain the lower implant failure rate using the DEPS technique compared with using conventional PPS.
One of the limitations of DEPS is that this technique might be slightly difficult to apply at lumbar spine level. The sagittal pedicle angle (measured between the superior endplate of the vertebral body and a line extending down the axis of the pedicle) is greater in the thoracic spine than in the lumbar spine20). Accordingly, in DEPS, the thoracic spine has a greater chance of being able to engage the superior endplate. In contrast, the sagittal pedicle angle is nearly zero in the mid lumbar spine and can be negative in the lower lumbar spine20), which makes it more difficult to engage the superior endplate in the lumbar spine using the DEPS technique. Even if the screw could penetrate only a single endplate (SEPS technique), we consider that it could obtain a stronger fixation than using the conventional PPS technique and is comparable with using the PES technique.
It should be noted that there are some other limitations in this study. Firstly, the level of affected vertebra varied among the patients who underwent the SEPS/DEPS technique. Secondly, the control group included patients who had been treated not only with the conventional PPS technique but also with the open PS technique, and, therefore, it may be difficult to draw a precise direct comparison between the two techniques. Lastly, as the insertion torque was measured in only three patients, it may not be sufficient to draw definite conclusions. However, torque measurement was seen as a useful tool in assessing the stability of screw insertion.
Conclusion
We have demonstrated that this novel technique has a stronger insertion torque and fixation compared with the conventional PPS and PS techniques. The number of OVF patients with DISH will likely increase in the future and that combined Hybrid and SEPS/DEPS technique treatment will also become more accepted, and this study has demonstrated the efficacy and viability of this innovative approach. Further studies focusing on the biomechanical aspect of our SEPS/DEPS technique are required to validate our clinical results.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Author Contributions: Study conception and design; Takumi Takeuchi, Keitaro Matsukawa, Naobumi Hosogane
Acquisition of data; Takumi Takeuchi, Kenichiro Yamagishi
Analysis and interpretation of data; Takumi Takeuchi
Drafting of manuscript; Takumi Takeuchi
Critical revision; Naobumi Hosogane, Kazuhiko Satomi, Shoichi Ichimura
Informed Consent: Informed consent was obtained from all participants in this study.
References
- 1.Westerveld LA, Bemmel JC, Dhert WJA, et al. Clinical outcome after traumatic spinal fractures in patients with ankylosing spinal disorders compared with control patients. Spine J. 2014;14(5):729-40. [DOI] [PubMed] [Google Scholar]
- 2.Brooks F, Rackham M, Williams B, et al. Minimally invasive stabilization of the fractured ankylosed spine: a comparative case series study. J Spine Surg. 2018;4(2):168-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Okada E, Shiono Y, Nishida M, et al. Spinal fractures in diffuse idiopathic skeletal hyperostosis: Advantages of percutaneous pedicle screw fixation. J Orthop Surg. 2019;27(2):1-8. [DOI] [PubMed] [Google Scholar]
- 4.Yeoh D, Moffatt T, Karmani S. Good outcomes of percutaneous fixation of spinal fracture in ankylosing spinal disorders. Injury. 2014;45(10):1534-38. [DOI] [PubMed] [Google Scholar]
- 5.Heyde CE, Fakler JK, Hasenboehler E, et al. Pitfalls and complications in the treatment of cervical spine fractures in patients with ankylosing spondylitis. Patient Saf Surg. 2008;2:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi D. Fractures in ankylosing disorders of the spine: Easy to miss and high risk of deterioration. World Neurosurg. 2015;83(6):1029-31. [DOI] [PubMed] [Google Scholar]
- 7.Matsukawa K, Yato Y, Kato T, et al. Cortical bone trajectory for lumbosacral fixation: penetrating S-1 endplate screw technique: technical note. J Neurosurg Spine. 2014;21(2):203-9. [DOI] [PubMed] [Google Scholar]
- 8.Resnick D, Shaul SR, Robins JM, et al. Diffuse idiopathic skeletal hyperostosis (DISH): Forestiers disease with extraspinal manifestations. Radiology. 1975;115(3):513-24. [DOI] [PubMed] [Google Scholar]
- 9.Raley DA, Mobbs RJ. Retrospective computed tomography scan analysis of percutaneously inserted pedicle screws for posterior transpedicular stabilization of the thoracic and lumbar spine. Spine. 2012;37(12):1092-100. [DOI] [PubMed] [Google Scholar]
- 10.Belanger TA, Rowe DE. Diffuse idiopathic skeletal hyperostosis: musculoskeletal manifestations. J Am Acad Orthop Surg. 2001;9(4):258-67. [DOI] [PubMed] [Google Scholar]
- 11.Olerud C, Frost A, Bring J. Spinal fractures in patients with ankylosing spondylitis. Eur Spine J. 1996;5(1):51-5. [DOI] [PubMed] [Google Scholar]
- 12.Paxisons O, Tsitsopoulos PP, Zindrick MR, et al. Evaluation of pullout strength and failure mechanism of posterior instrumentation in normal and osteopenic thoracic vertebrae. J Neurosurg Spine. 2010;13(4):469-76. [DOI] [PubMed] [Google Scholar]
- 13.Caron T, Bransford R, Nguyen Q, et al. Spine fracture in patients with ankylosing spinal disorders. Spine. 2010;35(11):458-64. [DOI] [PubMed] [Google Scholar]
- 14.Abdu WA, Wilber RG, Emery SE, et al. Pedicular transvertebral screw fixation of the lumbosacral spine in spondylolisthesis. Spine. 1994;19(6):710-5. [DOI] [PubMed] [Google Scholar]
- 15.Minamide A, Akamaru T, Yoon ST, et al. Transdiscal L5-S1 screws for the fixation of isthmic spondylolisthesis: A biomechanical evaluation. J Spinal Disord Tech. 2003;16(2):144-9. [DOI] [PubMed] [Google Scholar]
- 16.Nottmeier EW, Pirris SM. Placement of thoracic transvetebral pedicle screws using 3D image guidance. J Neurosurg Spine. 2013;18(5):479-83. [DOI] [PubMed] [Google Scholar]
- 17.Rodriguez-Martinez NG, Savardekar A, Nottmeier EW, et al. Biomechanics of transvertebral screw fixation in the thoracic spine: an in vitro study. J Neurosurg Spine. 2016;25(2):187-92. [DOI] [PubMed] [Google Scholar]
- 18.Sandquist L, Carr D, Tong D, et al. Preventing proximal junctional failure in long segmental instrumented cases of adult degenerative scoliosis using a multilevel stabilization screw technique. Surg Neurol Int. 2015;6:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lehman RA, Helgeson MD, Dmitriev AE, et al. What is the best way to optimize thoracic kyphosis correction? Spine. 2012;37(19):1171-6. [DOI] [PubMed] [Google Scholar]
- 20.Zindrick MR, Wiltse LL, Doornk A, et al. Analysis of the Morphometric characteristics of the Thoracic and Lumbar Pedicles. Spine. 1987;12(2):160-6. [DOI] [PubMed] [Google Scholar]


