To the Editor:
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first reported in Wuhan in December 2019 (1) and has since spread quickly around the world. This global pandemic urgently needed optimal treatment and management strategies for COVID-19 patients, especially for those critically ill. Although SARS-CoV-2 predominantly affects the respiratory system, recent publications reported acute kidney injury (AKI) as a significant comorbidity in COVID-19. The reported incidence of AKI in COVID-19 patients varies, and most reports from ICUs presented an incidence of 10–30% (2). Cheng et al (3) reported a significantly higher in-hospital mortality for COVID-19 patients with severe AKI even after adjusting for known confounders. Significantly, Pei et al (4) revealed that the mortality of COVID-19 pneumonia was significantly higher in patients with AKI than those without. These accumulated observations have indicated that careful management is necessary in the treatment of critically ill patients with respiratory failure and AKI as part of COVID-19.
Here, we report a retrospective analysis of urinary neutrophil gelatinase-associated lipocalin (NGAL) in ICU patients with COVID-19-associated respiratory failure. We included all adult patients admitted to the medical ICU of the University of Tokyo Hospital who were diagnosed with respiratory failure associated with COVID-19 through May 10, 2020. Reverse transcriptase-polymerase chain reaction on specimens obtained via nasopharyngeal swab or endotracheal suctioning was conducted to confirm SARS-CoV-2 infection. A treating physician who was independent from this study made all clinical decisions during the ICU stay for each patient. The study protocol was approved by the institutional review board of the University of Tokyo Faculty of Medicine (number 3820). Informed consent was waived due to the health record-based, retrospective nature of the study.
All clinical data and outcomes were extracted from the electronic health record system of the hospital. The final data extraction was conducted on June 10, 2020. AKI during ICU stay was defined in accordance with the serum creatinine and urinary output-based criteria by Kidney Disease Improving Global Outcomes (KDIGO) AKI guideline (5). The in-hospital clinical laboratory conducted urinary NGAL measurements by chemiluminescent immunoassay. Clinical outcomes of interest were AKI, length of mechanical ventilation, and ICU stay. The comparison of continuous values between AKI and non-AKI group was performed by Wilcoxon rank-sum test. Correlations between urinary NGAL values and outcomes in continuous variables were evaluated using the least squares method. If the regression was statistically significant, the resulting regression line was presented with the coefficient of determination (R2). p values of less than 0.05 were considered significant.
Seventeen consecutive ICU patients with COVID-19-associated respiratory failure, who were admitted between March 26, 2020, and May 7, 2020, were included in this study. All patients needed oxygen therapy during admission in the ICU. Table 1 shows a summary of baseline characteristics, laboratory data at ICU admission, clinical management, and outcomes. Two patients died on ICU days 7 and 14; both were under treatment-withholding orders since days 1 and 3, respectively. These two patients were excluded from the analysis on the length of mechanical ventilation and ICU stay. The median durations of the ventilation and ICU stay were 9 days (interquartile range [IQR], 9–22 d) and 12 days (IQR, 6–23 d), respectively. One patient was still on a ventilator and two were treated in the ICU as of June 10, 2020. Ten patients developed AKI during their ICU stay. The median duration from ICU admission to AKI diagnosis was 7 days; two patients met the KDIGO AKI criteria at ICU admission, while the others met criteria within 2–15 days from admission. Furthermore, patients who developed AKI during ICU stay (n = 10) showed significantly higher urinary NGAL level at ICU admission compared with those who never fulfilled the AKI diagnostic criteria (n = 7) (93.0 vs 26.6 ng/mL; p = 0.019; Fig. 1A). The area under the receiver operating characteristic curve for AKI diagnosis by urinary NGAL level at ICU admission was 0.84 (95% CI, 0.56–0.96). The optimal cutoff value of urinary NGAL was 73 ng/mL, with sensitivity of 0.70 and specificity of 0.86. Due to multiple urinary NGAL measurements in the first and second days at the ICU, we adopted the maximum value of NGAL within 48 hours from ICU admission as a predictor variable for the length of mechanical ventilation and ICU stay. As illustrated in Figure 1B, higher urinary NGAL level was correlated with longer length of mechanical ventilation (R2 = 0.78; p < 0.01). Higher urinary NGAL level was also correlated with longer length of ICU stay (R2 = 0.42; p < 0.01).
Table 1.
Baseline Characteristics, Management, and Outcomes of Critically Ill Patients With Coronavirus Disease 2019
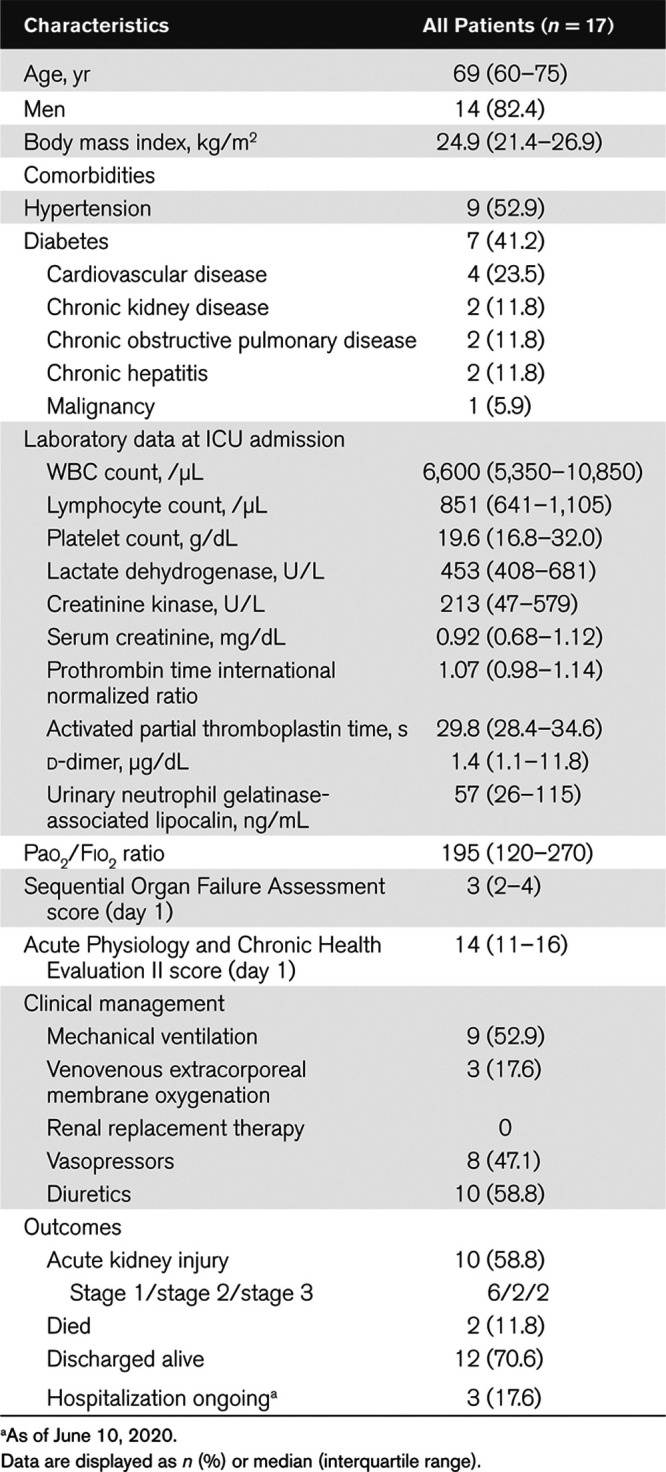
Figure 1.
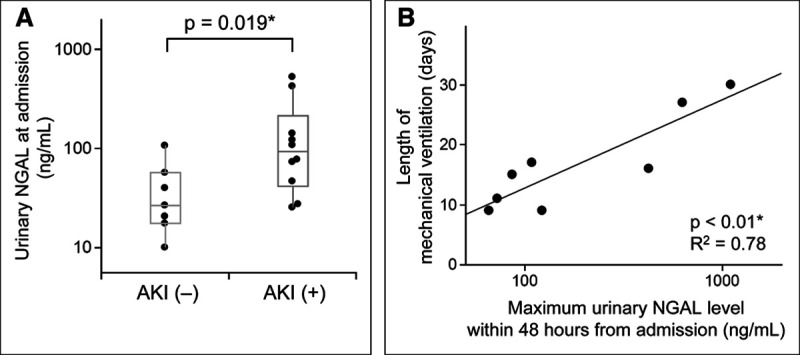
Urinary neutrophil gelatinase-associated lipocalin (NGAL) level in ICU patients with coronavirus disease 2019 associated with acute kidney injury (AKI) diagnosis and length of mechanical ventilation. Those who developed AKI (n = 10) manifested significantly higher urinary NGAL level at admission than those without AKI (n = 7) (93.0 vs 26.6 ng/mL; p = 0.019) (A). Lengths of mechanical ventilation are presented against maximum urinary NGAL level acquired within 48 hr from ICU admission in eight patients who required ventilator during ICU stay (B, except one dead patient). There was a significant positive correlation (p < 0.01) with coefficient of determination (R2) of 0.78. NGAL levels were illustrated with logarithmic scale. *p < 0.05.
In this study involving 17 critically ill COVID-19 patients, we found that urinary NGAL level at ICU admission was elevated in patients who went on to develop AKI during their ICU stay. Furthermore, the maximum urinary NGAL value in the first 48 hours from ICU admission was correlated with length of mechanical ventilation.
To the best of our knowledge, this is the first report on urinary NGAL measurement in critically ill patients with COVID-19. Our results suggest that urinary NGAL may be applicable as an AKI biomarker in this patient group. With regard to COVID-19, several reports indicated that SARS-CoV-2 could directly infect the kidneys. The cell surface protein, angiotensin-converting enzyme 2, which is used by the virus as an entry receptor, is abundantly expressed in renal tubular epithelial cells (6). In recent studies on autopsy cases of COVID-19, electron microscopy revealed viral structures, which were morphologically identical to SARS-CoV-2, in the renal tubular epithelium (7, 8). The direct infection of SARS-CoV-2 to renal tubular epithelial cells may enhance the clinical value of urinary NGAL as AKI marker among COVID-19 patients.
Another finding in this study was the correlation between urinary NGAL level in the early phase of ICU stay and the length of mechanical ventilation. This correlation suggested that urinary NGAL level might reflect not only the severity of kidney injury but also lung injury in the COVID-19 patients. NGAL was reportedly expressed in bronchial goblet cells and alveolar type II epithelial cells, and the expression was upregulated by inflammation (9). Further studies on the pathophysiology of lung injury in COVID-19 patients may highlight the efficacy of urinary NGAL as a biomarker for respiratory failure beyond its known role in AKI diagnosis.
As is common with a small cohort study of short duration, this study should be interpreted with caution, as the risk for selection bias and confounding preclude more definitive conclusions. Further studies with large sample size are urgently warranted to clarify the clinical impact of urinary NGAL in the context of treating COVID-19 patients with respiratory failure and AKI.
In conclusion, the urinary NGAL level was significantly associated with AKI diagnosis of ICU patients. The correlation between urinary NGAL level and the length of ventilator dependency suggested that NGAL also reflected the severity of lung injury in COVID-19 patients, although this hypothesis should be validated in future studies.
Footnotes
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Guan WJ, Ni ZY, Hu Y, et al. ; China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382:1708–1720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020; 8:475–481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheng Y, Luo R, Wang K, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020; 97:829–838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pei G, Zhang Z, Peng J, et al. Renal involvement and early prognosis in patients with COVID-19 Pneumonia. J Am Soc Nephrol. 2020; 31:1157–1165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kellum JA, Lameire N, Aspelin P, et al. Kidney Disease: Improving Global Outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012; 2:1–138 [Google Scholar]
- 6.Hamming I, Timens W, Bulthuis ML, et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004; 203:631–637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Su H, Yang M, Wan C, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020; 98:219–227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farkash EA, Wilson AM, Jentzen JM. Ultrastructural evidence for direct renal infection with SARS-CoV-2. J Am Soc Nephrol. 2020; 31:1683–1687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cowland JB, Sørensen OE, Sehested M, et al. Neutrophil gelatinase-associated lipocalin is up-regulated in human epithelial cells by IL-1 beta, but not by TNF-alpha. J Immunol. 2003; 171:6630–6639 [DOI] [PubMed] [Google Scholar]


