Abstract
Background:
Income is 1 of the socio-economic indicators and could directly influence the health outcomes of cardiovascular disease (CVD). The relationship between income and CVD has attracted more and more scholars’ attention in the past 20 years.
Methods:
To study the current research dynamics of this field, a bibliometric analysis was conducted to evaluate the publications from 1990 to 2018 based on the Science Citation Index Expanded database. By using the Derwent Date Analyzer software, the following aspects were explored:
-
(1)
historical trend of the topic;
-
(2)
the main contributor: leading countries, leading institutions, leading research areas and journals;
-
(3)
representative authors;
-
(4)
most frequently used keywords;
-
(5)
most cited papers.
Results:
The USA ranked first in this field, followed by UK and Canada in terms of number of publications. As for institutions, Harvard University took the leading place in the number of publications, as well as the h-index. Plos One had the most publications and “health” was the most frequent used keyword. The leading research area was “public environmental occupational health”.
Conclusions:
In conclusion, the elderly, the children and the puerpera were the main study population in this field and “disease prevention” was the main study direction. The most concerned health issues in this field were “obesity” and “diet”. There might be a lack of articles that explore the associations between income and CVD with a global perspective. Articles on this content are urgently warranted.
Keywords: cardiovascular disease, income, bibliometric, elderly, prevention
1. Introduction
Non-communicable diseases are reaching epidemic proportions worldwide [1] and responsible for nearly two-thirds of all global mortality with 41.1 million deaths in 2017.[2] Cardiovascular disease (CVD) is 1 of the Non-communicable diseases and had become a major global public health problem. According to the Global Burden of Disease 2017 study,[3–5] the worldwide numbers of CVD-related deaths increased from 11.9 million in 1990 to 17.8 million in 2017. An estimated mortality rate in 2017 was 233.1/100,000, in which 128.5/100,100 was in high-income countries, 254.1/100,000 was in upper-middle-income countries, 316.9/100,000 was in lower-middle-income countries and 285.3/100,000 was in low-income countries.[2] Compared with high-income countries, the mortality rate of CVD was much higher in lower- and middle-income countries.
Income is 1 of the socio-economic indicators and there are mainly 3 ways expressing the relationships between income and health including the individual income, country's gross national product, and income inequalities among different areas.[6] So far, numerous studies had indicated that income inequalities were a generalizable determinant that could directly influence some health outcomes,[7] such as life expectancy,[8–10] mortality,[11,12] incidence,[13,14] and so on.
As a common non-communicable disease, the health outcomes of CVD are also influenced by income. Researches found higher-income was associated with lower CVD mortality among the population aged 40 to 64.[15] Moreover, associations between CVD and income were inconsistent among countries with different income levels. Taking heart problems as an example, in the high-income countries, the population aged 45 to 64 in the lowest income quartile had the highest risk of CVD (prevalence).[16] But in the low- and middle-income countries, the results were contrary. The population aged 45 to 59 in the medium-income quartile had a higher risk than those in the lowest income quartile.[17] In addition to age or countries, gender is also a factor which is clearly linked either with income and with CVD. For instance, negative associations between household income and hypertension prevalence were found in both genders. However, in the same level of income increase, the decrease in prevalence seemed to be more obvious in women than men.[18] Therefore, generally speaking, there are still many unknowns in the field of “income and CVD” that deserve the attention of the academic community.
So far, there are many reviews articles have been published to summarize the associations between income and CVD, and discuss the status of CVD in countries with different income level.[19,20] But it seems that no 1 has ever studied the current research dynamics of this field.
Bibliometric analysis is an effective method to quantitatively analyze the published scientific articles and illuminate the research trends, hotspots, and collaborations. It is fundamentally different from a meta-analysis. Meta-analysis is a statistical method that combines results from different studies and calculates a quantitative estimated overall effect of a specific intervention or variable on a particular outcome, and it is mostly used in clinical research. Unlike meta-analysis, bibliometrics analysis mainly focuses on the research dynamics of a specific study field and it has been applied in many disciplines, including medicine[21] chemistry,[22] computing,[23] management,[24] economic,[25] and robotics.[26]
In this study, by using the bibliometrics analysis, we would like to present a different overview of this field with the following aspects:
-
(1)
historical trend of the topic;
-
(2)
the main contributor: leading countries, leading institutions, leading research areas and journals;
-
(3)
representative authors;
-
(4)
most frequently used keywords;
-
(5)
most cited papers.
2. Methodology and data source
By using the Derwent Date Analyzer (DDA) software,[26–31] the bibliometric analysis of this paper is based on publications related to “income and cardiovascular disease” published from 1990 to 2018. Literature was collected from the Science Citation Index-Expanded (SCI-E) and Social Science Citation Index on June 13, 2019. The document types were defined as review and article. The ethics approval of this study was not required because it did not use individual-level data.
CVD is a class of diseases that involve the blood vessels or heart, including coronary artery diseases, stroke, heart failure and so on.[32] For developing a comprehensive search strategy for CVD, we searched the meta-analysis studies related to “CVD” in the Cochrane library. By integrating the search strategies of these studies,[33–36] the search formula of CVD was finally formulated as TS = ((hyperlipid∗ OR hyperlip?emia∗ OR hypercholesterol∗ OR hypercholester?emia∗ OR hyperlipoprotein?emia∗ OR hypertriglycerid?emia∗) OR (“high blood pressure”) OR (hypertensi∗ OR “peripheral arter∗ disease∗”) OR (stroke OR stokes OR cerebrovasc∗ OR cerebral OR apoplexy OR (brain SAME accident∗) OR (brain SAME infarct∗)) OR (“atrial fibrillat∗” OR tachycardi∗ OR endocardi∗) OR (pericard∗ OR isch?em∗ OR emboli∗ OR arrhythmi∗ OR thrombo∗) OR (cardio∗ OR cardia∗ OR heart∗ OR coronary∗ OR angina∗ OR ventric∗ OR myocard∗)). Then, this formula of CVD and the formula of income (TS = income) were searched simultaneously in the databases of Web of Science (WoS). Since the “topic” searching in WoS is only applied to the title, abstract, and keyword, there are certainly some related publications have not been covered.
Using DDA software, search results were quantitatively and qualitatively analyzed. A line chart was used to describe the publishing trend of global countries. Bibliometric indicators including the number of citations, number of publications and h-index were showed in tables to characterize the “income and CVD” research from different aspects. A cross-relationship map was made to illustrate the collaborative relationships between countries/regions. A bubble chart was applied to show the development trends of journals and author keywords.
3. Results and discussion
3.1. The Performance of related publications and countries
A total of 158 countries have published 17,764 articles and reviews, of which 264 are the Essential Science Indicators (ESI) Highly Cited articles and 13 are ESI hot articles. The total number of publications increased year by year (Fig. 1), which indicated that more and more scientists had focused their studies on this field. The top 3 most productive countries were the USA, UK, and Canada. The USA was the top country with most literature, and its increasing publishing trend was consistent with that of global. However, the increasing speed of the UK and Canada was relatively slower. The publications of these 2 countries started to show an obvious growth trend until 2002. During 2002-2011, they both increased almost at the same speed, but since 2012, UK exceeded Canada.
Figure 1.
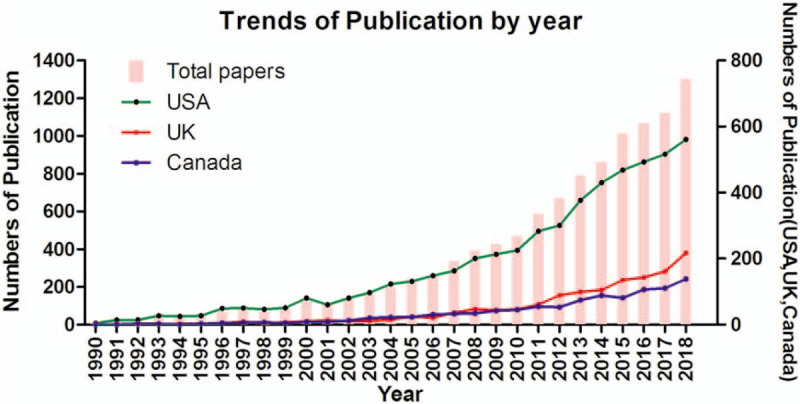
Trends in the total number of published papers related to income and CVD by year.
3.2. Cooperation of countries/regions
For better understanding, the contributions of each country/region in this field, the corresponding information of the top 20 most productive countries/regions were analyzed. As shown in Table 1, the USA was still at the top of the list and its publications had been accounted for almost half of the total papers. However, its indicator of average citations per paper (ACPP) was not the highest. In other words, the publishing quality of some countries (ie, Japan, Switzerland) was relatively better than that of the USA.
Table 1.
The top 20 most productive countries or regions in income and CVD field during 1990-2018.
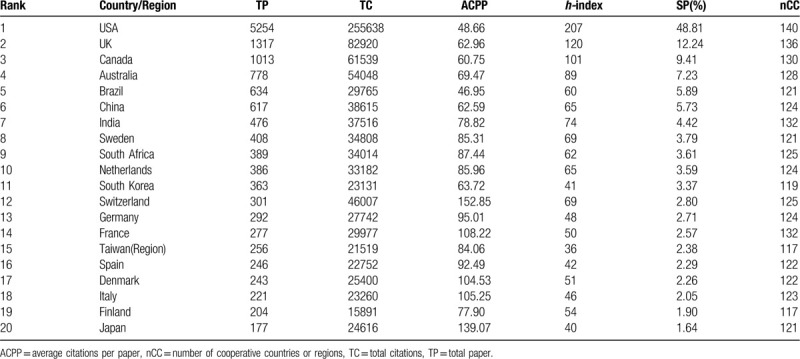
Moreover, there were only 5 developing countries/regions in this top 20 list, including Brazil, China, India, South Africa and Taiwan (region). Compared with developing countries, developed countries were paying more attention to “income and CVD” research.
Using DDA software, we draw a network diagram on the basis of the co-occurrence matrix (Fig. 2). The size of the node indicated the number of publications and the thickness of the connecting lines presented the frequencies of cooperation. As shown in Figure 2, there seemed to be no significant differences in cooperation between countries. Only the connecting lines between the USA and China, as well as the USA and India, seemed thicker than others. This might be indicated that developed countries like the USA had turned their researches into the income field of developing countries.
Figure 2.
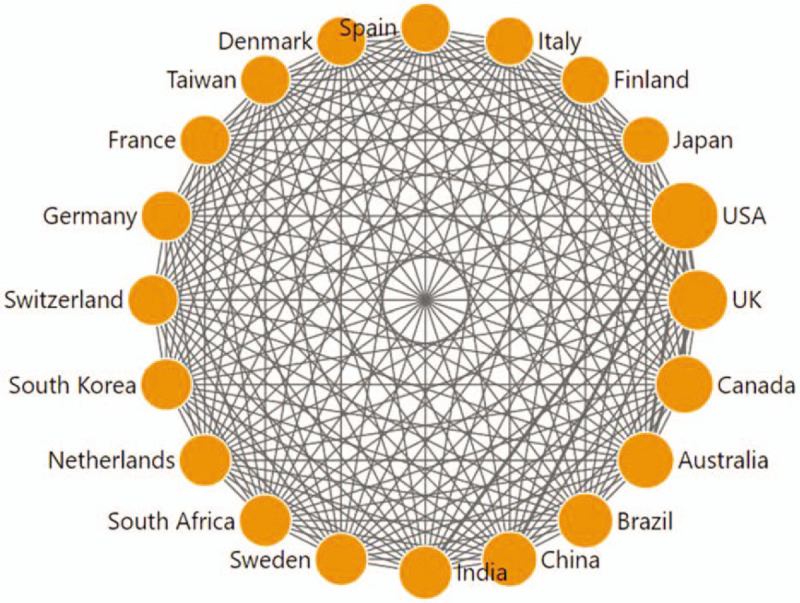
Collaboration matrix map among the top 20 productive countries/regions. Taiwan is a region of China.
3.3. Contribution of leading institutions
The top 20 productive institutions in “income and CVD” research were shown in Table 2, along with their numbers of publications, citations, and h-index. Among the 20 institutions, the USA had the largest share (12), followed by the UK (2), Canada (1), Australia (1), Brazil (1), South Korea (1), South Africa (1) and Sweden (1). Obviously, the 20 institutions are from the 8 countries which were exactly in the list of the top 10 most productive countries (Table 1). Only 2 countries which were also in the list, China and India, had no institutions in the top 20. Coincidentally, China and India happened to be the countries with the closest cooperation with the USA, according to Figure 2. Thereby, scholars in China and India might publish their studies on “income and CVD” mainly through cooperation with USA institutions.
Table 2.
The top 20 most productive institutions of publication, citations and h-index during 1990-2018.
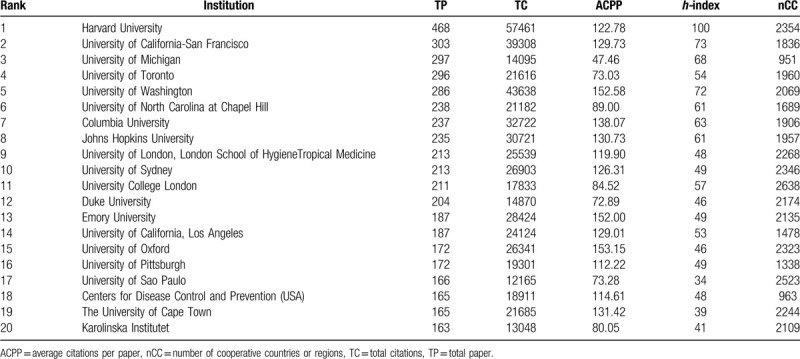
The top 3 productive institutions were also shown in Table 2, which were all from the USA. They were Harvard University, University of California-San Francisco and the University of Michigan in order. As for ACPP, the University of Oxford led the list with 153.15. Regarding the h-index, Harvard University still ranked first, also followed by the University of California-San Francisco and the University of Michigan, meaning the USA was an outstanding country with excellent academic institutions in this field of income and CVD.
3.4. Contribution of leading research areas and journals
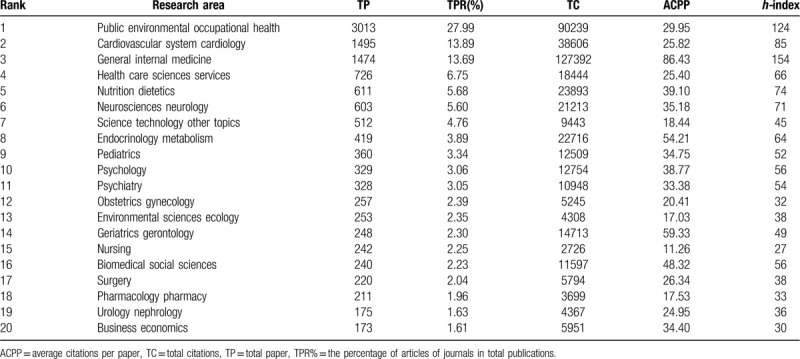
The top 20 WoS research areas ranked by the number of publications related to income and CVD were shown in Table 3. Surprisingly, “public environmental occupational health” dominated the research area list with 3013 papers, followed by “cardiovascular system cardiology”, “general internal medicine” and “health care sciences services”. Among the top 20 areas, 18 of them were related to medicine and the other 2 were related to science technology or economics. From the list of top 20 areas, we also noticed that the study population in the “income and CVD” field was mainly focused on children, the elderly and the puerpera.
Table 3.
Contribution of the top 20 research areas in income and CVD research.
The top 20 journals with most literature in the “income and CVD” field were listed in a bubble chart (Fig. 3). In 1990, Int J Epidemiol and Am J Prev Med firstly published related papers. The next year, in 1991, more and more journals began to publish papers related to income and CVD, including Lancet, J Epidemiol Community Health, Am J Public Health and Diabetes Care. As for the total publications during 1990-2018, Plos One took the leading position, followed by BMC Public Health, Soc Sci Med, BMJ Open and Lancet. But Plos One published the first paper since 2009. Both Plos One and BMC Public Health had seen a sharp increase in the number of publications since 2012. The annual publications of Soc Sci Med were relatively stable, but it seemed to have decreased in the past 2 years. Almost all these 20 journals were medicine related journals and the majority of them belong to the field of public health. In other words, current research on income and CVD mainly focuses on population prevention, rather than individual treatment.
Figure 3.
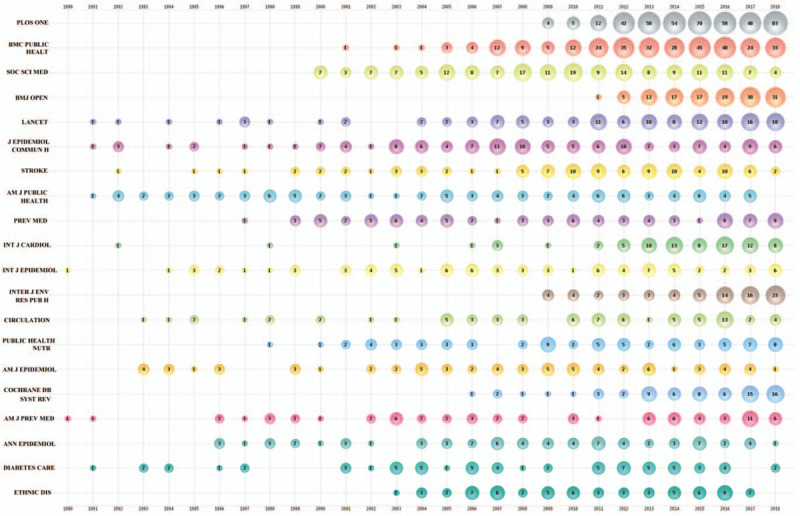
Bubble chart of top 20 productive journals by year.
3.5. Contribution of leading authors
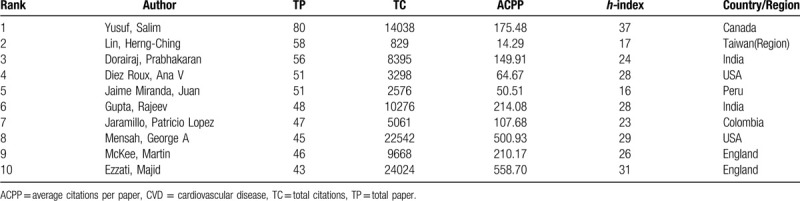
The top 10 productive authors were shown in Table 4. According to the number of publications, Yusuf, Salim was ranked the first, followed by Lin, Herng-Ching and Dorairaj, Prabhakaran. As for ACPP, Ezzati, Majid led the list and the second place became Mensah, George A. Moreover, 5 of the top 10 authors came from developing countries, indicating scholars in developing countries had been paying attention to this field, although their national publications had not yet caught up with developed countries.
Table 4.
Contribution of the Top 10 Authors in Income and CVD Research.
3.6. Analysis of author keywords
To reveal the hot spots and development trend of income and CVD research; more than 12,000 author keywords were analyzed using DDA software. The keywords with the same meanings had been combined. However; since some publications do not require author keywords; these papers were not included in this analysis.
The top 20 author keywords by year are shown in Figure 4. “Health[37–39]” was the most frequently used keyword, then followed by “socioeconomic status,[40–42]” “cardiovascular disease,[43–45]” “hypertension[46–48]” and “income.[49–51]” The frequency of all the top 20 keywords increased during 1990-2018.
Figure 4.
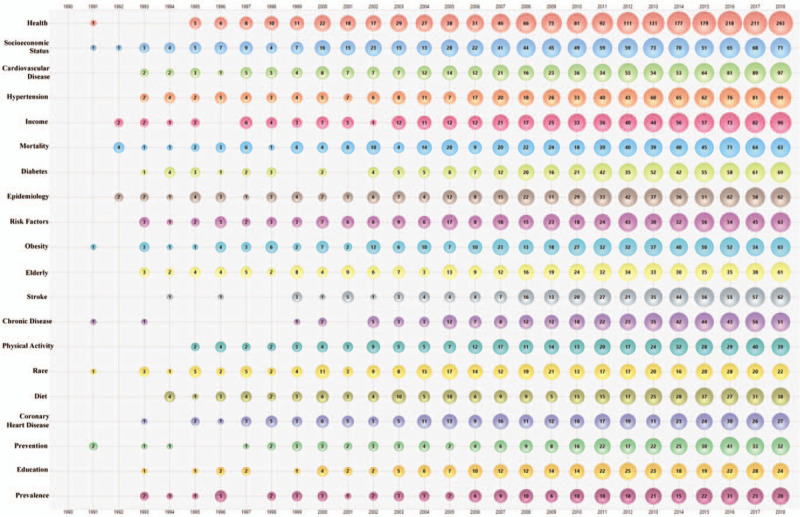
Bubble chart of top 20 author keywords by year.
In this study, the keyword “Health” mostly referred to as “Health Disparity/Inequality.[52–54]” A health disparity/inequality is a particular type of difference in health between different populations with various socio-demographic characteristics (i.e. socioeconomic status, racial/ethnic group, and education level).[55,56] For instance, a health disparity of coronary heart disease was observed in Americans with different family incomes and races. The worthiest Americans and Hispanics had the least risk of coronary heart disease.[49] Therefore, it was obvious that the published papers in this field mainly focused on evaluating the health disparity of CVD among different income levels.
Moreover, studying on these top 20 keywords, we could also find some hot spots in “income and CVD” field. First, the elderly[57–59] were the main study population in this field. Its main concern was the impact of income on CVD risk,[60] the efficacy of CVD therapy,[61] and the CVD outcome[62] in the elderly. Second, besides “income”, “race[57,63,64]” and “education[65–67]” were the most frequent social-demographic characteristics. In terms of either racial disparity or differences in education levels, the disease burden of CVD was different. Black persons and White persons lost 1.2 and 0.1 potential life-years before 75 years of age per person, respectively, with a difference of 1.1 years. Compared with the more-educated persons (2.8 potential life-years), the less-educated persons lost more potential life-years (4.6) for CVD.[67] Third, “disease prevention”[68–70] (including primary prevention[71] and secondary prevention[72,73]), and “risk factor”[68,74,75] were the main study direction. For instance, socioeconomic status, childhood and early-life factors, inequalities in health services, place of residence, wealth distribution, and work-related factors can affect CVD risk. Medical workers should reduce these risk factors via effective primary and secondary prevention.[71] Forth, “prevalence”[76–78] and “mortality”[38,79,80] were both the study epidemiological indicators of this field, including hypertension prevalence,[81] prevalence of peripheral artery disease,[82] cardiorespiratory mortality,[83] premature cardiovascular mortality[84] and so on. Fifth, the most concerned health issues in this field were “obesity”[85–87] and “diet”[85,88,89]. Income may affect someone's dietary intake behaviors, leading to obesity which was 1 of the risk factors for CVD. Sixth, hypertension,[90,91] diabetes,[92–94] stroke[95–97] and coronary heart disease[98–100] were the most studied chronic diseases associated with this field.
Moreover, gender is a factor which is clearly linked either with income and with CVD. Therefore, the keyword “gender” was studied although its frequency was not in Top 20 (ranked 33rd). First, women were more concerned than men about the relationship between income and CVD, such as low-income elderly women,[101] women at high risk for stroke,[102] black women[103] and so on. Second, “gender-differences” were the most discussed topics, and low income seemed to have a greater impact on the CVD risk in men than women. For instance, compared with women, 10-year estimated coronary heart disease risk was more tightly linked in men with lower household monthly income.[104] Also, low income was associated with hypertension prevalence in men, but not in women.[105]
3.7. An analysis of the most cited papers
The number of citations is an indicator that evaluating the impact of a scientific publication, and it reflects an article's contribution to the field of interest. Many scholars had published bibliometric analyses on the most-cited papers in a specialty field.[106–109] In this study, we also used this indicator of an article to reflect the hotspots of “income and CVD” research. The top 10 most cited publications were listed in Table 5.
Table 5.
Top 10 most cited publications in income and CVD research during 1990-2018.
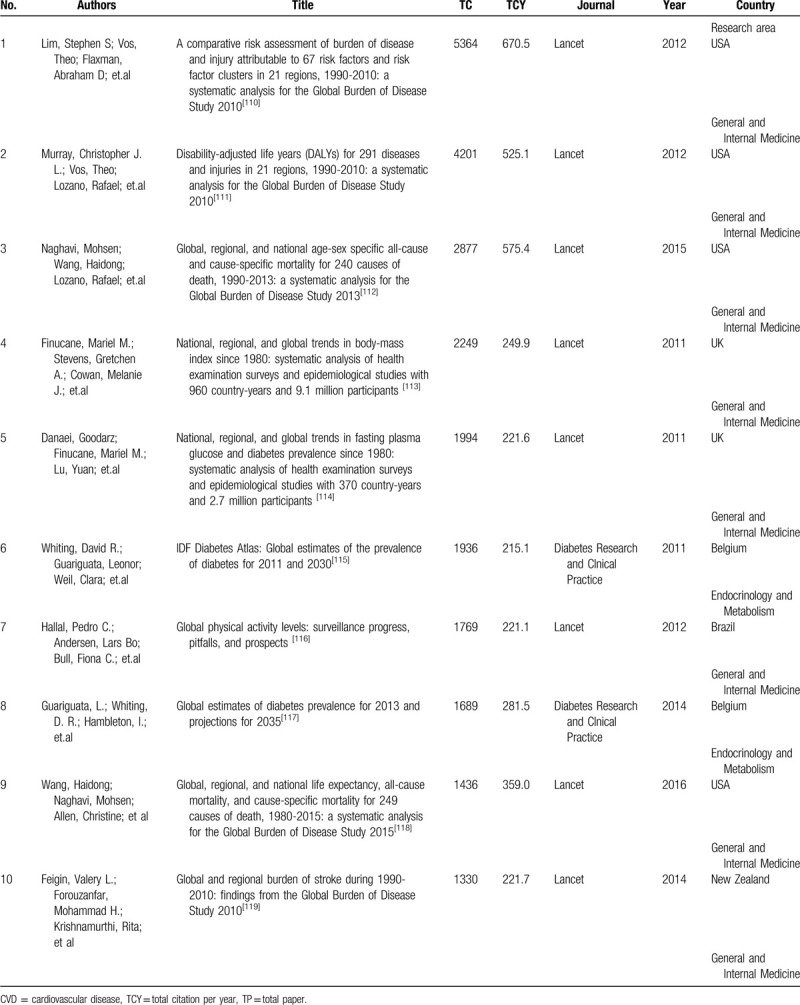
The most highly cited paper was “A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010” published in Lancet. This paper described the distributions of risk factors (ie, high blood pressure) in countries with different income levels.
The contents of the other 9 most cited papers were basically similar to this 1. They were all descriptive studies of global health issues using epidemiological indicators and could help scholars understand the global health issues quickly and accurately. Therefore, they became the top 10 most cited papers.
However, these 10 most cited papers might not be the best articles explaining the associations between income and CVD. Articles that explore the associations between income and CVD with a global perspective are urgently warranted.
4. Conclusions
Based on bibliometrics and DDA software, this study provides a new perspective on the field of “income and CVD” through the information analysis involving yearly publication trends, leading countries, institutions, authors, journals, keywords and so on. Several findings could be summarized as follows.
First, the field of “income and CVD” has attracted the increasing attention of numerous global scholars.
Second, compared with developing countries, developed countries are paying more attention to “income and CVD” research. As developing countries, China and India have the closest cooperation with the USA, and these 2 countries may publish their studies on “income and CVD” mainly through cooperation with USA institutions.
Third, the elderly, the children and the puerpera are the main study population in this field, especially for these populations of different races and educational levels.
Forth, “disease prevention” is the main study direction, and “prevalence” and “mortality” are the main study epidemiological indicators of this field.
Fifth, the most concerned health issues in this field are “obesity” and “diet”, and the most studied chronic diseases are hypertension, diabetes, stroke, and coronary heart disease.
Sixth, there is a lack of articles that explore the associations between income and CVD with a global perspective. Articles on this content are urgently warranted.
In general, this study can help scholars better understanding the global overview of “income and CVD”, and provide the information of potential collaborators, as well as the information of promising attractive areas for future research.
Author contributions
Conceptualization: Yuehua Wan, Qing Shen.
Data curation: Xufen Ding.
Formal analysis: Xufen Ding, Yuehua Wan.
Funding acquisition: Ye Ding, Dingwan Chen.
Investigation: Ye Ding, Dingwan Chen, Xufen Ding, Guan Wang
Methodology: Qing Shen.
Project administration: Yuehua Wan, Qing Shen.
Resources: Dingwan Chen.
Visualization: Guan Wang.
Writing – original draft: Ye Ding.
Writing – review and editing: Yuehua Wan
Footnotes
Abbreviations: ACPP = average citations per paper, CVD = cardiovascular disease, DDA = Derwent date analyzer, WoS = web of science.
How to cite this article: Ding Y, Chen D, Ding X, Wang G, Wan Y, Shen Q. A bibliometric analysis of income and cardiovascular disease: status, hotspots, trends and outlook. Medicine. 2020;99:34(e21828).
This study was supported by the General Project of Department of Education of Zhejiang Province [grant number: Y201840321], Soft Science Research Program of Zhejiang Province [grant number: 2018C35023] and Humanity and Social Science Project of Zhejiang Education Department [Y201738172].
This article is a bibliometric analysis. No patients or the public were included in our study.
This study did not use individual-level data, so ethics approval was not required.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors have no conflicts of interest to disclose.
References
- [1].Daar AS, Singer PA, Persad DL, et al. Grand challenges in chronic non-communicable diseases. Nature 2007;450:494–6. [DOI] [PubMed] [Google Scholar]
- [2].Jagannathan R, Patel SA, Ali MK, et al. Global updates on cardiovascular disease mortality trends and attribution of traditional risk factors. Curr Diab Rep 2019;19:44. [DOI] [PubMed] [Google Scholar]
- [3].Keil U, Kuulasmaa K. WHO MONICA project: risk factors. Int J Epidemiol 1989;18:46–55. [PubMed] [Google Scholar]
- [4].Yusuf S, Hawken S, Ôunpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Orvosi Hetilap 2006;147:675. [DOI] [PubMed] [Google Scholar]
- [5].Yusuf S, Reddy S, Ounpuu S, et al. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 2001;104:2746–53. [DOI] [PubMed] [Google Scholar]
- [6].Marmot M. The influence of income on health: views of an epidemiologist. Health Aff 2002;21:31–46. [DOI] [PubMed] [Google Scholar]
- [7].John L, George Davey S, Sam H, et al. Is income inequality a determinant of population health? Part 1. A systematic review. Milbank Q 2004;82:5–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Jetter M, Laudage S, Stadelmann D. The Intimate Link between Income Levels and Life Expectancy: Global Evidence from 213 Years. Social Science Electronic Publishing 2019;100:1387–403. [Google Scholar]
- [9].Kinge JM, Modalsli JH, Overland S, et al. Association of household income with life expectancy and cause-specific mortality in Norway, 2005-2015. JAMA 2019;321:1916–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Jetter M, Laudage S, Stadelmann D. The Intimate Link Between Income Levels and Life Expectancy: Global Evidence from 213 Years. Soc Sci Q 2019;100:1387–403. [Google Scholar]
- [11].Lee H, Park JH, Floyd JS, et al. Combined effect of income and medication adherence on mortality in newly treated hypertension: nationwide study of 16 million person-years. J Am Heart Association 2019;8:e013148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Pabayo R, Cook DM, Harling G, et al. State-level income inequality and mortality among infants born in the United States 2007-2010: a Cohort study. BMC Public Health 2019;19:1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Bell JS, Koffie RM, Rattani A, et al. Global incidence of brain and spinal tumors by geographic region and income level based on cancer registry data. J Clin Neuro 2019;66:121–7. [DOI] [PubMed] [Google Scholar]
- [14].Bonell A, Azarrafiy R, Huong VTL, et al. A systematic review and meta-analysis of ventilator-associated pneumonia in adults in Asia: an analysis of national income level on incidence and etiology. Clin Infec Dis 2019;68:511–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Toivanen S, Hemstrom O. Income differences in cardiovascular disease: is the contribution from work similar in prevalence versus mortality outcomes? Int J Behav Med 2006;13:89–100. [DOI] [PubMed] [Google Scholar]
- [16].Korda RJ, Paige E, Yiengprugsawan V, et al. Income-related inequalities in chronic conditions, physical functioning and psychological distress among older people in Australia: cross-sectional findings from the 45 and up study. BMC Public Health, 14,1(2014-07-22) 2014;14:741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Shangren Q, Zirui H, Ye D. Income-Related Inequalities in Chronic Disease Situation Among the Chinese Population Aged Above 45 Years. Inquiry 2019;56: 46958019860383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Tang K, Zhang Y, Wang H, et al. Regional economic development, household income, gender and hypertension: evidence from half a million Chinese. BMC Public Health 2020;20:901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Bowry AD, Lewey J, Dugani SB, et al. The burden of cardiovascular disease in low- and middle-income countries: epidemiology and management. Can J Cardiol 2015;31:1151–9. [DOI] [PubMed] [Google Scholar]
- [20].Sun LY, Lee EW, Zahra A, et al. Risk Factors of Cardiovascular Disease and Their Related Socio-Economical, Environmental and Health Behavioral Factors: Focused on Low-Middle Income Countries- A Narrative Review Article. Iran J Public Health 2015;44:435–44. [PMC free article] [PubMed] [Google Scholar]
- [21].Chen H, Wan Y, Jiang S, et al. Alzheimer's disease research in the future: bibliometric analysis of cholinesterase inhibitors from 1993 to 2012. Scientometrics 2014;98:1865–77. [Google Scholar]
- [22].Hernandez-Garcia YI, Chamizo JA, Kleiche-Dray M, et al. The scientific impact of mexican steroid research 1935-1965: A bibliometric and historiographic analysis. J Assoc Inf Sci Tech 2015;67:1245–56. [Google Scholar]
- [23].Franceschet M. A comparison of bibliometric indicators for computer science scholars and journals on Web of Science and Google Scholar. Scientometrics 2010;83:243–58. [Google Scholar]
- [24].Mingers J, Yang L. Evaluating journal quality: a review of journal citation indicators and ranking in business and management. Eur J Oper Res 2017;257:323–37. [Google Scholar]
- [25].Merigó JM, Rocafort A, Aznar-Alarcón JP. Bibliometric overview of business and economics research. J Bus Econ Manag 2016;17:397–413. [Google Scholar]
- [26].Bao G, Fang H, Chen L, et al. Soft robotics: academic insights and perspectives through bibliometric analysis. Soft Robot 2018;5:229–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Wu YQ, Wan YH, Zhang FZ. Characteristics and trends of C-H activation research: a review of literature. Curr Org Synth 2018;15:781–92. [Google Scholar]
- [28].He L, Fang H, Chen C, et al. Metastatic castration-resistant prostate cancer: academic insights and perspectives through bibliometric analysis. Medicine (Baltimore) 2020;99:e19760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Li L, Lu J, Fang H, et al. Lattice Boltzmann method for fluid-thermal systems: status, hotspots, trends, and outlook. IEEE Access 2020;8:27649–75. [Google Scholar]
- [30].Liu T, Hu H, Ding X, et al. 12 years roadmap of the sulfur cathode for lithium sulfur batteries (2009-2020). Energy Storage Materials 2020;30:344–6. [Google Scholar]
- [31].Wang C, Wu R, Deng L, et al. A Bibliometric analysis on no-show research: status, hotspots. Trends and Outlook Sustainability 2020;12:3997. [Google Scholar]
- [32].Geneva World Health Organization., Mendis S, Puska P, Norrving B, et al. Global atlas on cardiovascular disease prevention and control. 2011. [Google Scholar]
- [33].Al-Khudairy L, Flowers N, Wheelhouse R, et al. Vitamin C supplementation for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev 2017;3:CD011114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Clar C, Oseni Z, Flowers N, et al. Influenza vaccines for preventing cardiovascular disease. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Hartley L, May MD, Loveman E, et al. Dietary fibre for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev 2016;1:CD011472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Uthman OA, Hartley L, Rees K, et al. Multiple risk factor interventions for primary prevention of cardiovascular disease in low- and middle-income countries. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Johnson RC. Addressing racial health disparities: looking back to point the way forward. Ann Am Acad Polit Soc Sci 2018;680:132–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Pappas G, Queen S, Hadden W, et al. THE increasing disparity in mortality between socioeconomic groups in the United-States, 1960 and 1986. N Engl J Med 1993;329:103–9. [DOI] [PubMed] [Google Scholar]
- [39].Braveman P, Tarimo E. Social inequalities in health within countries: not only an issue for affluent nations. Soc Sci Med 2002;54:1621–35. [DOI] [PubMed] [Google Scholar]
- [40].Seto J, Davis J, Taira DA. Examining the association between different aspects of socioeconomic status, race, and disability in Hawaii. J Racial Ethn Health Disparities 2018;5:1247–53. [DOI] [PubMed] [Google Scholar]
- [41].Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health 2001;55:111–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research - One size does not fit all. JAMA-J Am Med Assoc 2005;294:2879–88. [DOI] [PubMed] [Google Scholar]
- [43].Paudel R, Lee K, Singh JK, et al. Prevalence of behavioral risk factors of cardiovascular diseases and associated socio-economic factors among pregnant women in a rural area in Southern Nepal. BMC Pregnancy Childbirth 2018;18:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Roth GA, Johnson C, Abajobir A, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol 2017;70:1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Wolfe F, Freundlich B, Straus WL. Increase in cardiovascular and cerebrovascular disease prevalence in rheumatoid arthritis. J Rheumatol 2003;30:36–40. [PubMed] [Google Scholar]
- [46].Mayega RW, Ekirapa E, Kirunda B, et al. "What kind of life is this?.’ Diabetes related notions of wellbeing among adults in eastern Uganda and implications for mitigating future chronic disease risk. BMC Public Health 2018;18:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 2016;134:441–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Perneger TV, Whelton PK, Klag MJ. Race and end-stage renal-disease socioeconomic-status and access to health-care as mediating factors. Arch Intern Med 1995;155:1201–8. [PubMed] [Google Scholar]
- [49].Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health 2010;100: Suppl 1: S186–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Ataklte F, Erqou S, Kaptoge S, et al. Burden of undiagnosed hypertension in Sub-Saharan Africa a systematic review and meta-analysis. Hypertension 2015;65:291-U115. [DOI] [PubMed] [Google Scholar]
- [51].Taylor WC, Baranowski T, Young DR. Physical activity interventions in low-income, ethnic minority, and populations with disability. Am J Prev Med 1998;15:334–43. [DOI] [PubMed] [Google Scholar]
- [52].Schnittker J, McLeod JD. The social psychology of health disparities. Annu Rev Sociol 2005;31:75–103. [Google Scholar]
- [53].Signorello LB, Hargreaves MK, Steinwandel MD, et al. Southern community cohort study: establishing a cohort to investigate health disparities. J Natl Med Assoc 2005;97:972–9. [PMC free article] [PubMed] [Google Scholar]
- [54].Chen E, Martin AD, Matthews KA. Understanding health disparities: the role of race and socioeconomic status in children's health. Am J Public Health 2006;96:702–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health 2006;27:167–94. [DOI] [PubMed] [Google Scholar]
- [56].Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health 2011;32:381–98. [DOI] [PubMed] [Google Scholar]
- [57].Kanchi R, Perlman SE, Chernov C, et al. Gender and race disparities in cardiovascular disease risk factors among New York City Adults: New York City Health and Nutrition Examination Survey (NYC HANES) 2013-2014. J Urban Health 2018;95:801–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Bassuk SS, Glass TA, Berkman LF. Social disengagement and incident cognitive decline in community-dwelling elderly persons. Ann Intern Med 1999;131:165–73. [DOI] [PubMed] [Google Scholar]
- [59].Klipstein-Grobusch K, Geleijnse JM, den Breeijen JH, et al. Dietary antioxidants and risk of myocardial infarction in the elderly: the Rotterdam Study. Am J Clin Nutr 1999;69:261–6. [DOI] [PubMed] [Google Scholar]
- [60].Philbin EF, Dec GW, Jenkins PL, et al. Socioeconomic status as an independent risk factor for hospital readmission for heart failure. Am J Cardiol 2001;87:1367–71. [DOI] [PubMed] [Google Scholar]
- [61].Benner JS, Glynn RJ, Mogun H, et al. Long-term persistence in use of statin therapy in elderly patients. JAMA-J Am Med Assoc 2002;288:455–61. [DOI] [PubMed] [Google Scholar]
- [62].Kant AK. Dietary patterns and health outcomes. J Am Diet Assoc 2004;104:615–35. [DOI] [PubMed] [Google Scholar]
- [63].Gornick ME, Eggers PW, Reilly TW, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med 1996;335:791–9. [DOI] [PubMed] [Google Scholar]
- [64].Cohen S, Schwartz JE, Epel E, et al. Socioeconomic status, race, and diurnal cortisol decline in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Psychosom Med 2006;68:41–50. [DOI] [PubMed] [Google Scholar]
- [65].Lumme S, Manderbacka K, Karvonen S, et al. Trends of socioeconomic equality in mortality amenable to healthcare and health policy in 1992-2013 in Finland: a population-based register study. BMJ Open 2018;8:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Braveman P, Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep 2014;129:19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Wong MD, Shapiro MF, Boscardin WJ, et al. Contribution of major diseases to disparities in mortality. N Engl J Med 2002;347:1585–92. [DOI] [PubMed] [Google Scholar]
- [68].Pogosova N, Oganov R, Saner H, et al. Potential and limitations of health policy to improve coronary heart disease prevention and to reduce the burden of disease: a Russian experience. Eur J Prev Cardiol 2018;25:1725–34. [DOI] [PubMed] [Google Scholar]
- [69].Beaglehole R, Bonita R, Horton R, et al. Priority actions for the non-communicable disease crisis. Lancet 2011;377:1438–47. [DOI] [PubMed] [Google Scholar]
- [70].Danaei G, Finucane MM, Lin JK, et al. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5.4 million participants. Lancet 2011;377:568–77. [DOI] [PubMed] [Google Scholar]
- [71].Clark AM, DesMeules M, Luo W, et al. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol 2009;6:712–22. [DOI] [PubMed] [Google Scholar]
- [72].Dehghan M, Mente A, Zhang XH, et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet 2017;390:2050–62. [DOI] [PubMed] [Google Scholar]
- [73].Bushnell CD, Olson DM, Zhao X, et al. Secondary preventive medication persistence and adherence 1 year after stroke. Neurology 2011;77:1182–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Patel V, Chatterji S, Chisholm D, et al. India: towards universal health coverage 3 chronic diseases and injuries in India. Lancet 2011;377:413–28. [DOI] [PubMed] [Google Scholar]
- [75].Sadhu JS, Novak E, Mukamal KJ, et al. Association of alcohol consumption after development of heart failure with survival among older adults in the cardiovascular health study. JAMA Netw Open 2018;1:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Altobelli E, Rapacchietta L, Profeta VF, et al. Risk factors for abdominal aortic aneurysm in population-based studies: a systematic review and meta-analysis. Int J Environ Res Public Health 2018;15:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].van der Linde D, Konings EEM, Slager MA, et al. Birth Prevalence of congenital heart disease worldwide a systematic review and meta-analysis. J Am Coll Cardiol 2011;58:2241–7. [DOI] [PubMed] [Google Scholar]
- [78].Yang GH, Wang Y, Zeng YX, et al. Rapid health transition in China, 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2013;381:1987–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Shpilsky D, Bambs C, Kip K, et al. Association between ideal cardiovascular health and markers of subclinical cardiovascular disease. Clin Cardiol 2018;41:1593–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Bjelakovic G, Gluud LL, Nikolova D, et al. Vitamin D supplementation for prevention of mortality in adults. Cochrane Database Syst Rev 2014;257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA-J Am Med Assoc 2013;310:959–68. [DOI] [PubMed] [Google Scholar]
- [82].Fowkes FGR, Rudan D, Rudan I, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet 2013;382:1329–40. [DOI] [PubMed] [Google Scholar]
- [83].Abe KC, dos Santos GMS, Coelho M, et al. PM10 exposure and cardiorespiratory mortality - estimating the effects and economic losses in Sao Paulo, Brazil. Aerosol Air Qual Res 2018;18:3127–33. [Google Scholar]
- [84].Cao B, Bray F, Ilbawi A, et al. Effect on longevity of one-third reduction in premature mortality from non-communicable diseases by 2030: a global analysis of the Sustainable Development Goal health target. Lancet Glob Health 2018;6:E1288–96. [DOI] [PubMed] [Google Scholar]
- [85].Banik S, Rahman M. Prevalence of overweight and obesity in Bangladesh: a Systematic Review of the Literature. Curr Obes Rep 2018;7:247–53. [DOI] [PubMed] [Google Scholar]
- [86].Ahrens W, Bammann K, Siani A, et al. The IDEFICS cohort: design, characteristics and participation in the baseline survey. Int J Obes 2011;35:S3–15. [DOI] [PubMed] [Google Scholar]
- [87].Malik VS, Willett WC, Hu FB. Global obesity: trends, risk factors, and policy implications. Nat Rev Endocrinol 2013;9:13–27. [DOI] [PubMed] [Google Scholar]
- [88].Zanchim MC, Kirsten VR, De Marchi ACB. Consumption of dietary intake markers by patients with diabetes assessed using a mobile application. Cienc Saude Coletiva 2018;23:4199–208. [DOI] [PubMed] [Google Scholar]
- [89].Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr 2008;87:1107–17. [DOI] [PubMed] [Google Scholar]
- [90].Augustovski F, Chaparro M, Palacios A, et al. Cost-effectiveness of a comprehensive approach for hypertension control in low-income Settings in Argentina: trial-based analysis of the hypertension control program in Argentina. Value Health 2018;21:1357–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Mendis S, Lindholm LH, Mancia G, et al. World Health Organization (WHO) and International Society of Hypertension (ISH) risk prediction charts: assessment of cardiovascular risk for prevention and control of cardiovascular disease in low and middle-income countries. J Hypertens 2007;25:1578–82. [DOI] [PubMed] [Google Scholar]
- [92].Hsu PK, Kor CT, Hsieh YP. Effect of New-Onset diabetes mellitus on renal outcomes and mortality in patients with chronic kidney disease. J Clin Med 2018;7:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med 2010;71:1027–36. [DOI] [PubMed] [Google Scholar]
- [94].Agardh E, Allebeck P, Hallqvist J, et al. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol 2011;40:804–18. [DOI] [PubMed] [Google Scholar]
- [95].Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2014;383:245–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol 2009;8:345–54. [DOI] [PubMed] [Google Scholar]
- [97].O’Donnell MJ, Chin SL, Rangarajan S, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet 2016;388:761–75. [DOI] [PubMed] [Google Scholar]
- [98].Mayosi BM, Flisher AJ, Lalloo UG, et al. Health in South Africa 4 The burden of non-communicable diseases in South Africa. Lancet 2009;374:934–47. [DOI] [PubMed] [Google Scholar]
- [99].Banks J, Marmot M, Oldfield Z, et al. Disease and disadvantage in the United States and in England. JAMA-J Am Med Assoc 2006;295:2037–45. [DOI] [PubMed] [Google Scholar]
- [100].O’Donnell M, Mente A, Rangarajan S, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med 2014;371:612–23. [DOI] [PubMed] [Google Scholar]
- [101].Yang SO, Jeong GH, Kim SJ, et al. Correlates of self-care behaviors among low-income elderly women with hypertension in South Korea. J Obstet Gynecol Neonatal Nurs 2014;43:97–106. [DOI] [PubMed] [Google Scholar]
- [102].Dearborn JL, McCullough LD. Perception of risk and knowledge of risk factors in women at high risk for stroke. Stroke 2009;40:1181–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Martin MY, Prayor-Patterson H, Kratt P, et al. Characteristics of insufficiently active hypertensive Black women who volunteer to be in a physical activity promotion intervention: an application of social cognitive theory and the transtheoretical model. Ethn Dis 2007;17:604–10. [PubMed] [Google Scholar]
- [104].Wiernik E, Meneton P, Empana JP, et al. Cardiovascular risk goes up as your mood goes down: Interaction of depression and socioeconomic status in determination of cardiovascular risk in the CONSTANCES cohort. Int J Cardiol 2018;262:99–105. [DOI] [PubMed] [Google Scholar]
- [105].Choi HM, Kim HC, Kang DR. Sex differences in hypertension prevalence and control: analysis of the 2010-2014 Korea National Health and Nutrition Examination Survey. PLoS One 2017;12:e0178334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [106].Chen G, Ju B, Fang H, et al. Air bearing: academic insights and trend analysis. Int J Adv Manuf 2020;106:1191–202. [Google Scholar]
- [107].He L, Fang H, Wang X, et al. The 100 most-cited articles in urological surgery: a bibliometric analysis. Int J Surg 2020;75:74–9. [DOI] [PubMed] [Google Scholar]
- [108].Chen Y, Jin Q, Fang H, et al. Analytic network process: academic insights and perspectives analysis. J Clean Prod 2019;235:1276–94. [Google Scholar]
- [109].Bao G, Pan L, Fang H, et al. Academic review and perspectives on robotic exoskeletons. IEEE Trans Neural Syst Rehabil Eng 2019;27:2294–304. [DOI] [PubMed] [Google Scholar]
- [110].Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111].Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2197–223. [DOI] [PubMed] [Google Scholar]
- [112].Mortality GBD. Causes of Death C, Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113].Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 2011;377:557–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [114].Danaei G, Finucane MM, Lu Y, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 2011;378:31–40. [DOI] [PubMed] [Google Scholar]
- [115].Whiting DR, Guariguata L, Weil C, et al. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract 2011;94:311–21. [DOI] [PubMed] [Google Scholar]
- [116].Hallal PC, Andersen LB, Bull FC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380:247–57. [DOI] [PubMed] [Google Scholar]
- [117].Guariguata L, Whiting DR, Hambleton I, et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 2014;103:137–49. [DOI] [PubMed] [Google Scholar]
- [118].Mortality GBD. Causes of Death C, Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1459–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [119].Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2014;383:245–54. [DOI] [PMC free article] [PubMed] [Google Scholar]


