Abstract
This study aimed to investigate the effectiveness of tendon suture fixation versus cortical screw fixation for the treatment of distal tibiofibular syndesmosis injury.
This study recruited 42 patients with Danis-Weber type B, C1 and C2 fractures concomitant with lower tibiofibular syndesmosis injury, who were randomly assigned to 2 groups according to treatment with cortical screw fixation (n = 21) and tendon suture fixation (n = 21). Operation time, intraoperative blood loss, time to full weight-bearing activity, medical cost, ankle function, and ankle pain were compared between the 2 groups.
The operation time was significantly less with cortical screw fixation (57.1 ± 5.3 min) than with tendon suture fixation (63.3 ± 6.3 min; p = 0.01), but there was no significant difference in intraoperative blood loss. The time until full weight-bearing was possible was significantly longer after cortical screw fixation (10.9 ± 2.7 weeks) than after tendon suture fixation (7.1 ± 1.9 weeks; P < .001). The medical cost was much greater for cortical screw fixation (1861.6 ± 187.3 USD) than for tendon suture fixation (1209.6 ± 97.6 USD; P < .01). The rate of excellent and good ankle function at 3 months after surgery was significantly higher with tendon suture fixation (71.4%) than with cortical screw fixation (33.3%; P = .03).
Tendon suture fixation is associated with quicker recovery of ankle function, shorter time to full weight-bearing, and lower medical cost to the patient compared with screw fixation. Our findings suggest that tendon suture fixation is an effective method for the treatment of tibiofibular syndesmosis injury.
Keywords: ankle fracture, screw fixation, tendon suture, tibiofibular syndesmosis injury
1. Introduction
Ankle fractures are 1 of the most common clinical fractures requiring surgical treatment.[1] Severe ankle fracture is associated with disruption of distal tibiofibular syndesmosis, and distal tibiofibular syndesmosis injury accounts for approximately 13% of all ankle fractures.[2,3] Inadequate treatment of distal tibiofibular syndesmosis injury may lead to instability of the ankle joint, persistent ankle pain, and function disability, eventually resulting in osteoarthritis.[4] Therefore, it is necessary to maintain an anatomically stable reduction and fixation for treating ankle fractures associated with distal tibiofibular syndesmosis injury.
Cortical screw fixation is the traditionally used method for treatment of distal tibiofibular syndesmosis injury.[3] Several concerns persist regarding the use of screw fixation for treating syndesmotic injury. For example, screw fixation requires removal of the implanted screws at 6 to 16 weeks after surgery, and if the screws are not removed, screw loosening and breakage, local stimulation or osteolysis may occur after weight-bearing movement of the affected limb.[5–9] Even if the screws are not broken upon weight-bearing exercise, the presence of the screws may be associated with poor ankle function.[10] Surgical removal of the screws not only increases medical costs due to reoperation, but also is associated with an increase in the complication rate by approximately 22%.[11] Therefore, it is important to identify alternatives to screw fixation for treating distal tibiofibular syndesmosis injury.
To avoid the disadvantages of cortical screw fixation related to screw removal, several studies have adopted bioabsorptive screw fixation instead of metallic screw fixation for treating distal tibiofibular syndesmosis injury and achieved satisfactory outcomes.[12–14] However, similar to metallic screw fixation, bioabsorptive screw fixation is also associated with some disadvantages such as loss of reduction and high medical costs. Recently, the suture-button fixation method has been used to treat distal tibiofibular syndesmosis injury using braided polyethylene sutures.[15] It has been reported that suture-button fixation is as effective as screw fixation mechanically and allows more flexible movement of the distal tibiofibular joint.[16,17] However, suture-button fixation can be associated with some complications such as osteolysis and subsidence of the device that require removal of the sutures,[18] and is also associated with a high incidence of soft tissue complications.[19,20] In addition, since the biomechanical sutures are relatively expensive, identifying a relatively less expensive material is necessary to reduce medical costs to patients with distal tibiofibular syndesmosis injury.
Gough et al. demonstrated that flexible sutures are biomechanically feasible for fixation of the injured distal tibiofibular syndesmotic joint in cadavers.[21] Miller et al. reported that a flexible suture is a viable alternative to screw fixation for repairing distal tibiofibular syndesmotic joint injury.[22] We modified the internal fixation method and repaired distal tibiofibular syndesmosis injuries using a tendon suture (size, 5; Covidien). This suture has some advantages such as low cost, good biomechanical strength, and high biocompatibility and is widely used in orthopedic surgeries. However, it remains unclear whether tendon suture fixation is effective for treating distal tibiofibular syndesmosis injury. The purpose of this study was to investigate the effectiveness of tendon suture fixation in the treatment of distal tibiofibular syndesmosis injury in comparison with cortical screw fixation.
2. Methods
2.1. Patients
The study was approved by the Medical Ethics Committee of People's Hospital of Pengzhou City, and all patients gave their informed consent prior to their inclusion in the study. This prospective case-control study recruited 42 consecutive patients with distal tibiofibular syndesmosis injury, who visited our hospital between January 2014 and July 2017. Power analysis was performed with a power value >0.95, and thus the study had enough statistical power to validate the stengthth of the conclusion. Patients with a type B, C1 or C2 fracture according to the Danis-Weber classification were included in the study. The exclusion criteria were as follows:
-
(1)
preoperative T score <–2.5 measured by dual-energy x-ray absorptiometry;
-
(2)
body mass index >25 kg/m2;
-
(3)
no instability of the tibiofibular syndesmosis on intraoperative Cotton tests;
-
(4)
no recovery of the tibia to normal length after surgery; and
-
(5)
no postoperative anatomical reduction of the medial malleolus, lateral malleolus or posterior malleolus.
The patients were randomly assigned to 2 groups using a random number table for treatment with: cortical screw fixation (n = 21) or tendon suture fixation (n = 21). The treatment options were informed to the patient prior to the surgery, and the final treatment was decided by the patient if the random treatment method was not accepted by the patient. All patients underwent measurement of bone density by a double-energy X-ray absorptiometry, X-ray radiography to observe the anterioposterior and lateral views of the ankle joint, and computed tomography (CT) examination of the ankle joint preoperatively.
2.2. Surgical approaches
All patients underwent either continuous epidural anesthesia or combined spinal anesthesia. For patients with contraindications for theses anesthesia procedures, general anesthesia was performed. The patient was placed in a supine position. After exposure of the fracture, the medial malleolus fracture was first reduced, and the deltoid ligament was repaired if necessary. For patients without medial malleolus fracture, the deltoid ligament was repaired after exploration. Then, the lateral malleolus or the fibula was reduced and fixed. If preoperative radiologic findings showed separation of the tibiofibular syndesmosis, especially for the Danis-Weber type C1 and C2 fractures, cortical screw fixation or tendon suture fixation was performed to repair the tibiofibular syndesmosis injury. If preoperative radiologic findings showed no obvious separation of the tibiofibular syndesmosis, especially for Danis-Weber type B fractures, intraoperative Cotton test was performed by lateral pull of the fibula using a bone tenaculum. If obvious instability of the tibiofibular syndesmosis occurred, cortical screw fixation or tendon suture fixation was performed. If no obvious instability of the tibiofibular syndesmosis was found, intraoperative C-arm X-ray imaging was performed during the Cotton test. Widening of the tibiofibular space on the X-ray images indicated the instability of the tibiofibular syndesmosis, and cortical screw fixation or tendon suture fixation was performed. After fixation, C-arm X-ray imaging was performed again to confirm the stability of the tibiofibular syndesmosis, and reduction and fixation of the posterior malleolar fracture was performed if the patient had the following signs:
-
1)
fracture areas accounted for >25% to 30% of the inferior articular surface of the tibia,
-
2)
subluxation or dynamic instability of the ankle joint; and
-
3)
>2 to 3 mm step-off of the inferior articular surface of the tibia. When the stability of the tibiofibular syndesmosis and recovery of the normal anatomic structure of the ankle were achieved, the incision was cleaned and closed in layers after placement of a drainage tube.
For patients who underwent cortical screw fixation, the ankle was placed in a 5-degree dorsiflexion position. A 3.5-mm cortical screw was inserted at 2 to 3 cm above the articular surface of the distal tibia and passed through the fibula. If a plate was placed lateral to the fibula, the cortical screw was passed through the plate hole, angling 20 to 30 degrees posteroanteriorly in the horizontal plane and paralleling the articular surface of the distal tibia. Depending on the resistance upon inserting the screw, 3 cortices, including 2 cortices of the fibula and the lateral cortex of the tibia (commonly used), or 4 cortices, including 2 cortices of both the fibular and tibia, were fixed.
For patients who underwent tendon suture fixation, the ankle was placed in a 5-degree dorsiflexion position. Two holes at a distance of approximately 1 cm were drilled at 2 to 3 cm above the articular surface of the distal tibia, passing through the fibula and angling 25 to 30 degrees posteroanteriorly in the horizontal plane. An incision was made at the medial side of the fibula to facilitate the passage of a tendon suture. A tendon suture (size, 5; Ti-CronTM nonabsorbable coated braided polyester suture; Covidien) was passed through the 2 holes and knotted at the lateral side of the fibula. If a plate was placed lateral to the fibula, the tendon suture was passed through the plate hole and knotted there (Fig. 1).
Figure 1.
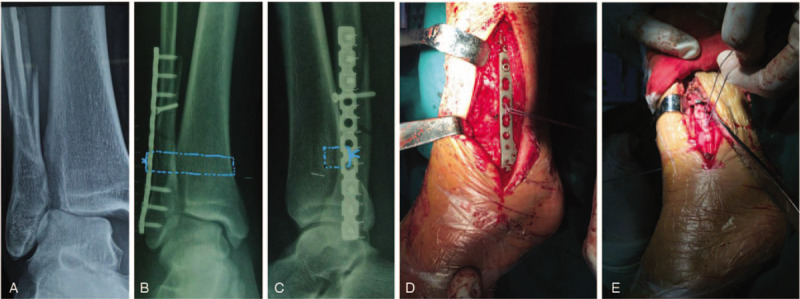
Surgical procedures for patients with tendon suture fixation. A, B. Preoperative (A) and postoperative (B) anterioposterior X-ray images of the ankle joint. Blue lines indicate the position of the tendon suture used to fix the tibiofibular syndesmosis injury. C. Postoperative lateral X-ray image of the ankle joint. Blue lines indicate the knot of the tendon suture at the plate placed lateral to the fibula. D. Intraoperative photograph showing that the tendon suture was knotted at the plate placed lateral to the fibula. E. Intraoperative photograph showing that the tendon suture was knotted at the lateral side of the fibula.
2.3. Postoperative management
At 1 day after surgery, the patient was instructed to actively flex and extend the hip, knee, and ankle joints of the affected limb. Based on the patient's pain tolerance, the patient was encouraged to get out of the bed and move with crutches, but weight-bearing movement of the affected limb was not allowed. The patient was discharged at 3 to 10 days after surgery, and was followed up every 1 to 2 weeks at the Outpatient department. At 6 weeks after surgery, the patient started gradual weight-bearing movement of the affected limb until full weight-bearing exercise was achieved. For patients treated with cortical screw fixation, the syndesmotic screw was removed at 12 weeks after surgery.
2.4. Patient follow-up
The operation time, volume of blood loss during surgery, the time to full weight-bearing activity, and the medical cost were recorded. The patients were followed up at 3 days, 3 months, and 6 months after surgery. During the follow-up period, all patients underwent X-ray radiography of the ankle. Ankle function was evaluated using the Baird-Jackson ankle scoring system (including pain, ankle joint function, and ankle X-ray radiograph) as follows: excellent, 96 to 100; good, 91 to 95; fair, 81 to 90; and poor, <80.[23] Ankle pain was evaluated using visual analog scale (VAS). Postoperative complications were also recorded, including wound infection, skin irritation or necrosis, non-healing fracture, loosening and breakage of internal fixation, and re-separation of the tibiofibular syndesmosis.
2.5. Statistical analysis
Statistical analyses were performed using SPSS 18.0 (SPSS Inc., Chicago, IL). Quantitative data are expressed as means ± standard deviation. Analysis of variance was used to identify differences in the means among groups. The Mann-Whitney test was used to identify a difference in ankle function between the 2 groups. A P value <.05 was considered statistically significant.
3. Results
A total of 42 patients with lower tibiofibular syndesmosis injury were enrolled in this study. Of the 42 patients, 31 patients were male, and 11 patients were female. The causes of distal tibiofibular syndesmosis injury included fall injury in 20 cases, automobile accident in 13 cases, sprain in 5 cases, falling from a height in 3 cases, and crush injury by a heavy object in 1 case. The average time between the injury and operation was 7.4 ± 2.6 days (range, 2–13 days). The average age of the patients was 37.2 ± 10.5 years (range, 19–64 years). Of the 42 patients, 21 patients received cortical screw fixation, and the other 21 patients received tendon suture fixation. There were no significant differences in age, sex, and type of fracture between the 2 groups (P > .05, Table 1).
Table 1.
Baseline characteristics of the patients in the 2 treatment groups (group A = cortical screw fixation group, group B = tendon suture fixation group).

The operation time, volume of blood loss during surgery, time to full weight-bearing activity, and medical cost were compared between the groups treated with cortical screw fixation and tendon suture fixation (Table 2). There was no significant difference in intraoperative blood loss between the 2 groups (97.0 ± 26.5 ml for screw fixation vs 97.1 ± 24.3 mL for suture fixation; P > .05). However, the operation time was significantly less for screw fixation (57.1 ± 5.3 minute) than for suture fixation (63.3 ± 6.3 min; P = .01). In addition, the time to full weight-bearing activity was 10.9 ± 2.7 months after screw fixation, which was significantly longer than that after suture fixation (7.1 ± 1.9 months; P < .001). The average medical cost was 1861.6 ± 187.3 USD for screw fixation, which was much greater than that for suture fixation (1209.6 ± 97.6 USD; P < .01).
Table 2.
Intraoperative and postoperative results for the 2 treatment groups.

We then compared ankle function at 3 days, 3 months, and 6 months after surgery between the 2 groups (Table 3). According to the Baird–Jackson ankle scoring system, at 3 days after surgery, the ankle function was good in 2 cases, fair in 11 cases, and poor in 8 cases of the cortical screw fixation group, resulting in a rate of excellent and good function of 9.5% (2/21). The same rate of excellent and good function (9.5%, 2/21) was found in the tendon suture fixation group (Table 3). However, at 3 months after surgery, ankle function was excellent in 7 cases, good in 8 cases, fair in 4 cases, and poor in 2 cases in the tendon suture fixation group, for a rate of excellent and good function of 71.4% (15/21), which was significantly higher than that in the screw fixation group (33.3%, 7/21; P = .03, Table 3). At 6 months after surgery, the rate of excellent and good function was comparable between the 2 groups (85.7% [18/21] with screw fixation vs 90.5% [19/21] with tendon fixation; P > .05, Table 3).
Table 3.
Ankle function at 3 d, at 3mo, and 6 mo after surgery.

We compared the patients’ ankle pain at 3 days, 3 months, and 6 months after surgery between the 2 groups (Table 4). The VAS scores at 3 days after surgery were not significantly different between the 2 groups (P > .05). However, at 3 months after surgery, the mean VAS score was significantly less in the suture fixation group compared with the screw fixation group (P = .005). At 6 months after surgery, the VAS scores again were not significantly different between the 2 groups (P > .05).
Table 4.
Postoperative pain at 3 d, 3 mo, and 6 mo after surgery.

Of all 42 cases, no skin necrosis, non-healing fracture, loosening of internal fixation, and re-separation of the tibiofibular syndesmosis occurred. In the screw fixation group, skin redness and tenderness occurred at postoperative 12 week after the screw was removed in 1 patient who had normal values for C reactive protein and routine blood tests. The wound had healed at 2 weeks after dressing change with no sinus formation. In the suture fixation group, subcutaneous nodules at the knot site occurred at 4 weeks after surgery in 1 patient. The suture knot was palpitated on the surface of the skin, and the skin was not broken. The tendon suture was removed under local anesthesia at 12 weeks after surgery. The wound had healed at 2 weeks after dressing change with no sinus formation. In addition, screw breakage occurred in 1 case in the screw fixation group. The tibiofibular space was not widened, and the ankle functioned well.
4. Discussion
Although screw fixation is the traditional method for treating distal tibiofibular syndesmosis injury,[24,25] use of suture-button fixation has recently increased in clinical practice. In the present study, we used a tendon suture (size, 5; Covidien) to fix distal tibiofibular syndesmosis and compared the effectiveness of this tendon suture fixation with cortical screw fixation for the treatment of distal tibiofibular syndesmosis injury. We found that in comparison with cortical screw fixation, tendon suture fixation was associated with a shorter time to full weight-bearing activity, quicker recovery of ankle function, and reduced ankle pain at 3 months after surgery. In addition, the medical cost for patients was significantly lower with tendon suture fixation compared with cortical screw fixation. Although the operation time was significantly less for screw fixation (57.1 ± 5.3 min) than for suture fixation (63.3 ± 6.3 min; P = .01), the 6-minute difference is not clinically relevant. Our study suggests that tendon suture fixation is an effective fixation method for surgical repair after distal tibiofibular syndesmosis injury and may be used as an alternative to cortical screw fixation.
A long and stable fixation is important for repair after distal tibiofibular syndesmosis injury, because repair of the fracture and injured ligament in the tibia and fibula is a slow process due to the poor blood supply to the tibiofibular joint.[26] Therefore, in clinical practice, the patient is commonly instructed to avoid all weight-bearing movement of the affected limb for at least 12 weeks after surgery.[8] The screws are commonly removed at 12 to 16 weeks after surgery. Otherwise, the screw is likely to be broken upon weight-bearing exercise, resulting in loss of internal fixation and separation of the tibiofibular syndesmosis.[27] Even though it has been reported that screw breakage has no effect on the recovery of ankle function,[28] broken screws are commonly not accepted by the patient if not removed. In addition, surgical removal of the screw becomes more difficult after postoperative 12 weeks.[27] Liu et al recommended that the screw should be removed as early as possible after the ankle fracture has healed.[29] Therefore, in this present study, the screws were removed at 12 weeks after surgery for all patients treated with cortical screw fixation.
Weight-bearing movement of the affected limb improves the recovery of ankle function, as long-term non-weight bearing mobilization can result in rigidity of the ankle joint, which delays the recovery time. Kocadal et al. used CT imaging to investigate the reduction performance of screw fixation and found that the use of screw fixation resulted in a poor restoration of the fibular rotation in the treatment of syndesmotic injuries.[30] Because normal ankle function requires external rotation and posterior displacement of the distal fibula,[31] screw fixation restricts the movement of normal motion of the fibula, thus limiting the biomechanical function of the ankle. Therefore, recent studies have tried to identify new alternative fixation methods to replace screw fixation for the treatment of distal tibiofibular syndesmosis injury.
Several fixation methods such as suture-button fixation, tightrope fixation, and syndesmotic hook fixation have been used in the treatment of distal tibiofibular syndesmosis injury, and satisfactory outcomes have been achieved using these methods.[25,32,33] Recently, suture-button techniques have been popularized for the treatment of distal tibiofibular syndesmosis injury, and several studies have reported that suture-button fixation can achieve satisfactory outcomes.[25,33–38] A recent systematic review reported that suture-button fixation is associated with a better objective range of motion, an earlier return to work, and lower rates of implant removal, implant failure, and malreduction, compared with screw fixation, though similar functional outcomes as measured by the AOFAS score and postoperative complication rates were found.[15] In addition, a meta-analysis by Gan et al has reported that dynamic fixation using suture-button fixation results in similar clinical outcomes for the treatment of distal tibiofibular syndesmosis injury compared with static fixation using screw fixation but is associated with a reduced requirement for secondary intervention.[39] In this study, we used tendon suture fixation for the treatment of distal tibiofibular syndesmosis injury and found that, in comparison with screw fixation, tendon suture fixation was associated with a similar clinical outcome at 6 months after surgery, but quicker ankle function recovery and reduced ankle pain at 3 months after surgery.
Recently, Wang et al reported that a novel elastic bionic fixation provided stable and reliable fixation with good functional recovery and relatively fewer complications in the treatment of distal tibiofibular syndesmosis injury.[40] However, these new biomechanical materials are relatively expensive and may be associated with some unknown complications. Therefore, it is necessary to identify an effective fixation method that is associated with low medical costs and easy to put into widespread use. In the present study, we selected a tendon suture (size, 5; Covidien) for fixation of distal tibiofibular syndesmosis, because this tendon suture has been demonstrated to have sufficient strength and biocompatibility in clinical use for treating conditions with high tension such as knee ligament injuries, Achilles tendon injuries, and tibial fractures. The tendon suture is not absorptive and thus can maintain persistent strength for fixing the tibiofibular joint for an extended time. The flexible biomechanical properties of the tendon suture enable normal movement of the distal fibula and avoid the shear force caused by the screw. However, because the tendon suture is thick and smooth, and at least 3 knots are required to provide sufficient fixation, subcutaneous nodules caused by the suture knots may occur in thin patients, and removal of the tendon suture may be required. In the present study, subcutaneous nodules formed in only 1 thin patient, and removal of the suture was performed in this patient.
In the present study, we also found that the use of the tendon suture fixation reduced the medical cost to the patient by approximately 650 USD compared with screw fixation. This lower medical cost may be due to the cheaper cost of the tendon suture and the cost saving of avoiding a second operation for screw removal. In addition, we also found that complications occurred in 2 cases with screw fixation, and only 1 case with tendon suture fixation. Fewer complications may also reduce the medical cost to the patient.
This study has some limitations. First, MRI and CT, which offer greater accuracy in the diagnosis and evaluation of distal tibiofibular syndesmosis injury,[41,42] were not used. Only X-ray radiography was performed for all patients in order to reduce the medical costs to the patients. In addition, during operation, a cortical screw or tendon suture was used to fix the fibula to the tibia in order to avoid rotation and dislocation of the fibula on the longitudinal axis. We also excluded the patients who had no postoperative anatomical reduction. Thus, all patients met the following criteria for anatomical reduction:
-
(1)
anterioposterior X-ray image showing the medial joint gap was ≤4 mm and the upper joint gap was ≤2 mm;
-
(2)
the inferior tibiofibular joint space was < 5 mm, and the overlay between the anterior tibial tubercle and the fibula was ≥10 mm; and
-
(3)
the fibula was not shortened, rotated, or angled.
Because no case showed rotation and dislocation of the fibula, and all cases achieved anatomical reduction, we think that X-ray imaging provides sufficient follow-up information without a need for routine CT imaging. Second, the sample size of this study was relatively small (n = 21 per group). Future studies with a larger sample size are needed to confirm the findings of this study. Third, the patients were followed up for a relative short period (6 months). Further study with a long-term follow-up period is required to investigate the effectiveness of tendon suture fixation for the treatment of tibiofibular syndesmosis injury.
In summary, we compared the effectiveness of tendon suture fixation versus cortical screw fixation for the treatment of tibiofibular syndesmosis injury and found that tendon suture fixation was associated with quicker recovery of ankle function, reduced ankle pain, shorter time to full weight-bearing activity, and lower medical cost to the patient compared with screw fixation. Our findings suggest that tendon suture fixation is an effective fixation method for the treatment of tibiofibular syndesmosis injury.
Author contributions
XXXX.
Footnotes
Abbreviation: CT = computed tomography.
How to cite this article: Song L, Liao Z, Kuang Z, Qu S, Zhang W, Yuan Y, Fang T. Comparison of tendon suture fixation and cortical screw fixation for treatment of distal tibiofibular syndesmosis injury: a case-control study. Medicine. 2020;99:34(e21573).
Pengzhou People's Hospital and Sichuan Health Commission jointly contributed 20,000 yuan ($2797), This work was supported by Sichuan Health and Health Commission.
Conflict of interest statement: The authors of this work have nothing to disclose.
All patients gave their informed consent prior to their inclusion in the study.
The study was approved by the Medical Ethics Committee of People's Hospital of Pengzhou City.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Goost H, Wimmer MD, Barg A, et al. Fractures of the ankle joint: investigation and treatment options. Dtsch Arztebl Int 2014;111:377–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Fong DT, Hong Y, Chan LK, et al. A systematic review on ankle injury and ankle sprain in sports. Sports Med 2007;37:73–94. [DOI] [PubMed] [Google Scholar]
- [3].Dattani R, Patnaik S, Kantak A, et al. Injuries to the tibiofibular syndesmosis. J Bone Joint Surg Br 2008;90:405–10. [DOI] [PubMed] [Google Scholar]
- [4].Porter DA. Evaluation and treatment of ankle syndesmosis injuries. Instr Course Lect 2009;58:575–81. [PubMed] [Google Scholar]
- [5].Veen EJ, Zuurmond RG. Mid-term results of ankle fractures with and without syndesmotic rupture. Foot Ankle Surg 2015;21:30–6. [DOI] [PubMed] [Google Scholar]
- [6].Hsu YT, Wu CC, Lee WC, et al. Surgical treatment of syndesmotic diastasis: emphasis on effect of syndesmotic screw on ankle function. Int Orthop 2011;35:359–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Miller AN, Paul O, Boraiah S, et al. Functional outcomes after syndesmotic screw fixation and removal. J Orthop Trauma 2010;24:12–6. [DOI] [PubMed] [Google Scholar]
- [8].Bell DP, Wong MK. Syndesmotic screw fixation in Weber C ankle injuries--should the screw be removed before weight bearing? Injury 2006;37:891–8. [DOI] [PubMed] [Google Scholar]
- [9].Schepers T. To retain or remove the syndesmotic screw: a review of literature. Arch Orthop Trauma Surg 2011;131:879–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Manjoo A, Sanders DW, Tieszer C, et al. Functional and radiographic results of patients with syndesmotic screw fixation: implications for screw removal. J Orthop Trauma 2010;24:2–6. [DOI] [PubMed] [Google Scholar]
- [11].Schepers T, Van Lieshout EM, de Vries MR, et al. Complications of syndesmotic screw removal. Foot Ankle Int 2011;32:1040–4. [DOI] [PubMed] [Google Scholar]
- [12].Ahmad J, Raikin SM, Pour AE, et al. Bioabsorbable screw fixation of the syndesmosis in unstable ankle injuries. Foot Ankle Int 2009;30:99–105. [DOI] [PubMed] [Google Scholar]
- [13].Cox S, Mukherjee DP, Ogden AL, et al. Distal tibiofibular syndesmosis fixation: a cadaveric, simulated fracture stabilization study comparing bioabsorbable and metallic single screw fixation. J Foot Ankle Surg 2005;44:144–51. [DOI] [PubMed] [Google Scholar]
- [14].Thordarson DB, Samuelson M, Shepherd LE, et al. Bioabsorbable versus stainless steel screw fixation of the syndesmosis in pronation-lateral rotation ankle fractures: a prospective randomized trial. Foot Ankle Int 2001;22:335–8. [DOI] [PubMed] [Google Scholar]
- [15].Zhang P, Liang Y, He J, et al. A systematic review of suture-button versus syndesmotic screw in the treatment of distal tibiofibular syndesmosis injury. BMC Musculoskelet Disord 2017;18:286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Forsythe K, Freedman KB, Stover MD, et al. Comparison of a novel FiberWire-button construct versus metallic screw fixation in a syndesmotic injury model. Foot Ankle Int 2008;29:49–54. [DOI] [PubMed] [Google Scholar]
- [17].Soin SP, Knight TA, Dinah AF, et al. Suture-button versus screw fixation in a syndesmosis rupture model: a biomechanical comparison. Foot Ankle Int 2009;30:346–52. [DOI] [PubMed] [Google Scholar]
- [18].Degroot H, Al-Omari AA, El Ghazaly SA. Outcomes of suture button repair of the distal tibiofibular syndesmosis. Foot Ankle Int 2011;32:250–6. [DOI] [PubMed] [Google Scholar]
- [19].Welck MJ, Ray P. Tibialis anterior tendon entrapment after ankle tightrope insertion for acute syndesmosis injury. Foot Ankle Spec 2013;6:242–6. [DOI] [PubMed] [Google Scholar]
- [20].Naqvi GA, Shafqat A, Awan N. Tightrope fixation of ankle syndesmosis injuries: clinical outcome, complications and technique modification. Injury 2012;43:838–42. [DOI] [PubMed] [Google Scholar]
- [21].Gough BE, Chong AC, Howell SJ, et al. Novel flexible suture fixation for the distal tibiofibular syndesmotic joint injury: a cadaveric biomechanical model. J Foot Ankle Surg 2014;53:706–11. [DOI] [PubMed] [Google Scholar]
- [22].Miller RS, Weinhold PS, Dahners LE. Comparison of tricortical screw fixation versus a modified suture construct for fixation of ankle syndesmosis injury: a biomechanical study. J Orthop Trauma 1999;13:39–42. [DOI] [PubMed] [Google Scholar]
- [23].Baird RA, Jackson ST. Fractures of the distal part of the fibula with associated disruption of the deltoid ligament. Treatment without repair of the deltoid ligament. J Bone Joint Surg Am 1987;69:1346–52. [PubMed] [Google Scholar]
- [24].Wu ZP, Chen PT, He JS, et al. Classification and treatment of syndesmotic injury. Zhongguo Gu Shang 2018;31:190–4. [DOI] [PubMed] [Google Scholar]
- [25].Schepers T. Acute distal tibiofibular syndesmosis injury: a systematic review of suture-button versus syndesmotic screw repair. Int Orthop 2012;36:1199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Warchol L, Mroz I, Mizia E, et al. Vascular density of inferior tibiofibular joint - cadaveric experimental study. Folia Med Cracov 2017;57:47–54. [PubMed] [Google Scholar]
- [27].Melvin JS, Downing KL, Ogilvie CM. A technique for removal of broken cannulated tricortical syndesmotic screws. J Orthop Trauma 2008;22:648–51. [DOI] [PubMed] [Google Scholar]
- [28].Stuart K, Panchbhavi VK. The fate of syndesmotic screws. Foot Ankle Int 2011;32:S519–525. [DOI] [PubMed] [Google Scholar]
- [29].Liu Q, Zhao G, Yu B, et al. Effects of inferior tibiofibular syndesmosis injury and screw stabilization on motion of the ankle: a finite element study. Knee Surg Sports Traumatol Arthrosc 2016;24:1228–35. [DOI] [PubMed] [Google Scholar]
- [30].Kocadal O, Yucel M, Pepe M, et al. Evaluation of reduction accuracy of suture-button and screw fixation techniques for syndesmotic injuries. Foot Ankle Int 2016;37:1317–25. [DOI] [PubMed] [Google Scholar]
- [31].Beumer A, Valstar ER, Garling EH, et al. Kinematics of the distal tibiofibular syndesmosis: radiostereometry in 11 normal ankles. Acta Orthop Scand 2003;74:337–43. [DOI] [PubMed] [Google Scholar]
- [32].Fei J, Lai Z, Wei W, et al. Biomechanical study on different internal fixation methods of joint stability reconstruction of distal tibiofibular syndesmosis injury. Zhongguo Gu Shang 2015;28:1147–52. [PubMed] [Google Scholar]
- [33].Colcuc C, Blank M, Stein T, et al. Lower complication rate and faster return to sports in patients with acute syndesmotic rupture treated with a new knotless suture button device. Knee Surg Sports Traumatol Arthrosc 2018;26:3156–64. [DOI] [PubMed] [Google Scholar]
- [34].Inge SY, Pull Ter Gunne AF, Aarts CAM, et al. A systematic review on dynamic versus static distal tibiofibular fixation. Injury 2016;47:2627–34. [DOI] [PubMed] [Google Scholar]
- [35].Clanton TO, Whitlow SR, Williams BT, et al. Biomechanical comparison of 3 current ankle syndesmosis repair techniques. Foot Ankle Int 2017;38:200–7. [DOI] [PubMed] [Google Scholar]
- [36].Teramoto A, Suzuki D, Kamiya T, et al. Comparison of different fixation methods of the suture-button implant for tibiofibular syndesmosis injuries. Am J Sports Med 2011;39:2226–32. [DOI] [PubMed] [Google Scholar]
- [37].Klitzman R, Zhao H, Zhang LQ, et al. Suture-button versus screw fixation of the syndesmosis: a biomechanical analysis. Foot Ankle Int 2010;31:69–75. [DOI] [PubMed] [Google Scholar]
- [38].Thornes B, Shannon F, Guiney AM, et al. Suture-button syndesmosis fixation: accelerated rehabilitation and improved outcomes. Clin Orthop Relat Res 2005;207–12. [PubMed] [Google Scholar]
- [39].Gan K, Zhou K, Hu K, et al. Dynamic fixation versus static fixation for distal tibiofibular syndesmosis injuries: a meta-analysis. Med Sci Monit 2019;25:1314–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Wang L, Zhang Y, Song Z, et al. A novel method of using elastic bionic fixation device for distal tibiofibular syndesmosis injury. Int Orthop 2018;42:2219–29. [DOI] [PubMed] [Google Scholar]
- [41].Sman AD, Hiller CE, Refshauge KM. Diagnostic accuracy of clinical tests for diagnosis of ankle syndesmosis injury: a systematic review. Br J Sports Med 2013;47:620–8. [DOI] [PubMed] [Google Scholar]
- [42].Han SH, Lee JW, Kim S, et al. Chronic tibiofibular syndesmosis injury: the diagnostic efficiency of magnetic resonance imaging and comparative analysis of operative treatment. Foot Ankle Int 2007;28:336–42. [DOI] [PubMed] [Google Scholar]


