Abstract
Traumatic end plate fractures (EPFs) refers to the EPF caused by trauma, rather than the pathological status of the end plate (EP). However, some old traumatic EPFs may be mistaken as osteoporotic in the elderly. The objective of this study is to describe the radiological features of traumatic EPF in different traumatic fracture type patients presenting in the Emergency department setting. And to compare the result with osteoporotic vertebral fracture (VF).
This study retrospectively analyzed the anatomical location of acute thoracolumbar vertebral traumatic EPFs in males (age≤55 years) and females (age≤50 years). The anatomic distribution of EPFs, the anterior and posterior wall fracture were analyzed in patients, who were scanned with 1 or more of the following methods: radiography, CT, and magnetic resonance imaging.
There were 194 cases of acute spine trauma involving at least 1 EPF, including 118 males and 76 females. The involved vertebra was mostly at L1 (29.7%), followed by T12 (18.3%), and then by L2 (12.9%). Excluding those with both upper and lower EP involvements, the ratio of superior EPF to inferior EPF was 33.5 for males and 45.5 for females. With the EP divided into 5 segments of equal length in the anteroposterior direction in different fracture types, fractures occurred mostly at a2 segment (71.48% for superior EPs and 7.60% for inferior EPs), followed by a1 segment (66.16% for superior EPs). The upper third of the anterior and posterior walls were most prone to fracture in traumatic vertebral fracture.
Traumatic EPFs more likely involve the anterior EP more than the posterior EP and is correlated with fracture type. These characteristics may help radiologist differential diagnosis between traumatic and osteoporotic EPF.
Keywords: end plate, epidemiology, traumatic, traumatic fractures
1. Introduction
Traumatic end plate fracture (EPF) refers to the EPF caused by trauma, rather than the pathological status of the end plate (EP). It is mainly need to differentiated from the osteoporosis EPF, which is characterized by low bone density and microstructure degradation, leading bone to fracture in a low-energy.[1]
Currently the radiological diagnostic criteria and classification of vertebral fractures (VF) are still controversial.[2] The semi-quantitative criteria proposed by Genant et al,[3] is commonly used in vertebral height reduction, in which the importance of loss of EP integrity is emphasized, but did not make diagnosis on this sign.[3,4] The algorithm-based qualitative (ABQ) approach, described by Jiang et al[5,6] initially, explained that the EP is a 100% sensitive finding in diagnosis VF, while vertebral height loss is not an indispensable indicator for VF. Recently, Wang[7] proposed a modified semi-quantitative grading, in which the percentage reduction in vertebral height was retained and the percentage reduction in vertebral area was removed.
The EP is the weakest part of the vertebral body, consisting of perforated cortical bone with a stratum of cartilage attached to the intervertebral disc surface. The thickness of the EP varies greatly, which may be related to vertebral segments and age. Even in the same vertebral the thickness of different parts is also asymmetric, and it is easy to fracture after trauma. However, the EP plays an important role in maintaining the structural integrity, in balancing biomechanical forces and supplying nutrition. Many scholars discussed the stress distribution and fracture characteristics of the EP from the aspects of cadaver specimens or finite element study, but few literature articles analyzed the clinical and imaging characteristics of the EPFs. It is important to identify and report EPF accurately and clearly, so that appropriate treatment and research can be initiated. What is more, traumatic VFs could present with minor symptoms at the time of injury, or symptoms may have been neglected, due to other injuries at the same time.[8] In this situation, some traumatic VFs in the aged may be mistakenly diagnosed as osteoporotic and cured by relative drugs, so we need to analyze characteristic of EPFs between osteoporotic and traumatic VFs.
The objective of this study is to describe the prevalence, distribution of traumatic EPFs in different traumatic fracture type patients presenting in the emergence department setting. And to compare the result with osteoporotic VF.[1]
2. Methods
From January 2017 to December 2018, patients with acute thoracolumbar vertebral EPFs admitted to Ningbo First Hospital, Ningbo Second Hospital, and Ningbo Women and Children's Hospital due to trauma were retrospectively analyzed. Male patients aged 55 or below and female patients aged 50 or below were recruited.
Institutional Review Board approval and patient consent for the use of clinical and radiological imaging records were obtained for this study.
2.1. Exclusion criteria
-
1)
Spine surgery had been done
-
2)
A T-value measure of –2.5 DS or less at the spine or femoral neck using dual-energy X-ray absorptiometry.
-
3)
A known malignancy (metastasis or myeloma) or infection or tuberculosis disease of spine.
-
4)
Has the underlying causes of osteoporosis including cortisol medication, menopause, and hyperthyroidism.
All patients were scanned with 1 or more of the following methods: left lateral and anteroposterior radiographs, CT, and MR. And 13 cases were excluded due to poor image quality, mainly including motion artifacts and insufficient exposure of radiograph; 8 cases were excluded because hormone therapy, 4 cases were associated with myeloma or metastatic tumor, 10 cases were excluded due to osteoporosis.
Their spine imaging examinations were performed on different imaging scanners in different hospitals. All patients underwent spine MR imaging on 1.5T (Siemens magnetom sonata and Siemens magnetom avanta). The sequences that were analyzed included T1-weighted fast spin-echo of sagittal images, T2-weighted fast spin-echo of sagittal and axial images, with or without fat-suppression. Some patients underwent spine CT on a 64-slice multidetector CT scanner (Simens somatom), some patients on 16-slice multidetector CT scanner (Philips Brilliance and LightSpeed of GE Healthcare).
2.2. Radiological assessment
-
1)
The height loss followed the criteria of Wang[7] modified semi-quantitative grading, vertebral height loss was classified according to less than 20% height loss, 20% to 34% height loss, and more than 34% loss. (The vertebral height loss was defined by subtracting the height of the fractured vertebra at the point of maximum loss from the average height of the vertebrae above and below the injured one and dividing the value by the average height).
-
2)
EPF was defined by the presence of EP cortical discontinuity or angulation on radiographs, sagittal, or coronal position of CT and magnetic resonance imaging (MRI), or disk material intrusion into the EP. For the assessment of the location of EPF on sagittal position, the EP was magnified and compared with a ruler and divided into 5 equal segments (from anterior to posterior were: a1, a2, m, p2, p1), EPFs involving 1 or more segments were recorded from the upper and lower EPs (Fig. 1).
-
3)
The VFs types were based on the 3 columns model of Denis,[9] which included compression, burst, flexion-distraction, and fracture-dislocation types.
Figure 1.
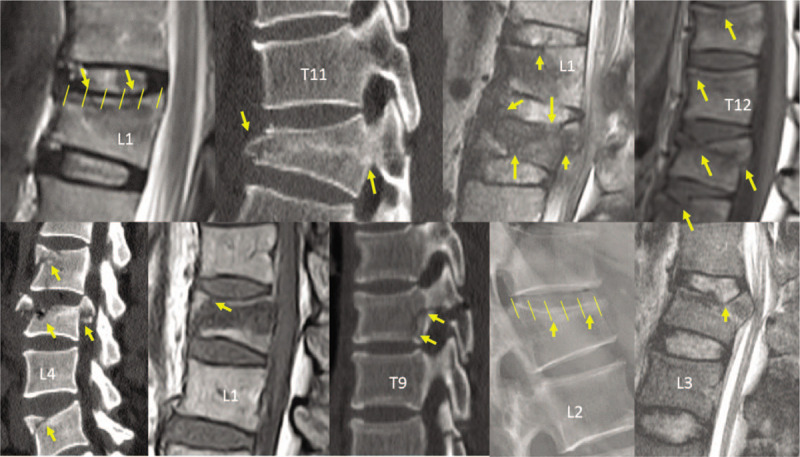
The end plate was divided into 5 equal segments in both superior and inferior end plates. Examples of vertebral end plate fracture (various arrows) identified by radiograph, CT, or magnetic resonance imaging.
Compression fractures are characterized by a merely failure of the anterior column. The posterior vertebral wall and spinal canal are intact.
Burst fractures result in failure of the anterior and middle columns. Its radiographic finding includes fracture of the posterior vertebral wall, loss height of the anterior, and posterior vertebral with vertebral body retropulsion into the canal from either or both EPs.
Flexion-distraction fractures are characterized by all 3 columns are affected. Distraction means divided into 2 parts. The middle and posterior columns, with the anterior column acting as a pivot (this will help to differentiate from the type of fracture-dislocation, in which the pivot is also fractured). Their typical radiographic signs include widening distance of interspinous, transverse fractures through posterior body and/or pedicles and increase height of posterior intervertebral disc and/or posterior vertebral body.
Fracture-dislocation injuries are failure of all columns, which lead vertebral body to subluxation or dislocations, and the posterior wall of the vertebral body can be normal when dislocation goes through the disc.
-
4)
The percentage of anterior wall and posterior wall fractures.
The anterior wall fractures appeared 1 of the following types: protruded, concave, inserted, and sequestered. Both anterior and posterior walls were divided into upper, middle, and lower parts, and fracture could involve 1 or more segments.
During the analysis of fracture type, EPFs location and anterior/posterior wall fracture, the reading was double-checked by an experienced radiologist, and then another radiologist experienced in VF reading was available for consultation and discussion during triple-checking, and the clinical data were hidden when viewed those images. Our intra-reader agreement Kappa was tested to 0.92 for the EPFs in CT, 0.85 in radiograph, 0.88 in MRI, which was higher than the result of Nazimi et al.[1]
SPSS 24.0 (SPSS Inc., IL) was used for statistical analysis, and P < .05 was considered statistically significant. Prevalence of EPFs was compared among 4 fracture type groups by using Chi-squared test for trend. Prevalence was compared between sex by using Chi-squared test of independence.
3. Results
There were 194 cases of acute spine trauma involving at least 1 EPF, including 118 males and 76 females. The mean age was 42.11 ± 9.82 years (range: 13–55 years). Among them 27 cases were ≤30 years; 36 cases were 30 to 40 years; 83 cases were 40 to 50 years; and 48 cases were ≥50 years. There were a total of 263 VFs, including 28 patients with 2 VFs, and 13 patients with 3 VFs, 2 patients with 4 VFs, and the remaining 3 cases had 5, and 6 VFs respectively.
The causes of the trauma included 134 cases of traffic accident (car, motorbike, and bicycle collision), 49 cases of fall, 5 cases of heavy objects hitting, 3 cases of sports (yoga and football) injuries, 1 case of elevator clamp injury, and 2 cases of unknown reasons.
3.1. The anatomical distribution of VF (Fig. 2)
Figure 2.
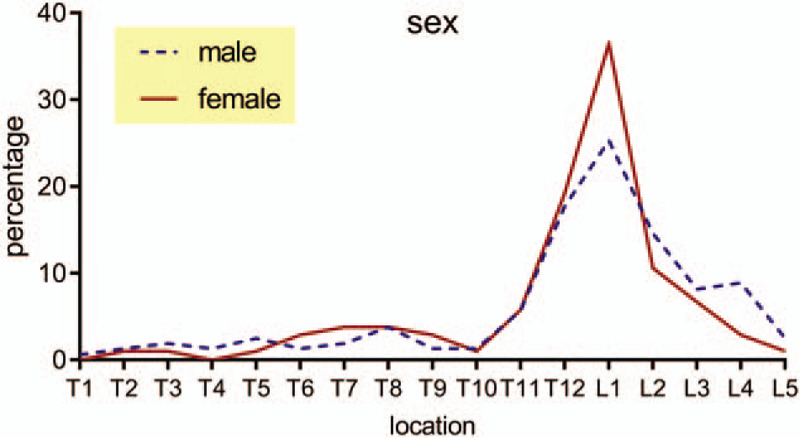
The anatomical distribution of vertebral fracture.
Regardless of gender, age, and the percentage of vertebral height compression, the involved vertebra was mostly L1 (29.7%), followed by T12 (18.3%), and then by L2 (12.9%). The anatomical distribution of the injuries is listed in Figure 2 (χ2 = 13.898, P = .606).
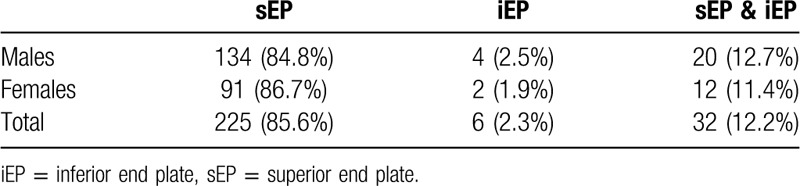
3.2. The distribution of traumatic EPFs in superior and inferior end plate (iEP)
Superior vertebral EP injury (85.6%) was more common than iEP injury (2.3%), while the combination of both was observed in 12.2% of the levels.
Except for those had both superior end plate (sEP) and iEP fractures, for males: sEP/iEP=134/4=33.5; for females: sEP/iEP=91/2=45.5. The distribution of EPFs is consistent in male and female (Table 1). (Chi-squared test, χ2 = 0.200, P = .899).
Table 1.
The distribution of traumatic end plate fractures in superior and inferior end plate.
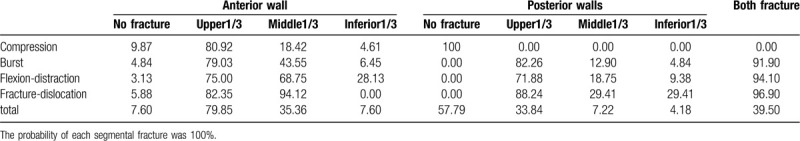
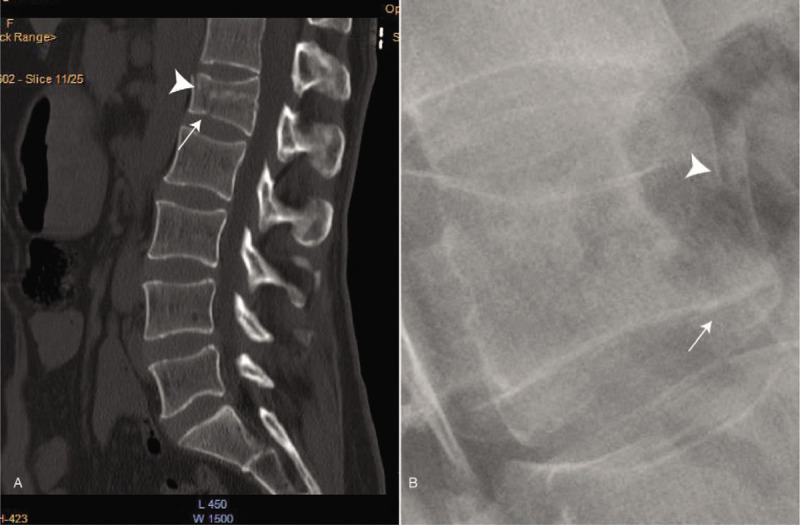
3.3. The distribution of superior and iEP fracture in different fracture types (Fig. 3) (all the segments involved summed were shown in Table 2)
Figure 3.
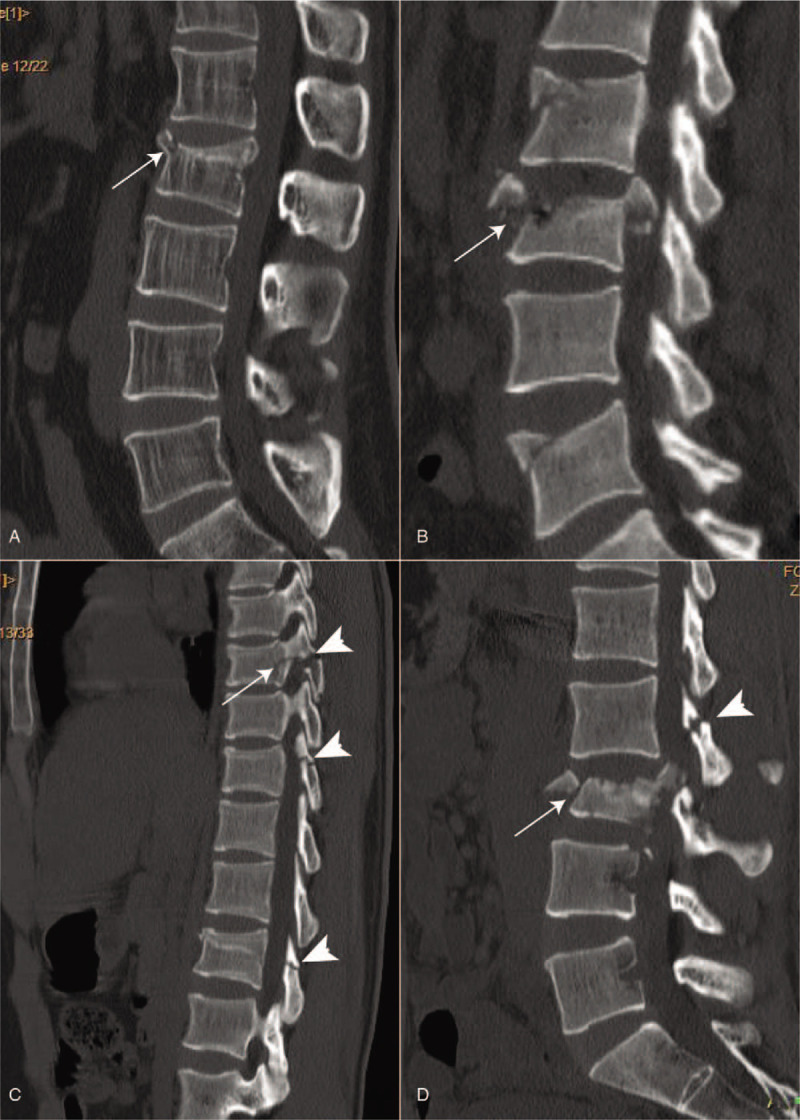
The distribution of end plate fracture in different fracture types (a) Compression fracture of L2. The thin arrow showed the fracture of the a1 segment of the superior end plate (sEP). In figure (b), L3 was a burst fracture, and bone fragments protruding from the anterior and posterior edges (thin arrows) were visible. The curvature of the anterior and posterior edges of the vertebral body was normal without obvious displacement. The sEP fracture involved the a2 and m and p2 segments, and the L2 and L5 were compression fractures. Figure (c) showed the fracture of Flexion-distraction type. Transverse fractures of the posterior vertebral body, posterior wall, and posterior vertebral arch can be seen (thin arrow). Separation of posterior spinous process fracture (thick arrow) can be seen. Figure (d) showed the fracture-dislocation type. The superior and inferior end plates of the L3 vertebral, and the anterior and posterior walls were fractured, and the vertebral bodies were shifted backward and upward, the distance between the posterior spinous process was widened, the posterior spinous process of the L2 fractured (thick arrow), and the p1 segment of L4 sEP were separated.
Table 2.
The distribution of superior and inferior end plate fracture in different fracture types (%).
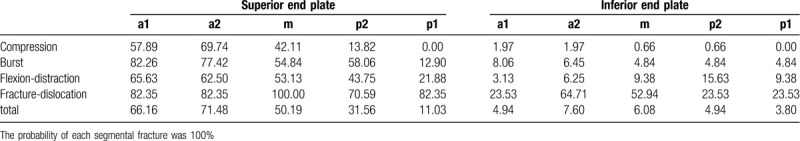
Of the 263 fractured vertebrae, 152 showed compression fracture, 62 showed burst fracture, 32 showed flexion-distraction fracture, and 17 showed fracture-dislocation. Compression fractures were given priority to involvement of the anterior part, involved mostly at a1 (57.89%) and a2 (69.74%) segments. The EPFs of burst and flexion fractures were involved in a wide range, mainly involving 3 or more segments, and the distribution trend was same in this 2 types, occurred often at segment-a1, followed by segment-a2 and then by segment-m. Fracture-dislocation type was characterized by all segments and simultaneous involvement of the superior and iEPs. All 5 segments of the sEP involved in 9 (52.94%) patients, and both the upper and lower EPs involved in 14 (83.33%) patients. It involved mostly at segment-m. When all the fracture types summed together, we can see traumatic EPFs occurred mostly at segment-a2, followed by segment-a1 and then by segment-m in sEPs. (Chi-squared test, χ2 = 448.466, P = .000). The anterior EPF more than the posterior EP in both sEP and iEP.
3.4. The anterior wall fracture appeared in 92.4% patients, with the protruded (198/263, 75.3%) type being most common.
Both anterior and posterior walls had upper 1/3 fractured mostly, followed by middle 1/3, with the lower 1/3 being least affected (Table 3).
Table 3.
The distribution of anterior wall and posterior wall fracture in different fracture types (%).
For the posterior wall fracture, 68.5% involved areas close to the vertebral basal foramen (Fig. 4).
Figure 4.
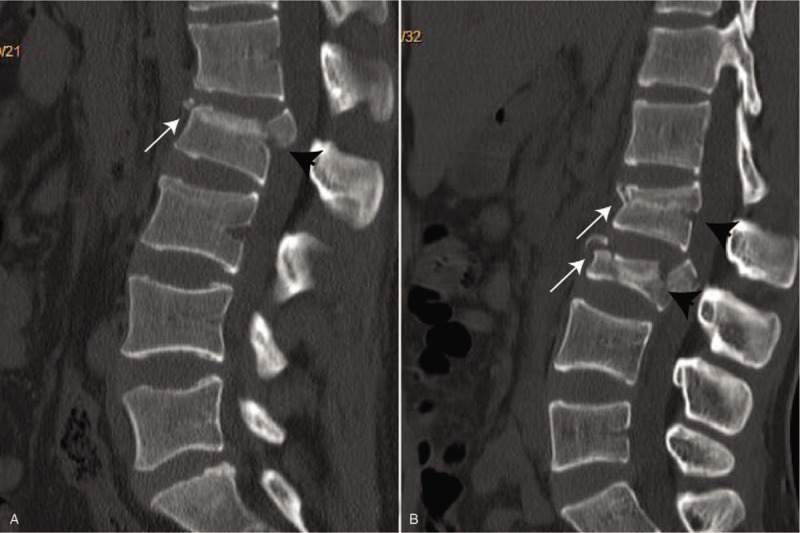
In figure (a), upper 1/3 of the anterior wall was fractured (thin arrow), and middle 1/3 of the posterior wall was fractured. The fracture line was close to the vertebral basal foramen (black thick arrow). In figure (b), the middle segment of the anterior wall of the L2 vertebra concave (thin arrow), the fracture line of the posterior wall near the vertebral basal foramen (thick arrow), and both the upper and middle 1/3 segments of the anterior and posterior walls of the L3 vertebra were fractured.
3.5. Examination technique
In this study, a total of 75 patients received radiographs examination either as a separately method or in combination with other methods. It can be seen from Table 4 that it appeared mainly in the compression fractures. Among them, in 13 patients EPF could not be accurately diagnosed (Figs. 5 and 6), with a misdiagnosis rate of 25.49%. From the 20 cases of Burst fracture examined by radiographs, 2 cases could not be diagnosed, the misdiagnosis rate was 10%.
Table 4.
Radiographs examination in different fracture types.
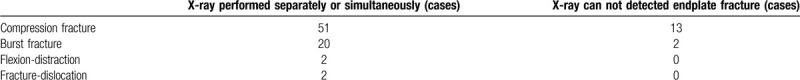
Figure 5.
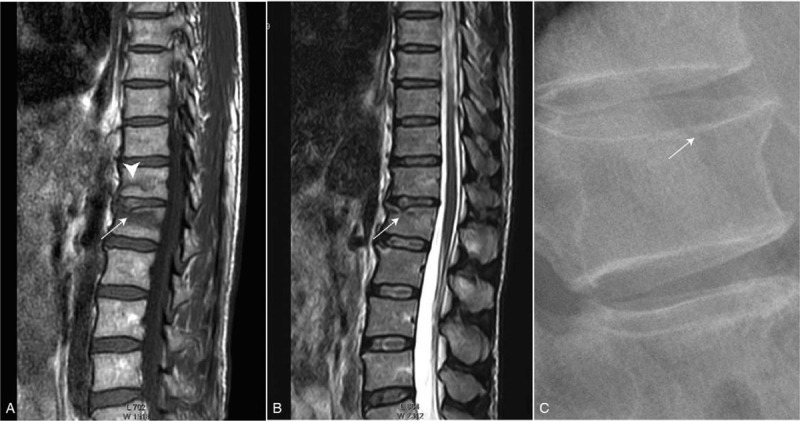
Figure (a) and (b) showed the fracture of a2 segment of the superior end plate in L2 vertebra, and (c) showed that radiograph cannot displayed clearly (thin arrow). Low-signal fracture line of L1 vertebra can see on T1WI (thick arrow), without involving the end plate.
Figure 6.
On CT sagittal reconstruction, fracture of a2 segment of inferior end plate of L1 vertebra can be seen in figure (a) (thin arrow), and bone discontinuity of upper 1/3 of the anterior cortex (thick arrow) can be seen, too. In figure (b), fracture line of inferior end plate of L1 was not shown clearly (thin arrow), and anterior cortical discontinuity can be seen clearly (thick arrow).
4. Discussion
4.1. The significance of studying the EP
EPs serve as the interface between pliant intervertebral disk and rigid vertebral body. The thickness of the vertebral EP is about 0.44 to 0.89 mm in the cervical vertebra, as thin as 0.12 mm in the thoracic vertebra, and 0.64 ± 0.41 mm in the thoracolumbar segment.[10] The structure of the EP has important biomechanical and nutritional function. Because the lumbar spine suffers significant forces and disks do not have blood supply, EPs must balance conflicting of being strong to prevent vertebral collapse and porous to facilitate the transport of vertebral capillaries to intervertebral disc cells.[11]
4.2. Changes in an ageing EP
In the young disk, the proteoglycan content in EP cartilage is 300 μg/mg, with water being 78% and type I collagen contents 0.9 ng/mg, respectively.[12] During aging, changes occurred in the proteoglycan and collagen of cartilage EP, resulting in thinning, and calcification gradually.[12] Proteoglycan decreases to 150 μm/mg by age 80 years. Simultaneously, water decrease to 67% and type I collagen to 0.25 ng/mg, respectively.[12] Hence, EP becomes stiff and weaker as the adjacent disks degenerate.[13–14] In order to compare between osteoporotic EPFs, we chose male patients aged less than or equal to 55 years old and female patients aged less than or equal to 50 years old, in order to make sure the EP was in a healthier state.
4.3. Comparision between traumatic and osteoporotic VFs.
As we mentioned above, some traumatic VFs in the elderly may be mistakenly treated as osteoporotic. In order to differentiate between traumatic and osteoporotic VF, we compare radiological features between them.
The common method for diagnosing an osteoporotic VF relies on the manifestation of a vertebral deformity on radiographs, it includes wedge, biconcave, and crush deformity.[15] While in the traumatic, types are based on the Denis[9] 3 columns model that include compression, burst, flexion-distraction, and fracture-dislocation types.
This study shows, for both males and females, the fracture involved vertebra was mostly at L1 (29.7%), followed by T12 (18.3%), and then by L2 (12.9%). The prevalence found in this study closely resembled reported by Nazimi et al,[1] which showed thoracolumbar junction had the highest prevalence of osteoporotic EPFs, mostly at L1 vertebra (26.4%), followed by T12 (20.7%). Min Deng et al[16] also showed in Asian elderly women from Hong Kong, Indonesia, Thailand, and Japan that VFs are found particularly common at the thoracolumbar junction (T12 and L1 levels). This result are consistent with the earlier finding of Copper et al[17] that T12 and L1 are biomechanically most vulnerable to impact in thoracolumbar spine.
SEPs is known to be more vulnerable injured than iEPs, because iEPs are thicker and supported by more below trabecular bone.[18,19] The underlying cancellous bone of iEP is more dense than that of the sEP. Zhao et al[18] reported that thickness was greater for caudal than craninal EP (P = .001) and in pedicle compare to mid-saggital slice (P = .003). And what is more, pal et al[20] concluded that the caudal EP being thickened and strengthened by the trabecular arch at the pedicles. These changes in EP structure may be related to inherent characteristic of the spine rather than aging.[18,19] Wang et al[19] also reported the asymmetric structure of vertebral trabeculae was not associated with age and disc degeneration. Our research showed except for those had both sEP and iEP fractures, for males: sEP/iEP=134/4=33.5; for females: sEP/ iEP=91/2=45.5. Zhao et al[18] reported sEP/iEP=57/2 in an ex vivo biomechanial testing. And Nazimi et al[1] reported that prevalence of VFs in osteoporotic people occur more likely at sEP, with sEPF/iEPF ratio (5.1 for combined males and females results). Interestingly, we can find sEP is distinctly more likely to fracture in traumatic compared with osteoporotic, whether it make sense need further research.
It is known that the thickness of EP varied in different regional, being reported to be thinner centrally.[21] Because the central of EP has more contact channels which is known to be most porous,[22] as the intervertebral disc nucleus has the greatest nutritional needs. This potential increases with age, where the EPs become more porous (60%) and their hardness and strength decrease with the adjacent plates degenerate.[13–14] Some scholars have concluded[18] that the density of bone trabeculae was higher in posterior region than in anterior (P < .001) and middle (P < .001) regions. Melton III & Kallmes et al[23] showed that the weakest part of a vertebral body is the anterior and inferior part, because they are thinner and supported by less dense trabecular bone. The thickening of the iEPs is most obvious, with iEP being thickened and strengthened by trabecular arcades from the pedicles.[20] Nazimi[1] research, in osteoporotic fracture, the most fractured point occur in segment-m-of the EP, followed by segment-a2 and p2. Their study did not show segment-a1 and p1 have EPF in osteoporotic population.
However, this is not entirely consistent with our results, in our study, we discovered that a statistically significant correlation existed between the position of EPFs and fracture type. Compression fractures is given priority to involvement of the anterior part of EP, mainly at a1 and a2 segment. While in burst and flexion fractures, the EPs fracture involved in a wide range, mainly involving 3 or more segments, and the distribution trend was mostly occur in the a1 and a2 segment of the EP, and then followed by segment-m and p2. In fracture-dislocation type, segment-m is the most occurred place. When we summed all involved segments together, the a2 segment occur most, followed by a1 and m, that means the anterior part of EPF more than posterior par in both superior and iEPs.
There are many factors affecting the sensitivity of EP damage, including the nature of mechanical loads, the local shape of EP structures, properties of tissue materials, and conditions of intervertebral discs.[11] I think the difference between traumatic and osteoporotic EPF may be caused by the following reasons. First, the nature of the mechanical loading, traumatic EPFs suffer a high and rapid energy, or acute low energy, leading the bone marrow and other liquid flow out from the compressed vertebral body. At the same time, the pressure in the intervertebral disc increases, and the EP bulges out to both sides, sometimes isolated.[24] While osteoporotic EPFs often caused by chronic and low energy. Second, it is the condition of the intervertebral disk. For the discs, lower BMD in ageing was associated with a decrease of anterior height and posterior height, and an increase in middle height in both men and women. The disc biconvex index was increased.[25] Because of biconvex, the pressure focus on the middle of EP. What is more, the central area of the bony EP becomes more porous and less stiff and weaker as the adjacent intervertebral disks degenerate.[13–14] Pollitine et al[26] also found that disc degeneration alter the loading pattern of the vertebral body. A healthy intervertebral disc transmits compressive force evenly from 1 vertebral body to another. While Upon ageing, the disc becomes fibrous and shortens in height, which resulting in uneven load distribution.
In traumatic VFs, both anterior and posterior walls had upper 1/3 fractured mostly, followed by middle 1/3, with the lower 1/3 being least affected. Both wall fractured in 39.5% cases. For the posterior wall fracture, most involved areas close to the basivertebral foramen, which is a path for vertebral capillaries and nerves enter the vertebral body, and form an “artery grid” in the center of the vertebral body, branching, and terminating near the cartilage EP.[27]
While in osteoporotic VFs, mostly fractures were concave and wedge type, without involvement of both wall.
4.4. Examination method
Radiographic diagnosis is an adequate starting method for patients who have sustained a low energy trauma. Both anteroposterior and lateral films are usually performed, which are helpful to asses vertebral height loss and the presence of fracture lines. However, sometimes it is difficult to identify the fracture lines involved by radiographs alone, especially in patients with low grade deformity and concomitant with old fractures. In most hospital, spine multidetector computerized tomography (MDCT) is nowadays chose as the first method in the imaging protocol of high energy trauma, and as a method of ruling out thoracic and abdominal injuries in all cases. MDCT is also needed in cases of low energy trauma with normal radiographs, if clinical doubt persists. When fracture is demonstrated on radiograph of a patient with low energy trauma, we also advocate CT scans that include at least 2 vertebrae up and below the fracture, because radiographs are known to underestimate the severity of fractures, including instability, or misdiagnose of burst fractures as compression fractures.[33,34] Therefore, for surgical planning, radiographs alone is not enough, and additional CT scans are required for fracture classification and treatment decisions.[28] MRI, compared with radiography and CT, is superior in providing information on soft tissue and allows better inspection of bone marrow and oedema, indicating whether a fresh fracture, due to better contrast differentiation.[29] In our study, a total of 75 patients received radiographs examination either as an isolated method or in combination with other methods, radiographs examination used mostly in compression fracture, in which the misdiagnosis rate is highest (25.49%.). While in burst and other fracture type, CT and MRI used more.
4.5. Limitations of this study
First, 20 cases EPFs evaluation was based on only radiograph, while due to its underestimate the severity of fracture, some EPFs may be missed. In order to minimally mistake, all EPFs in this study have been triple-checked. Second, another possibility is that not all patients did BMD examination, a few traumatic EPFs may be osteoporotic in which the EP in a osteoporotic statement, so we asked the history of patient carefully, to excluded the underlying causes of osteoporosis. Third, because of collecting patients from different hospital, scanning parameters may be different, so all films were double checked by the same radiologist, and then 1 more time checked by another radiologist experienced in VF. However, we expect these limitations would not affect the overall conclusion of this study.
5. Conclusion
In conclusion, this study demonstrates traumatic EPFs more likely involve the anterior part than the posterior part in both superior and iEPs, and location of EPFs is correlation with the fracture type. The fracture rate of sEP is much higher than that of iEP. What is more, the upper third of the anterior and posterior walls are most prone to fractures in traumatic VF. Additionally, we expect the characteristic of EPFs described in this study may help orthopedic surgeons. Orthopedic surgeons should try to place the support in a place where the EP is relatively rigid during surgery, and try to repair the integrity of the EP. Secondly, the position of traumatic EPF is not completely consistent with the reported osteoporosis EPF, which is beneficial for doctors to judge the fracture cause and decide whether osteoporosis treatment is needed.
Currently, plain radiograph is an adequate starting method for patients who have sustained a low energy trauma, but because of underestimating the severity of fractures, MDCT scanning is suitable for accurate fracture classification and treatment decision making.
Acknowledgments
We thank Professor Yi Xiang Wang of the Chinese University of Hong Kong, Prince of Wales Hospital very much for providing guidance and clarification on the topics discussed in this article.
Author contributions
Data curation: Feirong Xu, Yuan Fu, Huanhuan Chen.
Formal analysis: Xiaorong Wang, Feirong Xu.
Funding acquisition: Xiang Gao, Qiuli Huang.
Methodology: Xiaorong Wang, Xiang Gao.
Software: Xiaorong Wang, Qiuli Huang.
Writing – original draft: Xiaorong Wang.
Writing – review & editing: Qiuli Huang.
Footnotes
Abbreviations: EP = end plate, EPF = end plate fracture, iEP = inferior end plate, MDCT = multidetector computerized tomography, MRI = magnetic resonance imaging, sEP = superior end plate, VF = vertebral fracture.
How to cite this article: Wang X, Xu F, Fu Y, Chen H, Gao X, Huang Q. Traumatic vertebral fractures involve the anterior end plate more than the posterior end plate: a retrospective study. Medicine. 2020;99:34(e21572).
The authors have no conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Nazmi CN, Min D, James FG, et al. Prevalent osteoporotic vertebral fractures more likely involve the upper endplate than the lower endplate and even more so in males. Ann Transl Med 2018;6:442–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Lentle BC, Oei E, Goltzman D, et al. Vertebral fractures and morphometric deformities. J Bone Miner Res 2018;33:1544–5. [DOI] [PubMed] [Google Scholar]
- [3].Genant HK, Wu CY, van Kuijk C, et al. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993;8:1137–48. [DOI] [PubMed] [Google Scholar]
- [4].Schwartz EN, Steinberg D. Detection of vertebral fractures. Curr Osteoporos Rep 2005;3:126–35. [DOI] [PubMed] [Google Scholar]
- [5].Jiang G, Eastell R, Barrington NA, et al. Comparison of methods for the visual identification of prevalent vertebral fracture in osteoporosis. Osteoporos Int 2004;15:887–96. [DOI] [PubMed] [Google Scholar]
- [6].Ferrar L, Jiang G, Clowes JA, et al. Comparison of densitometric and radiographic vertebral fracture assessment using the algorithm-based qualitative (ABQ) method in postmenopausal women at low and high risk of fracture. J Bone Miner Res 2008;23:103–11. [DOI] [PubMed] [Google Scholar]
- [7].Wáng YX. A modified semi-quantitative (mSQ) grading scheme for osteoporotic vertebral fracture in elderly women. Quant Imaging Med Surg 2019;9:146–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Jiang G, Luo J, Pollintine P, et al. Vertebral fractures in the elderly may not always be “osteoporotic”. Bone 2010;47:111–6. [DOI] [PubMed] [Google Scholar]
- [9].Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983;8:817–31. [DOI] [PubMed] [Google Scholar]
- [10].Kumar A. Biomechanical testing of vertebral endplate strength: a cadaver study. Presented at 8th annual meeting of the North American Spine Society 1993. [Google Scholar]
- [11].Lotz JC, Fields AJ, Liebenberg EC. The role of the vertebral end plate in low back pain. Global Spine J 2013;3:153–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Antoniou J, Goudsouzian NM, Heathfield TF, et al. The human lumbar endplate. Evidence of changes in biosynthesis and dena turation of the extracellular matrix with growth, maturation, aging, and degeneration. Spine 1996;21:1153–61. [DOI] [PubMed] [Google Scholar]
- [13].Rodriguez AG, Slichter CK, Acosta FL, et al. Human disc nucleus properties and vertebral endplate permeability. Spine 2011;36:512–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Rodriguez AG, Rodriguez-Soto AE, Burghardt AJ, et al. Morphology of the human vertebral endplate. J Orthop Res 2012;30:280–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Pham T, Azulay-Parrado J, Champsaur P, et al. “Occult” osteoporotic vertebral fractures: vertebral body fractures without radiologic collapse. Spine (Phila Pa 1976) 2005;30:2430–5. [DOI] [PubMed] [Google Scholar]
- [16].Deng M, Zeng XJ, He LC, et al. Osteoporotic vertebral fracture prevalence in elderly Chinese men and women: a comparison of endplate/cortex fracture-based and morphometrical deformity-based methods. J Clin Densitom 2019;22:409–19. [DOI] [PubMed] [Google Scholar]
- [17].Cooper C, Atkinson EJ, O’Fallon WM, et al. Incidence of clinically diagnosed vertebral fractures: a population-based study in rochester, minnesota, 1985-1989. J Bone Miner Res 1992;7:221–7. [DOI] [PubMed] [Google Scholar]
- [18].Zhao FD, Pollintine P, Hole BD, et al. Vertebral fractures usually affect the cranial endplate because it is thinner and supported by less-dense trabecular bone. Bone 2009;44:372–9. [DOI] [PubMed] [Google Scholar]
- [19].Wang Y, Battie MC, Boyd SK, et al. The osseous endplates in lumbar vertebrae: thickness, bone mineral density and their associations with age and disk degeneration. Bone 2011;48:804–9. [DOI] [PubMed] [Google Scholar]
- [20].Pal GP, Cosio L, Routal RV. Trajectory architecture of the trabecular bone between the body and the neural arch in human vertebrae. Anat Rec 1988;222:418–25. [DOI] [PubMed] [Google Scholar]
- [21].Roberts S, McCall IW, Menage J, et al. Does the thickness of the vertebral subchondral bone reflect the composition of the intervertebral disc? Eur Spine J 1997;6:385–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Edwards WT, Zheng Y, Ferrara LA, et al. Structural features and thickness of the vertebral cortex in the thoracolumbar spine. Spine 2001;26:218–25. [DOI] [PubMed] [Google Scholar]
- [23].Melton LJ, III, Kallmes DF. Epidemiology of vertebral fracture: implicaiton for vertebral augmentation. Acad Radiol 2006;13:538–45. [DOI] [PubMed] [Google Scholar]
- [24].Yang XJ, Wang ZG, Zhu PF, et al. Study on dynamic mechanism of thoracolumbar burst fracture and its stability. Chin J Traumatol 1999;15:103–6. [Google Scholar]
- [25].Kwok AW, Wang YX, Griffith JF, et al. Morphological changes of lumbar vertebral bodies and intervertebral discs associated with decrease in bone mineral density of the spine: a cross-sectional study in elderly subjects. Spine (Phila Pa 1976) 2012;37:1415–21. [DOI] [PubMed] [Google Scholar]
- [26].Pollintine P, Dolan P, Jon HT, et al. Intervertebral disc degeneration can lead to “stress—shielding” of the anterior vertebral body, a cause of osteoporotic vertebral fracture? Spine 2004;29:774–82. [DOI] [PubMed] [Google Scholar]
- [27].Bailey JF, Liebenberg E, Degmetich S, et al. Innervation patterns of PGP 9. 5-positive nerve fibers within the human lumbar vertebra. J Anat 2011;218:263–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Dai LY, Wang XY, Jiang LS, et al. Plain radiography versus computed tomography scans in the diagnosis and management of thoracolumbar burst fractures. Spine (Phila Pa 1976) 2008;33:548–52. [DOI] [PubMed] [Google Scholar]
- [29].Marongiu G, Congia S, Verona M, et al. The impact of magnetic resonance imaging in the diagnostic and classification process of osteoporotic vertebral fractures. Injury 2018;49:26–31. [DOI] [PubMed] [Google Scholar]


