Abstract
Obturator hernia is a relatively rare type of abdominal hernia, in which abdominal contents protrude through the obturator canal, a condition that can lead to small bowel obstruction. Its rarity and nonspecific signs and symptoms make a preoperative diagnosis difficult. The present study analyzed the clinical manifestations, diagnostic methods and operative treatment outcomes in patients with obturator hernia.
Between January 2012 and October 2019, 1028 adults underwent surgical repair of abdominal wall hernia at the Department of Surgery, Kyungpook National University Hospital. The medical records of eleven patients who were treated for small bowel obstruction due to obturator hernia were retrospectively evaluated. Patient characteristics, clinical presentation, preoperative radiological diagnosis, operative findings, treatment, complications, and outcomes were recorded.
All 11 patients were elderly women, with a mean age of 80.2 years (range, 71–87 years). Their mean body mass index was 17.9 kg/m2 (range, 11.9–22.2 kg/m2). Symptoms at presentation were abdominal pain and vomiting, with a mean duration of symptoms prior to admission of 5.6 days (range, 1–15 days). Based on abdominopelvic computed tomography (CT) scans, all 11 patients were preoperatively diagnosed with obturator hernia, followed by laparoscopic exploration or laparotomy as soon as possible. Of the 11 patients, 6 (54.5%) had left-sided, four (36.4%) had right-sided, and one (9.1%) had bilateral obturator hernias. Three patients (27.3%) required resection of the ileum due to perforation or strangulation. All underwent simple closure of the hernia defect with interrupted or purse-string sutures. Ten patients recovered uneventfully, whereas one had wound seroma and ileus. Recurrence has not been observed in the 8 surviving patients.
Obturator hernia should be included in the differential diagnosis of intestinal obstruction of unknown origin, especially in emaciated elderly women with chronic disease. Early surgical intervention without delay is imperative to avoid postoperative morbidity and mortality associated with intestinal strangulation due to obturator hernia. Obturator hernia can be sufficiently repaired with simple suture closure without mesh.
Keywords: computed tomography, intestinal obstruction, obturator hernia
1. Introduction
Obturator hernia is a relatively rare type of abdominal hernia, in which abdominal contents protrude through the obturator canal, a condition that can lead to small bowel obstruction.[1–5] Obturator hernia, which accounts for less than 1% of all abdominal wall hernias, usually occurs in elderly, thin, multiparous women.[6–10] Obturator hernia accounts for 0.2% to 1.6% of patients with mechanical obstruction of the small bowel.[1,5,6] More than 90% of patients with obturator hernia present with intestinal obstruction.[3] Despite advances in diagnostic imaging modalities, a correct preoperative diagnosis is often delayed because the signs and symptoms of obturator hernia are nonspecific and physical examination is indeterminate. The high postoperative mortality rate in patients with this condition is often attributed to delays in presentation and diagnosis, the advanced age of the patients, and the co-occurrence of concurrent medical illnesses and debilitating conditions.[10,11] The aim of this study is to analyze the clinical characteristics and postoperative outcomes of 11 patients with obturator hernia who were treated in our hospital over a period of 7 years. We also reviewed previously published data to compare with our experience and to establish a guideline for the accurate diagnosis and treatment of this rare type of hernia.
2. Materials and methods
Between January 2012 and October 2019, 1028 adults underwent surgical repair of abdominal wall hernia at the Department of Surgery, Kyungpook National University Hospital. There were 845 inguinal hernia (82.2%), 88 incisional hernia (8.56%), 46 femoral hernia (4.47%), 24 umbilical hernia (2.33%), 13 obturator hernia (1.26%), 7 epigastric hernia (0.68%), 4 Spigelian hernia (0.39%), and 1 lumbar hernia (0.1%). Thirteen (1.26%) of these patients were treated for small bowel obstruction due to obturator hernia. After excluding two patients with insufficient clinical information, the medical records of the remaining 11 patients were retrospectively evaluated. Patient characteristics, clinical presentation, comorbidities, preoperative radiological diagnosis, operative findings, treatment, complications, and outcome were recorded. The literature review was conducted by searching in PubMed using the keywords “obturator hernia”. We found 11 articles describing more than 10 surgical cases of obturator hernias, published in the last 25 years. The study protocol was approved by the Institutional Review Board of Kyungpook National University Hospital (IRB No. 2019-11-036).
3. Results
3.1. Patient characteristics and clinical presentation
All 11 patients were elderly women, with a mean age of 80.2 years (range, 71–87 years). Their mean body weight and height upon admission were 38.8 kg (range, 28–50 kg) and 150.8 cm (range, 145–157 cm), respectively, and their mean body mass index was 17.9 kg/m2 (range, 11.9–22.2 kg/m2). All 11 patients presented with intestinal obstruction. Symptoms at presentation were abdominal pain and vomiting, with a mean duration of symptoms of 5.6 days before admission (range, 1–15 days). One patient (Patient No. 1) had a prior history of symptoms and signs of self-limited partial intestinal obstruction. Concomitant comorbid conditions included hypertension, chronic obstructive pulmonary disease, asthma, cerebrovascular accident, congestive heart failure, dementia, atrial fibrillation, and Alzheimer's disease. One patient had undergone a subtotal gastrectomy with Billroth I anastomosis due to gastric cancer, one had undergone total knee replacement arthroplasty for an osteoarthritic knee and another had undergone closed reduction with internal fixation for bilateral femur fractures. The detailed demographic characteristics of these 11 patients are summarized in Table 1.
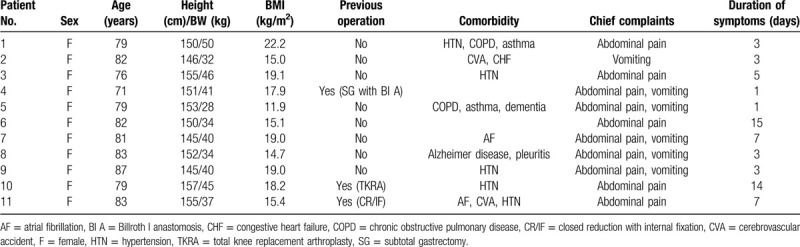
Table 1.
Demographic characteristics of the 11 patients with obturator hernia.
3.2. Preoperative radiologic diagnosis
Five of 11 patients were transferred after performing abdominopelvic computed tomography (CT) scan in other hospitals, and remaining 6 patients underwent abdominopelvic CT scan at our hospital. The average time taken for abdominopelvic CT scan after arrival at our hospital was 135.5 minutes (range; 85–282 minutes). Obturator hernia was diagnosed in all 11 patients preoperatively, based on abdominopelvic CT scans that showed a low-density mass between the pectineus and the external obturator muscles (Fig. 1). Unfortunately, patient No. 1, 10, and 11 had obturator hernia on the initial abdominopelvic CT scan, but we failed to recognize the presence of the disease initially. Later, we found and diagnosed the disease while reviewing the abdominopelvic CT scan again. Therefore, surgery was delayed in three patients.
Figure 1.
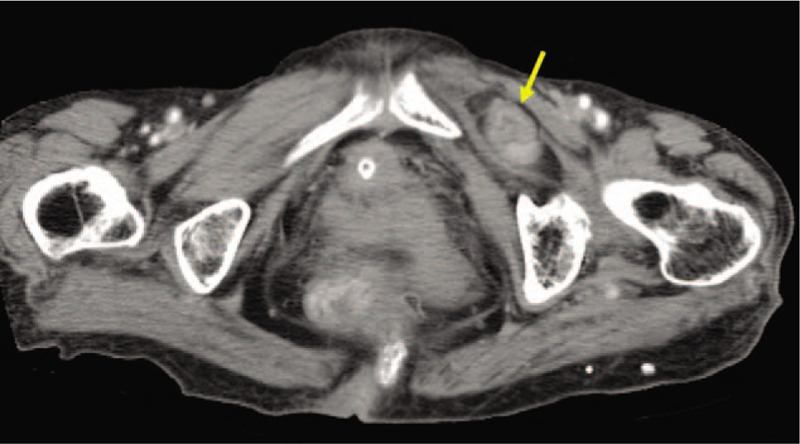
Axial view on an abdominal computed tomography scan showing an incarcerated small bowel between the external obturator and pectineal muscles (arrow).
3.3. Operative findings and treatment
All 11 patients underwent laparoscopic exploration or laparotomy as soon as their diagnosis of obturator hernia was confirmed on the abdominopelvic CT scans. Initial surgery included laparotomy with lower midline incisions in 4 patients and laparoscopic exploration in seven. However, 3 of the latter patients were converted to open surgery (mini-laparotomy) due to bowel resection or technical problems resulting from severe bowel distention or adhesion. Of these 11 patients, 6 (54.5%) had left-sided, 4 (36.4%) had right-sided, and 1 (9.1%) had bilateral obturator hernias. The patient with bilateral obturator hernia (Patient No. 5) was diagnosed with right obturator hernia on preoperative abdominopelvic CT scan, but left obturator hernia was found incidentally during the surgery. Incarcerated ileum was found in the obturator canals of 8 patients (Fig. 2). At the time of surgery, however, incarcerated ileum was already reduced in 3 patients (Patient No. 4, 5, and 7). Three patients required resection of the ileum due to perforation or strangulation. All 11 patients underwent simple closure of the hernia defect with non-absorbable black silk, interrupted or purse-string sutures, with none requiring mesh. The clinical and surgical details of the 11 patients are summarized in Table 2.
Figure 2.
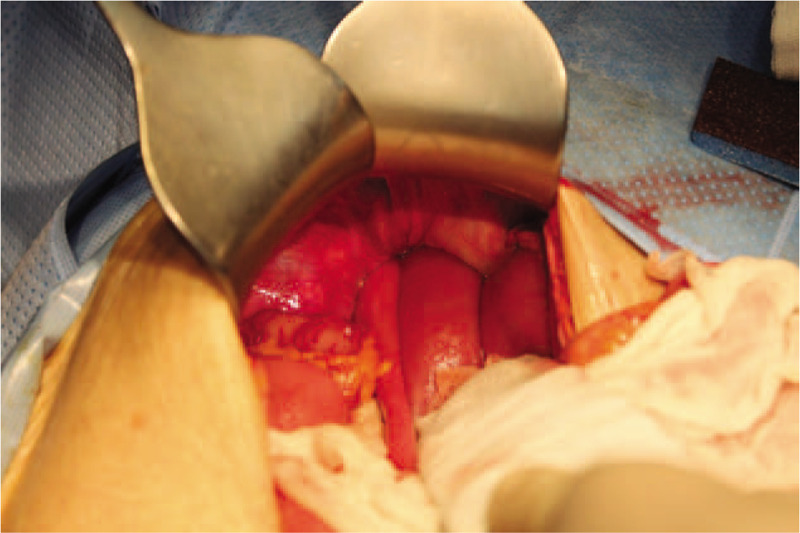
Photograph taken during exploratory laparotomy, showing an incarcerated ileum through the left obturator foramen.
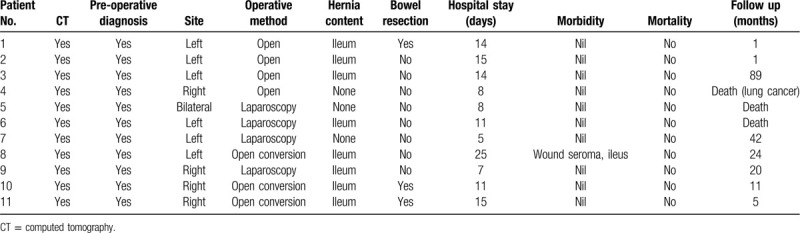
Table 2.
Clinical and surgical details of the 11 patients with obturator hernia.
3.4. Outcome
Postoperative hospital stay ranged from 5 to 25 days, with a mean of 12 days. Following surgery, 10 of the 11 patients recovered uneventfully. One patient had wound seroma and ileus, which were treated conservatively. During follow-up, 3 patients died of unrelated causes, 2 died of old age, each at 5 months and 2 years after surgery, and the third died of lung cancer 4 years after surgery. The 8 surviving patients have been followed-up for a mean 24 months (range, 1–89 months), with none experiencing a recurrence of obturator hernia.
4. Discussion
Obturator hernia is a relatively rare type of abdominal hernia in which abdominal contents protrude through the obturator canal, a condition that can lead to small bowel obstruction.[1–5] This condition usually occurs in elderly, thin, emaciated patients aged 70 to 90 years.[6–15] Obturator hernias are nine times more common in women than in men due to factors that may increase the risk of obturator hernia development such as, having a wider pelvis and more triangular obturator canal opening with a greater transverse diameter.[1,6] Obturator hernias have been reported to account for 0.05% to 1.4% of all hernias and to be present in 0.2% to 1.6% of patients with mechanical obstruction of the small bowel.[1,5,6,16] Similarly, we found that obturator hernia was present in 13 (1.26%) of the 1028 patients who underwent surgical repair of abdominal wall hernia.
Obturator hernia is thought to result from progressive relaxation of the pelvic floor, which may be associated with advanced age, emaciation, increased intraabdominal pressure, and multiparity. Factors predisposing to obturator hernia include the loss of protective preperitoneal fat and lymphatic tissue over the obturator canal due to aging or malnutrition, resulting in a larger space around the vessels and nerves and facilitating hernia formation.[6] Several concomitant conditions, such as chronic constipation, chronic obstructive pulmonary disease, ascites, kyphoscoliosis and multiparty, can predispose patients to herniation by increasing intraabdominal pressure and relaxing the peritoneum.[17] Obturator hernia occurs more frequently on the right side than on the left side because the sigmoid colon may cover the left obturator foramen, preventing herniation.[12] In our series, however, left-sided obturator hernia was more common than right-sided obturator hernia.
Three anatomic stages in the formation of obturator hernia have been described. The first stage is the entrance of the preperitoneal fat tissue into the pelvic orifice of the obturator canal, forming a pilot fat plug. During the second stage, a peritoneal dimple develops through the canal and progresses to the formation of a peritoneal sac. The third stage consists of the onset of symptoms resulting from the herniation of viscera into this sac.[9,10]
Most patients with obturator hernia present with the symptoms of intestinal obstruction, such as nausea, vomiting, and pain associated with abdominal cramps.[18] One third of patients may experience intermittent symptoms of intestinal obstruction if the herniated content migrates into the peritoneal cavity spontaneously. Transient improvement of intestinal obstruction by spontaneous reduction of the hernia is also an important diagnostic clue.[3,17] One patient in our series (Patient No. 1) had previously experienced an episode of small bowel obstruction of unknown origin; at the time the presence of an obturator hernia was not detected despite an abdominopelvic CT scan.
Obturator hernia itself is not palpable or detectable by physical examination because of its deep location between the pectineus and adductor longus muscles.[2] Palpation of a mass near the rectum or vagina can increase clinical suspicions of obturator hernia. However, physical examination of obturator hernia usually yields nonspecific results. The Howship-Romberg sign, defined as pain along the obturator nerve caused by compression of the nerve by the hernia sac, is pathognomic of an obturator hernia. This pain is frequently exacerbated by extension and abduction or medial rotation of the thigh and has been reported in 15% to 50% of patients with obturator hernia.[5] Because osteoarthritis of the hip is common in elderly patients, the Howship-Romberg sign is often misinterpreted in patients with arthritis; these patients are often referred to orthopedic surgeons or neurologists, delaying the diagnosis and treatment of obturator hernia. In addition, severe abdominal pain due to incarceration or strangulation of the intestine can mask the less severe symptoms of obturator neuropathy.[6,8] Unfortunately, the presence of the Howship-Romberg sign was overlooked in our series due to the early diagnosis using abdominopelvic CT scan. Moreover, it was difficult to evaluate the presence of the Howship-Romberg sign in the patients who had undergone total knee replacement arthroplasty for osteoarthritic knee and closed reduction with internal fixation for bilateral femur fractures. The Hannington-Kiff sign, which indicates the absence of an adductor reflex in the thigh, is more specific than the Howship-Romberg sign but less well known.[9]
Obturator hernia is difficult to diagnose preoperatively, with most patients diagnosed during laparotomy for intestinal obstruction or peritonitis. Previous studies have reported mean times between the onset of symptoms and treatment ranging from 4.4 to 9 days, similar to the mean of 5.6 days observed in our series.[3–5,11,14]
Various imaging modalities have been utilized in the diagnosis of obturator hernia, such as barium enema fluoroscopy, ultrasonography, herniography and CT scanning.[17,19,20] Plain abdominal X-rays can demonstrate dilatation of the small bowel and air-fluid levels. Gas shadow in the area of the obturator foramen is indicative of obturator hernia. Abdominopelvic CT scans are more sensitive and specific, showing a mass-like lesion between the obturator externus and pectineus muscles. Yokoyama et al reported that the introduction of CT scan since 1987 increased the preoperative diagnostic rate of obturator hernia.[1] Kammori et al also reported that 15 of 16 patients with obturator hernia were correctly diagnosed by CT alone since 1987.[5] Haraguchi et al reported that the diagnostic rate of obturator hernia by CT was 87%.[8] Although CT scanning of the abdomen and pelvis has been reported to be useful in the definitive and early diagnosis of obturator hernia,[10,11] utilization of abdominopelvic CT scan did not reduce the rates of bowel strangulation and postoperative morbidity and mortality because most patients do not visit the hospital upon first experiencing the symptoms.[1,6]
Several operative approaches have been suggested for the repair of the defect, including the Cheatle-Henry retropubic, preperitoneal, inguinal, obturator, and intraabdominal approaches.[18,19] The most common is the abdominal approach via a low vertical midline incision; its advantages include avoidance of obturator vessels, better exposure of the obturator ring, and facilitation of bowel resection, if needed.[10,18] Obturator hernia can also be diagnosed and treated by laparoscopic surgery, with both transabdominal and extraperitoneal approach.[15,21–23] This minimally invasive surgical approach enables visualization of the myopectineal orifice and identification of the presence of a synchronous contralateral obturator hernia. Laparoscopic surgery may also provide additional benefits for high-risk patients, such as shorter hospital stay, less postoperative ileus and pain, and fewer pulmonary complications. Because the space in the abdominal cavity is limited due to dilated intestine, the laparoscopic approach is challenging for surgeons and is reserved for selected patients.[16] In our series, 3 of the 7 patients who underwent laparoscopic surgery were converted to open surgery (mini-laparotomy) due to bowel resection or technical problems resulting from severe bowel distention or adhesion.
The management of hernia defects depends on its size.[7] Small defects can be repaired by inversion and simple ligature of the sac, direct herniorrhaphy, or simple interrupted or purse-string suture repair. However, large defects require hernioplasty with adjacent tissue such as aponeurosis, periosteum and muscle, greater omentum, round ligaments, uterine fundus, ovaries, bladder walls, or synthetic mesh.[7,9]
The recurrence rate in the literature was extremely low. Nakayama et al and Rodríguez-Hermosa et al reported that there was no recurrence after surgery.[3,9] Chan et al reported that one out of 21 patients developed recurrent right obturator hernia.[12] Ng et al reported 2 recurrences in the 16 laparoscopic surgery group.[15]
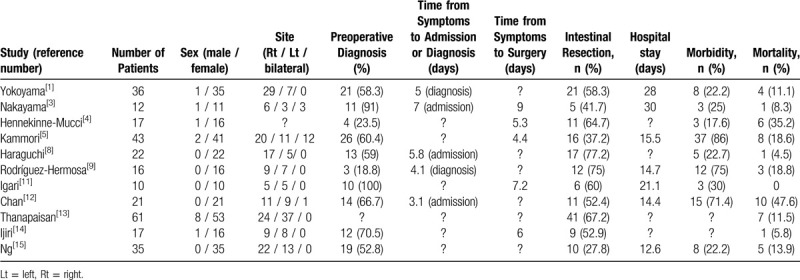
Table 3 summarizes recent studies describing patients treated for obturator hernia, including their demographic and clinical characteristics, times from initial symptoms to diagnosis and to surgery, and rates of intestinal resection, morbidity, and mortality.[1,3–5,8,9,11–15] The postoperative morbidity and mortality rates were high, ranging from 17.6% to 86% and from 0% to 47.6%, respectively. Delays in surgical treatment increased the risks of bowel strangulation, morbidity, and mortality, suggesting that prompt surgical treatment can reduce the morbidity and mortality associated with intestinal strangulation caused by obturator hernia.[7]
Table 3.
Previous studies of patients with obturator hernia.
5. Conclusions
Obturator hernia is a relatively rare type of abdominal hernia that is difficult to diagnose if overlooked. Obturator hernia should be included in the differential diagnosis of intestinal obstruction of unknown origin, especially in emaciated elderly women with chronic diseases. Prompt abdominopelvic CT scan can clarify the cause of intestinal obstruction due to obturator hernia, and early surgical intervention can avoid postoperative morbidity and mortality associated with intestinal strangulation. Obturator hernia can be sufficiently repaired with simple suture closure without mesh.
Author contribution
Jinyoung Park was involved with the operation and general management of the patient and writing of the manuscript for important intellectual content.
Guarantor: Jinyoung Park.
Footnotes
Abbreviation: CT = computed tomography.
How to cite this article: Park J. Obturator hernia: clinical analysis of 11 patients and review of the literature. Medicine. 2020;99:34(e21701).
The study protocol was approved by the Institutional Review Board of Kyungpook National University Hospital (IRB No. 2019-11-036).
This research was supported by Kyungpook National University Research Fund, 2019.
The authors have no conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Yokoyama Y, Yamaguchi A, Isogai M, et al. Thirty-six cases of obturator hernia: does computed tomography contribute to postoperative outcome? World J Surg 1999;23:214–7. [DOI] [PubMed] [Google Scholar]
- [2].Nishina M, Fujii C, Ogino R, et al. Preoperative diagnosis of obturator hernia by computed tomography in six patients. J Emerg Med 2001;20:277–80. [DOI] [PubMed] [Google Scholar]
- [3].Nakayama T, Kobayashi S, Shiraishi K, et al. Diagnosis and treatment of obturator hernia. Keio J Med 2002;51:129–32. [DOI] [PubMed] [Google Scholar]
- [4].Hennekinne-Mucci S, Pessaux P, Du Plessis R, et al. Strangulated obturator hernia: a report of 17 cases. Ann Chir 2003;128:159–62. [DOI] [PubMed] [Google Scholar]
- [5].Kammori M, Mafune K, Hirashima T, et al. Forty-three cases of obturator hernia. Am J Surg 2004;187:549–52. [DOI] [PubMed] [Google Scholar]
- [6].Chang SS, Shan YS, Lin YJ, et al. A review of obturator hernia and a proposed algorithm for its diagnosis and treatment. World J Surg 2005;29:450–4. [DOI] [PubMed] [Google Scholar]
- [7].Munoz-Forner E, Garcia-Botello S, Lopez-Mozos F, et al. Computed tomographic diagnosis of obturator hernia and its surgical management: a case series. Int J Surg 2007;5:139–42. [DOI] [PubMed] [Google Scholar]
- [8].Haraguchi M, Matsuo S, Kanetaka K, et al. Obturator hernia in an ageing society. Ann Acad Med Singapore 2007;36:413–5. [PubMed] [Google Scholar]
- [9].Rodríguez-Hermosa JI, Codina-Cazador A, Maroto-Genover A, et al. Obturator hernia: clinical analysis of 16 cases and algorithm for its diagnosis and treatment. Hernia 2008;12:289–97. [DOI] [PubMed] [Google Scholar]
- [10].Mantoo SK, Mak K, Tan TJ. Obturator hernia: diagnosis and treatment in the modern era. Singapore Med J 2009;50:866–70. [PubMed] [Google Scholar]
- [11].Igari K, Ochiai T, Aihara A, et al. Clinical presentation of obturator hernia and review of the literature. Hernia 2010;14:409–13. [DOI] [PubMed] [Google Scholar]
- [12].Chan KV, Chan CK, Yau KW, et al. Surgical morbidity and mortality in obturator hernia: a 10-year retrospective risk factor evaluation. Hernia 2014;18:387–92. [DOI] [PubMed] [Google Scholar]
- [13].Thanapaisan C, Thanapaisal C. Sixty-one cases of obturator hernia in Chiangrai Regional Hospital: retrospective study. J Med Assoc 2006;89:2081–5. [PubMed] [Google Scholar]
- [14].Ijiri R, Kanamaru H, Yokoyama H, et al. Obturator hernia: the usefulness of computed tomography in diagnosis. Surgery 1996;119:137–40. [DOI] [PubMed] [Google Scholar]
- [15].Ng DC, Tung KL, Tang CN, et al. Fifteen-year experience in managing obturator hernia: from open to laparoscopic approach. Hernia 2014;18:381–6. [DOI] [PubMed] [Google Scholar]
- [16].Chen D, Fei Z, Wang X. Bowel obstruction secondary to incarcerated obturator hernia. Asian J Surg 2017;40:193–6. [DOI] [PubMed] [Google Scholar]
- [17].Cai X, Song X, Cai X. Strangulated intestinal obstruction secondary to a typical obturator hernia: a case report with literature review. Int J Med Sci 2012;9:213–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Hodgins N, Cieplucha K, Conneally P, et al. Obturator hernia: a case report and review of the literature. Int J Surg Case Rep 2013;4:889–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kulkarni SR, Punamiya AR, Naniwadekar RG, et al. Obturator hernia: A diagnostic challenge. Int J Surg Case Rep 2013;4:606–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Mnari W, Hmida B, Maatouk M, et al. Strangulated obturator hernia: a case report with literature review. Pan Afr Med J 2019;32:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Petrushnko W, Isaacs A, Hackland T, et al. Case report: Laparoscopic totally extraperitoneal repair of an obturator hernia with self-gripping mesh under spinal anaesthesia. Int J Surg Case Rep 2019;62:14–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Joe C, Gowda V, Koganti S. Laparoscopic assisted repair of strangulated obturator hernia-Way to go. Int J Surg Case Rep 2019;61:246–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Susmallian S, Ponomarenko O, Barnea R, et al. Obturator hernia as a frequent finding during laparoscopic pelvic exploration: a retrospective observational study. Medicine 2016;95:e4102. [DOI] [PMC free article] [PubMed] [Google Scholar]


