To the Editor:
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in Mexico, in the month of May, has reached an alarming case fatality rate (CFR) of 11%, with a high prevalence of acute respiratory distress syndrome (ARDS) by coronavirus disease 2019 (COVID-19). These patients have shown a high asynchrony index and a correlation with the CFR.
Asynchronies are common in patients with ARDS, and invasive mechanical ventilation (IMV) is common and can occur in all ventilatory modes. Blanch reported that an asynchrony index greater than 10% (number of asynchronies among the total respiratory cycles multiplied by 100) is associated with an increase in mortality and more days of IMV (1). Patients with ARDS due to COVID-19 that needed intubation and IMV present a challenge for the physician and have been associated with a mortality rate of 24.5% (2), despite this, to this date, it has not been described the prevalence of asynchronies in patients with ARDS because of COVID-19 infection and its relationship with the prognosis of their disease.
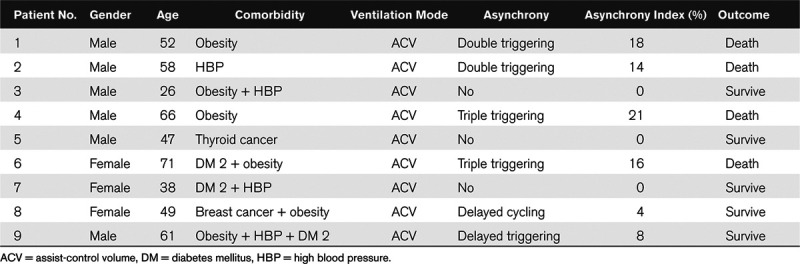
We present a series of nine patients diagnosed with ARDS for COVID-19 and mechanical ventilation. Six patients were men; the average age was 52 years (47–71 yr), in 100% of patients it was ventilated by assisted-volume-controlled mode, with tidal volume (TV) of 6 mL/kg of predicted weight. Four patients died, in whom the asynchronies observed were double and triple triggering. The average 1-minute asynchrony rate was 17% (14–21%) for patients who died versus 2.4% (0–8%) for survivors. The asynchronies observed in survivors were delayed triggering and delayed cycling (Fig. 1). Obesity was present in 75% (3) of the deceased patients (Table 1).
Figure 1.
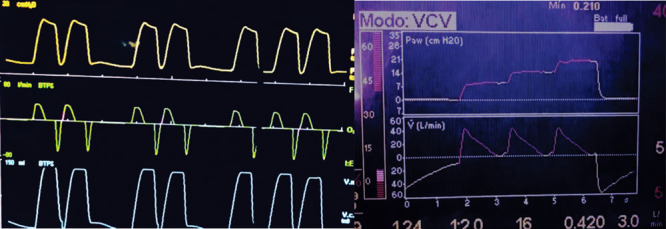
Asynchronies in coronavirus disease 2019. Left: double triggering and right: triple triggering. BTPS = body temperature and pressure, satured, I:E = relation, inspiration:expiration, Paw = pressure airway, V. = flow, V.C. = volume control, VCV = volume cycled ventilation.
Table 1.
Characteristics, Type of Asynchronies, and Outcomes of the Patients
A possible explanation for the multiple, double, and triple triggering could be that, according to the pathology reports of patients with ARDS by COVID-19, diffuse alveolar damage, scaling of pneumocytes, and hyaline membrane formation have been observed, which generates alterations of the gas exchange and subsequent hypoxemia (3); therefore, the patient’s respiratory drive could be increased, as well as their inspiratory effort, same that added to a low TV of 6 mL/kg of predicted weight, could not satisfy their “air hunger,” generating an excessive inspiratory effort that will culminate in multiple triggerings that can cause volutrauma and barotrauma (4). Neuromuscular blockade (NMB) for 24 to 48 hours could be an alternative to avoid triggering asynchronies in this type of patient; NMB has been shown to improve oxygenation, reduce the prevalence of barotrauma and is associated with a reduction in mortality in patients with ARDS (5). A problem raised during the pandemic is fatigue and burnout of physicians, this type of critical care patients with COVID-19 under IMV needs a constant monitoring (6).
The limitation of this study is the small sample size; however, it corresponds to the characteristics of the patients reported worldwide, which reports a predominance of COVID-19 in male patients with cardiovascular comorbidities and obesity, as well as the percentage of mortality associated with patients who required IMV (2).
In summary, close monitoring of patients with COVID-19 and mechanical ventilation is required, staying at the patient’s bedside is necessary to identify life-threatening asynchronies and must be resolved promptly, as well as finding strategies for their prevention of asynchronies. Studies are needed to determine the prevalence of asynchronies in patients with IMV and SARS-CoV-2 infection and its association with poor results.
Footnotes
The authors have disclosed that they do not have any potential conflicts of interest.
Dr. Perez-Nieto was responsible for the conceptualization of the study and the revision and approval of this article. Dr. Guerrero-Gutiérrez was responsible for the accuracy, collect the data, and drafted the article. Dr. Ñamendys-Silva critically reviewed the article. All the authors read and approved the final version of the article.
Collected data and CT images are found in the clinical records of patients at their respective medical centers, data are available on request.
The present study did not require approval by the ethics committee or consent to participate because no intervention was performed and is limited to nine cases. We respect the confidentiality of patients.
REFERENCES
- 1.Blanch L, Villagra A, Sales B, et al. Asynchronies during mechanical ventilation are associated with mortality. Intensive Care Med. 2015; 41:633–641 [DOI] [PubMed] [Google Scholar]
- 2.Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized With COVID-19 in the New York City area. JAMA. 2020; 323:2052–2059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020; 8:420–422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Haro C, Ochagavia A, López-Aguilar J, et al. Patient-ventilator asynchronies during mechanical ventilation: Current knowledge and research priorities. Intensive Care Med Exp. 2019; 7Suppl 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hua Y, Ou X, Li Q, et al. Neuromuscular blockers in the acute respiratory distress syndrome: A meta-analysis. PLoS One. 2020; 15:e0227664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Niederman MS, Richeldi L, Chotirmall SH, et al. Rising to the challenge of COVID-19: Advice for pulmonary and critical care and an agenda for research. Am J Respir Crit Care Med. 2020; 201:1019–1022 [DOI] [PMC free article] [PubMed] [Google Scholar]


