Abstract
The first case of atypical pneumonia caused by coronavirus disease 2019 (COVID-19) was reported in Wuhan, China in December 2019. Since then, cases of novel coronavirus-infected pneumonia (NCIP) have been reported throughout China as well as in 25 other countries. With the rapid growth of this global outbreak, psychological disorders or impact among the healthcare nurses caused by the COVID-19 pandemic is of great importance and worth to be evaluated. Here, we aimed to determine the levels of stress and psychological disorders of nurses who provided nursing care during the COVID-19 outbreak. A total of 159 nurses who provided healthcare work for COVID-19 patients were enrolled in our study. The psychological disorders and stress level were assessed via a questionnaire implemented by the mobile app. The results showed that the nurses who worked in the non-critical care ward (general ward in which the invasive medical procedure such as mechanical ventilation is absent) scored significantly higher on the traumatization condition (P < .05) and stress level (P < .01) as well as the impact of event scale -revised level (P < .01) compared with those worked in the critical care ward. In contrast to the previous report, our findings revealed that the future intervention for preventing the mental crisis among the healthcare nurses needs to be focusing on the individuals in the non-critical care ward instead of those in the critical care ward under the spreading of COVID-19.
Keywords: coronavirus disease 2019, critical care, healthcare nurses, psychological disorders
1. Introduction
In December 2019, the atypical pneumonia cases of unknown etiology were reported in Wuhan, China.[1–3] The pathogen has been later identified as a novel coronavirus (SARS-CoV-2).[4] With rapid increases in international and overseas travel as the result of the globalization, the rapid escalation of cases and deaths has now been reported all over the world.[5] During this outbreak, a large number of patients with the infection have been admitted to the hospitals, leading to the tremendous burden for the healthcare settings in China and other countries.[6]
Many healthcare staff experience serious emotional distress during the pandemic of infectious disease such as severe acute respiratory syndrome (SARS).[7,8] Notably, healthcare workers, especially nurses, are vulnerable to have a plenty of psychological disorders when facing the pandemic situation.[9,10] Thus, to protect the mental health in the healthcare workers is paramount not only to constitute the front line response against high-threat pandemic pathogens but also to set good example for the public as healthcare workers are the main force to perform the medical procedures for patients.
It was reported that a huge proportion of nurses working for the patients with SARS infection experienced psychological problem.[11] In addition, most of healthcare nurses in Saudi Arabia were found to have an emotional impairment during the medical process in treating patients with Middle East respiratory syndrome (MERS) infection.[12] Currently, as the rapid escalation of coronavirus disease 2019 (COVID-19) over the global scale accompanied with the increasing number of the deaths derived from this pandemic disease, elevated levels of anxiety and stress among the healthcare nurses could be attributed to involuntary affection occurred in the bidirectional interactions deriving from the patients even their colleagues.[13] Moreover, if the patients are dead, there is a higher probability of traumatization disorders occurring on these healthcare workers who cover these patients.
The close contact with the patients in the severe condition combined with the tense atmosphere in the work environment may render the nurses working in the CCU (Critical Care Unit) and ICU (Intensive Care Unit) more possibility of being vulnerable to the psychological stress than those working in the general ward.[14,15] However, the previous report revealed that vicarious traumatization severity of non-frontline nurses is more serious than that of front-line nurses when under the current COVID-19 outbreak.[16] Therefore, the evidence of the psychological condition of the nurses working in the different ward is still lacking. To this end, this study aimed to provide the updated information with regard to the mental health condition among the frontline nurses working in the different ward treating with COVID-19 patients.
2. Methods
2.1. Settings and participants
The data collection of the study is performed by using the questionnaire survey (https://www.wjx.cn) via an app named “Wechat” (Chinese version of WhatsApp) on the smart cellphone due to the official requirement of keeping the safe distance and avoiding the gathering. From February 26, 2020 to March 19, 2020, this survey was completed by 2 independent medical staff. This study was approved by the ethics committee of Yichang Central People's Hospital.
At the time of the COVID-19 outbreak, a total of 159 nurses who were providing nursing care for patients with COVID-19 infection in our hospital participated our survey by filling in the questionnaire.
2.2. Measures
First, the demographic data consisting of gender, age, professional titles, years of working, educational background, marriage status, number of child, duration of shift, precaution measures, previous experience of working with the pandemic outbreak, prior knowledge about COVID-19 as well as the whole working time in this outbreak were collected. Next, the psychological condition of the healthcare nurses working with the COVID-19 patients in different ward was assessed. Basically, the subjects were divided into 2 groups, 1 for the critical care ward (Intensive Care unit (ICU), Respiratory and Critical Care Medicine as well as Infectious Disease) which provide the nursing care mainly consisting of invasive procedure such as mechanical ventilation, and the other 1 for the non-critical care ward (general ward) which provided the medical care for COVID-19 patients with mild symptoms or condition. The questionnaire was modified according to the reported trauma-related evaluation, such as the Traumatic Stress Institute Belief Scale,[17] Impact of event scale revised (IES-R)[18] as well as the stress questionnaire[19] for assessing the psychological disorders and distress in hospital workers. Cronbach's alpha (internal consistency)[20] for the questionnaire in our study reached 0.94, demonstrating its favorable reliability.
2.3. Statistical analysis
SPSS (version 25.0) was used for all analyses. Mean ± SD was used to describe the continuous measurements if they are normally distributed or the interquartile range (IQR) was used if not, and categorical variables were presented as count (%). A t-test or ANOVA was utilized to evaluate the group difference for continuous measurements and Chi-squared analysis was used to assess the group difference for categorical variables. Data were considered statistically significant when P < .05
3. Results
3.1. Investigation of general characteristic between nurses from critical care ward and non-critical care ward
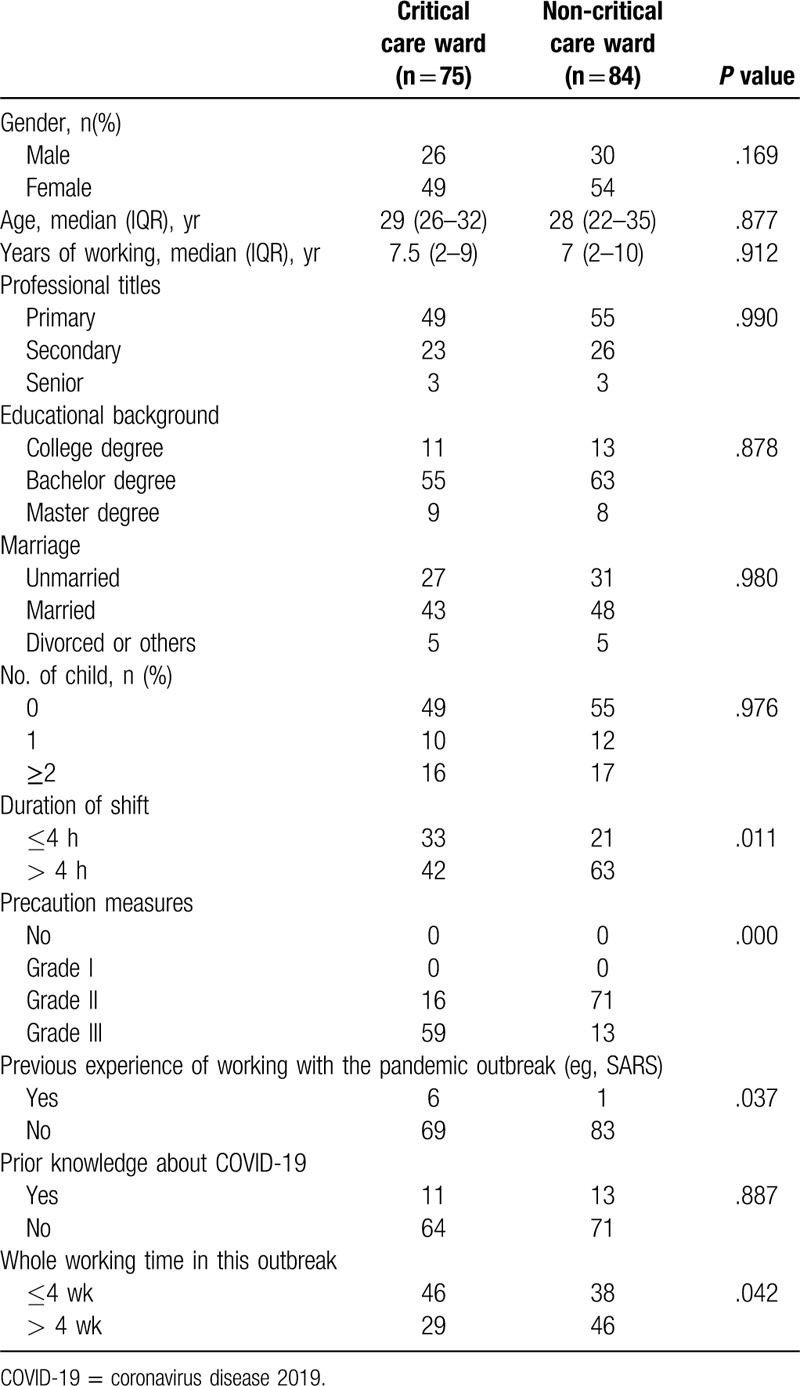
A total of 159 individuals (75 nurses in critical care ward, and 84 nurses in non-critical care ward) were enrolled in our study. There was no significant difference between these 2 groups regarding to the gender, age, years of working, professional titles, educational background, the number of child as well as prior knowledge about COVID-19 (P > .05). However, a significant difference was observed between the 2 groups with regard to the duration of shift (P = .011), precaution measures (P = .000), previous experience of working with the pandemic outbreak (eg, SARS) (P = .037) and whole working time in this outbreak (P = .042) (Table 1).
Table 1.
Comparison of general characteristics nurses from the critical care ward and non-critical care ward.
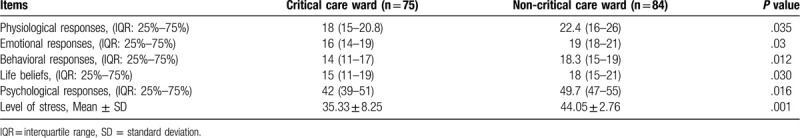
3.2. Comparison of traumatization condition and stress level between nurses from critical care ward and non-critical care ward
The traumatization condition scores consisting of physiological, emotional, behavioral and psychological responses as well as the life beliefs showed a statistical difference between the critical care ward and non-critical care ward (P < .05), suggesting the nurses from non-critical care ward experienced more severe psychological distress during this outbreak of COVID-19 (Table 2). Similarly, the markedly increased level of stress was observed in the nurses working in the non-critical care ward compared with those in the critical care ward (44.05 ± 2.7 vs 35.33 ± 8.25, P < .01).
Table 2.
Comparison of traumatization condition and stress level between the nurses from the critical care ward and non-critical care ward.
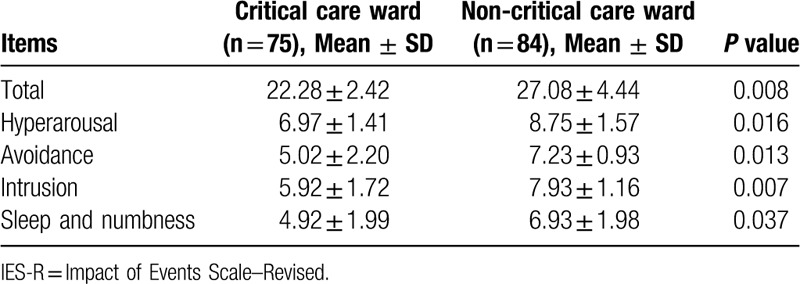
3.3. Evaluation of IES-R sub-scores between nurses from critical care ward and non-critical care ward
The healthcare nurses working in the non-critical care ward had significantly higher IES-R scores (total, P < .01) and sub-items, consisting of hyperarousal (P < .05), avoidance (P < .05), intrusion (P < .05), and sleep and numbness (P < .05), than those who were engaged in the critical care ward (Table 3).
Table 3.
Comparison of IES-R sub-scores between the nurses from the critical care ward and non-critical care ward.
4. Discussion
Although the global pandemic of COVID-19 stimulated a number of related researches, few evidence was reported on the psychological impact of healthcare nurses who directly provide the nursing care for infectious patients.[21,22] Notably, psychological evaluation in medical professionals especially the nurses, are of great importance for controlling the spreading of pandemics, further providing solid evidence for rapid social recovery after this COVID-19 outbreak. In this study, our findings revealed that during the COVID-19 outbreak, the nurses working in the non-critical care wards not only exhibited higher traumatization condition and stress level but also scored higher on the IES-R level, pointing out the future potential target for the mental healthcare of the nurses--those working in the non-critical care ward. Our results are consistent with the findings reported by Yang et al. who concluded that vicarious traumatization scores were significantly lower in the front-line nurses during COVID-19 outbreak.[16] To our best knowledge, this study is the first to evaluate the psychological disorders condition among the frontline nurses working in the different occupational wards.
The main symptoms of psychological disorders after the outbreak of infectious diseases consisted of several unique aspects such as fear, physical decline, irritability, sleep disorder, numbness, fatigue, inattention, and even despair. Normally, these symptoms may give rise to trauma responses and interpersonal conflicts.[23] Previous study has also proved that the post-traumatic stress disorder (PTSD) showed tremendously increased prevalence among the healthcare workers at the end of the infectious diseases.[24] Thus, the medical staff will more or less experience mental disorder during and after the COVID-19 pandemic. To this end, recognizing and providing optimized strategy to solve this mental stress issues among the healthcare professionals at an early stage is crucial.
In the past, the healthcare individuals who performed MERS related tasks showed more serious mental impact upon themselves compared with general public.[25] Consistently, the research focusing on the 2003 SARS outbreak proving that nearly a half of healthcare staffs experienced serious mental stress after the outbreak.[8,26] Among the different occupational ward, it is well acknowledged that the nurses working in the critical care ward may easily experience more severe psychological problems or distress because they normally perform routine task involving invasive procedures (airway suction, manual ventilation, etc) with high risk exposure to the infectious patients.[27,28] However, in our study, we reveal that the traumatization distress and psychological impact of non-critical care ward nurses are more severe than those working in the critical care wards. We consider it may be attributed to the several reasons as follows: First, the nurses who worked in the critical care ward were selected preferentially upon those who have previous experience with the similar pandemic outbreak (eg, SARS) (P < .05, compared with the nurses in the non-critical care ward). In other word, the mental endurance of nurses working in the critical care ward is stronger. Second, advanced precaution measures implemented on the nurses working in the critical care ward (P < .001) rendered them more invulnerable when facing the similar negative psychological impact. Third, the more serious psychological burden derived from the longer duration of shift of the nurses working in the non-critical care ward may partially explain the difference in the psychological impact.
Our findings may provide critical information for further strategy to manage and address the psychological distress among healthcare professionals:
-
(1)
Optimal or advanced precaution measures need to be implemented for all the nurses who perform the COVID-19 related tasks;
-
(2)
Effective strategy to curtail the working duration in each shift should be taken in consideration to minimalize the fear, distress and other psychological disorder among the nurses;
-
(3)
The government is compulsory to announce the elaborate information regarding to the epidemic characteristics of COVID-19 especially for the healthcare nurses.
This study has several limitations. First, limited numbers of subjects may give rise to the selection bias, which may result in certain impact upon the conclusion. Thus, we are further planning to enroll more subjects in our study to enlarge the research scale to address this issue. Secondly, as a descriptive cross-sectional 1, the correlation between different factors is difficult to assess in our study. To this end, a longitudinal large-sized intervention study involving more medical staff such as doctors or medical workers needs to be evaluated for better investigation of the detailed underlying characteristics of psychological disorder in the healthcare setting.
5. Conclusion
Our results suggest that the traumatization condition and stress level of non-critical care ward is more serious than that of critical care ward. Therefore, future intervention for preventing the mental crisis among the healthcare nurses needs to be focusing on the individuals in the non-critical care ward instead of those in the critical care ward.
Author contributions
Dr K. Shou had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Acquisition, analysis, or interpretation of data: X. Song, W. Wu, H. Xie.
Administrative, technical, or material support: H. Xie, X. Cheng.
Concept and design: J. Chen, Z. Xi, K. Shou.
Critical revision of the manuscript for important intellectual content: X. Cheng, Z. Xi.
Drafting of the manuscript: H. Xie, K. Shou.
Obtained funding: Z. Xi, K. Shou.
Statistical analysis: X. Song, H. Xie.
Supervision: J. Chen, Z. Xi, K. Shou.
Footnotes
Abbreviations: COVID-19 = coronavirus disease 2019, IES-R = impact of event scale -revised.
How to cite this article: Xie H, Cheng X, Song X, Wu W, Chen J, Xi Z, Shou K. Investigation of the Psychological disorders in the healthcare nurses during a coronavirus disease 2019 outbreak in China. Medicine. 2020;99:34(e21662).
HX, XC, and XS contributed this work equally. Dr K. Shou had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
This work was supported by Grants from the Hubei Natural Science Foundation of China (Grant no. 2019CFB550).
The authors have no conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
- [1].Lu M, Lu Z, Zhang T, et al. Efficacy and safety of Chinese patent medicine injection for COVID-19: a protocol for systematic review and meta-analysis. Medicine 2020;99:e20706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (London, England) 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Choi KR, Skrine Jeffers K, Logsdon MC. Nursing and the novel coronavirus: risks and responsibilities in a global outbreak. J Adv Nurs 2020;76:1486–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet (London, England) 2020;395:565–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med 2020;8:e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Wu P, Fang Y, Guan Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry 2009;54:302–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Maunder RG, Lancee WJ, Rourke S, et al. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom Med 2004;66:938–42. [DOI] [PubMed] [Google Scholar]
- [9].Kang X, Fang Y, Li S, et al. The benefits of indirect exposure to trauma: the relationships among vicarious posttraumatic growth, social support, and resilience in ambulance personnel in China. Psychiatry Investig 2018;15:452–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Chughtai AA, Seale H, Islam MS, et al. Policies on the use of respiratory protection for hospital health workers to protect from coronavirus disease (COVID-19). Int J Nurs Stud 2020;105:103567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Chen CS, Wu HY, Yang P, et al. Psychological distress of nurses in Taiwan who worked during the outbreak of SARS. Psychiatr Serv 2005;56:76–9. [DOI] [PubMed] [Google Scholar]
- [12].Nour M, Babilghith A, Natto H, et al. Knowledge, attitude and practices of healthcare providers towards MERS-CoV infection at Makkah hospitals, KSA. Int J Res Med Sc 2015;3:103–12. [Google Scholar]
- [13].Mathieu F. Occupational hazards: compassion fatigue, vicarious trauma and burnout. Can Nurse 2014;110:12–3. [PubMed] [Google Scholar]
- [14].Salmon G, Morehead A. Posttraumatic stress syndrome and implications for practice in critical care nurses. Crit Care Nurs Clin North Am 2019;31:517–26. [DOI] [PubMed] [Google Scholar]
- [15].Faraji A, Karimi M. Occupational stress and its related demographic factors among Iranian CCU nurses: a cross-sectional study. BMC Res Notes 2019;12:634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Li Z, Ge J, Yang M, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Lisa McCann I, Pearlman LA. Vicarious traumatization: a framework for understanding the psychological effects of working with victims. J Trauma Stress 1990;3:131–49. [Google Scholar]
- [18].Jenkins SR, Baird S. Secondary traumatic stress and vicarious trauma: a validational study. J Trauma Stress 2002;15:423–32. [DOI] [PubMed] [Google Scholar]
- [19].DePrince AP, Zurbriggen EL, Chu AT, et al. Development of the trauma appraisal questionnaire. J Aggress Maltreat Trauma 2010;19:275–99. [Google Scholar]
- [20].Tavares LS, Moreno NA, de Aquino BG, et al. Reliability, validity, interpretability, and responsiveness of the DEMMI mobility index for Brazilian older hospitalized patients. PLoS One 2020;15:e0230047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA 2020;Feb 24. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- [22].Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Creighton G, Oliffe JL, Ferlatte O, et al. Photovoice ethics: critical reflections from men's mental health research. Qual Health Res 2018;28:446–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Hong X, Currier GW, Zhao X, et al. Posttraumatic stress disorder in convalescent severe acute respiratory syndrome patients: a 4-year follow-up study. Gen Hosp Psychiatry 2009;31:546–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Lee SM, Kang WS, Cho AR, et al. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Comprehensive Psychiatry 2018;87:123–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Chan AO, Huak CY. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occupational medicine (Oxford, England) 2004;54:190–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Borenstein M. Compassion fatigue and vicarious trauma in caregivers. Soins Pediatrie, puericulture 2018;39:13–5. [DOI] [PubMed] [Google Scholar]
- [28].Taylor J, Bradbury-Jones C, Breckenridge JP, et al. Risk of vicarious trauma in nursing research: a focused mapping review and synthesis. J Clin Nurs 2016;25:2768–77. [DOI] [PubMed] [Google Scholar]


