Abstract
An intermittent closure with silk suture is routinely used for closing different surgical wounds. However, subcuticular closure with absorbable sutures has gained considerable attention due to convenience and better cosmetic appearance.
To compare the clinical outcomes and risk of surgical-site infection of subcuticular and intermittent closure after total-knee arthroplasty (TKA), 106 patients that underwent TKA between January 2017 to June 2019 at the Department of Orthopedics in Xiangya Hospital of Centre South University were retrospectively assessed. Forty-three had received running subcuticular closure (group A) and 58 underwent intermittent closure (group B). The Knee Society score was measured before and 6 months after operation. Inflammation markers including the serum levels of procalcitonin, interleukin-6, and C-reactive protein, and the erythrocyte sedimentation rate were evaluated before operation, 1 day after and 1 month after operation. Patient satisfaction with the closure was evaluated using the Likert scale at the last follow-up.
No significant difference was seen in the 6-month postoperative Knee Society score, or in the 1-day and 6-month postoperative inflammation marker levels between both groups (P > .05). Likert scores were higher in group A compared to group B (4.0 ± 1.0 vs 3.6 ± 1.2, P < .05).
Running subcuticular closure after TKA results in a better appearance compared to intermittent closure, although neither method has an advantage in terms of efficacy and risk of infection.
Keywords: clinical outcome, surgical-site infections, total-knee arthroplasty
1. Introduction
Poor skin closure after total-knee arthroplasty (TKA) may lead to pain, impaired physical activity and joint stiffness,[1,2] in addition to surgical-site infections (SSIs) that may progress to a periprosthetic joint infection and bring economic burdens.[3,4] In addition to running subcuticular or intermittent closure using staples or barbed sutures,[5–7] a novel “zip” device and skin adhesives have also been explored for post-TKA skin closure.[8,9] Although intermittent closure with silk suture is routinely used for different surgical wounds, subcuticular closure with absorbable sutures are increasingly being considered owing to their convenience and better cosmetic appearance. In this retrospective study, we compared the 6-month clinical outcome of running subcuticular closure and intermittent closure post-TKA.
2. Materials and methods
2.1. Patients
A total of 106 patients aged 50 to 81 years who had undergone primary TKA at the department of orthopedics in Xiangya Hospital of Centre South University (Reviewer #1 point 1) from January 2017 to June 2019 were enrolled after ethics committee review approval. All surgeries were performed by 1 surgeon. Patients that received bilateral TKA and those without knee osteoarthritis were excluded. Absorbable suture was used for running subcuticular closure in all surgeries until April 2018 (group A), whereas intermittent closure was performed using silk suture (group B). The final analysis was conducted on 101 patients since 5 were lost during the 6-month follow-up.
2.2. Surgical technique
Cemented prostheses were implanted after osteotomy and a test model using the medial patellar approach. The length of incision ranged between 15 and 20 cm. After placing a drainage tube, the tendon, subcutaneous, and skin layers were sequentially closed with 0 absorbable line (VICRYL Plus VCP358 and Stratafix SXPP1A401), a 2-0 PDO (QUILL RA-1028Q), and 3-0 monoderm (YA-1023Q; group A) or silk (MERSILK W570; group B) suture, respectively. Antibacterial prophylaxis, painkillers, and anticoagulant were used in all patients postoperatively. Wound dressing was changed once in 3 days, and the stitches were taken out 14 days after surgery in group B. All patients received the same rehabilitation postoperatively (Figs. 1 and 2).
Figure 1.

(A) Running subcuticular postoperation. (B) Running subcuticular closure at the last follow-up. (C) AP X-ray for knee in running subcuticular closure group preoperation. (D) Lateral X-ray for knee in running subcuticular closure group preoperation. (E) Lateral X-ray for knee in running subcuticular closure group at the last follow-up. (F) AP X-ray for knee in running subcuticular closure group at the last follow-up.
Figure 2.

(A) Intermittent closure postoperation. (B) Intermittent closure at the last follow-up. (C) AP X-ray for knee in intermittent closure group preoperation. (D) Lateral X-ray for knee in intermittent closure group preoperation. (E) Lateral X-ray for knee in intermittent closure group at the last follow-up. (F) AP X-ray for knee in intermittent closure group at the last follow-up.
2.3. Parameters
The Knee Society score (KSS) was assessed before and 6 months after the operation. Inflammatory markers including serum levels of procalcitonin (PCT), interleukin (IL)-6, and C-reactive protein (CRP), and the erythrocyte sedimentation rate (ESR) were measured before, 1 day postsurgery, and 1 month after operation. Patient satisfaction with skin closure was evaluated using the Likert scale at the last follow-up. In addition, all surgery and postoperation hospital records were also collected.
2.4. Statistical analysis
The data were analyzed by the IBM SPSS 19.0 statistical software. Age, BMI, KSS, inflammation marker levels, and Likert scores were compared using independent-samples t test. The Chi-squared test was used to assess categorical variables like sex. P < .05 was considered statistically significant.
3. Results
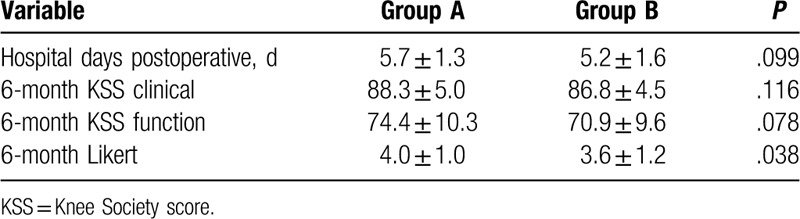
The 6-month postoperative clinical (88.3 ± 5 vs 86.8 ± 4.5) and functional (74.4 ± 10.3 vs 70.9 ± 9.6) KSS were similar between the running subcuticular and intermittent closure groups. Likewise, the duration of postoperation hospitalization also did not show any significant difference between both groups (running subcuticular closure 5.7 ± 1.3 days vs 5.2 ± 1.6 days intermittent closure). However, patients that received the running subcuticular closure expressed greater satisfaction in terms of the Likert score compared to the intermittent closure group (4 ± 1.0 vs 3.6 ± 1.2; P < .05). The inflammation-related markers were also not significantly different between the 2 groups (Reviewer #1 point 4). For instance, PCT levels 1-day and 1-month postoperation were, respectively, 0.06 ± 0.04 μg/L and 0.06 ± 0.13 μg/L in the running subcuticular closure group, and 0.07 ± 0.06 μg/L and 0.05 ± 0.04 μg/L in the intermittent closure group. Similarly, the IL-6 levels at the above time points were 43.35 ± 34.86 pg/mL and 6.19 ± 3.83 pg/mL in the running subcuticular closure group, and 55.12 ± 38.72 pg/mL and 7.79 ± 7.68 pg/mL in the intermittent closure group. Postoperative CRP levels were, respectively, 27.00 ± 23.28 mg/L and 9.29 ± 11.48 mg/L after 1 day and 1 month in the running subcuticular closure group, and 32.96 ± 22.21 mg/L and 17.33 ± 34.08 mg/L in the intermittent closure group. Finally, the 1-day and 1-month postoperative ESR in the running subcuticular closure group were 46.53 ± 33.01 mm/h and 55.63 ± 31.07 mm/h, respectively, and 38.86 ± 31.07 mm/h and 62.52 ± 30.59 mm/h in the intermittent closure group at the same time points. In addition, no severe adverse events occurred in either group except for 1 case in the running subcuticular closure group that showed superficial infection 3 months after the operation. The patient was treated with sensitive antibiotics, debridement, and polyethylene liner replacement (Reviewer #1 point 4, Reviewer #1 point 6) (Tables 1–3).
Table 1.
Comparison between 2 types of closures preoperative.

Table 3.
Comparison between 2 types of closures postoperative.

Table 2.
Comparison between 2 types of closures postoperative.
4. Discussion
Wound closure after TKA affects the outcome and risk of infection. We compared 2 common techniques of wound closure in 101 patients, and did not observe any significant differences in the 6-month follow-up KSS or inflammation markers. However, the subjective Likert score was higher for patients who underwent running subcuticular closure compared to those that received an intermittent closure.
The outcomes of TKA are pain relief and improved range of motion and function of the knee. Rehabilitation training is necessary following TKA[10,11] to prevent joint contracture, deep vein thrombosis (Reviewer #1 point 7) or hypostatic pneumonia. The tension is distributed uniformly along the entire incision in running subcuticular closure, whereas that in the intermittent closure method is restricted to the elevated stitch compared to the region between consecutive stitches. This difference in tension distribution can potentially affect early pain and the range of knee motion, resulting in different outcomes. However, we found no significant differences in the outcomes between both suture techniques, indicating that the latter is not a determinant of TKA efficacy. This is consistent with previous studies that have compared various wound closure methods used in TKA and found no major differences in terms of the 6-month outcome. However, Smith et al reported a higher incidence of superficial dehiscence with barbed sutures.[6]
Cosmetic appearance postsurgery is an important part of patient satisfaction, and as per the Likert scale, was higher in patients that received absorbable sutures. This is likely due to the fact that the rough surface of unabsorbable silk suture can lead to aseptic inflammation of the local skin, and its uneven tension results in the formation of centipede-like scar perpendicular to the suture. In addition, removal of these stitches leaves “pinholes” that can occasionally cause a localized skin inflammation.
Periprosthetic infection is a serious complication of TKA that incurs extensive costs and poor prognosis.[12,13] The running subcuticular closure results in better skin and soft-tissue perfusion close to the incision compared to intermittent closure,[14] which accelerates wound healing. Furthermore, the tighter suture used in intermittent closure not only worsens perfusion but also prevents drainage of the liquefied subcutaneous fat, which may lead to subcutaneous necrosis and infection[15] (Reviewer #1 point 4). We evaluated the levels of CRP, ESR, PCT, and IL-6, which are reliable makers of SSIs,[16,17] and found no differences between 2 groups. This can be attributed to the imperceptible antibacterial effect of absorbable sutures, as well as the elevated IL-6, CRP, and ESR following stress response postoperation (Reviewer #1 point 5). Yoon et al conducted a meta-analysis of 18 studies including 1835 subjects, a high positive likelihood ratio were found in both IL-6 and PCT test indicated both of them may be a good rule-in tests for the diagnosis of periprosthetic joint infection[18] (Reviewer #1 point 3). Lin et al recently concluded a prospective, randomized, open-label clinical trial on the risk of SSIs in patients that received triclosan-coated or plain polyglactin sutures after TKA, and detected lower levels of IL-6 with the former between 4 weeks and 3 months after operation.[19]
All the surgeries included in our study were performed by one surgeon, thus eliminating any possible bias due to individual variations. Furthermore, the risk of infection was assessed using objective indicators like IL-6, PCT, ESR, and CRP which eliminated observer bias. However, the retrospective nature of the study was a limitation, along with heterogeneity among the patients and the inaccuracy of the time of wound closure. Some potentially confounding variables like self-healing ability, history of using corticosteroids, or incomplete medical records were also not considered. Nevertheless, we can conclude from our findings that the running subcuticular closure results in better cosmetic appearance compared to intermittent closure, without affecting the 6-month outcome and risk of SSIs.
5. Conclusion
Running subcuticular closure after TKA results in a better appearance compared to intermittent closure, although neither method has an advantage in terms of function and risk of infection.
Author contributions
Liang Chen and Min Zeng designed the study.
Jie Xie, Yihe Hu, and Min Zeng performed the surgeries.
Liang Chen, Junxiao Yang, and Min Zeng collected and analyzed the data.
Liang Chen and Min Zeng wrote the main manuscript.
All authors reviewed the manuscript.
Footnotes
Abbreviations: CRP = C-reactive protein, ESR = erythrocyte sedimentation rate, IL-6 = interleukin-6, KSS = Knee Society score, PCT = procalcitonin, SSIs = surgical-site infections, TKA = total-knee arthroplasty.
How to cite this article: Chen L, Yang J, Xie J, Hu Y, Zeng M. Clinical outcome of different skin closure in total-knee arthroplasty: running subcuticular closure vs intermittent closure: a retrospective study. Medicine. 2020;99:34(e21947).
This work was supported by the Natural Science Foundation of Hunan Province (grant number: 2019JJ50951) and Changsha Science and Technology project (grant number: kq1907153).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Zech A, Hendrich S, Pfeifer K. Association between exercise therapy dose and functional improvements in the early postoperative phase after hip and knee arthroplasty: an observational study. PM R 2015;7:1064–72. [DOI] [PubMed] [Google Scholar]
- [2].Hardt S, Schulz M, Pfitzner T, et al. Improved early outcome after TKA through an app-based active muscle training programme-a randomized-controlled trial. Knee Surg Sports Traumatol Arthrosc 2018;26:3429–37. [DOI] [PubMed] [Google Scholar]
- [3].Roerdink RL, Plat AW, van Hove RP, et al. Reduced wound leakage in arthroplasty with modified wound closure: a retrospective cohort study. Arch Orthop Trauma Surg 2019;139:1505–10. [DOI] [PubMed] [Google Scholar]
- [4].Zawadzki N, Wang Y, Shao H, et al. Readmission due to infection following total hip and total knee procedures: a retrospective study. Medicine (Baltimore) 2017;96:e7961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Yuenyongviwat V, Iamthanaporn K, Hongnaparak T, et al. A randomised controlled trial comparing skin closure in total knee arthroplasty in the same knee: nylon sutures versus skin staples. Bone Joint Res 2016;5:185–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Smith EL, DiSegna ST, Shukla PY, et al. Barbed versus traditional sutures: closure time, cost, and wound related outcomes in total joint arthroplasty. J Arthroplasty 2014;29:283–7. [DOI] [PubMed] [Google Scholar]
- [7].Newman JT, Morgan SJ, Resende GV, et al. Modality of wound closure after total knee replacement: are staples as safe as sutures? A retrospective study of 181 patients. Patient Saf Surg 2011;5:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Benner RW, Behrens JP. A novel skin closure device for total knee arthroplasty: randomized controlled trial versus staples. J Knee Surg 2019. [DOI] [PubMed] [Google Scholar]
- [9].Yuenyongviwat V, Iamthanaporn K, Tuntarattanapong P, et al. Adhesive strips as the sole method for skin closure is effective in total knee arthroplasty. J Orthop Surg (Hong Kong) 2019;27:1–4. [DOI] [PubMed] [Google Scholar]
- [10].Moffet H, Collet JP, Shapiro SH, et al. Effectiveness of intensive rehabilitation on functional ability and quality of life after first total knee arthroplasty: a single-blind randomized controlled trial. Arch Phys Med Rehabil 2004;85:546–56. [DOI] [PubMed] [Google Scholar]
- [11].Christensen JC, Paxton RJ, Baym C, et al. Benefits of direct patient discharge to outpatient physical therapy after total knee arthroplasty. Disabil Rehabil 2019;42:660–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Delanois RE, Mistry JB, Gwam CU, et al. Current epidemiology of revision total knee arthroplasty in the United States. J Arthroplasty 2017;32:2663–8. [DOI] [PubMed] [Google Scholar]
- [13].Ma CY, Lu YD, Bell KL, et al. Predictors of treatment failure after 2-stage reimplantation for infected total knee arthroplasty: a 2- to 10-year follow-up. J Arthroplasty 2018;33:2234–9. [DOI] [PubMed] [Google Scholar]
- [14].Wyles CC, Jacobson SR, Houdek MT, et al. The Chitranjan Ranawat Award: running subcuticular closure enables the most robust perfusion after TKA: a randomized clinical trial. Clin Orthop Relat Res 2016;474:47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Liu S, Wang Y, Kotian RN, et al. Comparison of nonabsorbable and absorbable suture in total knee arthroplasty. Med Sci Monit 2018;24:7563–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Drago L, Vassena C, Dozio E, et al. Procalcitonin, C-reactive protein, interleukin-6, and soluble intercellular adhesion molecule-1 as markers of postoperative orthopaedic joint prosthesis infections. Int J Immunopathol Pharmacol 2011;24:433–40. [DOI] [PubMed] [Google Scholar]
- [17].Parvizi J. New definition for periprosthetic joint infection. Am J Orthop (Belle Mead NJ) 2011;40:614–5. [PubMed] [Google Scholar]
- [18].Yoon JR, Yang SH, Shin YS. Diagnostic accuracy of interleukin-6 and procalcitonin in patients with periprosthetic joint infection: a systematic review and meta-analysis. Int Orthop 2018;42:1213–26. [DOI] [PubMed] [Google Scholar]
- [19].Lin SJ, Chang FC, Huang TW, et al. Temporal change of interleukin-6, C-reactive protein, and skin temperature after total knee arthroplasty using triclosan-coated sutures. Biomed Res Int 2018;2018:9136208. [DOI] [PMC free article] [PubMed] [Google Scholar]


