Abstract
A new study uses the OpenSAFELY health analytics platform to identify risk factors for COVID-19 mortality. This analysis, which includes data for more than 17 million people in the UK, suggests that patients with chronic kidney disease are at higher risk than those with other known risk factors, including chronic heart and lung disease.
Subject terms: End-stage renal disease, Risk factors, SARS-CoV-2
Refers to Williamson, E. J. et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 10.1038/s41586-020-2521-4 (2020)
To aid efforts to manage the coronavirus disease 2019 (COVID-19) pandemic, it is essential to understand the epidemiology of the disease. We need to know which individuals are at increased risk of SARS-CoV-2 infection as well as their risk of morbidity and mortality if they become infected. The number of articles describing these aspects is multiplying almost at the same pace as the pandemic, reflecting our uncertainty regarding this disease. The first publications described single-centre experiences in small numbers of patients in China where the pandemic was first reported1. These reports were soon followed by multicentre experiences from China2, and shortly thereafter from Europe3,4 and the USA5, mimicking the course of the epicentre of the pandemic as it moved across the globe. In general, these reports identify older age, male sex, obesity, hypertension, diabetes, cardiovascular disease and chronic lung disease as risk factors for COVID-19 mortality. Notably, few reports have mentioned the possible importance of chronic kidney disease (CKD). A new study by Williamson et al. recently published in Nature addresses this knowledge gap6.
Reported mortality rates and the risk conferred by individual risk factors differ considerably between COVID-19 studies. This variation can only partly be explained by differences in the age distributions of the study populations7. At least two other methodological aspects should be taken into consideration. First, it is important to note the study population. Some papers describe outcomes in the general population, whereas others report on disease-specific populations, for example, patients with a history of cardiovascular disease8. Moreover, some studies include all patients who are diagnosed with COVID-19, whereas others include only those who are hospitalized. It is to be expected that disease-specific cohorts, especially those that only include hospitalized patients, will have higher mortality rates and different risk factor profiles from general population cohorts that include all infected patients. Second, the criteria used to identify infected patients differ between studies. In some studies, patients are classified as having COVID-19 based merely on clinical suspicion, whereas in others they must have a positive PCR test on a nasopharyngeal swab or a CT scan showing abnormalities compatible with the disease. In addition, some studies screened patients because of signs or symptoms of COVID-19, whereas others also screened asymptomatic contacts of infected patients. Inclusion of asymptomatic patients in study populations will result in lower COVID-19-associated mortality rates and a different risk factor profile.
In the study by Williamson et al., the researchers created a secure health analytics platform, named OpenSAFELY, which uses data from an electronic health record system that has been widely used in general practice in the UK since 1998 (ref.6). Their analysis was based on the health records of more than 17 million adults for whom at least 1 year of previous data was available. Between 1 February and 6 May 2020, 10,926 individuals were identified as having a COVID-19-related death based on a death certificate mentioning a COVID-19-related ICD-10 code. The large size of the study population enabled the researchers to make well-powered conclusions about vulnerability to COVID-19 in patient subgroups. Notably, in this study design COVID-19 mortality is determined not only by the risk of death for individual patients once infected with SARS-CoV-2, but also by their risk of being infected. Mortality rates are therefore 100- to 1,000-fold lower in this study than in previous reports that reported mortality among infected patients. This study design may also explain, at least in part, some of the findings. For example, people with non-white ethnicity had a 40–50% higher risk of COVID-19-related death than those with white ethnicity. A multivariable Cox proportional hazards model showed that this increased risk of death was only partially attributable to co-morbidities or other known risk factors. Rather than reflecting a higher risk of dying from COVID-19, the higher mortality risk among non-white ethnic groups could potentially reflect a higher risk of contracting the infection owing to differences in living conditions or occupational exposure. Regardless of the explanation, these new data are important from a public health perspective as they could help to identify which population subgroups should be shielded to prevent transmission of the infection.
patients with severe forms of CKD have a very high risk of COVID-19 mortality
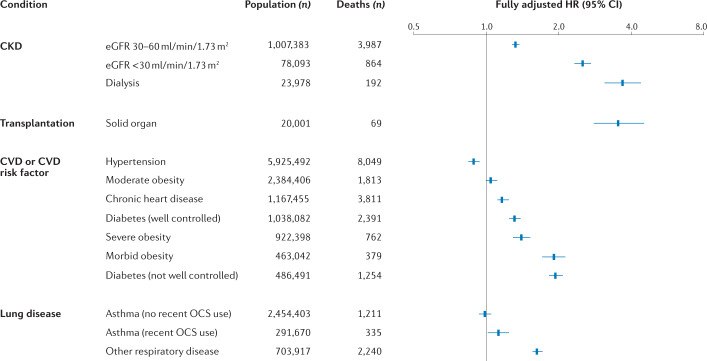
This study also highlights the importance of CKD as a risk factor for COVID-19 mortality. Previous reports either did not include information on CKD or failed to state the definition of CKD used in the study. By contrast, the study by Williamson et al. includes data for three subgroups with CKD (those with an estimated glomerular filtration rate (eGFR) of 30–60 ml/min/1.73 m2, those with an eGFR of <30 ml/min/1.73 m2 and those who were receiving maintenance dialysis) as well as a subgroup of solid organ transplant recipients. Although transplant type is not reported, the majority of this latter group will have received a kidney transplant. When the data for the CKD subgroups are compared, it becomes clear that a graded association exists between the level of kidney dysfunction and the risk of COVID-19 mortality (Fig. 1). These data also demonstrate that patients with severe forms of CKD have a very high risk of COVID-19 mortality, which is even higher than that of other known high-risk groups, including patients with hypertension, obesity, chronic heart disease or lung disease.
Fig. 1. Risk factors for COVID-19-related deaths identified using the OpenSAFELY database.
Estimated hazard ratios (HRs) from a multivariable model. Error bars represent 95% confidence intervals. All HRs are adjusted for all other factors. Well-controlled diabetes is defined as HbA1c < 58 mmol/mol; not well controlled diabetes is defined as HbA1c ≥ 58 mmol/mol. CKD, chronic kidney disease; CVD, cardiovascular disease; CI, confidence interval; OCS, oral corticosteroids. Data obtained and figure adapted from ref.6, Springer Nature Limited.
The CKD data indicate that these patients deserve special attention with regard to COVID-19. In March 2020, the European Renal Association–European Dialysis and Transplant Association (ERA-EDTA) established the ERACODA database to collect information on the incidence, clinical course and outcomes of COVID-19 in patients with kidney failure (formally known as end-stage kidney disease) who are treated with dialysis or living with a kidney transplant9. Although similar data collections have been initiated at national or regional level, a pan-European database allows collection of a larger patient sample in a shorter timeframe, which will enable timely, statistically well-founded conclusions to be drawn regarding outcomes and risk factors in this vulnerable patient population. This information will have important consequences for clinical decision-making, for example, when deciding whether a patient on dialysis with COVID-19 should be admitted to an intensive care unit.
The CKD data indicate that these patients deserve special attention with regard to COVID-19
In summary, the study by Williamson et al. provides important information on the epidemiology of COVID-19 and is the first to convincingly demonstrate the importance of CKD as a risk factor for COVID-19 mortality. These findings necessitate a call for action. The nephrological community should collect more epidemiological data to obtain a better understanding of the course of COVID-19 and of risk factors for mortality among patients with CKD. We should make every effort to ensure that these patients with high mortality risk are included in clinical trials of disease-modifying treatments. Likewise, patients with CKD, including those who are on dialysis or living with a kidney transplant, should be included in vaccination trials because uraemia and the use of immunosuppressive agents could potentially hamper vaccination responses.
Competing interests
The authors declare no competing interests.
Footnotes
Related links
ERACODA: www.ERACODA.org
Contributor Information
Ron T. Gansevoort, Email: R.T.Gansevoort@umcg.nl
Luuk B. Hilbrands, Email: Luuk.Hilbrands@radboudumc.nl
References
- 1.Huang C, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan WJ, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur. Respir. J. 2020;55:2000547. doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grasselli G, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern. Med. 2020 doi: 10.1001/jamainternmed.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Docherty AB, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. Br. Med. J. 2020;369:m1985. doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim L, et al. Risk factors for intensive care unit admission and in-hospital mortality among hospitalized adults identified through the U.S. Coronavirus Disease 2019 (COVID-19)-associated Hospitalization Surveillance Network (COVID-NET) Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williamson EJ, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sudharsanan N, Didzun O, Bärnighausen T, Geldsetzer P. The contribution of the age distribution of cases to COVID-19 case fatality across countries: a 9-country demographic study. Ann. Intern. Med. 2020 doi: 10.7326/M20-2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li X, et al. Impact of cardiovascular disease and cardiac injury on in-hospital mortality in patients with COVID-19: a systematic review and meta-analysis. Heart. 2020 doi: 10.1136/heartjnl-2020-317062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noordzij M, et al. ERACODA: the European database collecting information of patients on kidney replacement therapy with COVID-19. Nephrol. Dial. Transplant. 2020 doi: 10.1093/ndt/gfaa179/5891689. [DOI] [PMC free article] [PubMed] [Google Scholar]