Abstract
Background
Open defecation was largely a rural phenomenon most widely attributed to poor latrine ownership at community level. We aimed at examining latrine ownership and its determinants in rural villages of the Tigray region, Northern Ethiopia.
Methods
Community-based cross-sectional study was conducted from June to July 2018. A total of 756 randomly selected households were involved in the study. The multistage cluster sampling technique was used to select study households. Data were checked, coded, and entered into Epi-Info version 7. Besides, it was exported to SPSS version 20 for data analysis. Multivariable logistic regression analysis was involved to estimate the net effect size of factors associated with latrine ownership.
Results
The proportion of households owning latrine was 35.7%. The majority (84.4%) of constructed latrines were utilized by household families. Households advocated latrine IEC by Health Extension Workers (HEWs) (AOR = 1.902, 95% CI: 1.269–2.852), living in their private house (AOR = 3.13, 95% CI: 1.528–6.401), and the occupation status of government employees (AOR = 3.54, 95% CI: 0.586–21.397) are more likely to lead to the construction of latrines. The availability of latrine made on slab floor (AOR = 1.790, 95% CI: 0.297–3.102), having a latrine constructed inside the household compound (AOR = 4.463, 95% CI: 1.021–19.516), and delivery of latrine IEC by Women Development Armies (WDAs) (AOR = 2.425, 95% CI: 0.728–8.083) may lead to better latrine utilization at the household level.
Conclusion
Households owning latrine at the community level were low. The desired level of latrine ownership will be realized if all sanitation and hygiene components are kept on eye side by side in line with identified predictor factors.
1. Introduction
Globally, more than 2.5 billion people lacked improved sanitation and hygienic facilities [1]. A disease associated with poor water, sanitation, and hygiene accounts for more than 4% of the total disease burden and deaths [1–3].
Open defecation was largely a rural phenomenon most widely practiced in the southern part of Asia and Sub-Saharan Africa. This was due to poor sanitation and hygienic practice. In Sub-Saharan Africa, an estimated one-third of the population still do not have access to improved hygiene and sanitation facilities [4–6].
In Ethiopia, only six percent of household members were reported using improved hygiene and sanitation facilities. Some evidence suggested that financial constraints of raw materials needed to construct latrine and poor interest of the household members to construct latrine rented house with occupancy of the landlord were factors for enhancing sanitation and hygiene facilities at the community level [3]. Latrine ownership in the rural community was low, resulting in high burden of diarrheal and other communicable diseases. It is evident from Ethiopian Demographic and Health Surveys (EDHS, 2016) that an estimated 56% of the rural households practiced using unimproved latrine [7]. Meanwhile, urban areas were four times more likely to own latrine at the household level [3, 7]. Pooled latrine prevalence (50.02%) was reviewed from 17 community-based studies in Ethiopia. The highest prevalence (67.4%) was documented in Southern Nations Nationality and People Regional State (SNNPS) followed by Amhara Region (50.1%), almost consistent with the national estimate. Respondents who completed high school and above education levels were more likely (1.79; 95% CI: 1.05–3.05) to own latrine at the community level as compared to their counterparts [8].
In the Tigray region of northern Ethiopia, different fragmented small pocket studies have been conducted to assess the level of latrine ownership at the community level in different areas within the region. However, the reported findings were with highly varying figures. Regarding latrine utilization, more than half (59.8%) was reported from the La'ilay Maichew district of central Tigray and Enderta district of Mekelle Zone (68.4%) that showed a significant variability [9, 10]. Meanwhile, latrine prevalence was only reported from South Eastern part of Tigray (53%) [11]. Community members familiar with community lead total sanitation (CLTS) (1.78; 95% CI: 1.57–2.03), accessibility of health facilities near the rural village (2.37; 95% CI: 2.14–2.64), and increased educational attainment of the head of the household were positively influenced the households to own latrine at community level [9].
Increasing latrine prevalence and utilization are essential and a cost-effective strategy to overcome the disease burden associated with improper excreta management by strengthening latrine ownership [12–15]. Latrine ownership is affected by a range of behavioral, cultural, social, geographic, and economic factors across different community members [11, 16–21]. However, reviewed determinant factors of latrine ownership at the regional level in the previous studies were limited to behavioral factors. Besides, none was documented concerning latrine ownership that showed the regional estimate. Therefore, we aimed to use the latrine ownership ladder model [22] (Figure 1) to assess the latrine ownership and its determinant factors in rural villages of the Tigray region, Northern Ethiopia.
Figure 1.
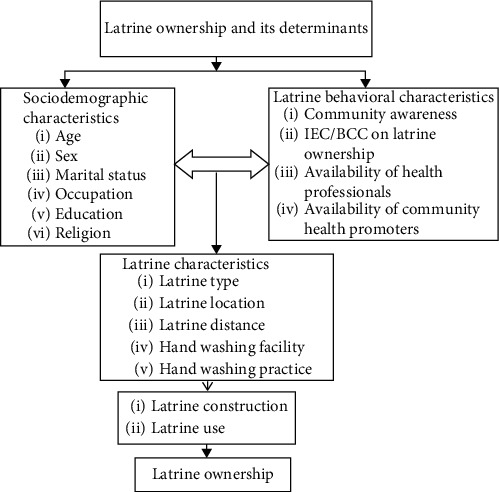
The latrine ownership ladder: a conceptual framework for enhancing sanitation uptake in low-income settings [22].
2. Methods and Materials
2.1. Study Design and Settings
The study involved community-based cross-sectional survey. It was conducted in rural villages of Tigray, Northern Ethiopia from June to July 2018. Tigray region is among the nine regional states administratively demarcated and it is located in the northern part of Ethiopia at a distance of 805 kms from the capital city, Addis Ababa. The region is further administratively subdivided into seven zones, namely, East, South, South East, Western, Northwestern, Central, and Mekelle which contained the smallest administrative units of 52 districts (34 rural and 18 urban) [23] as shown in Figure 2.
Figure 2.
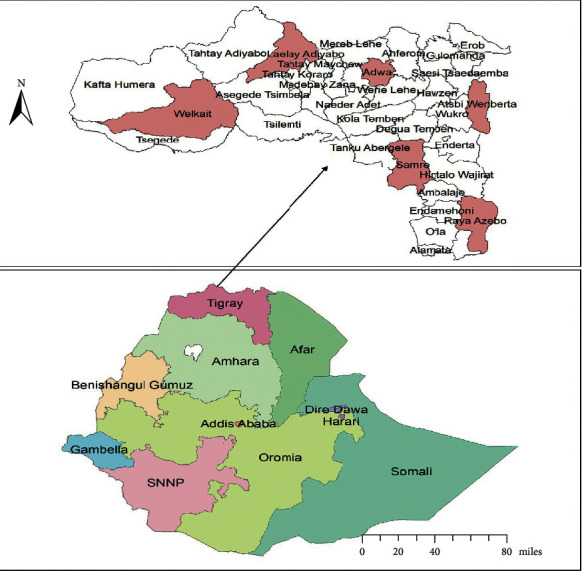
Map of the Tigray region and selected study districts were shaded by rose color.
2.2. Sampling and Sample Size Determination
Multistage cluster sampling techniques were used to select study households. Administrative zones and districts were used as a cluster. Of the seven clusters, one zone (Mekelle) was excluded since it was urban. From the six rural zones, one district was randomly selected making a total of six districts. Meanwhile, twelve kebelles were randomly selected by the lottery method considering two kebelles from each district. Finally, proportional to size allocation was used to select a total household that participated in the study (Figure 3).
Figure 3.
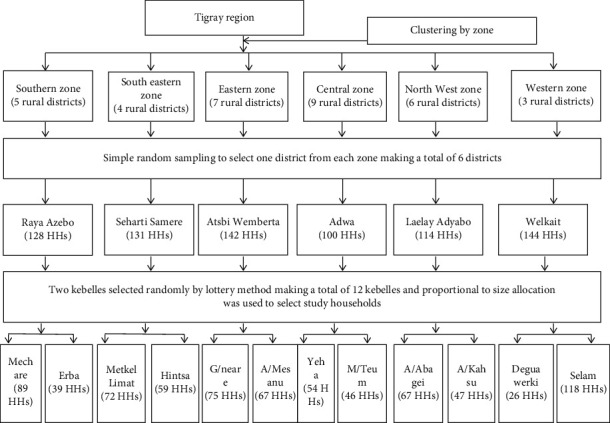
Schematic diagram of the sampling procedure.
The sample size was determined by using single population proportion formula with an assumption of 34% latrine prevalence (P=0.34) from a previous study [24], Z-score Z(α/2) = 1.96 at a confidence level of 95%, and a margin of error ε = 0.05 (5%). The sample size was 690. Since the sampling procedure was multistage, we considered the design effect of 2 and 10% nonresponse rate making a total sample size of 759.
2.3. Data Collection Procedure
We used a standardized pretested structured questionnaire for data collection adopted from previously conducted similar studies [11, 12]. During the data collection procedure, face to face interviews were conducted by the head of the household. Besides, direct observation was involved with household compounds to confirm the availability of latrine, type of latrine, its location, and how it was utilized. The data collection tool was originally prepared in English and translated to Tigrigna (local language), and responses were then translated back to English. Data collection was conducted by recruiting six trained environmental health professionals. Data collection was conducted under the close supervision of the principal investigators.
2.4. Data Quality Assurance
To enhance data quality, training was provided for data collectors and supervisors with the objective of the study, the nature of the data collection tools, ways of approaching during interviews, observation, and inspecting latrines. During the data collection period, there was a strict supervision scheme. Completed questionnaires were checked on a daily basis by a supervisor and principal investigator.
2.5. Operational Definitions
Latrine ownership: the proportion of households owning and utilizing latrine [7].
Hand washing facility: any setup of a container with water and soap in the household compound for hand washing purposes observed at the time of data collection.
Women Development Armies: women enrolled under 25–30 teams for implementing health extension package at the community level.
2.6. Data Processing and Analysis
Data were entered into Epi-info version 7 and exported to SPSS version 20 statistical package for analysis. Frequency distribution and percentages were performed using frequency tables. Bivariate logistic regression analysis was done for each outcome variable for latrine ownership (latrine prevalence and utilization). All variables at P-value of ≤0.25 in the bivariate analysis were included in the multivariable logistic regression model. Finally, all variables with P-value of ≤0.05 were considered statistically significant as predictor factors.
3. Result
3.1. Sociodemographic Characteristics
A total of 756 (99.6%) households completed the study. The majority (98%) of the respondents were Orthodox Christian. More than half (58.2%) were unable to read and write (Table 1).
Table 1.
Sociodemographics of households in rural villages of Tigray, Northern Ethiopia, 2018 (n = 756).
| Characteristics | Frequency (%) |
|---|---|
| Respondent role | |
| Mother | 527 (69.7) |
| Father | 137 (18.1) |
| Adult daughter | 91 (12.1) |
| Gender | |
| Male | 182 (24.1) |
| Female | 574 (75.8) |
| Religious background | |
| Orthodox | 741 (98) |
| Muslim | 11 (1.5) |
| Protestant | 3 (0.4) |
| Age category | |
| <30 years | 257 (44) |
| 30–45 years | 289 (38.2) |
| >45 years | 191 (25.3) |
| Educational status | |
| Able to read and write | 440 (58.2) |
| Unable to read and write | 316 (41.7) |
| Occupational status | |
| Daily laborer | 5 (0.7) |
| Farmer | 676 (89.4) |
| Government employee | 18 (2.4) |
| Merchant | 21 (2.8) |
| Unemployed | 36 (4.7) |
| Marital status | |
| Married | 550 (72.8) |
| Single | 93 (12.3) |
| Divorced | 62 (8.2) |
| Widowed | 48 (6.3) |
3.2. Latrine Ownership and Its Characteristics
The study revealed that 270 (35.7%) surveyed households owned latrine at the community level. More than half (64%) constructed latrines were made of wood and mud floor and were found inside the household compound. Regarding their location, 90.7% were nearly 50 meters away from the kitchen as per standard. Besides, 84.4% of constructed latrines were utilized by household members. Accordingly, the majority (87%) of adults and children utilized latrine regularly. The majority (85.2%) of constructed latrines lacked hand washing facilities. The very low proportion of family members (5.6%) washed their hands with soap and water after latrine use (Table 2).
Table 2.
Latrine ownership and its characteristics among households in rural villages of Tigray, Northern Ethiopia, 2018 (n = 756).
| Characteristics | Frequency (%) |
|---|---|
| Household owned latrine | |
| Yes | 270 (35.7) |
| No | 486 (64.3) |
| Latrine type | |
| Pit latrine with wood and mud floor | 174 (64) |
| Pit latrine with slab floor | 94 (34.8) |
| Ventilated improved pit latrine | 2 (0.7) |
| Latrine location | |
| Inside the compound | 177 (65.6) |
| Outside the compound | 93 (34.4) |
| Latrine distance from the house compound | |
| <50 meters | 245 (90.7) |
| ≥50 meters | 25 (9.3) |
| Latrine utilization | |
| Yes | 228 (84.4) |
| No | 42 (15.6) |
| Household members utilized latrine | |
| Only adults | 33 (12.2) |
| Only children | 2 (0.7) |
| Both adults and children | 235 (87.1) |
| Hand washing practice after latrine use | |
| Yes | 15 (5.6) |
| No | 255 (94.4) |
| Latrine with hand washing facility | |
| Yes | 40 (14.8) |
| No | 230 (85.2) |
| Households knew latrine importance | |
| Yes | 670 (88.6) |
| No | 86 (11.4) |
| Reasons for not constructing latrine | |
| Lack of money | 51 (6.7) |
| Lack of space | 36 (4.8) |
| Demolished latrines | 520 (68.8) |
| Lack of awareness | 53 (7) |
| Others | 96 (12.7) |
| Households having information on latrine | |
| Yes | 549 (72.6) |
| No | 207 (27.4) |
| Source of information | |
| Health extension workers | 277 (50.5) |
| Radio | 130 (23.7) |
| Women development armies | 116 (21.1) |
| Others | 26 (4.7) |
| Possess radio | |
| Yes | 470 (62.2) |
| No | 286 (37.8) |
3.3. Determinant Factors for Latrine Ownership
The study revealed that households advocated latrine IEC by Health Extension Workers (HEWs) (AOR = 1.902, 95% CI: 1.269–2.852), living in a private house (AOR = 3.13, 95% CI: 1.528–6.401), and the occupation status of government employees (AOR = 3.54, 95% CI: 0.586–21.397) were more likely to lead to the construction of latrines. The availability of latrine made on slab floor (AOR = 1.790, 95% CI: 0.297–3.102), having a latrine constructed inside the household compound (AOR = 4.463, 95% CI: 1.021–19.516), and delivery of latrine IEC by Women Development Armies (WDAs) (AOR = 2.425, 95% CI: 0.728–8.083) may lead to better utilized latrine at the household level (Table 3).
Table 3.
Determinants of latrine ownership among households in rural villages of Tigray, Northern Ethiopia, 2018 (N = 756).
| Variables | Latrine ownership | |||
|---|---|---|---|---|
| Latrine prevalence | Latrine utilization | |||
| COR (95% CI) | AOR (95% CI) | COR (95% CI) | AOR (95% CI) | |
| Occupation | ||||
| Farmer | 4.67 (1.072–20.423)∗⊃ | 4.27 (0.92–19.4) | ||
| Government employee | 8.50 ,(1.50448.049)∗ | 3.542 (0.586–21.397) ∗ | 0.27 (0.062–1.187)∗ | 0.25 (0.05–1.13) |
| Unemployed | 1 | 1 | 1 | 1 |
| Marital status | ||||
| Married | 0.39 (0.154–0.995)∗ | 0.36 (0.13–0.95) | ||
| Single | 5 (0.872–28.663) | 4.57 (0.75–27.22) | ||
| Divorced | 2 (0.117–34.096) | 1.83 (0.099–32.39 | ||
| Widowed | 1 | 1 | ||
| Possess radio | ||||
| Yes | 0.82 (0.606–1.117)∗ | 0.75 (0.52–1.06) | ||
| No | 1 | 1 | ||
| Latrine type | ||||
| Slab floor pit | 2.51 (0.103–4.512)∗ | 1.790 (0.296–3.102) ∗ | ||
| Ventilated pit | 1 | 1 | ||
| House ownership | ||||
| Relative | 3.05 (1.107–8.396)∗ | 2.79 (0.95–7.976) | ||
| Private | 3.09 (1.588–5.999)∗ | 3.13 (1.528–6.401) ∗ | ||
| Rental | 1 | 1 | ||
| Latrine location | ||||
| Inside the household compound | 3.991 (0.876–18.183)∗ | 4.463 (1.021–19.516) ∗ | ||
| Outside the household compound | 1 | 1 | ||
| Information source | ||||
| Health extension workers (HEWs) | 0.586 (0.389–0.884)∗ | 1.902 (1.269–2.852) ∗ | ||
| Women development armies (WDAs) | 1.633 (0.422–2.952)∗ | 1.49 (0.36–2.80) | 1.706 (1.1.29–2.579)∗ | 2.425 (0.728–8.083) ∗ |
| Others | 1 | 1 | 1 | 1 |
Note. Abbreviations: AOR: adjusted odds ratio, COR: crude odds ratio, P-value: precision value; statistical decisions: ∗ = P-value ≤0.05; ∗ = P-value <0.01, ∗ = P-value ≤0.001.
4. Discussion
This was the first regional estimate to latrine ownership and its determinants among rural residents in the Tigray region, Northern Ethiopia.
The study revealed that households that owned latrine were 35.7%. Five out of six constructed latrines were utilized by household members. Accordingly, latrine prevalence was almost consistent with the national estimate (44%) as documented in EDHS, 2016 [7]. Similar evidence was reported from South East Zone of Tigray, Northern Ethiopia (37.6%), Central Zone of Tigray, Northern Ethiopia (37.4%), and Dabat district, North West Ethiopia (47%) [11, 25, 26].
As to the factors responsible for latrine ownership, households living in their own house were 3.3 times more likely to construct latrines as compared to their counterparts. This was consistent with the finding in Dabat district, North West Ethiopia, in which households in rented houses had a difficulty in constructing latrines [25]. This finding showed the need for extraordinary attention and awareness creation to address this special community groups.
Study finding showed latrine ownership is low when compared to elsewhere in Bahirdar Zuria of Northern Ethiopia (58.4%) [24], Debere Tabor in Amhara region, Northern Ethiopia (93.5%) [12], and Oromya region, South West Ethiopia (88.2%) [27]. Besides, a report from the current study was lower when compared with evidence from Nepal [17]. The discrepancy might be due to the recruitment of graduated model households due to the implementation of Community Led Total Sanitation (CLTS) in Bahirdar and enrollment of urban households in the remaining two studies. In contrast, the present study recruited all household members from the rural community.
Regarding latrine utilization, it was higher than evidence from systematic reviews at the national level (37.7%), Central zone of Tigray, Northern Ethiopia (58.9%), Awabel district of Amhara region (52%), and Gulomekeda of Tigray region (57.3%) [8, 9, 19, 28]. Latrine location inside the house compound was four times more likely utilized by household members (AOR = 4.463, 95% CI: 1.021–19.516). However, similar evidence was also reported in [8, 9]. Therefore, the variation might be the use of denominator for calculating latrine utilization rate in which the later studies use the total household including those that did not construct latrine, but it is appropriate to use households owned latrine as a denominator [7, 23]. In addition, a pooled result due to systematic reviews of different pocket studies was a reason for the low utilization rate. However, slightly lower evidence was reported from Hullet Ejj Enese of the Amhara region of Northern Ethiopia (92%) and Nepal (94.3%) [17, 29]. The discrepancy among the study findings might be related to climatic zones which are believed to affect the construction and durability of latrines for sustainable use [30–32]. Progressive sanitation facilities and good community awareness might be the reason in Nepal [29]. Similar reports were documented from Jimma of South West Ethiopia (87.8%), Hawassa town of Southern Ethiopia (85.4%), Wondogent of Southern Ethiopia (83%) [33, 34].
As evidenced in Kenya [35] and Ethiopia [36], more than 80% of latrine constructed in rural communities was not used more than one year due to their demolishing characteristics. A similar challenge was reported that forcing households to construct latrine during mass advocacy and campaign results in poor quality latrine construction at the community level. Therefore, it is essential to consider enabling factors for households to own and utilize latrine sustainably. This study reported that constructing latrine using slab floor was two times more likely owned by households than wood and mud floor pit latrines and similarly, three times for privately owned houses and occupation with government employees (Table 2). This finding was consistent with evidence from Hawusen, Dabat, Bahirdar, and Nepal [17, 24, 25, 33].
The scientific evidence shows that household members were four times as likely to use a latrine if it was located inside, rather than outside, the family compound [21, 22]. In this study, more than half of the latrines constructed were located inside the household compound. This was the reason for the high latrine utilization rate evidenced at the community level. Having these realities, program implementers should acknowledge health promoters and households to own latrine inside the household compound. Women Development Armies (WDAs) at the community level reported two times more influence to utilize latrine than health extension workers (HEWs). The reason might be health extension workers were overloaded at the health facility level for health care service provision resulting in poor support for the community than women development armies (WDAs) at the community level. Similar evidence was reported from other studies [33, 36, 37].
5. Conclusion
The study showed that households owned latrine at the community level were low. However, the majority of constructed latrines were utilized by household members. Adults and children were more adhered to utilize latrine. The desired level of latrine ownership and utilization would be realized if and only if all sanitation and hygiene components in the country's health extension package were kept on eye side by side in line with identified predictor factors.
Acknowledgments
A government research grant was provided to Tigray Health Research Institute with a grant number THRI-341/02/6223. This grant was allocated for WASH program evaluation. The funders had no role in study design, data collection, analysis, interpretation, and decision to publish, or preparation of the manuscript. Our great appreciation goes to Tigray Health Research Institute for financial and technical support. The authors also thank the Tigray Regional Health Bureau, health facilities managers, household members, supervisors, and data collectors for their supportive approach during the entire period of the study.
Abbreviations
- EDHS:
Ethiopian demographic health survey
- AOR:
Adjusted odds ratio
- COR:
Crude odds ratio
- IEC:
Information, education, and communication.
Data Availability
The data are available upon reasonable request from the corresponding author.
Ethical Approval
The study protocol was reviewed and approved by the Institutional Review Board of Tigray Health Research Institute (institusionsl.review.board.thri@gmail.com) with a reference and approval no. THRI-IRB 0040/2018. Permission was also received from the Tigray Regional Health Bureau.
Consent
Data collection was conducted only after oral informed consent was given.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
KF, AbA, AsA, AG, and NM conceived and designed the study; KF, AbA, AsA, AG, NM, and AG oversaw data collection: KF analyzed and interpreted data; KF drafted the manuscript. All authors critically reviewed and approved the manuscript.
References
- 1.World Health Organization. Sanitation. 2015. http://www.who.int/mediacentre/factsheets/fs392/en/ [Google Scholar]
- 2.Prüss A., Kay D., Fewtrell L., Bartram J. Estimating the burden of disease from water, sanitation, and hygiene at a global level. Environmental Health Perspectives. 2002;110(5):537–542. doi: 10.1289/ehp.110-1240845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.UNICEF. Water, sanitation and hygiene, annual results report 2016. 2016. https://www.unicef.org/publicpartnerships/files/2016arr_wash.pdf.
- 4.WHO. Progress on Drinking Water, Sanitation and Hygiene: 2017 Update and SDG Baselines. Geneva, Switzerland: UNICEF; 2017. [Google Scholar]
- 5.Galan D. I., Kim S.-S., Graham J. P. Exploring changes in open defecation prevalence in sub-Saharan Africa based on national level indices. BMC Public Health. 2013;13(1):p. 527. doi: 10.1186/1471-2458-13-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mara D., Lane J., Scott B., Trouba D. Sanitation and health. PLoS Medicine. 2010;7(11) doi: 10.1371/journal.pmed.1000363.e1000363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Central Statistical Agency. 2016 Ethiopia Demographic and Health Survey. Addis Ababa, Ethiopia: CSA and ICF; 2017. [Google Scholar]
- 8.Leshargie C. T., Alebel A., Negesse A., et al. Household latrine utilization and its association with educational status of household heads in Ethiopia: a systematic review and meta-analysis. BMC Public Health. 2018;18(1):p. 901. doi: 10.1186/s12889-018-5798-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gebremedhin G., Tetemke D., Gebremedhin M., et al. Factors associated with latrine utilization among model and non-model families in Laelai Maichew Woreda, Aksum, Tigray, Ethiopia: comparative community based study. BMC Research Notes. 2018;11(1):p. 586. doi: 10.1186/s13104-018-3683-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Belachew A. B., Abrha M. B., Gebrezgi Z. A., Tekle D. Y. Availability and utilization of sanitation facilities in Enderta district, Tigray, Ethiopia. Journal of Preventive Medicine and Hygiene. 2018;59(3):E219–E225. doi: 10.15167/2421-4248/jpmh2018.59.3.826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gebremedhin H., Abay T., Gebregzabher T., Yemane D., Gebreegziabiher G., Shewaye B. Latrine utilization and associated factors in south east zone of Tigray region, north Ethiopia. European Journal of Biomedical and Pharmaceutical Sciences. 2016;3(6) [Google Scholar]
- 12.Tafere Y., Woldie M., Assefa H. Investigations of latrine coverage and associated factors among Debretabor town, Amhara region north west Ethiopia. International Journal of Public Health Science (IJPHS) 2016;5(2):137–141. doi: 10.11591/.v5i2.4777. [DOI] [Google Scholar]
- 13.WHO. Geneva, Switzerland: WHO and UNICEF; 2015. Progress on sanitation and drinking water—2015 update and MDG assessment. [Google Scholar]
- 14.Clasen T. F., Bostoen K., Schmidt W. P., et al. Interventions to improve disposal of human excreta for preventing diarrhoea. Cochrane Database of Systematic Reviews. 2010;2010(6) doi: 10.1002/14651858.cd007180.pub2.CD007180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.WHO. Geneva, Switzerland: WHO; 2012. Global costs and benefits of drinking-water supply and sanitation interventions to reach the MDG target and universal coverage. [Google Scholar]
- 16.Asfaw G., Molla E., Vata P. K. Assessing privy (Latrine’s) utilization and associated factors among households in Dilla town, Ethiopia. International Journal of Health Sciences and Research. 2015;5(6):537–544. [Google Scholar]
- 17.Budhathoki S. S., Shrestha G., Bhattachan M., Singh S. B., Jha N., Pokharel P. K. Latrine coverage and its utilisation in a rural village of eastern Nepal: a community-based cross-sectional study. BMC Research Notes. 2017;10(1):p. 209. doi: 10.1186/s13104-017-2539-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Debesay N., Ingale L., Gebresilassie A., Assefa H., Yemane D. Latrine utilization and associated factors in the rural communities of Gulomekada district, Tigray region, north Ethiopia, 2013: a community based cross-sectional study. Journal of Community Medicine & Health Education. 2015;5(2):p. 338. doi: 10.4172/2161-0711.1000338. [DOI] [Google Scholar]
- 19.Gedefaw M., Amsalu Y., Tarekegn M., Awoke W. Opportunities, and challenges of latrine utilization among rural communities of Awabel district, northwest Ethiopia, 2014. Open Journal of Epidemiology. 2015;5(2):98–106. doi: 10.4236/ojepi.2015.52013. [DOI] [Google Scholar]
- 20.Koyra H. C., Sorato M. M., Unasho Y. S., Kanche Z. Z. Latrine utilization and associated factors in rural community of Chencha district, southern Ethiopia: a community based cross-sectional study. American Journal of Public Health Research. 2017;5(4):98–104. doi: 10.12691/ajphr-5-4-2. [DOI] [Google Scholar]
- 21.Yimam Y. T., Gelaye K. A., Chercos D. H. Latrine utilization and associated factors among people living in rural areas of Denbia district, northwest Ethiopia, 2013, a cross-sectional study. Pan African Medical Journal. 2014;18:p. 334. doi: 10.11604/pamj.2014.18.334.4206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Obeng P. A., Keraita B., Oduro-Kwarteng S., Bregnhøj H., Abaidoo R. C., Konradsen F. The latrine ownership ladder. Management of Environmental Quality: An International Journal. 2015;26(5):752–763. doi: 10.1108/meq-05-2014-0079. [DOI] [Google Scholar]
- 23.The Government of Tigray National Regional State. 2008 EFY Annual Profile. Ethiopia: Tigray National Regional State; 2008. [Google Scholar]
- 24.Awoke W., Muche S. A cross sectional study: latrine coverage and associated factors among rural communities in the district of Bahir Dar Zuria, Ethiopia. BMC Public Health. 2013;13(1):p. 99. doi: 10.1186/1471-2458-13-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ashebir Y., Rai Sharma H., Alemu K., Kebede G. Latrine use among rural households in northern Ethiopia: a case study in Hawzien district, Tigray. International Journal of Environmental Studies. 2013;70(4):629–636. doi: 10.1080/00207233.2013.835533. [DOI] [Google Scholar]
- 26.Zeleke D. A., Gelaye K. A., Mekonnen F. A. Community-led total sanitation and the rate of latrine ownership. BMC Research Notes. 2019;12(1):p. 14. doi: 10.1186/s13104-019-4066-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oljira D., Berkessa T. S. Latrine use and determinant factors in southwest Ethiopia. Journal of Epidemiology and Public Health Reviews. 2017;1(6) doi: 10.16966/2471-8211.133. [DOI] [Google Scholar]
- 28.Debesay N., Ingale L., Gebresilassie A., Assefa H., Latrine Yemane D. Utilization and associated factors in the rural communities of Gulomekada district, Tigray region, North Ethiopia: a community based crosssectional study. Community Medicine & Health Education. 2013;5(2):p. 8. doi: 10.4172/21610711.100033. [DOI] [Google Scholar]
- 29.Nepal WASH Alliance. Open defecation free (ODF) status updates in Nepal. Water, sanitation and hygiene resource centre network Nepal. 2016. http://www.wash-rcnn.net.np/nwa/odf-updates.html.
- 30.Sinha A., Nagel C. L., Schmidt W. P., et al. Assessing patterns and determinants of latrine use in rural settings: a longitudinal study in Odisha, India. International Journal of Hygiene and Environmental Health. 2017;220(5):906–915. doi: 10.1016/j.ijheh.2017.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alemu F., Kumie A., Medhin G., Gebre T., Godfrey P. A socio-ecological analysis of barriers to the adoption, sustainability and consistent use of sanitation facilities in rural Ethiopia. BMC Public Health. 2017;17(1):p. 706. doi: 10.1186/s12889-017-4717-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oswald W. E., Teferi T., Emerson P. M., et al. Prediction of low community sanitation coverage using environmental and sociodemographic factors in Amhara region, Ethiopia. The American Journal of Tropical Medicine and Hygiene. 2016;95(3):709–719. doi: 10.4269/ajtmh.15-0895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tulu L., Abera K., Hawas S. B., Demissie H. F., Segni M. T. Latrine utilization and associated factors among Kebeles implementing and non-implementing urban community led total sanitation and hygiene in Hawassa town, Ethiopia. African Journal of Environmental Science and Technology. 2017;11(3) doi: 10.5897/ajest2016.2223. [DOI] [Google Scholar]
- 34.Dadi A. F., Ashenafi T., Gizaw Z. Latrine utilization and associated factors among Kebeles declared open defecation free in Wondo Genet district, South Ethiopia 2015. ISABB Journal of Health and Environmental Sciences. 2018;5(5):43–51. doi: 10.5897/ISAAB-JHE2018.0050. [DOI] [Google Scholar]
- 35.Gudda F. O., Moturi W. N., Oduor O. S., Muchiri E. W., Ensink J. Pit latrine fill-up rates: variation determinants and public health implications in informal settlements, Nakuru-Kenya. BMC Public Health. 2019;19(1):p. 68. doi: 10.1186/s12889-019-6403-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beyen D. T., Tucho A. E., Moga T. T. Effect of latrine utilization on diarrhea diseases in Abukako Kebele, Jimma, South west, Ethiopia. Journal of Research in Environmental Science and Toxicology. 2019;8(1):9–15. doi: 10.14303/jrest.2019.024. [DOI] [Google Scholar]
- 37.Anteneh A., Kumie A. Assessment of the impact of latrine utilization on diarrhoeal diseases in the rural community of Hulet Ejju Enessie Woreda, east Gojjam zone, Amhara region. Ethiopian Journal of Health Development. 2010;24(2):111–113. doi: 10.4314/ejhd.v24i2.62959. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are available upon reasonable request from the corresponding author.


