Abstract
Delayed sequelae from mild traumatic brain injury (Glasgow Coma Score at admission >13, TBI) has been documented in case reports however larger studies of these effects are sparse. We undertook a telephone based survey to assess the long term sequelae of TBI. We tracked 100 pediatric TBI patients via our trauma registry for demographic data including age, injury severity, and mechanism of injury. Then we proceeded to contact these patient’s parents via telephone. We asked regarding residual symptoms and signs of concussive injury.
Duration out from initial concussive injury ranged from 4 to 68 months. The parents of 66 boys and 34 girls were surveyed. The age of the patients at the time of mild TBI ranged from 1 to 14 years. The injury severity score ranged from 1 to 21. One being the most common Injury severity score. Thirty-three percent of patients had residual effects of concussion at the time of telephone survey. Fourteen percent had memory loss issues, 21% had anxiety/depression issues, 20% had learning disability issues, and 15% had sleep disturbance issues. Duration of time post concussive injury, mechanism, and age did not influence incidence of sequelae. Mild traumatic brain injury has significant long term sequelae. Better identifying characteristics are needed to characterize patients susceptible to long term residual effects of concussion.
Keywords: Traumatic brain injury, pediatrics, residual sequealae, telephone survey
Introduction
Traumatic brain injury (TBI) is the leading cause of morbidity and mortality in children and adolescents in the US. Even mild TBIs in children are a serious problem, threatening pediatric health and exacerbating the social and economic burden.1-4 Sports related TBI in children has garnered significant attention recently but data regarding non-sports related TBI is sparse. Identification of delayed sequelae will shed light on the area of treatment options related to seemingly mild TBI. We have previously examined the epidemiology of self-reported neurologic and neuro-psychiatric symptoms in pediatric patients with mild TBI within 14 months’ post-injury. We found that headaches (39.4%), anxiety (30.3%), fear (18.2%), and anhedonia (18.2%) were the most frequently reported symptoms.2 A literature review conducted at the School of Nursing at the University of Pennsylvania has concluded that upon pediatric head injuries, providers should ensure that patients undergo psychological screening and early intervention.5 They declare that their review implies that new onset disorders of mood, personality, anxiety, or stress related disorders can emerge as an immediate consequence or even develop several years later.5 This paper however did not specify the initial degree of injury as mild, moderate, or severe. We were interested in looking at longer periods of time post injury after mild TBI in children (age <15 years) to see if the sequelae persisted for longer periods of time. We found in our search of the literature that data on patients that had seemingly innocuous TBI (mild TBI) is lacking. Our hypothesis was that significant sequelae are present in our pediatric patients that suffer, non-sports related, seemingly mild TBI.
Materials and Methods
We queried out trauma registry at our ACS verified urban pediatric level 2 trauma center for all patients under the age of 15 who came to our emergency department between 2015 and 2019 with a head injury and were subsequently diagnosed with mild Traumatic Brain Injury (TBI) and admitted. Electronic medical records were reviewed to obtain demographic data which included age, gender, Injury Severity Score (ISS), Abbreviated Injury Score for the head region (AIS-H), hospital length of stay, intensive care unit length of stay, mechanism of injury, revised trauma score (RTS), admission Glasgow coma score, admission vital signs, and any pre-existing conditions as well as other injuries present at the initial presentation. Contact phone number was also obtained for both the minor patient and legal guardian. A telephone questionnaire was then developed based on previous published investigations, and our own previous experience (Figure 1). The legal guardian for each patient or the patient was contacted by 1 researcher (B.K.) to complete the surveys. The guardian or patient was explained in detail that the trauma section from our institution was doing a follow up survey on the injury which was suffered as noted in our records. Their participation was purely voluntary, and this was part of a performance improvement project to better understand self-reported long-term effects of concussive injury. We separated the patients by number of months’ post injury, age at the time of injury, and mechanism of injury to better appreciate the complications post injury. After completion of the surveys, we de-identified the data and performed a one-way analysis of variance (ANOVA) of complications with age at admission broken down into 3 groups (A = age 0-5, B = age 6-10, C = age 11-14), time from injury to survey broken down into 7 groups by number of months post injury (A = 0-10 months, B = 11-20 months, C = 21-30 months, D = 31-40 months, E = 41-50 months, F = 51-60 months, G = 61-70 months), and mechanism of injury broken down into 3 groups (falls, pedestrian stuck, and other mechanisms) using a commercially available statistical analysis software package (JMP).
Figure 1.
Telephone survey questionnaire.
Results
We reviewed 168 charts of patients that were admitted and diagnosed in our trauma registry as Mild TBI. While we attempted to reach all the patients, we were able complete 100 surveys of 34 girls and 66 boys with mild TBI. The age at the time of admission ranged between 1 and 14 years. The injury severity score (ISS) ranged between 1 and 21. The duration of time from initial injury to survey ranged from 4 to 68 months. As for mechanisms of injury, we had 69 patients suffer from falls, 18 patients that were pedestrian stuck and 13 had other mechanisms (Motor Vehicle Crashes, bicyclist struck, assault, object struck) (Figure 2). Overall, we noted the following complicating sequelae in our patients: 33% had some residual effect related to TBI. Of the 33%, 21% of patients had anxiety/depression issues, 20% had learning disability issues, 15% had sleep disturbance issues, and 14% had memory loss issues (Figure 3). Various sequelae at much lower frequency persisted in our children after mild TBI, including deficit in hearing, alteration in gait, presence of nausea or vomiting, migraines, and persistent fatigue. There were no gender related differences in outcome.
Figure 2.
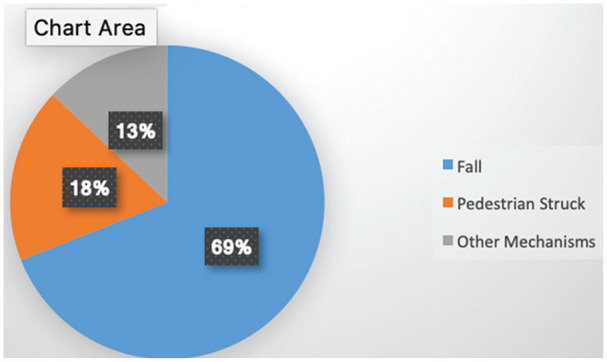
Mechanisms of injury.
Figure 3.
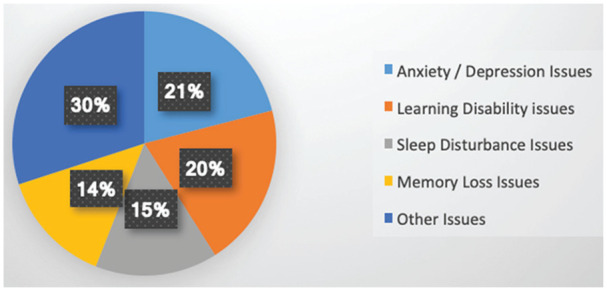
Predominant residual effects related to mild TBI %.
A comparison of the groups by time out from injury to the persistence of sequelae, did not show any difference between the 7 groups (Table 1). A comparison of groups by age at the time of injury in relation to persistent sequelae failed to show statistical difference between the 3 groups (Table 2). There was no association between mechanism of injury and persistent sequelae of TBI noted. As the vast majority of patients had normal GCS and very low ISS there was no association between acute injury scores (RTS, AIS-H, ISS) and persistent sequelae of TBI. Persistence of sequelae does not seem to be associated with pharmaceutical use, physical therapy, or duration of bed rest post-trauma as our patients noted different approaches post TBI.
Table 1.
Duration of Time From Injury to Survey Association With Persistent Sequelae of TBI, All Groups Were Compared to All Other Groups, Univariate Analysis.
| Group | Months from injury | Number of patients | % of patients with persisting sequelae mean ± SEM |
P value |
|---|---|---|---|---|
| A | 0-10 | 15 | 40 ± 12 | n.s. |
| B | 11-20 | 15 | 26 ± 12 | n.s. |
| C | 21-30 | 14 | 43 ± 12 | n.s. |
| D | 31-40 | 17 | 22 ± 11 | n.s. |
| E | 41-50 | 17 | 35 ± 11 | n.s. |
| F | 51-60 | 14 | 45 ± 14 | n.s. |
| G | 61-70 | 8 | 38 ± 17 | n.s. |
Abbreviations: SEM, standard error of the mean; n.s., not significant.
Table 2.
Age at the Time of Injury Association With Persistent Sequelae of TBI.
| Group | Age (years) | Number of patients | % of patients with persisting sequelae mean ± SEM |
P value |
|---|---|---|---|---|
| 1 | 0-5 | 52 | 33 ± 6 | n.s. |
| 2 | 6-10 | 27 | 30 ± 9 | n.s. |
| 3 | 11-14 | 21 | 38 ± 10 | n.s. |
Abbreviations: SEM, standard error of the mean; n.s., not significant.
Discussion
Almost half a million children 1 to 14 years old suffer from TBI each year in The United States. While these occur from various mechanisms, the most frequent causes are falls, being struck by a motor vehicle, or abusive injuries.6 Mild TBI is often accompaniedby long term behavioral and neuropsychological defects.2,7 Mild TBI usually occurs with head trauma due to contact and/or acceleration or deceleration forces. The type of mechanical forces may determine the nature of the resultant injury.8 What effect this injury has on the developing brain is unclear.9 Despite the fact that mild TBI seems to be associated with significant morbidity, there is very little data in the literature on long term sequelae related to mild traumatic injury unrelated to sports injuries. An interesting study by Manley et al10 reviewed potential long-term effects of sports related concussion looking at sequelae 10 years after injury. However, this was inclusive of professional athletes as well as high school athletes. It was also not specific regarding exact type of concussive injury. It did find that some former athletes in contact, collision, and combat sports suffer from depression and cognitive deficits later in life, and there is an association between these deficits and a history of multiple concussions. This would suggest that children with mild TBI would be at such risk with repetitive injury. The exact relationship with the repetitive injury and progression to chronic traumatic encephalopathy is unclear. Our review of the current literature did not show any article regarding children that was similar to this paper.
Our current study focused on TBI occurring from non-sports related injuries, and long-term sequelae related to TBI. In this study we extended our data to a period of time much further than our previous study which went only to 14 months’ post injury. Weaknesses of our study are that we are unable to verify pre-existing mental conditions even though we asked about pre-existing issues, and as our survey was self-reported, we are unable to formally attach a diagnosis to our patients. With regard to pre-existing neurologic issues prior to the mild TBI, we were unable to find any such issues in our patient population. We found once again that persistent sequelae are present after seemingly innocuous TBI. Unlike our previous study which showed persistence of headaches, this study shows a persistence of anxiety and depression which once again suggest post-traumatic stress disorder (PTSD). As suggested in our previous paper, learning disabilities and memory loss are very problematic to patients and families. Since the persistence of neuropsychiatric issues beyond 5 years is significant in our population, perhaps routine neuro-psychiatric testing of all patients with mild TBI should be considered. Because we identified many patients with long term sequelae, we were able to guide them to our neurology colleagues to follow up and address these issues. Unfortunately, due to the retrospective and self-reported nature of our study no association between initial data and persistent sequelae was found. Further studies looking at non-sports related mild TBI are needed with specific data looking into objective data on neuro-psychological issues. Mild TBI clearly has a profound long-term impact on the developing brain. We also understand that comparing issues such as anxiety in a child aged 4 may not be comparable to a child of age 14. We made the assumption that, as the survey was being answered by the parent or guardian, we could make a general comparison. We also did a statistical analysis between each of the age groups (age 1-14) and because our numbers were small, we found no difference, hence we decided to combine age groups so as to look for any difference, which was also not present. The earlier identification and more detailed analysis of patients at risk may yield better outcomes in child with mild TBI. We conclude that significant sequelae are present in our pediatric patients that suffer, non-sports related, seemingly mild TBI.
Footnotes
Author Contributions: All authors participated in the planning, and authorship of the article. Author BK was also involved in the actual performance of the survey and tabulation of the data. AC was involved in all phases of the project.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Akella Chendrasekhar  https://orcid.org/0000-0001-9678-2067
https://orcid.org/0000-0001-9678-2067
Ethics Approval and Informed Consent: The institutional review board at SUNY Downstate Medical center waived the need for ethics approval and the need to obtain consent for the collection, analysis and publication of the retrospectively obtained and anonymized data for this non-interventional study.
References
- 1. Luerssen TG, Kauber MR, Marshall LF. Outcome from head injury related to patient’s age. A longitudinalprospective study of adult and pediatric head injury. J Neurosurg. 1988;68:409-416. [DOI] [PubMed] [Google Scholar]
- 2. Chendrasekhar A. Persistent symptoms in mild pediatric traumatic brain injury. Pediatric Health Med Ther. 2019;10:57-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mckinlay A, Dalrymple-Alford JC, Horwood LJ, et al. Long-term psychosocial outcomes after mild head injury in early childhood. J Neurol Neurosurg Psychiatry. 2002;73:281-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Schultzman SA, Greenes DS. Pediatric minor head trauma. Ann Emerg Med. 2001;37:65-74. [DOI] [PubMed] [Google Scholar]
- 5. Li L, Liu J. The effect of pediatric traumatic brain injury on behavioral outcomes: a systematic review. Dev Med Child Neurol. 2013;55:37-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Araki T, Yokota H, Morita A. Pediatric traumatic brain injury: characteristic features, diagnosis, and management. Neurol Med Chir (Tokyo). 2017;57:82-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lee JB, Affeldt BM, Gamboa Y, et al. Repeated pediatric concussions evoke long term oligodendrocyte and white matter microstructural dysregulation distant from the injury. Dev Neurosci 2018;40:358-375. [DOI] [PubMed] [Google Scholar]
- 8. Duhalme AC, Christian CW, Rorke LB, et al. Non-accidental injury in infants - the “shaken baby syndrome”. N Engl J Med. 1998;338:1822-1829. [DOI] [PubMed] [Google Scholar]
- 9. Medana IM, Esiri MM; Axonal damage: a key predictor of outcome in human CNS diseases. Brain. 2003;126:515-530. [DOI] [PubMed] [Google Scholar]
- 10. Manley G, Gardner AJ, Schneider KJ, et al. A systematic review of potential long-term effects of sport-related concussion. Br J Sports Med. 2017;51:969-977. [DOI] [PMC free article] [PubMed] [Google Scholar]



