Abstract
In this review of 100 years of the Yale System of Medical Education, a portrait emerges of what it is and what it has made possible. Founded in the 1920s under the leadership of Dean Milton C. Winternitz, the Yale System abandoned most educational mainstays including: grades, class rankings, roll call, daily assignments, course exams, and class year affiliations. Instead, a thesis and two broad qualifying examinations were required. Revised over decades, the essential elements endure. The Yale System has cultivated generations of humane physicians, academics, and leaders through the rise of modern medicine, and medicine’s constantly evolving knowledge base.
Keywords: Yale System, Yale School of Medicine, Education, Medical Education, Milton C. Winternitz, Flexner Report
Introduction
In a history of the Yale System of Medical Education published in 1986, historian Arthur J. Viseltear wrote that some argued “that there is no System, that it is a figment of the imagination.” Even the Yale School of Medicine Bulletin, he noted, made no mention of the Yale System [1(p627)].
Indeed, for a century, medical education at Yale has been characterized by its lack of emphasis on usual requirements. Since the 1920s, the Yale School of Medicine has either refused or de-emphasized nearly all educational mainstays, particularly: grades, class rankings, quizzes, course examinations, reading requirements, and even class attendance requirements.
Could this really be called a system?
Today in 2020, the Yale School of Medicine Bulletin is now primarily a digital publication [2]. The online Bulletin, and the Yale School of Medicine website both state, “The Yale System of Medical Education remains unique among medical schools [3].”
By now it is agreed that the Yale System exists. Beyond this, consensus falls short.
Disagreement for the past 100 years centers upon whether course exams and class attendance should be required, and to what extent. At the same time, many gasp at the scant requirements of the Yale School of Medicine in an era when vigorous standardized testing begins in the first grade.
Discussion of the Yale System focuses on what it isn’t and what it lacks. There is relatively little discussion about what the Yale System is, or what students are expected to do. Therefore, when complaints arise, remedies tend to center upon more exams and more requirements, thereby engendering more complaints.
Yet the founding principle of the Yale System is often forgotten—that medical education at Yale should be like graduate school, rather than trade school.
As might be imagined, there is little research as to when the Yale System began. An urgency of reviewing the Yale System lies in the question of its centennial. If the Yale System is worthy of a centennial acknowledgment, when should it occur?
Is the Yale System’s hundredth year actually, upon us now?
Background
The Yale School of Medicine’s close relationship with Yale University lends consideration to the term, “Yale System.”
Yale embraced the humanitarian mission of medicine from its earliest days. Founded in 1701, the school graduated its first clerical physician, Phineas Fiske, in 1704, the same year Isaac Newton published Opticks. In 1723, Yale College conferred North America’s first MD degree to Daniel Turner, a London-educated physician. In the 18th century, the majority of the distinguished medical practitioners in Connecticut were clergymen who had graduated from Yale College [4(pp23-24)].
After more than a century of educating physicians, the Medical Institution of Yale College was chartered in 1810. According to Gerard Burrows, 14th Dean of the Yale School of Medicine, the school’s close association with Yale University has informed its character from the beginning.
This history suggests that an essential element of the Yale System is medical students engaging in the larger resources of Yale University, and flexibility of the medical school curriculum to encourage this.
The Flexner Report and the “Yale Plan”
The origins of the Yale Plan, as it was first called, can be traced to reform movements in the early 1900s that would shape the future of medical practice and medical education. In the early 1900s, medical practice still primarily derived from the ancient Greek philosophy that sickness was caused by an imbalance of bodily humors, such as black bile versus yellow bile. Non-scientific methods such as bloodletting by leeches and lancets were standard practices, hence the name of the medical journal, The Lancet.
Many US medical schools were profit-making storefronts run by sole proprietors. Admission was largely dependent upon the ability to pay, and medical degrees were often granted after a few months of instruction, and no experience with patients.
The rise of scientific medicine and medical education in the US was led by the American Medical Association (AMA). In the early 1900s, tonic manufacturers, snake oil salesmen, and medicine men “quacking” their cures pervaded the American landscape. In response, the AMA founded a Council on Pharmacy and Chemistry in 1905 to test “medicines.” In 1906, the federal government followed suit and founded the Food and Drug Administration (FDA) which regulates medicines to this day. The terms, “snake oil” and “quack,” remain in our language, as a cultural memory of this early era of health care reform [5].
The AMA’s Council on Medical Education was founded in 1904. At the council’s urging, the Carnegie Foundation recruited Abraham Flexner to study medical schools.
The Flexner Report is now regarded as the beginnings of modern medical education and modern medicine in North America. Flexner recommended closure of all but 31 of the 155 medical schools in the US and Canada, especially schools run by sole proprietors, and schools centered on electrotherapy, homeopathy, and non-science based methods. Half of US medical schools soon closed.
Flexner believed that medical schools should be based within a university. In New England, Flexner designated only two medical schools as worthy of staying open— Harvard Medical School, and the Medical Institution of Yale College. Flexner’s critique of medical education circa 1910 was prescient of the Yale System:
“From morning to night their time is taken up with classes; they rush out of one lecture hall into another, hearing a huge mass of facts and theories put forward. One can readily imagine the condition inside their heads by the time night comes. The actual outcome of this absurd overcrowding is that only a small amount of what is heard is retained [6(pp76-77)].”
In the next decades, Flexner himself was involved with shaping the Yale School of Medicine and the Yale System.
Dean Milton C. Winternitz
The Yale System originated during Milton C. Winternitz’s term as Dean of the School of Medicine between 1920-1935. Winternitz was a new kind of physician who had earned his college degree and medical degree from Johns Hopkins University (Baltimore, MD), at a time when a college education was not a prerequisite to be a physician. For example, his predecessor at Yale, Dean George Blumer, had never attended college, and was part-time faculty with a private practice, like most medical school faculty at the time.
At Johns Hopkins, Winternitz had been mentored by William Welch, Yale Class of 1870. Welch was a founder of the Johns Hopkins School of Medicine and was sometimes called the Dean of American Medicine. Thanks to Welch’s recommendation, Winternitz was offered the position of Chief of the Pathology Department at the Yale School of Medicine, at a salary of $4,000. He accepted [7(p23)].
When the Winternitz family arrived at Yale in 1917, science and the industrial revolution had already changed the everyday lives of Americans. The railroad allowed travel from Winternitz’ hometown of Baltimore, to New Haven. He would soon drive a Ford Model T, the first affordable, manufactured automobile. His father-in-law, Thomas Watson, had invented the telephone with Alexander Graham Bell. New Haven was a prosperous manufacturing town, the home of Winchester Rifles and Shotguns, Sargent Tools, and hundreds of companies [8(p4)].
Yet science and manufacturing had yet to impact medical treatment in a significant way.
For Yale University’s bicentennial celebration in 1901, Welch was invited to give a keynote speech about the relation of Yale to medicine. Writing to his sister, he complained,
“the subject ‘Relation of Yale to Medicine’ is about the most barren theme I ever tackled. The relation is so slight that I shall have to beat around the bush and talk on side issues. If they had only asked me to talk on the relation of Yale to Calvinism or football there would be something to say [9(p74)].”
The situation was worse when Winternitz became Dean of the Yale School of Medicine in 1920. Only seven faculty members had not resigned. Only 68 potential students applied for admission. Even Winternitz questioned whether the School of Medicine “should close its doors [10(p6)].”
That same year, 1920, Winternitz published The Pathology of Influenza, on the heels of the Spanish Flu Pandemic of 1918 [10,11]. The 144-page book concluded that the pathogenic bacteria remained unknown. Not until 1931 would the responsible pathogen be found. It would prove to be not a bacteria, but a virus. In the 1950s, the same industrial methods that built the Model T would be used to manufacture flu vaccines to prevent influenza on a global scale.
But 1920 was still the pre-dawn of modern medicine. (Figure 1).
Figure 1.
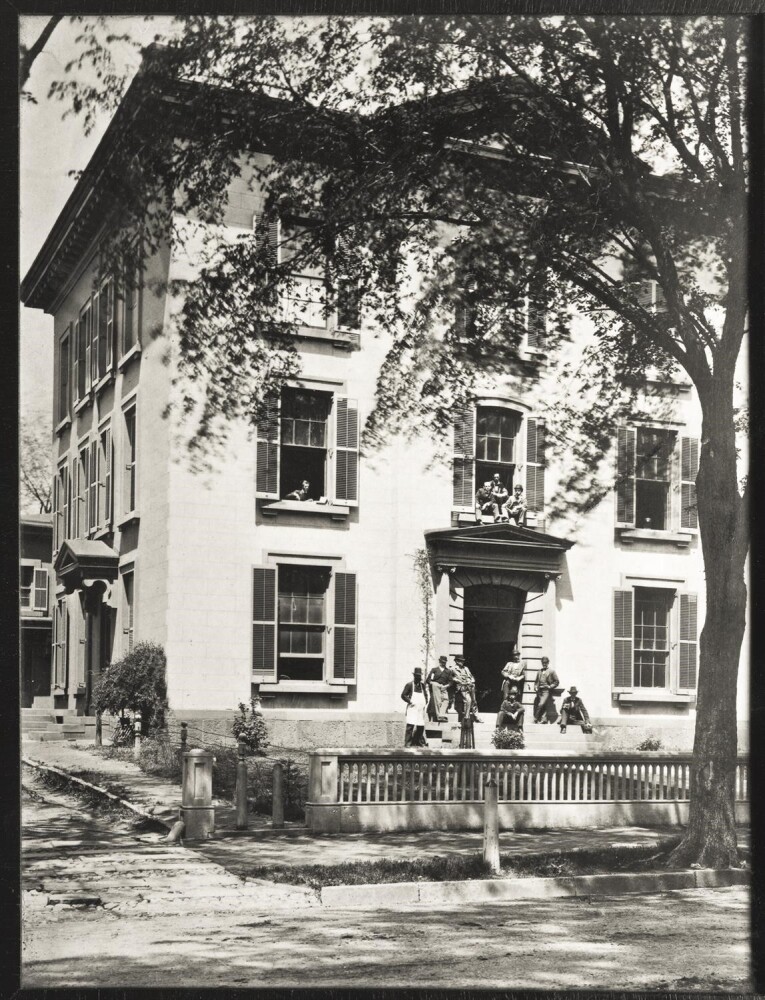
A converted house at 150 York Street was the entire Yale School of Medicine from 1860 to 1907. By 1920, two more converted houses on Cedar Street were recruited. The three houses, army barracks, and the Brady Laboratory comprised the Yale School of Medicine circa 1920. (Medical Historical Library, Harvey Cushing/John Hay Whitney Medical Library, Yale University).
“A Great Machine for Teaching”
Winternitz made no secret of his disdain for lectures and passive learning. His strategy for the Yale School of Medicine was to build “a great machine for teaching” so that students could immerse themselves for self-directed learning.
“Universities should be interested primarily in providing opportunity for learning and not in giving instruction. Teaching need enter only in so far as there is failure to learn [12(p149)].”
“Every effort must be made not to stifle the opportunities for learning by building up a great machine for teaching [12(p150)].”
Winternitz wished for departments to remain open during vacations, believing that when freed from requirements, students could learn in a more intimate manner from professors. In today’s terms, one could say that Winternitz did not believe in micro-managing.
“The student may go fishing, or play golf, or he may go to some other school to learn pathology. He will be tested eventually not on what I think I should have taught him but on his knowledge of pathology, or rather on what the examiners believe he should know of pathology… [13(p211)].”
Toward building his great machine for teaching, Winternitz wasted no time, accomplishing so much that Yale President James R. Angell called Winternitz “a steam engine in pants [4(p30)].”
Medical school faculty became Yale University faculty, thus elevating the quality of faculty, while strengthening ties with Yale University. Departments were reorganized into their modern form. Previously, physiology was taught in four different departments, in the medical school and university. A department of pediatrics was created.
By the fall of 1921, a landmark was achieved. All faculty in the major departments became full-time and salaried. The Flexner Report had recommended that medical schools employ full-time, salaried faculty, a controversial idea that Harvard Medical School outright rejected. Johns Hopkins instituted the full-time system in 1914. But in the process, they lost William Osler, the Father of American Medicine, who departed Johns Hopkins for Oxford University in 1905 to avoid the impending change [9(p31)].
In 1920, the Yale School of Medicine had no campus. Anatomy lab and most classes were held in a converted house at 150 York Street. Two other former houses on Cedar Street, army barracks, and the Brady Laboratory comprised the entire medical school.
Yale’s lack of a teaching hospital was a primary reason Harvey Cushing, Yale Class of 1891, made his career at Harvard. Only in retirement, did the Father of Neurosurgery return to Yale for a fruitful post-retirement career. Although the New Haven Hospital was near the School of Medicine, Cushing critiqued it as not under the control of the school, and not recognizing students as essential to its operation.
The New Haven Hospital began as a hotel (the words hotel and hospital share common roots). Refurbished in 1833 and named State Hospital, it continued to rent rooms to boarders. It was later re-named Knight Hospital, after Jonathan Knight, a founding member of the Medical Institution of Yale College and the American Medical Association. In 1844, it became New Haven Hospital.
Winternitz merged New Haven Hospital, and the New Haven Dispensary, which was renamed, “The Clinic for Ambulatory Patients.” He arranged for both to be full teaching facilities.
Winternitz’s tireless fundraising efforts made much of this possible. Abraham Flexner, after leaving the Carnegie Foundation, became a member of the Rockefeller Foundation’s General Education Board. According to Flexner:
“Between 1919 and 1921, Mr. Rockefeller, Senior, presented the General Education Board with almost $50,000,000 to be spent, principal and interest, for the improvement of medical education in the United States. Winternitz was among the first and most persistent of those who sat at my doorstep [14(p575)].”
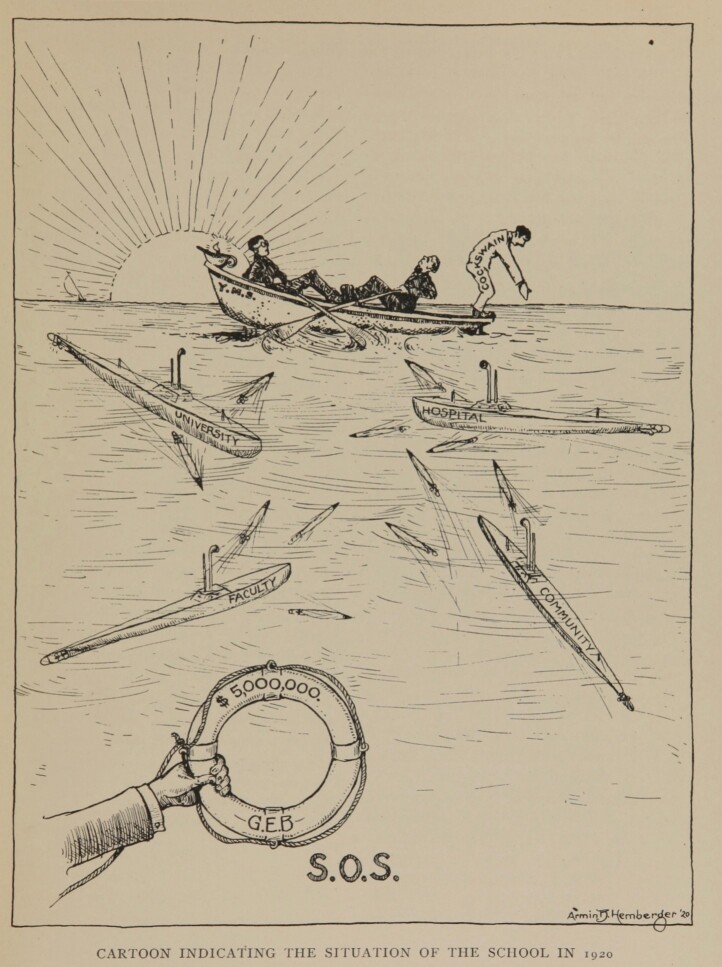
In 1920, Winternitz sent a plea to the Rockefeller Foundation General Education Board in the form of a cartoon depicting the Yale Medical School’s precarious situation, as if a rowboat at sea, dodging torpedoes. A lifesaver of $5,000,000 from the GEB was their SOS. Flexner granted Winternitz his request, along with many more requests to come (Figure 2).
Figure 2.
A request for funding, in cartoon form, was sent by Dean Milton Winternitz to the Rockefeller General Education Board in 1920. The $5 million was granted. (Photo from Winternitz MC. Past, Present, Future of the Yale University School of Medicine and Allied Institutions. New Haven, Yale University, 1922. Pg 7.)
Progress came quickly.
The December 30, 1921 issue of the Yale Alumni Weekly hailed a “Reconstructed Medical School:”
“the University’s oldest professional School, founded in 1810, is attaining a position of such prominence among American medical schools and among professional schools everywhere [15(p364)].”
One could hardly imagine today, a Yale publication likening medicine to what is most commonly called the oldest profession. But such was the state of the Yale School of Medicine, and of American medicine at the time.
A lead article was descriptively titled, “The Yale School of Medicine: A New Building to be erected from the Sterling Funds—Closer Relationship with the Hospital and Dispensary, Departmentalization, Full Time Basis, and the Organization of a New Department indicate the School’s Recent Progress.”
Whereas the school had only 68 applicants for the class entering in 1920, within two years, there were 450 candidates for 56 first-year medical school positions.
Recognizing this progress, the Yale Corporation acquired a city block to create a central campus for the medical school, and committed funds for a new medical school building.
The new building was to be called the Sterling Hall of Medicine, with a soaring brick entrance on Broad Street. Funds of $1.32 million were allocated from the Sterling bequest, donated by attorney John W. Sterling, Yale Class of 1864, upon his passing in 1918. Sterling’s bequest of $15 million to Yale was partly administrated by his partner of 40 years, James O. Bloss [15].
According to the article, Yale’s commitment of the Sterling funds signified the medical school’s importance “in the University, the medical profession, and the world.”
When Did the Yale System Begin?
According to Howard Spiro and Priscilla Waters Norton, in their biography of Milton C. Winternitz, “The Yale Plan had its beginnings in Winter’s first year as dean [7(p103)].” Winternitz was unanimously voted as the new dean on May 7, 1920. Requirements were cut soon after he became dean. By 1922, he had “salvaged” 1208 hours, or the equivalent of a year of coursework.
But more importantly, he began constructing his great machine for teaching immediately, recruiting excellent full-time faculty, acquiring the New Haven Hospital and Dispensary as teaching facilities, and blueprinting the future, in a volume titled, The Past, Present and Future of the Yale University School of Medicine and Affiliated Institutions [9]. Published in 1922, the volume ended with an article, “Proposed Changes in the Curriculum of the Yale School of Medicine” by Frank P. Underhill, Chairman of the Curriculum Committee.
“In the first place scientific progress during the last twenty-five years has been so great that each coordinate science in medicine has widely extended its borders. In recognition of the fact the medical course has been lengthened to four years. Again, in the enthusiasm of teaching his own subject, there is the decided tendency for each instructor to over-teach—to expect the student to become in turn a finished anatomist, physiologist, pathologist, etc. [17(p64)].”
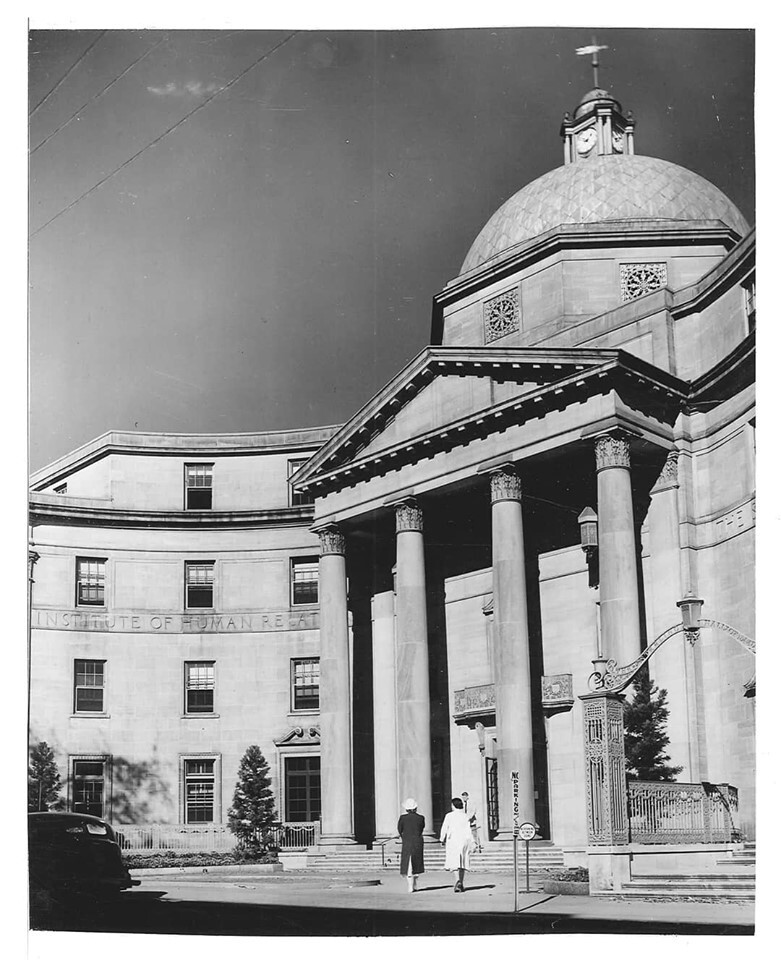
The greatest change in the curriculum occurred only after the Sterling Hall of Medicine was built and dedicated on February 23, 1925. It had a brick entrance with soaring classical columns. The Yale School of Medicine now had a building for its school, a teaching hospital and clinic, and excellent full-time faculty, to comprise a close-knit campus. Vernon Lippard, Dean of the Yale School of Medicine, 1952-1967, would later write,
“It was under these circumstances that the faculty had the courage to introduce a program in which the medical student was treated as a graduate student and given more than customary responsibility for his own development [18(p18)] (Figure 3).”
Figure 3.

The Sterling Hall of Medicine, with its soaring brick façade, was built on the corner of Broad Street and Cedar Street and dedicated on February 23, 1925. Dean Winternitz’s philosophy was for self-directed learning in a “great machine for teaching.” Upon becoming Dean in 1920, Winternitz began constructing a campus for the School of Medicine, and he also cut classroom time and requirements. With the completion of this building, the School of Medicine had classrooms, clinical facilities at the New Haven Hospital, and laboratories at the Brady building, along with full-time faculty. After completion of this building, he virtually eliminated all requirements aside from the thesis and qualifying exams. (Photo from the Yale Alumni Weekly, December 30, 1921).
“The Graduate Plan in Medical Education”
Winternitz instituted a new curriculum in the 1926-1927 school year. In the July 1927 issue of the Bulletin of the Association of American Medical Colleges, he referred to “The Graduate Plan in Medical Education [13(pp208-213].” Here the main points of Winternitz’s paper are pulled from the narrative, and numbered. His precise wording is stated:
1. “There are definite requirements for admission to the so-called School of Medicine. The phrase ‘so-called’ is used because it is not particularly desired to continue the name ‘School of Medicine.’ These requirements are three years of collegiate education with certain specific prerequisites. Under the new system, students who may not have met all of these specific requirements are not necessarily refused.”
2. “After considerable experimentation, it has been concluded that it is undesirable to classify students according to classes. The class system has been abolished and students are listed alphabetically, irrespective of year.”
3. “After the student is admitted to a course, the responsibility of the instructor, in the old sense, is at an end. For example, no roll is called, no tab is kept on the work of the individual, there are no formal daily assignments, and examinations in course or at its end are abolished. Every effort is made to interest the student in the fundamentals of the subject, and he uses his discretion in taking advantage of his opportunities.”
4. “After a varying interval, usually two years, but in some instances one year and in others three years, the student will come to a conclusion concerning his later work, and he will present himself for a qualifying examination, when in his judgment he is properly prepared.”
5. “At the end of an arbitrary period (usually not less than two years) and after the acceptance of his graduating thesis, he again presents himself for examination, and if this is successfully completed, he is recommended for the degree.”
The admission requirement of college, albeit 3 years, reflected the new high standards of the Yale School of Medicine.
The tradition of belonging to a specific class was abolished. Students selected their own courses and the sequence, based upon prior experience and knowledge. They also bore responsibility for approaching professors to gain admittance into courses. A curriculum did not need to be sequential, according to Winternitz. There could be benefits to a reverse order.
The abolishment of roll call, daily assignments, and course examinations became common features of the Yale System through the decades. The qualifying exams and thesis are other features that have been preserved (the National Board Exam has served the function of the qualifying exam, for most of the past century). Although the plan was radically different from medical education at the time (or even now), Winternitz concluded,
“Obviously, there is nothing new in this plan. It is graduate education as this is known all over the world, even in the United States.”
Charles R. Stockard, Professor of Anatomy at Cornell Medical College, commended the “Yale Plan:”
“The great advantage of the Yale plan is the emancipation of the student from the rigid class which holds back the quick, bright individual and embarrasses the intelligent, slow student, neither of whom keeps step with the mediocre pace-makers [19(p1510)].”
The Institute of Human Relations
In referring to the “so-called School of Medicine” as not a particularly desired name, Winternitz may have been alluding to his plans to enlarge the study of medicine. As an eminent scientist, Winternitz also envisioned that medicine needed to be preventative, and to incorporate the social sciences. The School of Medicine, he thought, should be linked to the School of Law, and the Divinity School.
Winternitz envisioned a new Institute of Human Relations that would strive for a unity of human knowledge, incorporating psychology, sociology, anthropology, and a new department of psychiatry. According to Viseltear, the “Yale Plan” was to be an extension of the principles underlying the Institute of Human Relations in the same way that the Institute of Human Relations found expression in the Yale Plan. Each unified, resonated, and reinforced the other [20(p636)].
The Institute of Human Relations was founded in 1929, with the approval of Yale President James Angell. The building was designed as a domed structure, and centerpiece of the Yale School of Medicine Cedar Street campus (Figure 4).
Figure 4.
The elegant domed structure, a prominent symbol of the Yale School of Medicine, was originally built as the entrance for the Institute of Human Relations and the Sterling Hall of Medicine. Today the domed structure is known simply as the Sterling Hall of Medicine. The Institute of Human Relations was short-lived, but its name remains etched in stone above the entrance, and visible from the office of the Dean of the School of Medicine. (Photo courtesy of the Human Relations Area Files.)
The Institute of Human Relations was dedicated on May 9, 1931. It was a professional triumph amidst devastating loss for Winternitz, who was newly widowed.
The prior year, on April 26, 1930, Helen Watson Winternitz, herself a Johns Hopkins-educated physician, died at the age of 45, after a lengthy illness, of what was believed to be nephritis. Today, common causes of renal disease in someone her age would be an infection of the urinary tract, or a post-streptococcal nephritis. Today, Helen Winternitz might be easily cured by antibiotics. But not until 1941, would penicillin be used for the first time in a human, a British constable who was pruning roses when a thorn scratched his face. Within a month, his head was covered with abscesses, and he had lost an eye. Such were the hazards of everyday life, before the age of antibiotics. The constable was given an injection of penicillin, and his fever subsided. But despite all available penicillin, and re-harvesting it from his urine, there was not enough penicillin to rescue his life.
Penicillin worked, but how could enough be produced? To solve this problem, John Farquhar Fulton, a Yale School of Medicine professor, connected Oxford penicillin researcher Howard Florey with American manufacturers.
In 1942, when Anne Miller, the wife of Yale athletic director Ogden Miller, developed a streptococcus infection and fever, Fulton obtained penicillin for her, manufactured by Merck. Miller’s infection subsided, and her life continued.
At Yale, an antibiotic saved a human life for the first time. It was a landmark event in heralding the beginnings of modern medicine, an event that occurred within the “great machine” built by Winternitz.
By the end of the decade, antibiotics were manufactured and widely available. Science and the industrial revolution were finally harnessed in service of lifesaving medical care. The world was a different, safer place.
The Institute of Human Relations was short-lived. The Law School and Divinity School were built elsewhere on the Yale University campus. Winternitz was consoled by his friend, Abraham Flexner, when the IHR dissolved in the late 1930s. Flexner said that the Institute of Human Relations was in actuality, Yale University.
Yet the white dome and soaring classical columns designed for the Institute of Human Relations remains. The building is now known simply as the Sterling Hall of Medicine, or the main Yale School of Medicine building. Etched in stone, above the entrance, in direct view from the office of each dean since Winternitz is the inscription, “Institute of Human Relations.”
As for Winternitz, 1935 marked his last year as dean. He was a man who always evoked strong emotions. In 1935, a new dean was elected and Winternitz stepped down to his prior position as Chairman of the Department of Pathology. The prior year, Winternitz’ own mentor, William Welch had said,
“There is nothing in modern medical education so remarkable as the recent transformation of the Yale School of Medicine from the old type into a modern medical school. The process has taken place with incredible rapidity and it has been complete. The Yale School of Medicine now ranks with the best in the country [9(p79)].” (Figure 5)
Figure 5.
Milton Winternitz in 1957. Winternitz was Dean of the School of Medicine from 1920 to 1935, when the Yale System was founded. Under his leadership, the Yale School of Medicine campus was built, and foundations were laid for Yale to be a leading institution in the era of modern medicine. The Yale System began during this time, as the foundation of medical education at Yale for the next century. Also called the Yale Plan, and the Graduate Plan of Medical Education, the underlying principle of the Yale System is that Yale medical students should be educated in the manner of graduate students, not trade students, in a “great machine for teaching” that included the medical school campus and Yale University. (Medical Historical Library, Harvey Cushing/John Hay Whitney Medical Library, Yale University.)
The Yale System since Dean Winternitz
Stanhope Bayne-Jones, Dean of the Yale School of Medicine between 1935-1940, was committed to the Yale Plan. He stated that Yale produced resourceful, practical students, and that the curriculum promoted a “cultivation of the intellectual capacity to distinguish means from ends [1(p638)].”
Dean Bayne-Jones appointed physiologist Hebbel Hoff to chair a special committee to review the Yale Plan, as it was then called. In 1940, Hoff’s committee concluded that quizzes and course exams were still being given in some departments, and that required coursework had crept up, and needed to be cut back [21(p8)].
But in 1941, all took a backseat to World War II. Medical school at Yale was reduced from 4 years to 3 years. Even the thesis, a staple since 1839, was temporarily suspended, as 89 medical school faculty were deployed in the war effort.
In 1947, Dean Cyril Norman Hugh Long reaffirmed commitment to the Yale System, and wrote about its essential elements:
1. No examination in courses;
2. Ample opportunities for, and a wide selection of, elective courses;
3. The opportunity to spend six years in the school instead of the conventional four, without extra tuition fees;
4. The provision of fellowship which enable the abler students to pursue special education either at Yale or elsewhere;
5. A minimum of required coursework;
6. The encouragement of an interest in research by requiring an original dissertation; and that,
7. Since medical students are adults, no attempt is made to enforce attendance either at classes or clinics or to exercise the kind of general supervision of their activities to which they may have been accustomed elsewhere [1(p643)].
The First Required Course Exams
The most significant change to the Yale System occurred in 1988, when mandatory exams were instituted during Leon Rosenberg’s term as dean. For each basic science course, students took an exam anonymously, with an identification code known only to the chaplain or registrar. The student assumed responsibility for approaching faculty for remediation, upon failing an exam. The chaplain or registrar could also break the identification code, and check with the student.
Robert Gifford, Associate Dean for Student Affairs when the exams were instituted, recalls casually mentioning the term, “minimal competency,” to emphasize that the purpose was to assure basic understanding and to help students prepare for the National Board Exam. To his surprise, the term “minimal competency” became adopted (but temporarily), and it even became the title of a student show. The exams have acquired many names over the years, not all worthy of mention. “Mandatory self-assessment” is a common term today.
The mandatory exams “set off a firestorm of protest by alumni, Dr. Viseltear, and students, who saw it as the end of the Yale System,” according to Gifford.
A decade later, on June 5, 1998 in a medical school reunion talk, Gifford explained the circumstances behind the exams. The National Boards had eliminated subject scores on Part One exams in 1988. Previously, YSM students were required to pass all subjects. Also in 1988, seventeen students failed Part One of the boards, amidst the school broadening admissions to include students with non-science backgrounds, and more diverse gender and ethnic backgrounds. Gifford stated, “But over time, I believe that most students have come to appreciate the way it has been administered, which is quite consistent with the principles of the Yale System.” (R. Gifford, personal communication, 6.3.99)
In 2020, when interviewed for this article, Gifford further explained that the accrediting body “wasn’t going to accredit us…The dean said we had to do it. So I referred to it as Minimal Competency Exams. We were forced to do it. We tried everything to devise a method, where no one would know the score.”
The mandatory exams instituted in 1988 have remained to this day.
Preserving and saving the Yale System has been a recurrent theme since then. Bearing the banner have been students, alumni, faculty, and even deans.
According to Dean Gerard Burrows:
“When Leon Rosenberg stepped down as dean at Yale, I returned to New Haven to meet with the search committee to lobby for the preservation of the Yale system [4(p.xii)].”
Burrows soon found himself as the next Dean of the Yale School of Medicine, a post he held from 1992 to 1997. However, as the new dean, he realized that it was under pressure from accreditation agencies that the course exams were instituted.
Another dean who bore the torch of the Yale System was Herbert Chase, the first Deputy Dean for Education, appointed by Dean David Kessler in 2000.
“The first thing I found was that there was no free time,” Chase said. “The students were in class from nine to five almost every day.” Echoing the founding cries of the Yale System, Chase acted to declutter the overcrowded curriculum. He cut 25 percent of the required hours, the same percentage cut by Winternitz upon becoming dean in 1920.
An unintended consequence occurred. Mandatory self-assessment exams became concentrated in the first year, leading students to experience an erosion of the Yale System. Nine medical students sent letters to approximately 5,000 alumni in February of 2002, asking alumni to sign a petition that exams remain optional. Their letter was signed,
“The Yale System Preservation Initiative.”
More than 500 alumni responded, mostly in favor of the petition [21(pp30-37)].
Dean Chase and Dean Kessler responded by cutting exams for modules in the second year. They affirmed their commitment to the Yale System. (Table 1 and 2).
Table 1. History of Exams in the Yale System.
| 1927 | First comprehensive exams |
| 1931 | Replaced by National Board Exams |
| 1937 | Dean Stanhope Bayne-Jones, a consultant to the National Board Exams, favored dropping it at Yale, because over 99% of students passed it |
| 1940 | A committee headed by Hebbel Hoff found that quizzes and exams were still given in courses, and concluded that they must be reduced |
| 1942 | National Board Exams reinstated |
| 1988 | Anonymous mandatory self-assessment exams instituted for basic science courses |
Table 2. History of Thesis Requirement at the Yale School of Medicine.
| 1839 | First mention in historical records of a thesis requirement |
| 1922 | Time for thesis increased to 3 years |
| 1942 | Eliminated during WWII, when 89 faculty left for military service |
| 1944 | Thesis reinstated |
Celebrating the Yale System
At the mention of the Yale System, many alumni express such loyalty, devotion, and deep personal gratitude, that it one can hardly imagine that the topic is medical school. For example, William Heydorn, Class of 1959, retired hospital commander of the Letterman Army Hospital in San Francisco states, “The Yale System laid the foundation for the rest of my life.” This author credits the Yale System for a career in medicine, but also for fostering a calling as a historian and writer.
During reunion weekend in June of 2017, the Association of Yale Alumni in Medicine presented two programs under the leadership of Richard Kayne, Class of 1976, AYAM President at the time. “The Yale System: A Celebration,” was a history of the Yale System presented by this author. “The Yale System: A Conversation” consisted of four luminary alumni in dialogue: Alexis Boer-Kimball, MD, MPH, Class of 1994, President and Chief Executive Officer of Harvard Faculty Physicians at Beth Israel Deaconess Medical Center; Lee Goldman, MD, MPH, Class of 1973, Dean of the Columbia University College of Physicians and Surgeons; Nobel Laureate Brian Kobilka, MD, PhD, Class of 1981; and Jerome Zeldis, MD, PhD, Class of 1978, former Chief Medical Officer of Celgene. Both programs are viewable online [22,23].
The AYAM has also begun videotaping oral histories of Yale School of Medicine alumni. This growing archive comprises over 70 videotaped oral histories and is held by the AYAM. An initial dissection of the Yale System’s anatomy, as told in these oral histories and in the 2017 recorded programs reveals common themes.
1. The Yale System allows a student to create a tailored, often more rigorous course of study, to further individual interests and talent.
Brian Kobilka took biochemistry and genetics courses in the graduate school, rather than at the medical school. “We had discussions on topics that probably wouldn’t be on boards for another decade,” Kobilka says. Kobilka shared the 2012 Nobel Prize in Chemistry with Robert Lefkowitz, for identifying the adrenalin receptor gene and characterizing the family of g-protein-coupled receptors. Kobilka calls the Yale System “a graduate school of medicine.”
Lee Goldman earned both an MD and an MPH during his four years of medical school. He sometimes brought a textbook to study rather than listen during lectures, often didn’t go at all, and passed the Part 1 of the National Boards before beginning his second year, not a small feat, considering that his undergraduate major was in history. His thesis project helped develop the computer skills needed for the Goldman Index and the research career that led to his becoming chair of medicine at UCSF and then dean of Columbia University’s Vagelos College of Physicians and Surgeons.
Alexis Boer-Kimball honed her communications skills not through courses, but by writing 43 articles for the Atlanta Journal Constitution, as well as news stories for the CBS Evening News with Connie Chung, all contributing to her career as a Harvard-based physician executive.
Jerome Zeldis, an elder statesman of the pharmaceutical industry, whose repurposing of thalidomide has doubled the survival for multiple myeloma, says, “My fund of knowledge was much greater because I had time to read.”
Vivek Murthy, MD, MBA, Class of 2002, was the 19th US Surgeon General. As a medical student at Yale, he created a course on physician wellness that continues to be offered today.
2. The Yale System cultivates a responsibility to learn, while de-emphasizing mastery of information that evolves and that may become outdated.
“What I became didn’t exist then. There was no field, pediatric rheumatology,” says Amy Starr, Class of 1974, a pediatric rheumatologist in Manhattan.
“When I took boards in pathology, there was one board in anatomic. Then there were two boards. Now there are eight boards: blood banking, microbiology, clinical, chemistry, forensic…,” says Dwight Miller, Class of 1956, Emeritus Director of the Pathology Lab at St. Mary’s Hospital in Waterbury, Connecticut.
“You learn rapidly that the things that come in those didactic lectures are only things that are good for maybe ten years, and then things are going to be different, and they’re not worth spending that much time learning them. So the big advantage of the Yale System is to learn how to think and how to process information,” says William Heydorn.
According to Goldman, “Knowledge is transient. The way you learn to think is durable…A curriculum that is too information based, by definition can’t succeed.”
3. The Yale System emphasizes questioning over answering.
Nobel Laureate Kobilka recalls that as an undergraduate, he was accustomed to spending all his time studying for exams. The Yale System changed him, “Not having a defined body of knowledge that I was responsible for—I started becoming more interested in pursuing subjects that I didn’t understand, things I found interesting.”
“Exploring my own questions inverted the process for me…I realized I could be more effective if the research focused on my own questions,” says Boer-Kimball, who has published over 250 scientific papers.
Amy Starr says simply of the Yale System, “And then it got to, well, what do I think is important?”
4. The thesis encourages critical thinking and use of the scientific method in clinical practice.
Anita Goodrich Licata, Class of 1989, who runs a large dermatology practice in Burlington, Vermont, says, “the Yale System taught me to always verify, to not work within the dogma of your profession.”
According to Amy Starr, the thesis “made me more skeptical of a lot of articles I read. It was very helpful my whole career.”
5. The lack of grades and tests fosters collaboration over competition.
According to Murthy, “Our team that I led as Surgeon General became a mutually supportive family. When we feel supported, when we feel we are coming to work with friends, we can often do more and achieve more than in an environment where we are fending for ourselves. That’s what the Yale System was like for me. The Yale System helped me see more clearly what is possible when you build a community of true belonging.”
Jesse Flaxenburg, Class of 1999, a nephrologist in Colorado Springs, Colorado, states, “The fact that you got here means that you’re an incredibly talented person. Adding that extra layer of competition between…maybe the top four percent, is totally unnecessary.”
6. The Yale System encourages a broader, more in-depth way of thinking.
“We studied. We didn’t study for an ‘A’. We studied for the material,” says Lauren Hyman, Class of 1994, who practices Obstetrics and Gynecology in Agoura Hills, California.
“I learned how to think, to know more than what was being fed to me,” says Ed Marut, Class of 1974, an endocrinologist in Chicago.
Goodrich-Licata says, “studying for tests and grades creates a lot of focus on just learning a small slice of material that doesn’t represent a whole field of study.”
7. The Yale System educates humane physicians.
“I was becoming a person between the age of twenty-one and twenty-five,” says Lauren Hyman. “Those are very formative years. To spend them locked in a library only studying medicine, that’s not what Yale is about, thank God.”
Anita Goodrich Licata says, “Removing that anxiety of competition enabled me to become the best person I could, and to become the best physician I could.”
Acknowledgments
The author expresses gratitude to the Association of Yale Alumni in Medicine and the student editors of the Yale Journal of Biology and Medicine for providing the vision and support for this work of scholarship. Special thanks go to AYAM Executive Committee members Donald Moore, MD; Harold Mancusi-Ungaro, Jr., MD; and J. McLeod Griffiss, MD. Robert Winn, JD, MFA, recorded the programs and many of the oral histories that were sources for this article. Steven Bergman, MPPA, provided feedback. Zoe Calott-Wang assisted with permissions. Editorial vision and support was provided by: Helen Beilinson, Amelia Hallworth, Devon Wasche, and Wei Ng.
Author Contributions
DCW wrote and edited the manuscript.
Author's Bio
Dora Calott Wang, MD, MA, Class of 1989, was a thesis student of medical historian David Musto, MD, MA, and was a student influenced by Arthur Viseltear, PhD. She earned her MA in English, with an emphasis in medical history, at the University of California, Berkeley. She is the author of two books. The Kitchen Shrink: A Psychiatrist’s Reflections on Healing in a Changing World (Riverhead/Penguin Random House, 2010) was nominated by her publisher for the Pulitzer Prize. The Daily Practice of Compassion: A History of the University of New Mexico School of Medicine, Its People and Its Mission, 1964-2014 (University of New Mexico School of Medicine Press, 2014) won a New Mexico-Arizona Book Award.
References
- Viseltear AJ. The Yale Plan of Medical Education: the early years. Yale J Biol Med. 1986. Nov-Dec;59(6):627–48. [PMC free article] [PubMed] [Google Scholar]
- Goff-Crews K, Baier L. School of Medicine 2019–2020. Bulletin of Yale University [Internet]. 2019. July;115(8): Available from: https://bulletin.yale.edu/sites/default/files/school-of-medicine-2019-2020.pdf [Google Scholar]
- Yale System and Educational Mission [Internet]. Medical Education at Yale. [cited 2020 May 11]. Available from: https://medicine.yale.edu/education/curriculum/yalesystem/
- Burrow GN. A history of Yale’s School of Medicine: passing torches to others. New Haven: Yale University Press; 2002. 10.12987/yale/9780300092073.001.0001 [DOI] [Google Scholar]
- Wang D. Health Care, American Style: How Did We Arrive? Where Will We Go? Psychiatr Ann. 2014. July;44(7):342–8. 10.3928/00485713-21040707-08 [DOI] [Google Scholar]
- Norton PW, Spiro HM. Dean Winternitz: Yale Medical School’s Passionate Humanist. New Haven (CT): Program for Humanities in Medicine, Yale University; 2011. [Google Scholar]
- Rae DW. City: Urbanism and Its End. Yale University Press; 2005. [Google Scholar]
- Falvey KL, Duffy TP, Belitsky R. Medicine at Yale: the first 200 years. New Haven, Conn.; London: Yale University Press; 2010. [Google Scholar]
- Winternitz MC. The past, present & future of the Yale University School of Medicine and allied institutions. New Haven: Yale University; 1922. [Google Scholar]
- Winternitz MC, Wason IM, McNamara FP. The pathology of influenza. New Haven (CT); 1920. [Google Scholar]
- Liebow AA, Waters LL. Milton Charles Winternitz February 19, 1885-October 3, 1959. Yale J Biol Med. 1959. December;32(3):b1–164. [PMC free article] [PubMed] [Google Scholar]
- Winternitz MC. The Graduate Plan of Medical Education. The Bulletin of the American Association of Medical Colleges. 1927. July;2(3). [Google Scholar]
- Flexner A. Milton Charles Winternitz. Yale J Biol Med. 1950. July;22(6):575–7. [PMC free article] [PubMed] [Google Scholar]
- Yale Alumni Weekly 1921. December 30;364–70.
- Sullivan W. Sterling sexuality: Was Yale patron gay? Yale Daily News [Internet]. 2003. April 3 [cited 2020 May 11]; Available from: https://yaledailynews.com/blog/2003/04/03/sterling-sexuality-was-yale-patron-gay/
- Underhill FP. Proposed Changes in the Curricuum of the Yale School of Medicine Past, Present, Future of the Yale University School of Medicine and Allied Institutions. New Haven (CT): Yale University; 1922. pp. 64–6. [Google Scholar]
- Lippard VW. The Yale plan of medical education after thirty years. J Med Educ. 1954. September;29(9):17–23. 10.1097/00001888-195409000-00001 [DOI] [PubMed] [Google Scholar]
- Stockard CR. Medical Education and the Yale Announcement. JAMA. 1926. May;86(20):1508–11. 10.1001/jama.1926.02670460016005 [DOI] [Google Scholar]
- Viseltear AJ, Milton C. Milton C. Winternitz and the Yale Institute of Human Relations: a brief chapter in the history of social medicine. Yale J Biol Med. 1984. Nov-Dec;57(6):869–89. [PMC free article] [PubMed] [Google Scholar]
- Burr H. Report of Section A of the Committee on Correlation of the Biological Sciences and Clinical Medicine on the New Educational Program and The Qualifying Examination. Board of Permanent Officers Minutes; 1929. [Google Scholar]
- Curtis J. Everyone loves the Yale System. So why can’t they all agree? [Internet]. Yale School of Medicine. [cited 2020 May 11]. Available from: https://medicine.yale.edu/ysm/news/yale-medicine-magazine/everyone-loves-the-yale-system-so-why-cant/
- The Yale System A Celebration - YouTube [Internet]. [cited 2020 May 12]. Available from: https://www.youtube.com/watch?v=SE4tAw0f2gk
- The Yale System A Conversation - YouTube [Internet]. [cited 2020 May 11]. Available from: https://www.youtube.com/watch?v=JVmEtiU8mkM