The New York City Sexually Transmitted Disease Prevention Training Center at Columbia University administered a provider survey to understand how the COVID-19 pandemic is affecting the availability of sexual health care services regionally.
Abstract
As the COVID-19 pandemic causes upheaval in New York City (NYC), 1 consequence is the accessibility of sexual health services. The NYC STD Prevention Training Center at Columbia University administered an online provider survey to understand how the COVID-19 pandemic is affecting the availability of sexual health care services regionally.
On March 1, 2020, Governor Cuomo of New York State (NYS) announced New York's first case of the SARS-CoV-2, a novel coronavirus 2019 known as “COVID-19.”1 Since this first case, New York City (NYC) has emerged as the epicenter in the United States for the COVID-19 pandemic. National Sexually Transmitted Disease (STD) awareness month falls in April 2020, and this month is traditionally dedicated to reaching out to communities to enhance recognition about the importance of preventing, testing, and treating sexually transmitted infections (STIs). In 2017, NYC case rates for chlamydia were 839.69 per 100,000, 275.15 per 100,000 for gonorrhea, and 21.07 for primary and secondary syphilis and perhaps most startling, 6.64 per 100,000 for congenital syphilis.2 Presently, NYC is faced with a 2-fold challenge being both the epicenter of the COVID-19 pandemic and having high STI rates that are in the top 10 nationally. With nonessential services closing as of March 22, 2020, and hospitals around the city encouraged to optimize their resources, sexual health services were reduced across NYC.
Key clinics that serve New York residents were either dramatically reduced or completely cut. Specifically, on March 18, 2020, the NYC Department of Health and Mental Hygiene informed the community that 7 of 8 sexual health clinics would close, and 1 clinic would be open for limited and emergency services only.3 In addition, a community health center, which is a major provider of health care and sexual health services targeted to New York's lesbian, gay, bisexual, and transgender communities, announced that they would be limiting their in-person visits. Their website announcement stated “At this time, all sexual health and preexposure prophylaxis appointments have been canceled. If you have had a recent exposure, need postexposure prophylaxis, or have an urgent question, please call the triage nurse.”4 The NYC Planned Parenthood clinics moved to a virtual appointment only model: “All services will be virtual, except for abortion services and select in-person visits.”5 Finally, New York-Presbyterian Hospital's human immunodeficiency virus (HIV) Prevention Program began tapering services starting March 19, 2020, limiting onsite visits to only urgent cases, such as postexposure prophylaxis. Those patients with symptomatic STIs were discouraged from coming into clinic to avoid their risk of COVID-19 exposure and were treated presumptively with a corresponding telehealth visit. Preexposure prophylaxis prescriptions were refilled without quarterly STI and HIV screening. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf.
It is understood that even in the time of “stay-at-home” orders (New York State instituted on March 22, 2020) and mandates to “shelter-in-place,” people may continue to have condomless sex, thus continuing the spread of STIs.6 Further, states are reporting redeployment of disease intervention specialists and STI program staff to assist in the public health response to COVID-19, including those responsible for contact tracing, an important part of the management of STIs.7 Contact tracing helps to prevent reinfection of the index case, minimize complications, and reduce the population prevalence of STIs in the community. If these resources are redirected toward COVID-19, there exists the potential for a proliferation of STIs, including HIV.
The NYC STD Prevention Training Center (PTC) at Columbia University Mailman School of Public Health provides clinical education on STIs to health care providers. To better understand how the COVID-19 pandemic is affecting the current availability of sexual health care services and educational needs of providers, a brief provider survey was distributed.
A convenience sample was used, made up of individuals on the NYC STD PTC educational mailing list and also key partners from both state and local health departments. The survey was administered via an online survey platform (Qualtrics, Provo, UT). Univariate analysis was done to assess the availability of sexual health services pre and post April 1, 2020, and in NYS and outside of NYS (respondents from Indiana, Ohio, Michigan, New Jersey, Puerto Rico, and United States Virgin Islands). The survey asked respondents to report on services that they offered before March 1, 2020, and services they were performing after April 1, 2020. These dates were chosen to clearly define a time preclinical and postclinical service provision considerations for the COVID-19 pandemic.
Seventy-three individuals responded to the survey (as of April 20th); 61 respondents were outside of NYS while 12 reported to be located within NYS. Sixty-two percent of the respondents stated that their clinic was located in an urban environment. Two thirds of respondents (67%) stated that they had expertise with an adolescent population. Fourteen (19%) of the respondents stated that their clinics had been closed due to the COVID-19 outbreak, and 40 (56%) were functioning on an appointment only basis.
As of April 1, 2020, the majority of clinics providing sexual health services indicated a significant decrease in the regular services they were able to provide (Fig. 1). There was a decrease in all services provided except for an expansion in telehealth services. Notably, 16 respondents stated that before March 1, 2020, they regularly offered services surrounding pregnancy termination, as of April 1, 2020, only 4 stated they were still able to offer these services regularly (75% reduction).
Figure 1.
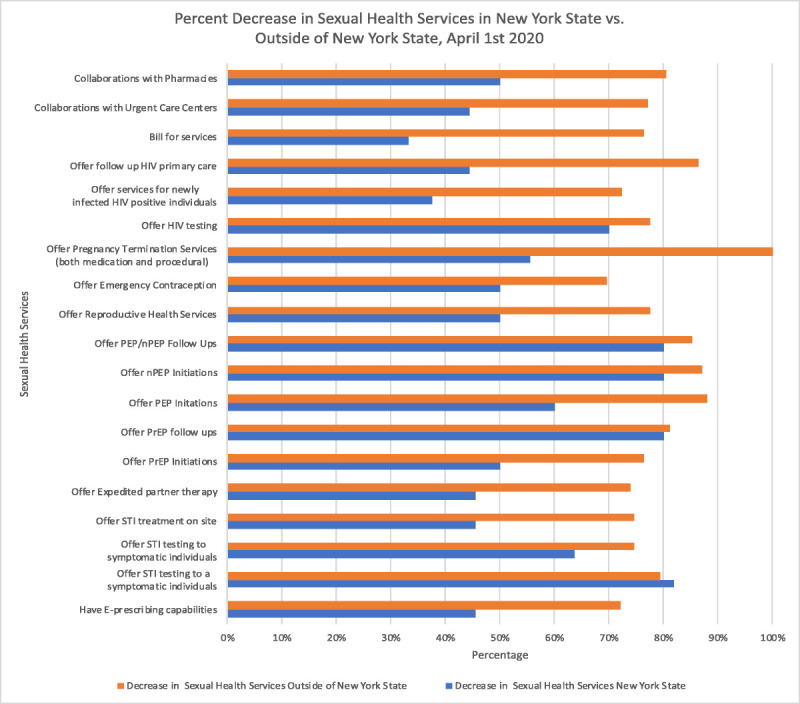
Respondents indicated in the survey what services they provided prior to March 1st 2020 and then after April 1st 2020. The graphic indicates the percent decrease in sexual health services divided into respondents providing services inside of New York State and those outside of New York State. Note: 61 survey respondents were providing services outside of NYS and 12 were located within NYS.
Before March 1, 2020, in NYS, 11 clinics reported offering STI testing either for symptomatic or asymptomatic patients; however, as of April 1, 2020, only 18% of those sites were still able to offer STI testing to asymptomatic patients. Overall, 80% of respondents stated that since the beginning of the COVID-19 outbreak in the United States, their clinic providers have resorted to treating STIs presumptively based on symptomology, before testing. Finally, as of April 1, 2020, just 25% of respondents located in NYS and 26% of sites outside of NYS are able to offer HIV testing.
The COVID-19 pandemic has resulted in a significant reduction in the availability of sexual health services. In response to these limitations on sexual health service partners in NYC, clinicians have been working to find innovative ways to accommodate the needs of their patients. For example, on April 7, 2020, the NYC Department of Health and Mental Hygiene expanded the Community Home Test Giveaway program to be available to their funded sites in New York City. Patients can now be provided with codes, through the Community Home Test Giveaway, to purchase a free HIV third-generation testing kit online and have those kits mailed to directly to their home for self-administration. However, there is still no feasible option for at home or off-site STI testing. Another example is at New York-Presbyterian's Columbia campus, where they implemented a system to address sexual health concerns for those individuals being seen in cough, cold, and fever tents outside of the emergency department. In these tents, patients with symptoms of COVID-19 are evaluated, and if the patient is also presenting with STI symptoms, they can conduct a Telehealth visit with one of their sexual health providers. The sexual health provider is then able to order the necessary treatment and HIV/STI testing to be conducted via the cough, cold, and fever tents, with the exception of extragenital STI screening. Expedited partner therapy (EPT), enables providers to provide prescriptions or medications to a patient's partner without an examination or visit and can be used to help mitigate the spread of STIs. This is particularly useful when in-person visits are not possible. States have and should continue to consider expanding the availability of EPT in response to COVID-19.
On April 6, 2020, the CDC released guidance for STD clinic settings where services have been disrupted and, particularly, for those offering telehealth. The guidance focuses on oral treatment options to consider for symptomatic patients and their partners when in-person clinical evaluation is not possible for complaints, such as vaginitis, male urethritis, genital ulcer disease, and proctitis syndrome.8 National STI rates had been increasing before the pandemic, reaching an all-time high in 2018 and marking the fifth consecutive year of increases for chlamydia, gonorrhea, and syphilis.9 The combination of syndromic treatment and EPT may mitigate some of the effects produced by the halt in widespread testing; however, many STIs are asymptomatic, and therefore, there will likely be a substantial decrease in the number of STIs detected and treated.10
A limitation of this survey is that respondents were asked to report their clinic zip codes and clinic name was optional, thus it is possible that multiple clinicians responded on behalf of the same clinical site.
The impact of the COVID-19 pandemic on nationwide sexual health service provision has only started to manifest. As the pandemic's impact becomes wider both regionally and nationally, the effects on the sexual health care of patients will continue to accumulate. With NYC at the leading edge of the COVID-19 epidemic, there is an opportunity for other jurisdictions, outside of New York State, to plan for the potential impact on the availability of sexual health services. There is an urgency to provide more support for STI and HIV services, develop innovative models for the continuation of sexual health services and provide educational guidance on effective clinical care. Further, there is a need to ensure that sexual health services should be part of future pandemic and emergency preparedness planning.
Footnotes
Conflict of Interest and Sources of Funding: J.Z. is supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under award number L30 AI133789.
REFERENCES
- 1.New York State Department of Health and Mental Hygiene. COVID-19 Frequently Asked Questions. Published: March 17th, 2020. https://coronavirus.health.ny.gov/system/files/documents/2020/03/faqscovid19_32120doh.pdf Accessed April 12, 2020.
- 2.The New York City Department of Health and Mental Hygiene Bureau of Sexually Transmitted Infections. Quarterly Report Vol. 16, No 2018. https://www1.nyc.gov/assets/doh/downloads/pdf/std/std-quarterlyreport2018-4.pdf. Accessed April 12, 2020. [Google Scholar]
- 3.The New York City Department of Health and Mental Hygiene Bureau of Sexually Transmitted Infections. Sexual Health Clinic Press Release: https://www1.nyc.gov/site/doh/services/sexual-health-clinics.page. Accessed April 12, 2020. [Google Scholar]
- 4.Callen-Lorde Health Center. COVID-19 Related Service Changes. https://callen-lorde.org/covid-19-related-service-changes/. Accessed April 12, 2020.
- 5.Planned Parenthood Greater New York. Press Release: https://www.plannedparenthood.org/planned-parenthood-greater-new-york. Accessed April 12, 2020.
- 6.Chiasson MA, Hirshfield S, Humberstone M, et al. Increased high risk sexual behavior after September 11 in men who have sex with men: An internet survey. Arch Sex Behav 2005; 34:527–535. 10.1007/s10508-005-6278-5. [DOI] [PubMed] [Google Scholar]
- 7.National Coalition of STD Directors, April 7 2020 COVID-19 Command Center Alert. https://www.ncsddc.org/resource/covid-command-center-for-std-programs/. Accessed April 12, 2020.
- 8.Centers for Disease Control and Prevention (CDC). Dear Colleague Letter. Published April 6 2020 https://www.cdc.gov/std/dstdp/DCL-STDTreatment-COVID19-04062020.pdf. Accessed April 12, 2020.
- 9.Centers for Disease Control and Prevention (CDC). Sexually Transmitted Disease Surveillance 2018, https://www.cdc.gov/std/stats18/default.htm. Accessed April 12, 2020.
- 10.Patton ME, Kidd S, Llata E, et al. Extragenital gonorrhea and chlamydia testing and infection among men who have sex with men—STD surveillance network, United States, 2010-2012. Clin Infect Dis 2014; 58:1564–1570. doi:10.1093/cid/ciu184. [DOI] [PMC free article] [PubMed] [Google Scholar]


