Highlights
-
•
The prevalence of anxiety and depression symptoms was 3.4% and 22.8% among workers during the COVID-19 epidemic in China.
-
•
Epidemic-related factors especially having confirmed cases in the community and having confirmed friends were associated with the higher risk of anxiety and depression symptoms.
-
•
Major traditional risk factors, such as general or poor health status and always drinking alcohol, were found still to be the dominant factors associating with the increased risk of anxiety and depression symptoms.
-
•
Approximately 67.3% and 26.8% of workers reported demand for psychological education and interventions, respectively.
Keywords: Coronavirus disease 2019, Anxiety symptoms, Depression symptoms, Epidemic-related factors, Workers
Abstract
Background
COVID-19 has gained intense attention globally. However, little is known about the COVID-19-ralated mental health status among workers.
Methods
The cross-sectional online survey with 123,768 workers was conducted from February 2, 2020 to February 7, 2020 on a mega-size labor-intensive factory in Shenzhen, China. Oral consent was obtained prior to the questionnaire survey. The information collected in the survey included demographic characteristics, psychological symptoms, COVID-19-related information, and demands for psychological education and interventions. Symptoms of anxiety and depression were measured by the Zung's Self-Rating Anxiety Scale and Self-Rating Depression Scale. Logistic regression models were performed to determine the association between related factors and mental health status.
Results
The prevalence of anxiety and depression symptoms was 3.4% and 22.8%, respectively. The dominant epidemic-related factors were having confirmed cases in the community (odds ratio [OR], 2.75, 95% CI, 2.37–3.19) and having confirmed friends (OR, 2.44; 95% CI, 1.69–3.52) for the increased risk of anxiety and depression symptoms, respectively. Nevertheless, major traditional risk factors such as general or poor health status and always drinking alcohol were still the dominant factors associated with the increased risk of anxiety and depression symptoms. Overall, 67.3% and 26.8% workers reported desire for psychological education and interventions, respectively.
Limitations
All assessments were self-reported, resulting in a risk of method bias.
Conclusions
Our findings show a relatively low prevalence of anxiety symptoms, a relatively high prevalence of depression symptoms, and urgent demand for psychological education and interventions among workers during the COVID-19 outbreak.
1. Introduction
In December 2019, the Chinese city of Wuhan reported an outbreak of acute respiratory illness (Lu et al., 2020), which was subsequently named Coronavirus Disease 2019 (COVID-19) by the World Health Organization (WHO). Cases spread not only to other cities in China, but also internationally as well (Holshue et al., 2020; Hui et al., 2020; Phan et al., 2020; Wang et al., 2020; WHO, February 9, 2020). On January 30, 2020, the WHO declared the event to be a public health emergency of international concern (WHO, Jan 30, 2020). To control the spread of COVID-19, the Chinese government ordered all companies not to resume operations until February 10, 2020 (General Office of the State Council, Jan 27, 2020). Over 80 million people returned to work near or after February 10, 2020, triggering a return trip peak for workers. Due to a low level of education, a relatively weak awareness of infectious diseases prevention and control, a high-intensity workload, and high crowd densities after returning to work, workers were high–risk populations for the spread and rebound of the epidemic. Thus, government departments needed to pay more attention to the workers for prevention and control of the COVID-19 epidemic.
Previous studies have shown that a large-scale epidemic disease not only seriously endangers people's life and property safety but also has a negative impact on mental health, such as anxiety, depression, and other negative emotions, and can cause a psychological crisis. For instance, the public became more pessimistic in their life after experiencing the epidemic of the severe acute respiratory syndrome (SARS) in 2003 (Lau et al., 2006). Other previous studies on large–scale epidemics also showed that the probability of group panic in an outbreak is much higher than the risk of contracting the disease (Betancourt et al., 2016; Kelly et al., 2019; Leung et al., 2005; Mohammed et al., 2015; Reardon, 2015; Shultz et al., 2015). Therefore, the National Health Commission issued the "Guiding Principles for Emergency Psychological Crisis Intervention for the Pneumonia Epidemic of New Coronavirus Infection" (National Health Commission of China, Jan 26, 2020.). Emerging studies on the relationship between COVID-19 and mental health status have been published (Huang and Zhao, 2020; Ma et al., 2020; Nie et al., 2020; Wang et al., 2020; Xiao et al., 2020). However, the available studies mainly focused on the general population, medical workers, and infected patients. Currently, there is no known information about the mental health status of factory workers during the peak of the COVID-19 epidemic.
Therefore, in a large cross–sectional online study, we investigated the prevalence of anxiety and depression symptoms, as well as related factors, among factory workers during the epidemic period of COVID-19. Moreover, we also explored the demand for psychological education and interventions.
2. Methods
2.1. Study design and setting
The data used in the present study were derived from a cross-sectional online survey based on a mega-size labor-intensive factory in Shenzhen, Guangdong Province, China, with 180,000 employees from various provinces across the country. The survey was divided into seven modules, including demographic characteristics, lifestyle factors, epidemic-related factors, traffic information, knowledge, attitude, and practice (KAP), and demand for psychological education and interventions during the period of epidemic.
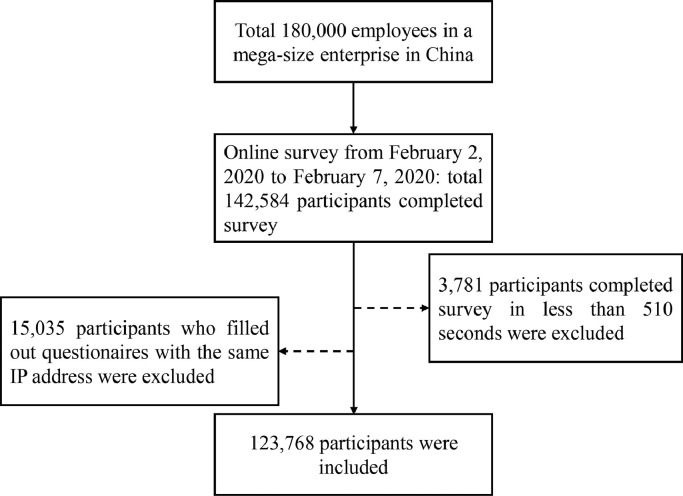
The present survey was conducted online using an electronic questionnaire. Oral consent was obtained from the respondents prior to beginning the survey. The survey was conducted from February 2, 2020 to February 7, 2020. Overall, 142,584 respondents completed the survey, yielding a response rate of 79.2%. After excluding respondents who filled out questionnaires with the same IP address (n = 15,035) and those who completed the survey in less than 510 seconds (n = 3781), 123,768 respondents were ultimately included in the analyses, yielding an effective response rate of 68.8% (Fig. 1 ). The distribution of the respondents by province or region can be found in Table S1 in the Supplement. The protocol of this study was approved by the Biomedical Ethics Committee of Southern Medical University.
Fig. 1.
Flowchart of respondent’ selection process.
2.2. Data collection
Data were collected online via a large free questionnaire platform — the Chinese survey website Wenjuanxing (https://www.wjx.cn/). Workers were asked to complete a self-administered questionnaire, which took approximately 10–15 minutes. To avoid repetition, questionnaires submitted from the same IP address as a previously submitted questionnaire were not accepted.
2.3. Survey tools
Anxiety and depression symptoms were assessed by the wildly used Zung's Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS) for testing mental health status (Zung, 1971; Zung et al., 1965). The SAS and SDS consist of 20 self–reporting items about anxiety and depression symptoms, respectively. Some of the items were worded symptomatically positive and rated on a 4–1 scale (a little of the time, some of the time, good part of the time, and most of the time), while others were symptomatically negative and rated on a 1–4 scale (a little of the time, some of the time, good part of the time, and most of the time). The tools used in this study are listed in the Supplement. A standardized scoring algorithm was used to determine anxiety and depression symptoms, with a total score of 20–80. Anxiety symptoms were identified if the SAS score was ≥50, while score of 50–59 was “mild”, 60–69 was “moderate”, and ≥70 was “severe”. Similarly, depression symptoms were identified if the SDS score was ≥ 53, while score of 53–62 was “mild”, 63–72 was “moderate”, and ≥ 73 was “severe”.
2.4. Definitions of subgroups
Two variable sets were considered to be stratification variables, including epidemic-related variables and demographic variables. The epidemic-related variables were defined as follows: cumulative number of confirmed cases in the provinces (1–499, 500–999,1000–9999, and ≥10,000); have infected cases in the community or not (no case, suspected cases, confirmed cases, and not clear); having infected relatives or not (no case, suspected cases, confirmed cases, and not clear); having infected friends or not (no case, suspected cases, confirmed cases, and not clear); having passed by, traveled to, or having lived in Hubei province in the last two weeks (none, having passed by Hubei province, having traveled to Hubei province, and having lived in Hubei province). The demographic variables were defined as follows: sex (male or female), age groups (≤ 25 years, 26–35 years, or ≥ 36 years), education levels (≤ 6 years, 7–9 years, 10–12 years, or ≥13 years), ethnicities (Han or minorities), provinces or regions (Hubei province or others), residence (urban or rural), marital status (married or not married), health status (very healthy, well, or general or poor), smoking status (hardly ever, sometimes, or always), and alcohol consumption (hardly ever, sometimes, or always), positions (general worker, line supervisor, group leader, or manager), and seniority (0–6 months, 7–12 months, 13–24 months, or >24months).
2.5. Assessment of demand of psychological education and interventions
The “demand for psychological education” was assessed with the following question: “Do you have a demand for psychological education?” with responses of “yes” or “no”. If someone answered yes, they would be asked “What kind of knowledge for psychological education do you need?” with responses of “the common symptom of COVID-19”, “ways to alleviate the psychological effects”, “ways to seek professional psychological help”, or “others”. The “demand for psychological interventions” was assessed with the following question: “Do you have a demand for receiving psychological interventions?” with responses of “very”, “moderate”, “a little” or “no”. If someone answered very, moderate, or a little, they would be asked “What kind of psychological interventions do you need?” with responses of “counselling”, “promotion of mental health knowledge”, “mental health training course”, “psychological assessment”, “group building and other development activities”, “psychological salon”, or “others”. Meanwhile, they also would be asked “When are you willing to receive the psychological interventions?” with responses of “morning meeting”, “after work”, “at weekend”, “lunchtime”, “dinner time”, and “others”.
2.6. Statistical analysis
All statistical analyses were performed using SPSS version 25; all tests were 2-sided, and statistical significance was set at p < 0.05. The mean and standard deviation (SD) (continuous variables) or number and percentage (categorical variables) were used to describe the characteristics of the respondents. Bivariable logistic regression analyses were applied to test the associations of potential explanatory variables including demographic variables and epidemic-related variables with anxiety and depression symptoms. To measure the associations of epidemic-related variables with anxiety and depression symptoms, multivariable logistic regression models were used to adjust for demographic variables including sex, age group, education level, residence, marital status, health status, smoking status, alcohol consumption, positions, and seniority.
3. Results
3.1. Demographic characteristics
This analysis included 123,768 (mean [SD] age: 30.3 [6.4] years) respondents, of whom 87,330 (70.6%) were male and 36,438 (29.4%) were female (Table 1 ). A majority (70.3%) of respondents completed high school, 89.1% were Han nationality, 8.0% lived in Hubei province during the survey, 55.3% lived in urban, and 40.4% were married. In terms of health status, 74.7% of workers reported “very healthy”, 23.3% reported “well”, and 2.1% reported “general or poor”. About 73.5% of respondents hardly ever smoke, and 90.3% hardly ever drink. In addition, about 76.4% of the respondents were general workers, 6.0% were line supervisors, 4.9% were group leaders, and 12.8% were managers. Respondents with more than 24 months of service accounted for 50.6%. Compared to female respondents, male respondents were more likely to have senior positions and lived in the province with a less cumulative number of confirmed cases (Table 1).
Table 1.
Demographic characteristics of respondents
| Characteristics | Total, No. (%) | No. (%) | Pearson χ2 | P Value | |
|---|---|---|---|---|---|
| Male | Female | ||||
| (N = 123,768) | (N = 87,330) | (N = 36,438) | |||
| Age, mean (SD), years | 30.3 (6.4) | 30.5 (6.4) | 30.1 (6.6) | 362.008 | <0.001 |
| Education levels, years | 6.109 | 0.106 | |||
| ≤6 Years | 1065 (0.9) | 766 (0.9) | 299 (0.8) | ||
| 7–9 Years | 35,682 (28.8) | 25,108 (28.8) | 10,574 (29.0) | ||
| 10–12 Years | 48,522 (39.2) | 34,128 (39.1) | 14,394 (39.5) | ||
| ≥13Years | 38,499 (31.1) | 27,328 (31.3) | 11,171 (30.7) | ||
| Ethnicities | 1.129 | 0.288 | |||
| Han | 110,243 (89.1) | 77,840 (89.1) | 32,403 (88.9) | ||
| Minorities | 13,525 (10.9) | 9490 (10.9) | 4035 (11.1) | ||
| Provinces or Regions | 2.275 | 0.131 | |||
| Hubei | 9924 (8.0) | 7068 (8.1) | 2856 (7.8) | ||
| Others | 113,844 (92.0) | 80,262 (91.9) | 33,582 (92.2) | ||
| Residence | 0.093 | 0.761 | |||
| Urban | 68,505 (55.3) | 48,361 (55.4) | 20,144 (55.3) | ||
| Rural | 55,263 (44.7) | 38,969 (44.6) | 16,294 (44.7) | ||
| Marital status | 0.051 | 0.822 | |||
| Married | 49,983 (40.4) | 35,250 (40.4) | 14,733 (40.4) | ||
| Not married | 73,785 (59.6) | 52,080 (59.6) | 21,705 (59.6) | ||
| Health status | 1.641 | 0.440 | |||
| Very healthy | 92,396 (74.7) | 65,147 (74.6) | 27,249 (74.8) | ||
| Well | 28,832 (23.3) | 20,363 (23.3) | 8469 (23.2) | ||
| General or poor | 2540 (2.1) | 1820 (2.1) | 720 (2.0) | ||
| Smoking status | 0.933 | 0.627 | |||
| Hardly ever | 91,008 (73.5) | 64,282 (73.6) | 26,726 (73.3) | ||
| Sometimes | 892 (7.2) | 6286 (7.2) | 2640 (7.2) | ||
| Always | 23,834 (19.3) | 16,762 (19.2) | 7072 (19.4) | ||
| Alcohol consumption | 2.830 | 0.243 | |||
| Hardly ever | 111,717 (90.3) | 78,889 (90.3) | 32,828 (90.1) | ||
| Sometimes | 11,032 (8.9) | 7742 (8.9) | 3290 (9.0) | ||
| Always | 1019 (0.8) | 699 (0.8) | 320 (0.9) | ||
| Positions | 9.342 | 0.025 | |||
| General worker | 94,523 (76.4) | 66,610 (76.3) | 27,913 (76.6) | ||
| Line supervisor | 7455 (6.0) | 5249 (6.0) | 2206 (6.1) | ||
| Group leader | 6008 (4.9) | 4187 (4,8) | 1821 (5.0) | ||
| Manager | 15,782 (12.8) | 11,284 (12.9) | 4498 (12.3) | ||
| Seniority, months | 0.392 | 0.942 | |||
| 0–6 months | 29,253 (23.6) | 20,680 (23.7) | 8573 (23.5) | ||
| 7–12 months | 16,317 (13.2) | 11,516 (13.2) | 4801(13.2) | ||
| 13–24 months | 15,560 (12.6) | 10,979 (12.6) | 4581(12.6) | ||
| >24months | 62,638 (50.6) | 44,155 (50.6) | 18,483(50.7) | ||
| Cumulative number of confirmed cases in the provinces | 70.549 | <0.001 | |||
| 1–499 | 26,860 (21.7) | 19,420 (22.2) | 7740 (20.4) | ||
| 500–999 | 84,283 (68.1) | 59,185 (67.8) | 25,098 (68.9) | ||
| 1000–9999 | 2701 (2.2) | 1945 (2.2) | 756 (2.1) | ||
| ≥10,000 | 9924 (8.0) | 6780 (7.8) | 3144 (8.6) | ||
CI, confidence interval.
3.2. Bivariable analysis: association of epidemic-related factors and major demographic factors with anxiety and depression symptoms
Overall, 3.4% of respondents reported anxiety symptoms, ranging from 2.9% mild to 0.3% moderate and 0.2% severe; while 22.8% of respondents reported depression symptoms, ranging from 9.6% mild to 13.1% moderate and 0.1% severe. Table 2 describes the results of the bivariate analysis. According to the influence on the risk of anxiety and depression symptoms, the epidemic-related exposures ranked as follows: having infected friends, having infected relatives, having infected cases in community, increased cumulative number of infected cases in provinces, and having lived in Hubei province in the last two weeks. Interestingly, the prevalence of anxiety and depression symptoms was significantly lower among respondents who recently lived in Hubei province compared with those who lived in other provinces or regions.
Table 2.
Bivariate analysis:association of epidemic-related factors and major demographic factors with anxiety and depression symptoms (N = 123,768)
| Characteristics | Anxiety symptoms | Depression symptoms | ||
|---|---|---|---|---|
| No. (%) [95% CI] | Crude OR (95% CI) | No. (%) [95% CI] | Crude OR (95% CI) | |
| Total | 4196 (3.4) [3.3–3.5] | 28,266(22.8) [22.6–23.1] | ||
| Epidemic-related factors | ||||
| Cumulative number of confirmed cases in the provinces | ||||
| 1–499 | 735 (2.7) [2.5–2.9] | 1 [Reference] | 4401 (16.4) [15.9–16.8] | 1 [Reference] |
| 500–999 | 2868 (3.4) [3.3–3.5] | 1.25 (1.15–1.36) | 20,152 (23.9) [23.6–24.2] | 1.60 (1.55–1.66) |
| 1000–9999 | 120 (4.4) [3.7–5.2] | 1.65 (1.36–2.01) | 777 (28.8) [27.1–30.5] | 2.06 (1.89–2.25) |
| ≥10,000 | 473 (4.8) [4.3–5.2] | 1.78 (1.58–2.00) | 2936 (29.6) [28.7–30.5] | 2.14 (2.03–2.26) |
| Have infected cases in the community or not | ||||
| No case | 1859 (2.2) [2.1–2.3] | 1 [Reference] | 16,040 (19.4) [19.1–19.6] | 1 [Reference] |
| Suspected cases | 240 (8.4) [7.4–9.4] | 3.99 (3.47–4.59) | 823 (28.8) [27.1–30.4] | 1.68 (1.55–1.83) |
| Confirmed cases | 268 (10.2) [9.0–11.3] | 4.94 (4.32–5.65) | 851 (32.3) [30.5–34.1] | 1.99 (1.83–2.16) |
| Not clear | 1829 (5.2) [4.9–5.4] | 2.37 (2.22–2.54) | 10,552 (29.8) [29.3–30.3] | 1.77 (1.72–1.82) |
| Have infected relatives or not | ||||
| No case | 3313 (2.8) [2.7–2.9] | 1 [Reference] | 24,613 (21.1) [20.8–21.3] | 1 [Reference] |
| Suspected cases | 35 (18.4) [12.9–24.0] | 7.74 (5.35–11.18) | 87 (45.8) [38.6–52.9] | 3.17 (2.38–4.21) |
| Confirmed cases | 18 (13.6) [7.7–19.6] | 5.41 (3.29–8.91) | 71 (53.8) [45.2–62.4] | 4.36 (3.10–6.14) |
| Not clear | 830 (12.6) [11.8–13.4] | 4.92 (4.54–5.33) | 3495 (52.9) [51.7–54.1] | 4.20 (4.00–4.42) |
| Have infected friends or not | ||||
| No case | 2285 (2.4) [2.3–2.5] | 1 [Reference] | 19,428 (20.7) [20.4–20.9] | 1 [Reference] |
| Suspected cases | 69 (20.9) [16.5–25.3] | 10.62 (8.12–13.89) | 146 (44.2) [38.9–49.6] | 3.05 (2.45–3.79) |
| Confirmed cases | 23 (15.0) [9.3–20.8] | 7.10 (4.55–11.09) | 82 (53.6) [45.6–61.6] | 4.44 (3.23–6.10) |
| Not clear | 1819 (6.2) [5.9–6.5] | 2.66 (2.50–2.84) | 8610 (29.4) [28.9–30.0] | 1.60 (1.56–1.65) |
| Have passed by, traveled to, or lived in Hubei province in the last two weeks | ||||
| None | 3757 (3.4) [3.3–3.5] | 1 [Reference] | 25,769 (23.1) [22.9–23.3] | 1 [Reference] |
| Have passed by Hubei province | 101 (5.7) [4.6–6.8] | 1.73 (1.42–2.13) | 222 (36.9) [33.1–40.8] | 0.83 (0.73–0.93) |
| Have traveled to Hubei province | 11 (8.9) [3.8–14.1] | 2.82 (1.52–5.24) | 243 (29.1) [26.0–32.2] | 1.31 (0.89–1.95) |
| Have lived in Hubei provincea | 327 (3.1) [2.8–3.5] | 0.93 (0.83–1.05) | 2032 (18.8) [18.1–19.6] | 0.78 (0.74–0.82) |
| Major demographic factorsb | ||||
| Health status | ||||
| Very healthy | 2029 (2.2) [2.1–2.3] | 1 [Reference] | 19,858 (21.5) [21.2–21.8] | 1 [Reference] |
| Well | 1674 (5.8) [5.5–6.1] | 2.75 (2.6–2.93) | 7279 (25.2) [24.7–25.7] | 1.23 (1.20–1.27) |
| General or poor | 493 (19.4) [17.9–20.9] | 10.73 (9.63–11.95) | 1129 (44.4) [42.5–46.4] | 2.92 (2.70–3.17) |
| Alcohol consumption | ||||
| Hardly ever | 3502 (3.1) [3.0–3.2] | 1 [Reference] | 24,504 (21.9) [21.7–22.2] | 1 [Reference] |
| Sometimes | 573 (5.2) [4.8–5.6] | 1.69 (1.55–1.85) | 3241 (29.4) [28.5–30.2] | 1.48 (1.42–1.55) |
| Always | 121 (11.9) [9.9–13.9] | 4.16 (3.43–5.05) | 521 (51.1) [48.1–54.2] | 3.72 (3.29–4.21) |
| Education levels, Years | ||||
| ≤6 Years | 90 (8.5) [6.8–10.1] | 1 [Reference] | 435 (40.8) [37.9–43.8] | 1 [Reference] |
| 7–9 Years | 1209 (3.4) [3.2–3.6] | 0.38 (0.30–0.48) | 10,260 (28.8) [28.3–29.2] | 0.59 (0.52–0.66) |
| 10–12 Years | 1471 (3.0) [2.9–3.2] | 0.34 (0.27–0.42) | 11,315 (23.3) [22.9–23.7] | 0.44 (0.39–0.50) |
| ≥13Years | 1426 (3.7) [3.5–3.9] | 0.42 (0.33–0.52) | 6256 (16.2) [15.9–16.6] | 0.28 (0.25–0.32) |
| Positions | ||||
| General worker | 3348 (3.5) [3.4–3.7] | 1 [Reference] | 23,426 (24.8) [24.5–25.1] | 1 [Reference] |
| Line supervisor | 205 (2.7) [2.4–3.1] | 0.77 (0.67–0.89) | 1746 (23.4) [22.5–24.4] | 0.93 (0.88–0.98) |
| Group leader | 157 (2.6) [2.2–3.0] | 0.73 (0.62–0.86) | 1042 (17.3) [16.4–18.3] | 0.64 (0.50–0.68) |
| Manager | 486 (3.1) [2.8–3.3] | 0.87 (0.79–0.95) | 2052 (13.0) [12.5–13.5] | 0.45 (0.43–0.48) |
| Residence | ||||
| Rural | 2091 (3.8) [3.6–3.9] | 1 [Reference] | 13,432 (24.3) [23.9–24.7] | 1 [Reference] |
| Urban | 2105 (3.1) [2.9–3.2] | 0.81 (0.76–0.88) | 14,834 (21.7) [21.3–22.0] | 0.82 (0.84–0.88) |
CI, confidence interval; OR, odds ratio.
In general, the people who have lived in Hubei for the past two weeks were almost native of Hubei province.
For demographic factors, only the top five are shown according to their positive influence on the risk of anxiety and depression symptoms.
Associations of demographic characteristics with anxiety and depression symptoms are shown in Table 2 and Table S2. Of note, health status and alcohol consumption were the most dominant factors influencing the risk of anxiety and depression symptoms.
3.3. Multivariable analysis: association of epidemic-related factors and major demographic factors with anxiety and depression symptoms
After adjusting for the demographic covariates, the epidemic-related factors with the highest to lowest risk of anxiety symptoms ranked as follows: having infected cases in the community, having infected friends, having infected relatives, and the increased cumulative number of infected cases in the provinces, and having passed by, traveled to, or lived in Hubei province in the last two weeks. The most dominant factors influencing the risk of depression symptoms were having infected relatives and infected friends (Table 3 ). For instance, compared with respondents with no infected friends, the adjusted odds ratios were 2.72 (95% CI, 1.96–3.78) for anxiety symptoms and 1.60 (95% CI, 1.25–2.05) for depression symptoms in those with suspected friends, and 1.93 (95% CI, 1.12–3.32) for anxiety symptoms and 2.44 (95% CI, 1.69–3.52) for depression symptoms in those with confirmed friends. Interestingly, the prevalence of anxiety (OR, 0.80; 95% CI, 0.70–0.90) and depression (OR, 0.81; 95% CI, 0.76–0.85) symptoms were significantly lower among respondents who recently lived in Hubei province compared with those who lived in other provinces or regions.
Table 3.
Multivariable analysis: association of epidemic-related factors and major demographic factors with anxiety and depression symptoms (N = 123,768).
| Characteristics | Anxiety symptoms | Depression Symptoms | ||
|---|---|---|---|---|
| No. | Adjusted OR (95% CI) | No. | Adjusted OR (95% CI) | |
| Total | 4196 | 28,266 | ||
| Epidemic-related factors | ||||
| Cumulative number of confirmed cases in the provinces | ||||
| 1–499 | 735 | 1 [Reference] | 4401 | 1 [Reference] |
| 500–999 | 2868 | 1.21 (1.10–1.32) | 20,152 | 1.44 (1.38–1.50) |
| 1000–9999 | 120 | 1.49 (1.20–1.86) | 777 | 1.68 (1.51–1.84) |
| ≥10,000 | 473 | 1.83 (1.58–2.11) | 2936 | 1.78 (1.67–1.90) |
| Have infected cases in the community or not | ||||
| No case | 1859 | 1 [Reference] | 16,040 | 1 [Reference] |
| Suspected cases | 240 | 2.01 (1.72–2.35) | 823 | 1.29 (1.18–1.41) |
| Confirmed cases | 268 | 2.75 (2.37–3.19) | 851 | 1.67 (1.53–1.83) |
| Not clear | 1829 | 1.50 (1.39–1.63) | 10 552 | 1.31 (1.27–1.36) |
| Have infected relatives or not | ||||
| No case | 3313 | 1 [Reference] | 24,613 | 1 [Reference] |
| Suspected cases | 35 | 1.70 (1.09–2.64) | 87 | 1.79 (1.30–2.47) |
| Confirmed cases | 18 | 1.67 (0.92–3.04) | 71 | 2.24(1.52–3.29) |
| Not clear | 830 | 2.37 (2.14–2.61) | 3495 | 2.99 (2.82–3.17) |
| Have infected friends or not | ||||
| No case | 2285 | 1 [Reference] | 19,428 | 1 [Reference] |
| Suspected cases | 69 | 2.72 (1.96–3.78) | 146 | 1.60 (1.25–2.05) |
| Confirmed cases | 23 | 1.93 (1.12–3.32) | 82 | 2.44 (1.69–3.52) |
| Not clear | 1819 | 1.13 (1.21–1.42) | 8610 | 1.02 (0.98–1.06) |
| Have passed by, traveled to, or lived in Hubei province in the last two weeks | ||||
| None | 3757 | 1 [Reference] | 25,769 | 1 [Reference] |
| Have passed by Hubei province | 101 | 1.04 (0.83–1.29) | 222 | 0.71 (0.63–0.81) |
| Have traveled to Hubei province | 11 | 1.66 (0.83–3.30) | 243 | 1.22 (0.79–1.89) |
| Have lived in Hubei provincea | 327 | 0.80 (0.70–0.90) | 2032 | 0.81 (0.76–0.85) |
| Major demographic factorsb | ||||
| Health status | ||||
| Very healthy | 2029 | 1 [Reference] | 19,858 | 1 [Reference] |
| Well | 1674 | 2.33 (2.17–2.49) | 7279 | 1.17 (1.13–1.21) |
| General or poor | 493 | 6.34 (5.64–7.13) | 1129 | 2.15 (1.98–2.35) |
| Alcohol consumption | ||||
| Hardly ever | 3502 | 1 [Reference] | 24,504 | 1 [Reference] |
| Sometimes | 573 | 1.60 (1.45–1.77) | 3241 | 1.41 (1.35–1.48) |
| Always | 121 | 3.02 (2.44–3.75) | 521 | 3.05 (2.67–3.49) |
| Education levels, years | ||||
| ≤6 Years | 90 | 1 [Reference] | 435 | 1 [Reference] |
| 7–9 Years | 1209 | 0.43 (0.34–0.54) | 10,260 | 0.62 (0.54–0.71) |
| 10–12 Years | 1471 | 0.39 (0.31–0.50) | 11,315 | 0.47 (0.41–0.53) |
| ≥13Years | 1426 | 0.54 (0.42–0.68) | 6256 | 0.35 (0.30–0.40) |
| Positions | ||||
| General worker | 3348 | 1 [Reference] | 23,426 | 1 [Reference] |
| Line supervisor | 205 | 0.82 (0.71–0.95) | 1746 | 0.99 (0.93–1.05) |
| Group leader | 157 | 0.74 (0.62–0.89) | 1042 | 0.89 (0.82–0.96) |
| Manager | 486 | 0.87 (0.77–0.97) | 2052 | 0.75 (0.71–0.79) |
| Residence | ||||
| Rural | 2091 | 1 [Reference] | 13,432 | 1 [Reference] |
| Urban | 2105 | 0.84 (0.78–0.90) | 14,834 | 0.87 (0.84–0.89) |
CI, confidence interval; OR, odds ratio.
Adjusted covariates included sex, age groups, education levels, residence, marital status, health status, smoking status, alcohol consumption, position, and seniority.
In general, the people who have lived in Hubei for the last two weeks were almost native of Hubei province.
For demographic factors, only the top five are shown according to the positive influence on the risk of anxiety and depression symptoms.
Association of demographic characteristics with anxiety and depression symptoms was shown in Table 3 and Table S3. Of note, health status and alcohol consumption were remained the dominant factors influencing the risk of anxiety and depression symptoms. Respondents with general or poor health status were more likely to have anxiety (OR, 6.34; 95% CI, 5.64–7.13) and depression (OR, 2.15; 95% CI, 1.98–2.35) symptoms. The prevalence of anxiety and depression symptoms among respondents who always drank alcohol was almost triple that of those who hardly ever drank alcohol.
3.4. The demands for psychological education and interventions
As shown in Table 4 , the prevalence of respondents reporting a demand for psychological education (overall rate: 67.3%) was higher in those with anxiety (78.4% vs 66.9%) and depression symptoms (69.0% vs 66.7%) than in those without. For all respondents, the most needed psychological knowledge was the common symptom of COVID-19, followed by the methods to alleviate the epidemic's psychological effects.
Table 4.
The demands for psychological education and interventions according to anxiety and depression symptoms.
| Total, No. (%) (N = 123,768) | Anxiety symptoms, No. (%) | Depression symptoms, No. (%) | |||||
|---|---|---|---|---|---|---|---|
| No | Yes | P Value | No | Yes | P Value | ||
| Demand for psychological education | <0.001 | <0.001 | |||||
| Yes | 83,251 (67.3) | 79,962 (66.9) | 3289 (78.4) | 63,742 (66.7) | 19,509 (69.0) | ||
| No | 40,517 (32.7) | 39,610 (33.1) | 907 (21.6) | 31,760 (33.3) | 8757 (31.0) | ||
| Knowledge for psychological educationa | <0.001 | <0.001 | |||||
| The common symptom of COVID-19 | 74,601 (41.4) | 71,937 (41.5) | 2667 (36.9) | 58,294 (42.0) | 16,307 (39.2) | ||
| Ways to alleviate the psychological effects | 54,384 (30.1) | 51,946 (30.0) | 2438 (33.7) | 41,162 (29.7) | 13,222 (31.8) | ||
| Ways to seek professional psychological help | 49,751 (27.6) | 47,700 (27.5) | 2051 (28.4) | 38,155 (27.5) | 11,596 (27.9) | ||
| Others | 1661 (0.9) | 1586(0.9) | 75 (1.0) | 1153 (0.8) | 508 (1.2) | ||
| Demand for psychological Interventions | <0.001 | <0.001 | |||||
| Very | 3763 (3.0) | 3200 (2.7) | 563 (13.4) | 1617 (1.7) | 2146 (7.6) | ||
| Moderate | 8232 (6.7) | 7371 (6.2) | 861 (20.5) | 5083 (5.3) | 3149 (11.1) | ||
| A little | 21,120 (17.1) | 19,881 (16.6) | 1239 (29.5) | 15,613 (16.3) | 5507 (19.5) | ||
| No | 90,653 (73.2) | 89,120 (74.5) | 1533 (36.5) | 73,189 (76.6) | 17,464 (61.8) | ||
| Psychological interventionsa | <0.001 | ||||||
| Counselling | 19,289(19.9) | 17,563 (19.7) | 1726 (22.3) | 12,500 (19.1) | 6789 (21.6) | ||
| Promotion of mental health knowledge | 23,149 (23.9) | 21,599 (24.3) | 1550 (20.1) | 16,574 (25.4) | 6575 (20.9) | ||
| Mental health training course | 20,299 (21.0) | 18,783 (21.1) | 1516 (19.6) | 13,964 (21.4) | 6335 (20.1) | <0.001 | |
| Psychological assessment | 16,031(16.6) | 14,580 (16.4) | 1451 (18.8) | 10,736 (16.4) | 5295 (16.8) | ||
| Group building and other development activities | 11,071(11.4) | 10,210 (11.5) | 861 (11.1) | 7332 (11.2) | 3739 (11.9) | ||
| Psychological salon | 6299(6.5) | 5728 (6.4) | 571 (7.4) | 3874 (5.9) | 2425 (7.7) | ||
| Others | 605(0.6) | 550 (0.6) | 55 (0.7) | 304 (0.5) | 301 (1.0) | ||
| Intervention perioda | <0.001 | <0.001 | |||||
| Morning meeting | 18,574(29.6) | 17,163 (29.8) | 1411 (28.4) | 12,587 (30.3) | 5987 (28.4) | ||
| After work | 15,653(25.0) | 14,516 (25.2) | 1137 (22.9) | 10,738 (25.8) | 4915 (23.3) | ||
| At weekend | 12,750(20.3) | 11,752 (20.4) | 988 (19.9) | 8576 (20.6) | 4174 (19.8) | ||
| Lunchtime | 7660(12.2) | 6936 (12.0) | 724 (14.6) | 4679 (11.3) | 2981 (14.1) | ||
| Dinner time | 7316(11.7) | 6663 (11.6) | 653 (13.1) | 4577 (11.0) | 2739 (13.0) | ||
| Others | 703(1.1) | 644 (1.1) | 59 (1.2) | 428 (1.0) | 275 (1.3) | ||
Psychological knowledge, psychological interventions, and intervention period were ranked according to the demand of respondents with anxiety and depression symptoms, respectively.
COVID-19, Coronavirus disease 2019.
The prevalence of respondents reporting a demand of psychological interventions (overall rate: 26.8%) was higher in those with anxiety (63.5% vs 25.5%) and depression symptoms (38.2% vs 23.4%) than in those without. For respondents with anxiety or depression symptoms, the most needed psychological intervention was counselling, followed by promotion of mental health knowledge. Morning meeting followed by the period after work were the two most desired time to receive psychological interventions. Interestingly, the prevalence of respondents who lived in Hubei province reporting the demands of psychological knowledge (63.9% vs. 67.6%) and interventions (22.8% vs. 27.1%) was slightly below that of those who lived in the other provinces or regions (Table S4).
4. Discussion
The aim of the present study was to investigate the prevalence and the related factors of anxiety and depression symptoms, and the demands for psychological education and interventions among workers during the epidemic period of COVID-19 in China. Approximately 3.4% and 22.8% of respondents exhibited symptoms of anxiety and depression, respectively. We also revealed the urgent demands for psychological education (67.3%) and interventions (26.8%) among workers. Moreover, after adjustment for the demographic covariates, epidemic-related factors especially having confirmed cases in the community and having confirmed friends were found to be significantly associated with the higher risk of anxiety and depression symptoms, respectively, but traditional risk factors such as health status and alcohol consumption remained the dominant factors. Interestingly, respondents who recently lived in Hubei province were more likely to report a lower risk of anxiety and depression symptoms, and slightly lower demands for psychological education and interventions.
Compared with previous studies performed on the general population in China before the outbreak, the prevalence of anxiety symptoms in this study was not significantly different, while the prevalence of depression symptoms was roughly 4–5 times or higher (Huang et al., 2019; Phillips et al., 2009). The prevalence of anxiety symptoms in the present study was lower than previous studies on the general population which reported 28.8% – 35.1%. The prevalence of depression symptoms in the present study from February 2, 2020 to February 7, 2020 was consistent with the results of an epidemiological study that was conducted in early February 2020 among the general population in China, which indicated that the overall prevalence of depressive symptoms was 20.1% (Huang and Zhao, 2020). An earlier survey that was performed in late January 2020 found that 16.5% respondents reported moderate to severe depressive symptom (Wang et al., 2020). Another later survey that was performed in early March 2020 reported that 27.9% of respondents had depression symptoms (Shi et al., 2020). These findings indicated that depression symptoms occurred among the workers during the epidemic period of COVID-19 in China and highlighted the importance of preventing and treating mental health problems of workers. The present study was conducted from February 2, 2020 to February 7, 2020, when these workers suspended their work because of the publication of the policy for postponing the resumption of work (General Office of the State Council, Jan 27, 2020). Soon afterwards they came back to work on February 10, 2020. Therefore, health authorities and factories should pay more attention on the psychological health of workers for improving mental health in workers after returning to work, which potentially improves productivity.
This study demonstrated a statistically significant association between epidemic-related exposure and a higher risk of anxiety and depression symptoms. Nevertheless, our findings further indicated that major traditional risk factors, such as physical health and alcohol consumption, were still the dominant factors influencing the risk of anxiety and depression symptoms, which was also reported in the previous studies. A study on 3031 migrant workers from 10 manufacturing factories in Shenzhen, China, showed that respondents with physical illness in the past two weeks were more likely to report poor mental health (OR, 1.72; 95% CI,1.43–2.05) (Zhong et al., 2018). Another study demonstrated that consuming an average of seven or more alcoholic drinks per day significantly increased the risk of depression compared with consuming an average of one or two alcoholic drinks (OR, 2.21; 95%%CI, 1.02–4.40) (Almeida et al., 2014). However, the association between alcohol consumption and mental health status might also be explained by “reverse causality”, in which increased motivation of frequently drinking would occur in the anxiety and depression symptoms (Cyders and Smith, 2008; Dir et al., 2013).
This study revealed an urgent need for psychological knowledge and interventions among workers. Of note, we found that respondents with anxiety symptoms were more likely to report the demands of psychological interventions (63.5% vs 25.5%), suggesting that health authorities and factories should pay more attention to those populations. Moreover, our findings also have several important, immediate implications for health authorities and factories. First, our findings suggested that the common symptom of COVID-19 was the most needed psychological knowledge. Second, counseling and promotion of mental health knowledge ranked as the top two demands for psychological interventions. Third, morning meeting followed by the period after work were the two most desired time to receive psychological interventions. In summary, we have identified the most desired psychological knowledge, interventions, and times to receive them, which could help health authorities to formulate targeted policies for workers to improve their mental health status.
Interestingly, we found that respondents who recently lived in Hubei province (the hardest–hit province of the COVID-19 epidemic) had a lower risk of anxiety and depression symptoms, and slightly lower demands for psychological education and interventions during the epidemic period of COVID-19. The reason for this finding may be family support (Bhugra and van Ommeren, 2006). People in Hubei province delayed returning to work due to the epidemic, and they were advised to avoid going to public places. Therefore, family members were likely to spend more time together with each other.
To our knowledge, the present study is the largest cross-sectional study to investigate the prevalence of anxiety and depression symptoms, as well as associations with epidemic-related factors during the epidemic period of COVID-19 in China. The present study not only revealed the mental health status of workers during the epidemic period of COVID-19, but also provided a reference for the mental health of workers in labor–intensive factories in China. The strengths of our study include the large sample size from various provinces or regions across the country, special population groups, a short-cycle survey, and careful measurement of epidemic-related factors and demographic covariates.
Nevertheless, several limitations of this study should be taken into account when interpreting the results. First, due to the urgency of the time and the limitation of current resources, it is not possible to carry out sampling surveys in all provinces of the country. However, the 123,768 respondents completing the questionnaire covered almost all provinces and regions in China, and some subjects from overseas, which improved the representativeness of the population and reduced the possibility of sampling error. Second, data were collected online via the Chinese survey website Wenjuanxing. There are cases whose questionnaires were filled out by others instead of by the respondents themselves. To reduce the error caused by this causes, we excluded questionnaires with the same IP address. Third, the measurement methods for anxiety and depression symptoms as well as demographic covariates, and epidemic-related factors relied on self–reporting, and therefore raised the possibility of common method bias. Finally, the present study used Zung's Self-Rating scales method. The results of anxiety and depression might lack comparability with clinical diagnostic measurements of anxiety and depression.
5. Conclusions
In conclusion, our survey found a relatively low prevalence of anxiety symptoms, a relatively high prevalence of depression symptoms, and the urgent demands for psychological knowledge and interventions among Chinese workers. Epidemic-related factors were significantly associated with the higher risk of anxiety and depression symptoms, but traditional risk factors, such as health status and alcohol consumption, were still the dominant factors. In addition, we also identified the most desired psychological knowledge, interventions, and times to receive them, which could help health authorities and factories to formulate targeted policies to increase workers’ adherence to knowledge and interventions, and thus improve workers’ mental health status.
Funding
This study was funded by Guangdong Province Universities and Colleges Pearl River Scholar Funded Scheme (2019), the Zhejiang University special scientific research fund for COVID-19 prevention and control (grant number K920330111), and the Construction of High-level University of Guangdong (grant numbers G820332010, G618339167 and G618339164).
Declaration of Competing Interests
All the authors declare no conflicts of interest.
CRediT authorship contribution statement
Xi-Ru Zhang: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Qing-Mei Huang: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Xiao-Meng Wang: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Xin Cheng: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Zhi-Hao Li: Software, Writing - review & editing. Zheng-He Wang: Software, Writing - review & editing. Wen-Fang Zhong: Software, Writing - review & editing. Dan Liu: Software, Writing - review & editing. Dong Shen: Software, Writing - review & editing. Pei-Liang Chen: Software, Writing - review & editing. Wei-Qi Song: Software, Writing - review & editing. Xian-Bo Wu: . Xingfen Yang: Conceptualization, Data curation, Project administration, Funding acquisition, Supervision. Chen Mao: Conceptualization, Data curation, Project administration, Funding acquisition, Supervision.
Acknowledgments
We are grateful to Teri Surprenant (affiliation: ACCDON; E-mail: t.surprenant@accdon.com) for polishing the English language and the employees of the mega-size factory in Shenzhen, Guangdong, China.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2020.08.041.
Appendix. Supplementary materials
References
- Almeida O.P., Hankey G.J., Yeap B.B., Golledge J., Flicker L. The triangular association of ADH1B genetic polymorphism, alcohol consumption and the risk of depression in older men. Mol. Psychiatry. 2014;19(9):995–1000. doi: 10.1038/mp.2013.117. [DOI] [PubMed] [Google Scholar]
- Betancourt T.S., Brennan R.T., Vinck P., VanderWeele T.J., Spencer–Walters D., Jeong J.…Pham Associations between mental health and ebola-related health behaviors: a regionally representative cross–sectional survey in post–conflict Sierra Leone. PLoS Med. 2016;13(8) doi: 10.1371/journal.pmed.1002073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhugra D., van Ommeren M. Mental health, psychosocial support and the tsunami. Int. Rev. Psychiatry. 2006;18(3):213–216. doi: 10.1080/09540260600655839. [DOI] [PubMed] [Google Scholar]
- Cyders M.A., Smith G.T. Emotion–based dispositions to rash action: positive and negative urgency. Psychol. Bull. 2008;134(6):807–828. doi: 10.1037/a0013341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dir A.L., Karyadi K., Cyders M.A. The uniqueness of negative urgency as a common risk factor for self–harm behaviors, alcohol consumption, and eating problems. Addict. Behav. 2013;38(5):2158–2162. doi: 10.1016/j.addbeh.2013.01.025. [DOI] [PubMed] [Google Scholar]
- General Office of the State Council. (Jan 27, 2020). Notice of the general office of the state council on the extension of the spring festival holiday in 2020. http://www.gov.cn/zhengce/content/2020–01/27/content_5472352.htm. (accessed Jan 27, 2020).
- Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H.…Pillai S.K. First Case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Wang Y., Wang H., Liu Z., Yu X., Yan J., …, Wu Y. Prevalence of mental disorders in China: a cross–sectional epidemiological study. Lancet Psychiatry. 2019;6(3):211–224. doi: 10.1016/S2215-0366(18)30511-X. [DOI] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web–based cross–sectional survey. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui D.S., E I.A., Madani T.A., Ntoumi F., Kock R., Dar O., …, Petersen E. The continuing 2019–nCoV epidemic threat of novel coronaviruses to global health – The latest 2019 novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly J.D., Hoff N.A., Spencer D., Musene K., Bramble M.S., McIlwain D.…Rimoin A.W. Neurological, cognitive, and psychological findings among survivors of ebola virus disease from the 1995 ebola outbreak in Kikwit, democratic republic of Congo: a cross–sectional study. Clin. Infect. Dis. 2019;68(8):1388–1393. doi: 10.1093/cid/ciy677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau J.T., Yang X., Tsui H.Y., Pang E., Wing Y.K. Positive mental health-related impacts of the SARS epidemic on the general public in Hong Kong and their associations with other negative impacts. J. Infect. 2006;53(2):114–124. doi: 10.1016/j.jinf.2005.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung G.M., Ho L.M., Chan S.K., Ho S.Y., Bacon–Shone J., Choy R.Y.…Fielding R. Longitudinal assessment of community psychobehavioral responses during and after the 2003 outbreak of severe acute respiratory syndrome in Hong Kong. Clin. Infect. Dis. 2005;40(12):1713–1720. doi: 10.1086/429923. [DOI] [PubMed] [Google Scholar]
- Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J. Med. Virol. 2020;92(4):401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y.F., Li W., Deng H.B., Wang L., Wang Y., Wang P.H., …, Xiang Y.T. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J. Affect. Disord. 2020;275:145–148. doi: 10.1016/j.jad.2020.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammed A., Sheikh T.L., Poggensee G., Nguku P., Olayinka A., Ohuabunwo C., Eaton J. Mental health in emergency response: lessons from Ebola. Lancet Psychiatry. 2015;2(11):955–957. doi: 10.1016/S2215-0366(15)00451-4. [DOI] [PubMed] [Google Scholar]
- National Health Commission of China. (Jan 26, 2020). Guiding principles for emergency psychological crisis intervention for pneumonia epidemic of new coronavirus infection. http://www.gov.cn/zhengce/zhengceku/2020–01/27/content_5472433.htm. (accessed January 27, 2020).
- Nie X.D., Wang Q., Wang M.N., Zhao S., Liu L., Zhu Y.L., Chen H. Anxiety and depression and its correlates in patients with coronavirus disease 2019 in Wuhan. Int. J. Psychiatry Clin. Pract. 2020:1–6. doi: 10.1080/13651501.2020.1791345. [DOI] [PubMed] [Google Scholar]
- Phan L.T., Nguyen T.V., Luong Q.C., Nguyen T.V., Nguyen H.T., Le H.Q.…Pham Q. Importation and human–to–human transmission of a novel coronavirus in Vietnam. N. Engl. J. Med. 2020;382(9):872–874. doi: 10.1056/NEJMc2001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips M.R., Zhang J., Shi Q., Song Z., Ding Z., Pang S., …, Wang Z. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001–05: an epidemiological survey. Lancet. 2009;373(9680):2041–2053. doi: 10.1016/S0140-6736(09)60660-7. [DOI] [PubMed] [Google Scholar]
- Reardon S. Ebola's mental–health wounds linger in Africa. Nature. 2015;519(7541):13–14. doi: 10.1038/519013a. [DOI] [PubMed] [Google Scholar]
- Shi L., Lu Z.A., Que J.Y., Huang X.L., Liu L., Ran M.S.…Lu L. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw. Open. 2020;3(7) doi: 10.1001/jamanetworkopen.2020.14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shultz J.M., Baingana F., Neria Y. The 2014 Ebola outbreak and mental health: current status and recommended response. JAMA. 2015;313(6):567–568. doi: 10.1001/jama.2014.17934. [DOI] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (covid-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Huang D., Huang H., Zhang J., Guo L., Liu Y., …, Geng Q. The psychological impact of COVID-19 pandemic on medical staff in Guangdong, China: a cross–sectional study. Psychol Med, 2020:1–9. doi: 10.1017/S0033291720002561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. (February 9, 2020). Novel coronavirus (2019–nCoV): situation report–20. https://www.who.int/docs/default–source/coronaviruse/situation–reports/20200209–sitrep–20–ncov.pdf?sfvrsn=6f80d1b9_4. (accessed February 10, 2020).
- WHO. (Jan 30, 2020). WHO director–general's statement on ihr emergency committee on novel coronavirus (2019–nCoV). https://www.who.int/dg/speeches/detail/who–director–general–s–statement–on–ihr–emergency–committee–on–novel–coronavirus–(2019–ncov). (accessed Jan 31, 2020).
- Xiao X., Zhu X., Fu S., Hu Y., Li X., Xiao J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: A multi–center cross–sectional survey investigation. J. Affect. Disord. 2020;274:405–410. doi: 10.1016/j.jad.2020.05.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong B.L., Liu T.B., Chan S.S.M., Jin D., Hu C.Y., Dai J., Chiu H.F.K. Common mental health problems in rural–to–urban migrant workers in Shenzhen, China: prevalence and risk factors. Epidemiol. Psychiatr. Sci. 2018;27(3):256–265. doi: 10.1017/S2045796016001141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zung W.W. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- Zung W.W., Richards C.B., Short M.J. Self-rating depression scale in an outpatient clinic. Further validation of the SDS. Arch. Gen. Psychiatry. 1965;13(6):508–515. doi: 10.1001/archpsyc.1965.01730060026004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.