Abstract
The ongoing pandemic of 2019 novel coronavirus disease (COVID-19) is challenging global public health response system. We aim to identify the risk factors for the transmission of COVID-19 using data on mainland China. We estimated attack rate (AR) at county level. Logistic regression was used to explore the role of transportation in the nationwide spread. Generalized additive model and stratified linear mixed-effects model were developed to identify the effects of multiple meteorological factors on local transmission. The ARs in affected counties ranged from 0.6 to 9750.4 per million persons, with a median of 8.8. The counties being intersected by railways, freeways, national highways or having airports had significantly higher risk for COVID-19 with adjusted odds ratios (ORs) of 1.40 (p = 0.001), 2.07 (p < 0.001), 1.31 (p = 0.04), and 1.70 (p < 0.001), respectively. The higher AR of COVID-19 was significantly associated with lower average temperature, moderate cumulative precipitation and higher wind speed. Significant pairwise interactions were found among above three meteorological factors with higher risk of COVID-19 under low temperature and moderate precipitation. Warm areas can also be in higher risk of the disease with the increasing wind speed. In conclusion, transportation and meteorological factors may play important roles in the transmission of COVID-19 in mainland China, and could be integrated in consideration by public health alarm systems to better prevent the disease.
Keywords: COVID-19, China, Transportation, Meteorological factors, Interaction
1. Introduction
The ongoing outbreak of coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first reported in Wuhan, China in December 2019 (Huang et al., 2020). Just in four months, COVID-19 has spread worldwide at an extremely fast speed. As of August 2, a total of 17.7 million people from over 180 countries have been affected, with a fatality rate around 3.9% (World Health Organization, 2020). Considering of the severe threat posed by the coronavirus, the World Health Organization (WHO) declared the outbreak as a pandemic on March 11, 2020. China has put into place very rigorous prevention and control measures since January, including the lockdown of the 11-million-people city of Wuhan and the restriction of social contact (Tu et al., 2020). The outbreak process of COVID-19 in mainland China mainly occurred in February, and has been well-controlled from March to now with very low incidence, most of which are imported abroad.
Before the lockdown, more than five million people have already left Wuhan by train, bus or plane for Spring Festival holidays, which might lead to rapid spread throughout the country (Collman, 2020). Although transportation has been suggested as a risk for spread of the disease (Du et al., 2020), how the travel-related risk factors influence the nationwide transmission remains to be investigated. Furthermore, multiple meteorological features are known to impact the infectivity of respiratory virus and immunity of the host, leading the different degree of local transmission (Moriyama et al., 2020). Nevertheless, the results about the effect of meteorological factors on SARS-CoV-2 transmission are controversial, making it difficult to refine prevention and control strategies (Sun et al., 2020). A negative effect of temperature on COVID-19 infection was found in Japan (Ujiie et al., 2020). However, other studies came to the opposite conclusion such as that of Jakarta (Tosepu et al., 2020), or no association was found in Spain (Briz-Redón and Serrano-Aroca, 2020). In addition, other studies found an unclear association between temperature and COVID-19 (Kassem, 2020), or an association depending on the temperature range such as that of China (Xie and Zhu, 2020).
In this report, we elaborated the spatiotemporal characteristics of COVID-19 in mainland China, identified the factors contributing to the fast spread and explored the potential interactions of meteorological elements, in order to provide evidence-based guidance for helping other countries fight against the pandemic.
2. Materials and methods
2.1. Data collection and management
We collected data of confirmed COVID-19 cases from the National Notifiable Infectious Disease Information System (until February 27) and the official updates by the national and provincial health commissions from February 28 to March 21, 2020. According to the Guideline for Diagnosis and Treatment of Novel Coronavirus Pneumonia issued by National Health Commission (NHC) (National Health Commission of China, 2020), the confirmed cases were patients who had related epidemiological history and clinical manifestations with one of the following etiological evidences: SARS-CoV-2 nucleic acid detected by specific real-time PCR assay, or viral gene sequence homologous to SARS-CoV-2. The database included demographic information, date of diagnosis and identified location. Meanwhile, we collected the data on the daily reported number of COVID-19 confirmed cases of each county. As this study constituted data analysis rather than research in human beings, ethical approval from institutional review boards was not required.
Travel-related data were gathered as well. Data on railways, freeways, and national highways were collected from the Ministry of Natural Resources of China (http://www.mnr.gov.cn/). Data on locations of airports were collected from Our Airports (https://ourairports.com/countries/CN/). Meteorological data including daily temperature, precipitation, relative humidity, sunshine duration, and wind speed were obtained from China Meteorological Data Sharing Service System (http://data.cma.cn). We measured the distance between Wuhan and the centroid of each affected county in ArcGIS 10.2 software (ESRI Inc., Redlands, CA, USA). The population size of county level was obtained from Chinese Statistic Yearbook (http://www.stats.gov.cn/tjsj/ndsj/), from which population densities were calculated according to the area of each county.
2.2. Statistical analysis
2.2.1. Travel-related factors for nationwide spread
We hypothesized that communication and transportation may play a crucial role in the nationwide spread of COVID-19, especially before the shutdown of Wuhan. Therefore a case-control study design was used to clarify communication and transportation contributing to the nationwide spread of COVID-19. All known affected counties (with cases) were taken as “cases”; all unaffected (without cases) counties were taken as “controls”. Univariate logistic regression was performed to examine the effect of each travel-related factors separately. Multivariate stepwise logistic regression was then conducted by including all significant factors in univariate model, with the adjustment for distance to Wuhan and population density of each county. Odds ratios (ORs) and their 95% confidence intervals (CIs) were estimated.
2.2.2. Meteorological factors for local transmission
After the shutdown of Wuhan city, local transmission became main pattern of dissemination of SARS-CoV-2. We hypothesis that meteorological factors may play important roles in local transmission. The outbreak of COVID-19 in Wuhan started much earlier than other places in mainland China. Considering of the different local transmission pattern of Wuhan, we used the affected counties except counties in Wuhan in mainland China to explore the factors on local transmission. We used Kriging interpolation and zonal statistic method to calculate the average temperature, temperature difference, relative humidity, sunshine duration, wind speed and cumulative precipitation in each affected county in February. Considering the incubation period (Linton et al., 2020) and time from onset to report (Xu, X.W. et al., 2020), log-transformed attack rate (AR) as of March 21 was taken as the dependent variable. Spearman correlation and a bottom-up strategy with Akaike information criterion (AIC) were used for model selection. A generalized additive model (GAM) with a Gaussian distribution was developed to estimate the effects of meteorological factors on spread of COVID-19 (Wood, 2004). Penalized thin plate regression splines were used for smooth function and representation of the non-linear effects of climate factors. The interactions of meteorological factors were then evaluated using GAM (Text S1). Based on the results of GAM, we modelled log-transformed AR with stratified linear mixed-effects model (LMM) to quantify the impacts of meteorological factors, in which fixed effects were used for meteorological factors, distance to Wuhan and population density; differences between provinces were the random effects (Lindstrom and Bates, 1988). All above statistical analyses were performed in R software (3.6.1). A two-sided p value less than 0.05 was considered to be statistically significant.
3. Results
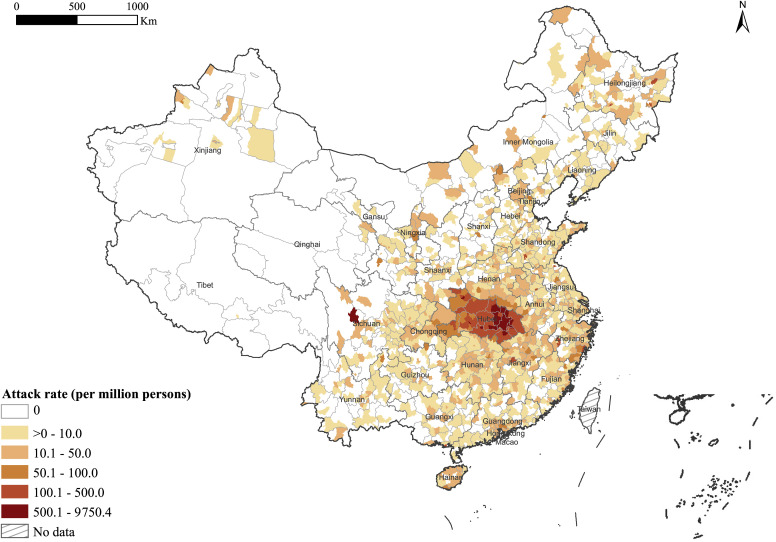
A total of 81,054 COVID-19 cases, which have affected 1668 counties in all 31 provinces of mainland China, were reported as of March 21, 2020. The ARs in affected counties ranged from 0.6 to 9750.4 per million persons (Fig. 1 ), with a median of 8.8 (interquartile range 4.0–20.3). The epicentre Wuhan city as a whole had an AR of 5058.8 per million persons. To investigate the role of transportation in extension of the outbreak, we displayed main transportation lines on the map of mainland China. By comparison with the thematic map of AR (Fig. 1), we observed the affected counties were more likely being crossed by a railway, freeway, national highway, or having airports (Fig. S1).
Fig. 1.
Spatial overview of the epidemic magnitude of COVID-19 in each affected county in mainland China.
To quantitatively evaluate the effects of transportation on the nationwide spread of COVID-19, we conducted a “case-control” study. The univariate logistic analyses found that the counties being intersected by a railway, freeway, national highway or having airports had significantly higher risk for the presence of COVID-19 than other counties. Then the multivariate logistic regression revealed that intersection with a railway, freeway, national highway and having airports remained significant risk factors even after adjusting for population density and distance to Wuhan, with adjusted ORs of 1.40 (95% CI 1.14–1.72; p = 0.001), 2.07 (95% CI 1.61–2.67; p < 0.001), 1.31 (95% CI 1.02–1.68; p = 0.04), and 1.70 (95% CI 1.31–2.22; p < 0.001), respectively (Table 1 ).
Table 1.
Travel-related factors contributing to the nationwide spread of COVID-19 in mainland China by logistic regression analyses.
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| Risk factors | OR (95% CI) | p value | Adjusted OR (95% CI) | p value |
| Intersected by railway | ||||
| No | Ref | Ref | Ref | Ref |
| Yes | 2.18 (1.84–2.59) | <0.001* | 1.40 (1.14–1.72) | 0.001* |
| Intersected by freeway | ||||
| No | Ref | Ref | Ref | Ref |
| Yes | 3.72 (3.08–4.49) | <0.001* | 2.07 (1.61–2.67) | <0.001* |
| Intersected by national highway | ||||
| No | Ref | Ref | Ref | Ref |
| Yes | 2.43 (2.01–2.94) | <0.001* | 1.31 (1.02–1.68) | 0.04* |
| Having any airport | ||||
| No | Ref | Ref | Ref | Ref |
| Yes | 1.44 (1.15–1.82) | 0.001* | 1.70 (1.31–2.22) | <0.001* |
| Population density | 1.24 (1.17–1.32) | <0.001* | 1.16 (1.11–1.22) | <0.001* |
| Distance to Wuhan | 0.87 (0.86–0.88) | <0.001* | 0.89 (0.88–0.90) | <0.001* |
Railway, freeway, national highway, airport, population density and distance to Wuhan were included in the multivariate logistic regression, with backward stepwise method for variable selection. A total of 2858 counties were analysed in the model, among which 1668 were affected (“cases”). Population density and distance to Wuhan were continuous variables, with the units of per 1000/km2 and per 100 km increase, respectively. OR = odds ratio, CI = confidence interval, Ref = reference. * statistically significant.
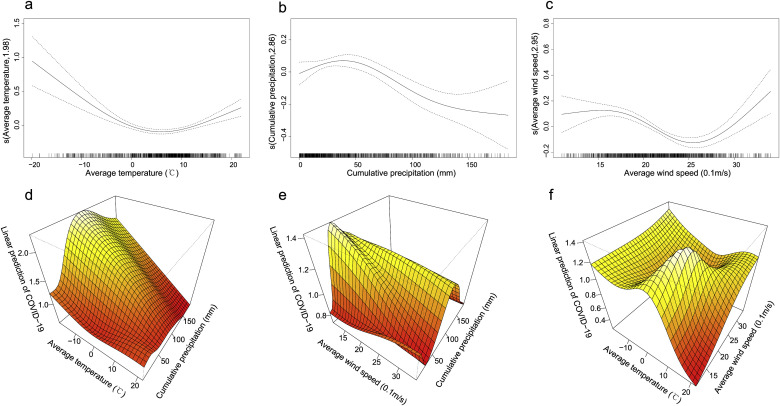
To identify the effects of meteorological variables on the local transmission, we collected and visualized the meteorological factors in China (Fig. S2), and then developed univariate and multivariate GAMs (Text S1). The AIC of every GAM in the process of selection was listed in Table S1 (Table S1). Final model included average temperature, cumulative precipitation and average wind speed, after adjustment for distance to Wuhan and population density (Table S2). The results of GAM revealed that the relationships between meteorological factors and COVID-19 were nonlinear. The risk of COVID-19 decreased with the increasing average temperature when temperature was relatively low (Fig. 2 a). When cumulative precipitation was less than around 50 mm, increasing cumulative precipitation was correlated with higher risk of COVID-19. When cumulative precipitation was over 50 mm, the risk of COVID-19 decreased with increasing cumulative precipitation but the confidence interval is much wider (Fig. 2b). The wind speed had a positive effect on the risk of COVID-19 when the speed was lower than 1.5 m/s or higher than 2.5 m/s, but had a negative effect between 1.5 m/s and 2.5 m/s (Fig. 2c).
Fig. 2.
The relationships of the attack rate of COVID-19 with meteorological factors and pairwise interactions among meteorological factors in mainland China. The relationships between the attack rate of COVID-19 and average temperature (a), cumulative precipitation (b), and average wind speed (c). The solid lines are the logarithmic relative risks of COVID-19, and the dotted lines represent the 95% confidence levels. The three-dimensional diagrams represent the interaction of average temperature with cumulative precipitation (d), the interaction of cumulative precipitation and average wind speed (e), and the interaction of average temperature with average wind speed (f), respectively.
Based on the results above, we explored the potential pairwise interactions of meteorological factors, including average temperature, cumulative precipitation and average wind speed using GAM, and constructed three-dimensional diagrams according to the GAM analysis results (Fig. 2d–f). A higher risk of COVID-19 occurred in the scenario of low average temperature and modest cumulative precipitation between around 50–120 mm (Fig. 2, d + e). Warm areas (temperature over 10 °C) can also be in higher risk of the disease with the increasing wind speed (Fig. 2f).
Given the nonlinear effects suggested by GAM, we classified average temperature, cumulative precipitation and average wind speed into two strata (for average temperature: <10 °C and ≥10 °C; for cumulative precipitation: <50 mm and ≥50 mm; for average wind speed: <2 m/s and ≥2 m/s), and conducted LMM respectively to quantify the effects of meteorological factors on transmission of COVID-19. Higher average temperature had a significant negative effect on risk of COVID-19 overall and when temperature was below 10 °C (Table 2 : model 0, model 1), but the effect was insignificant when temperature was over 10 °C (Table 2: model 2). Increasing cumulative precipitation was associated to increasing risk of COVID-19 when precipitation was lower than <50 mm (Table 2: model 3), yet the correlation became insignificant when precipitation was over 50 mm (Table 2: model 4). Increasing average wind speed was related to higher risk of COVID-19 overall and below 2 m/s (Table 2: model 0, model 5), no significant correlation observed when wind speed was over 2 m/s (Table 2: model 6).
Table 2.
Meteorological factors for the local transmission of COVID-19 in mainland China by linear mixed-effect modelling.
| β (SE) | RR (95% CI) | p value | |
|---|---|---|---|
| Model 0: Non-stratified model | |||
| Average temperature | −0.01 (0.01) | 0.99 (0.98–1.00) | 0.011* |
| Cumulative precipitation | 0.001 (0.001) | 1.00 (1.00–1.00) | 0.052 |
| Average speed wind | 0.01 (0.004) | 1.01 (1.00–1.02) | 0.022* |
| Population density | 0.02 (0.003) | 1.02 (1.01–1.02) | <0.001* |
| Distance to Wuhan | −0.02 (0.01) | 0.98 (0.97 0.99) | 0.002* |
| Model 1: Average temperature <10 °C | |||
| Average temperature | −0.03 (0.01) | 0.97 (0.95–0.98) | <0.001* |
| Cumulative precipitation | 0.01 (0.001) | 1.00 (1.00–1.01) | <0.001* |
| Average speed wind | 0.01 (0.01) | 1.01 (1.00–1.02) | 0.06 |
| Population density | 0.01 (0.003) | 1.01 (1.01–1.02) | <0.001* |
| Distance to Wuhan | −0.04 (0.01) | 0.97 (0.95–0.98) | <0.001* |
| Model 2: Average temperature ≥10 °C | |||
| Average temperature | −0.01 (0.01) | 0.99 (0.96–1.02) | 0.51 |
| Cumulative precipitation | −0.001 (0.001) | 1.00 (1.00–1.00) | 0.38 |
| Average speed wind | 0.02 (0.01) | 1.02 (1.00–1.03) | 0.02* |
| Population density | 0.02 (0.004) | 1.02 (1.01–1.03) | <0.001* |
| Distance to Wuhan | −0.04 (0.02) | 0.96 (0.94–0.99) | 0.02* |
| Model 3: Cumulative precipitation <50 mm | |||
| Average temperature | −0.01 (0.01) | 0.99 (0.98–1.00) | 0.03* |
| Cumulative precipitation | 0.01 (0.002) | 1.01 (1.00–1.01) | <0.001* |
| Average speed wind | 0.002 (0.01) | 1.00 (0.99–1.01) | 0.71 |
| Population density | 0.01 (0.003) | 1.01 (1.01–1.02) | <0.001* |
| Distance to Wuhan | −0.002 (0.01) | 1.00 (0.98–1.01) | 0.83 |
| β (SE) | RR (95% CI) | p value | |
|---|---|---|---|
| Model 4: Cumulative precipitation ≥50 mm | |||
| Average temperature | 0.03 (0.02) | 1.04 (1.00–1.07) | 0.04* |
| Cumulative precipitation | −0.001 (0.001) | 1.00 (1.00–1.00) | 0.42 |
| Average speed wind | 0.02 (0.01) | 1.02 (1.01–1.03) | 0.01* |
| Population density | 0.03 (0.01) | 1.03 (1.02–1.04) | <0.001* |
| Distance to Wuhan | −0.12 (0.02) | 0.89 (0.86–0.92) | <0.001* |
| Model 5: Average speed wind <2 m/s | |||
| Average temperature | −0.03 (0.01) | 0.97 (0.96–0.99) | <0.001* |
| Cumulative precipitation | 0.001 (0.001) | 1.00 (1.00–1.00) | 0.29 |
| Average speed wind | 0.03 (0.01) | 1.03 (1.01–1.04) | 0.003* |
| Population density | 0.02 (0.004) | 1.02 (1.01–1.03) | <0.001* |
| Distance to Wuhan | −0.04 (0.01) | 0.96 (0.94–0.98) | <0.001* |
| Model 6: Average speed wind ≥2 m/s | |||
| Average temperature | −0.002 (0.01) | 1.00 (0.99–1.01) | 0.82 |
| Cumulative precipitation | 0.002 (0.001) | 1.00 (1.00–1.00) | 0.12 |
| Average speed wind | 0.01 (0.01) | 1.01 (0.99–1.02) | 0.44 |
| Population density | 0.01 (0.003) | 1.01 (1.01–1.02) | <0.001* |
| Distance to Wuhan | −0.01 (0.01) | 0.99 (0.97–1.01) | 0.50 |
Average temperature, cumulative precipitation, average speed wind, population density and distance to Wuhan were included in the linear mixed-effects model as fixed effect, with provincial difference as random effect. All variables were continuous variables, with the units of average temperature: per °C; cumulative precipitation: per mm; average speed wind: per 0.1 m/s, population density: per 1000/km2; and distance to Wuhan: per 100 km increase, respectively. β = coefficient; SE = standard error; RR = relative ratio, CI = confidence interval. * statistically significant.
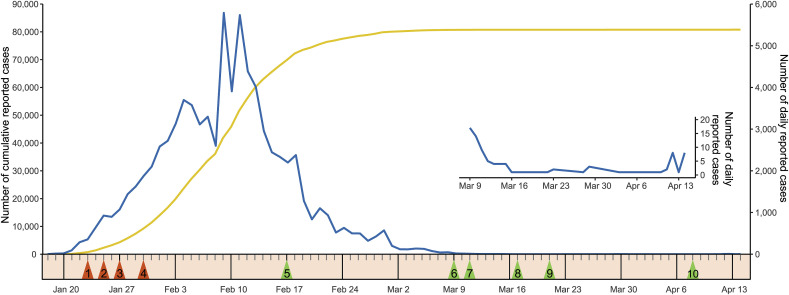
To control the extremely hard epidemic situation of COVID-19 which started at Wuhan city, a series of very strict measures have been taken in mainland China, including lockdown of Wuhan, extending the Spring Festival holidays, 14-day self-quarantines, and postponing school, etcetera. Meanwhile, medical assistance teams were organized and medical-related productions were resumed nationwide to support Hubei province including Wuhan city. The effect of measures was significant and the increasing trend of the disease got controlled in about two weeks. Due to the continuously declining impact of COVID-19, from February 17, Chinese authorities began to evaluate different areas based on the risks of the epidemic, and encouraged to resume production in “low-risk areas”. The schools in “low-risk areas” outside Hubei province started their spring terms since March 9 successively. In April 8, Wuhan ended the lockdown and reopened the city back to the normal life with caution, and these eases of restriction did not cause the epidemic rebound until now (Fig. 3 ).
Fig. 3.
Epidemic curves of COVID-19 on number of native cumulative reported cases and daily reported cases with crucial control measures and relaxing confinement measures in mainland China. Epidemic curves of COVID-19 from January 18 to April 14 are presented, including number of cumulative reported cases (yellow line) and number of daily reported cases (blue line). Crucial control measures (orange arrows) includes: (1) Lockdown of Wuhan city; (2) The first medical assistance team arrived in Wuhan; (3) China's Ministry of Education decided to postpone the spring semester for schools; (4) Medical-related productions were resumed nationwide. Relaxing confinement measures (green arrows) includes: (5) Chinese authorities began to evaluate different areas based on the risks of the epidemic, and encouraged to resume production in “low-risk areas” outside Hubei province; (6) The schools in “low-risk areas” outside Hubei province started spring terms; (7) Major industrial enterprises in Hubei but Wuhan started to resume production; (8) The medical assistance teams started to leave Hubei; (9) Major industrial enterprises in Wuhan started to resume production; (10) Wuhan officials eased restriction for outgoing travels and reopened Wuhan.
4. Discussion
The shock of COVID-19 pandemic to world has extremely challenged the capacity of the global public health response system. The epidemiological characteristics have been summarized using the surveillance data of 72,314 COVID-19 cases in mainland China (The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team, 2020). In this study, we did not generally describe the epidemic situation of China, but tried to quantify the epidemic magnitude and range. Furthermore, we tried to identify underlying factors for quick extension and transmission of COVID-19, thus to provide a scientific basis for prevention and control policies.
We used attack rate instead of the absolute number of reported cases to estimate the magnitude of COVID-19 outbreak at a finer scale of county level. Through mapping and spatiotemporal analyses, we discovered that the counties surrounding Wuhan had much higher ARs. This finding implies that the convenience of transportation and the mobility of population should have facilitated the quick transmission as has happened during the SARS outbreak (Fang et al., 2009). Wuhan is the political, cultural, economic, and transportation centre of not only Hubei province but also central China, hundreds of thousands of people in nearby counties work in Wuhan city using trains, cars or buses for travelling. When the epidemic in Wuhan began, many of them decided to return home, thereby spreading COVID-19 to surrounding areas.
Another geographical spread pattern is spreading to new epidemic areas through certain index cases, who have travelled to the epicentre, Wuhan, by air or inter-province trains. This pattern might play an important role in long-distance nationwide spread in the early period of the outbreak, especially before strict public health measures were taken (Riley, 2007). Furthermore, the outbreak of COVID-19 was coincided with the Spring Festival holidays, when people usually go back to their hometown to celebrate the most important Chinese festival. The large-scale population mobility especially from Wuhan have undoubtedly accelerated cross-province as well as cross-county transmissions (Kraemer et al., 2020) (Zhang et al., 2020). The risk for rapid spread along transportation routes is further proved by the logistic regression, in which counties crossed by a railway, a freeway, a national highway or having an airport had significantly higher risk for presence of COVID-19, even after adjusting for population density and distance to Wuhan. Another study on estimated risk for transportation of COVID-19 from Wuhan to other cities during travel by plane is consistent with our findings (Du et al., 2020). Therefore, lockdown of Wuhan and travel restriction should be a sensible choice and an effective way to control the nationwide spread of COVID-19.
Since the entrance of imported COVID-19 cases, local transmission might be one of main spread patterns in an area. We found that multiple meteorological factors were correlated with the AR of COVID-19, after controlling the distance to Wuhan and the population density. Average temperature was found to be negatively related to AR in our study. To date, most studies about meteorological effects on COVID-19 have explored the role of temperature. Several studies focusing mainland China have reported consistently with ours that the temperature was inversely associated with COVID-19, whereas none of them reported at county scale (Liu et al., 2020) (Qi et al., 2020) (Shi et al., 2020) (Wang et al., 2020). Some studies observed the positive or insignificant relationships between temperature and the disease, without adjusting for other meteorological factors (Bashir et al., 2020) (Yao et al., 2020). Considering the envelope structure of coronavirus (Schoeman and Fielding, 2019), low temperature may contribute to the stability of virus by promoting the ordering of lipids on the viral membrane (Polozov et al., 2008). A recent laboratory research on stability of SARS-CoV-2 reported that stability of the virus decreased with increasing temperature (Chin et al., 2020). Moreover, low temperature may also decrease the airway mucosal surface defence, making the host more vulnerable to coronavirus (Clary-Meinesz et al., 1992). Further experimental studies are needed to explore the infectivity of coronavirus under different conditions of temperature.
Our results also show the positive relationship between cumulative precipitation and transmission of COVID-19. A study in Mexico has observed positive effect of precipitation on transmission of COVID-19 (Méndez-Arriaga, 2020). Several studies have reported the relationship of relative humidity, rather than precipitation, with COVID-19, giving inconsistent evidences (Qi et al., 2020) (Wang et al., 2020) (Yao et al., 2020). The outbreak of COVID-19 in China is in winter, and the air of high relative humidity in most areas is too cold to contain enough water. Therefore, relative humidity may not appropriate to represent true content of water in the air (Moriyama et al., 2020). Our study also found that average wind speed had positive effect on the local transmission of COVID-19. Several studies have reported the precipitation and wind speed as one of climate drivers for the epidemic of flu (Gomez-Barroso et al., 2017) (Lopez et al., 2014) (Mahamat et al., 2013). Considering similar ways of transmission between flu and COVID-19, modest increasing precipitation may increase opportunity to spread virus infection by decreasing the evaporation of droplets, making them readily settle on surfaces (Lowen and Palese, 2009) (Lu et al., 2020). Increasing wind may facilitate the aerosol dissemination of SARS-CoV-2, thus rising the risk of COVID-19 (Lau et al., 2018).
We also found the existence of interactions among average temperature, cumulative precipitation and average wind speed. Higher risk of COVID-19 was reported in areas with low temperature and 50–120 mm of cumulative precipitation, Warm areas (average temperature over 10 °C) can also be in higher risk of the disease with the increasing wind speed. Some study have explored the interaction of meteorological factors on transmission of COVID-19 (Qi et al., 2020) (Xu, H. et al., 2020). Nevertheless, we have firstly reported the pairwise interactions between temperature, precipitation and wind speed. The interactions of meteorological factors discovered in our study may be one of reasons causing the severe epidemic situations in Spain, Italy, Iran and New York where the average temperature is below 10 °C and the precipitation is in range of 30–100 mm in February (Weather Atlas, 2020). Regions with above conditions should take greater efforts for the prevention of COVID-19. Meanwhile, the role of wind speed playing in the transmission of COVID-19 in the warm areas suggested by our study may be one of the reasons for COVID-19 prevalence in warm places such as Brazil, India and Peru. Indoor environment and social behaviour of people should also contribute significantly in transmission of COVID-19, as the measures including travel restriction, isolation taken by Chinese government showed positive influences rapidly. More studies are needed to explore factors causing pandemic of the disease.
Our study has some limitations. Firstly, we can only get data on main transportation routes and hubs such as railways, freeways, national highways and airports to estimate the risk for COVID-19 transmission while detailed travel data on county level, which are inaccessible, may be better. We conducted an ecological study on group-level, thus the exact risk for person-to-person transmission as well as transmissibility of the novel coronavirus could not be evaluated. Secondly, we adopted a cross-sectional design which is rational due to the short period of epidemic in China, while longitudinal studies for long-time observation are more powerful and needed for further exploration. Moreover, some risk factors that may affect the risk of SARS-CoV-2 infection were not included in our analysis, such as the proportion of imported cases to all cases, social and economic status, indoor environment, behaviour pattern and susceptibility.
In conclusion, COVID-19 spread rapidly from Wuhan, where it first occurred, to a wide range of China. The accessibility of main transportation are the risk factors for nationwide spread. Multiple meteorological factors can significantly affect the local transmission. Areas with highly developed transportation, low temperature and moderate precipitation have high risk for COVID-19, warm places with increasing wind speed also have higher risk for COVID-19. Therefore, countries with above conditions should pay more attention and take effective strategies such as travel restriction, isolation, disinfection and contact tracing to contain COVID-19.
Declaration of competing interest
Declarations of interest: none.
Acknowledgments
This work was supported by National Natural Science Foundation of China, China [grant ID 81621005], National Key Research and Development Program of China, China [grant ID 2019YFC1200505], and China Postdoctoral Science Foundation, China [grant ID 2020T130069ZX]. We acknowledge all colleagues for the data collection and cleaning, including Guan-Hui Ma, Peng-Yu Zhu, Ke-Ma, Hai-Tao Wang, Shu-Cheng Si, Ji-Qing Li, Gao-Pei Zhu, Xin-hui Liu, Ting-Xuan Liu, Yun-Xia Li, Cong-Cong Liu, Xiao-Lu Chen, Yan-Jia, Kai-Li She, Chao-Nan Yin, Zhen-Wei Li, Wen-Jing Wang, Wan-Yu Du, Da-Li Xu, Yi-Ping Feng, Tong-Hui Yuan, Wen-Chao Li, Li-Li Liu, Bo-Jie Wang, Feng-Ming Pan, Xin-Ying Wu, and Hong-Yu Zhao.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijheh.2020.113610.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Bashir M.F., Ma B., Bilal, Komal B., Bashir M.A., Tan D., Bashir M. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briz-Redón Á., Serrano-Aroca Á. A spatio-temporal analysis for exploring the effect of temperature on COVID-19 early evolution in Spain. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin A.W.H., Chu J.T.S., Perera M.R.A., Hui K.P.Y., Yen H.-L., Chan M.C.W., Peiris M., Poon L.L.M. Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe. 2020;1:e10. doi: 10.1016/s2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clary-Meinesz C., Cosson J., Huitorel P., Blaive B. Temperature effect on the ciliary beat frequency of human nasal and tracheal ciliated cells. Biol. Cell. 1992;76:335–338. doi: 10.1016/0248-4900(92)90436-5. [DOI] [PubMed] [Google Scholar]
- Collman A. 5 million people left Wuhan before the coronavirus quarantine - business Insider. 2020. https://www.businessinsider.com/5-million-left-wuhan-before-coronavirus-quarantine-2020-1 [WWW Document]. Bus. Insid. (accessed 8.3.20)
- Du Z., Wang L., Cauchemez S., Xu X., Wang X., Cowling B.J., Meyers L.A. Risk for transportation of coronavirus disease from Wuhan to other cities in China. Emerg. Infect. Dis. 2020 doi: 10.3201/eid2605.200146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang L.Q., De Vlas S.J., Feng D., Liang S., Xu Y.F., Zhou J.P., Richardus J.H., Cao W.C. Geographical spread of SARS in mainland China. Trop. Med. Int. Health. 2009;14:14–20. doi: 10.1111/j.1365-3156.2008.02189.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez-Barroso D., León-Gómez I., Delgado-Sanz C., Larrauri A. Climatic factors and influenza transmission, Spain, 2010–2015. Int. J. Environ. Res. Publ. Health. 2017;14 doi: 10.3390/ijerph14121469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassem A.Z.E. Cold Spring Harbor Laboratory Press; 2020. Do Weather Temperature and Median-Age Affect COVID-19 Transmission?, medRxiv. [DOI] [Google Scholar]
- Kraemer M.U.G., Yang C.H., Gutierrez B., Wu C.H., Klein B., Pigott D.M., du Plessis L., Faria N.R., Li R., Hanage W.P., Brownstein J.S., Layan M., Vespignani A., Tian H., Dye C., Pybus O.G., Scarpino S.V. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368:493–497. doi: 10.1126/science.abb4218. (80-.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau S.Y.F., Wang X., Wang M., Liu S., Zee B.C.Y., Han X., Yu Z., Sun R., Chong K.C., Chen E. Identification of meteorological factors associated with human infection with avian influenza A H7N9 virus in Zhejiang Province, China. Sci. Total Environ. 2018;644:696–709. doi: 10.1016/j.scitotenv.2018.06.390. [DOI] [PubMed] [Google Scholar]
- Lindstrom M.J., Bates D.M. Newton—raphson and EM algorithms for linear mixed-effects models for repeated-measures data. J. Am. Stat. Assoc. 1988;83:1014–1022. doi: 10.1080/01621459.1988.10478693. [DOI] [Google Scholar]
- Linton N.M., Kobayashi T., Yang Y., Hayashi K., Akhmetzhanov A.R., Jung S., Yuan B., Kinoshita R., Nishiura H. incubation period and other epidemiological characteristics of 2019 novel coronavirus infections with right truncation: a statistical analysis of publicly available case data. J. Clin. Med. 2020;9:538. doi: 10.3390/jcm9020538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhou J., Yao J., Zhang X., Li L., Xu X., He X., Wang B., Fu S., Niu T., Yan J., Shi Y., Ren X., Niu J., Zhu W., Li S., Luo B., Zhang K. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez D., Gunasekaran M., Murugan B.S., Kaur H., Abbas K.M. Proceedings - 2014 IEEE International Conference on Big Data, IEEE Big Data 2014. Institute of Electrical and Electronics Engineers Inc.; 2014. Spatial big data analytics of influenza epidemic in Vellore, India; pp. 19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowen A., Palese P. Transmission of influenza virus in temperate zones is predominantly by aerosol, in the tropics by contact. PLoS Curr. 2009;1 doi: 10.1371/currents.RRN1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu C. wei, Liu X. fen, Jia Z. fang. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020 doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahamat A., Dussart P., Bouix A., Carvalho L., Eltges F., Matheus S., Miller M.A., Quenel P., Viboud C. Climatic drivers of seasonal influenza epidemics in French Guiana, 2006-2010. J. Infect. 2013;67:141–147. doi: 10.1016/j.jinf.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Méndez-Arriaga F. The temperature and regional climate effects on communitarian COVID-19 contagion in Mexico throughout phase 1. Sci. Total Environ. 2020;735 doi: 10.1016/j.scitotenv.2020.139560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriyama M., Hugentobler W.J., Iwasaki A. Seasonality of respiratory viral infections. Annu. Rev. Virol. 2020;7 doi: 10.1146/annurev-virology-012420-022445. [DOI] [PubMed] [Google Scholar]
- National Health Commission of China Guideline for diagnosis and treatment of novel coronavirus Pneumonia (trial version 7) http://www.nhc.gov.cn/xcs/zhengcwj/202003/46c9294a7dfe4cef80dc7f5912eb1989/files/ce3e6945832a438eaae415350a8ce964.pdf [WWW Document] (accessed 8.3.20)
- Polozov I.V., Bezrukov L., Gawrisch K., Zimmerberg J. Progressive ordering with decreasing temperature of the phospholipids of influenza virus. Nat. Chem. Biol. 2008;4:248–255. doi: 10.1038/nchembio.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H., Xiao S., Shi R., Ward M.P., Chen Y., Tu W., Su Q., Wang W., Wang X., Zhang Z. COVID-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley S. Large-scale spatial-transmission models of infectious disease. Science. 2007;80 doi: 10.1126/science.1134695. [DOI] [PubMed] [Google Scholar]
- Schoeman D., Fielding B.C. Coronavirus envelope protein: current knowledge. Virol. J. 2019 doi: 10.1186/s12985-019-1182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi P., Dong Y., Yan H., Zhao C., Li X., Liu W., He M., Tang S., Xi S. Impact of temperature on the dynamics of the COVID-19 outbreak in China. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Z., Thilakavathy K., Kumar S.S., He G., Liu S.V. Potential factors influencing repeated SARS outbreaks in China. Int. J. Environ. Res. Publ. Health. 2020 doi: 10.3390/ijerph17051633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China (article in Chinese) http://rs.yiigle.com/yufabiao/1181998.htm [PMC free article] [PubMed]
- Tosepu R., Gunawan J., Effendy D.S., Ahmad L.O.A.I., Lestari H., Bahar H., Asfian P. Correlation between weather and Covid-19 pandemic in Jakarta, Indonesia. Sci. Total Environ. 2020;725:138436. doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tu W., Tang H., Chen F., Wei Y., Xu T., Liao K., Xiang N., Shi G., Li Q., Feng Z. vol. 2. China CDC Wkly; 2020. pp. 83–86. (Epidemic Update and Risk Assessment of 2019 Novel Coronavirus — China, January 28, 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ujiie M., Tsuzuki S., Ohmagari N. Effect of temperature on the infectivity of COVID-19. Int. J. Infect. Dis. 2020;95:301–303. doi: 10.1016/j.ijid.2020.04.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Tang K., Feng K., Lv W. High temperature and high humidity reduce the transmission of COVID-19. SSRN Electron. J. 2020 doi: 10.2139/ssrn.3551767. [DOI] [Google Scholar]
- Weather Atlas. 2020. https://www.weather-atlas.com/ [WWW Document] (accessed 8.3.20)
- Wood SimonN. Stable and efficient multiple smoothing parameter estimation for Generalized Additive Models. J. Am. Stat. Assoc. 2004;99:673–686. doi: 10.1198/016214504000000980. [DOI] [Google Scholar]
- World Health Organization Rolling updates on coronavirus disease (COVID-19) 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen [WWW Document]. Events as they happen. (accessed 8.3.20)
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H., Yan C., Fu Q., Xiao K., Yu Y., Han D., Wang W., Cheng J. Possible environmental effects on the spread of COVID-19 in China. Sci. Total Environ. 2020;731 doi: 10.1016/j.scitotenv.2020.139211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X.W., Wu X.X., Jiang X.G., Xu K.J., Ying L.J., Ma C.L., Li S.B., Wang H.Y., Zhang S., Gao H.N., Sheng J.F., Cai H.L., Qiu Y.Q., Li L.J. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368 doi: 10.1136/bmj.m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y., Pan J., Liu Z., Meng X., Wang Weidong, Kan H., Wang Weibing. No association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur. Respir. J. 2020 doi: 10.1183/13993003.00517-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C., Chen C., Shen W., Tang F., Lei H., Xie Y., Cao Z., Tang K., Bai J., Xiao L., Xu Y., Song Y., Chen J., Guo Z., Guo Y., Wang X., Xu M., Zou H., Shu Y., Du X. Impact of population movement on the spread of 2019-nCoV in China. Emerg. Microb. Infect. 2020 doi: 10.1080/22221751.2020.1760143. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.