ABSTRACT
The operating theatre staff is exposed to various constraints such as excessive working hours, severe medical conditions and dreadful consequences in case of malpractice. These working conditions may lead to high and chronic levels of stress, which can interfere with medical staff well-being and patients quality of care. The aim of this study is toassess the impact of music therapy on stress levels and burnout risk on the operating room staff. This is a pre-experimental study including the operating rooms staff of urology and maxillofacial surgery in the academic hospital of Sahloul Sousse (Tunisia) over a period of six weeks. The study consisted of three phases. The first was an initial assessment of stress level with a predefined survey. The second included three music therapy sessions per day over one month. The third was an immediate stress level reassessment following the intervention. Stress levels were evaluated using the Perceived Stress Scale version PSS-10 and the Maslach Burnout Inventory. The overall response rate was 73.9%.The average age of the study population was 37.8 ± 7.7 years with a female predominance (64.7%). After the music therapy program, Perceived Stress Scale average score decreased from 22 ± 8.9 to 16 ± 7.9 (p = 0.006). Concerning the burnout, only the average score of emotional exhaustion decreased significantly from 27 ± 10.8 to 19.2 ± 9.5 (p = 0.004). Music therapy is an innovative approach that seems to reduce operating theatre staff stress. It must be considered as a non pharmacological, simple, economic and non invasive preventive tool.
KEYWORDS: Music therapy, stress, burnout, operating room
1. Introduction
Stress is a physiological, psychological and behavioral reaction triggered by threatening situations, loss or challenge. It was integrated into the medical lexicon for the first time by Hans Selye to describe the ‘nonspecific response of the body to any demand’ [1,2]. It is considered as a general adaptation syndrome affecting personal and professional fields [3].
Occupational stress occurs once there is an imbalance between perceived environmental and occupational requirements; and individual adaptative capacities [3]. Recently, it has gained great attention because of technological progress, quality requirements and significant competitiveness [4,5]. Indeed, it has been considered as a public health problem due to its psychosomatic consequences and socio-economic cost [6,7]. According to the European Agency for Safety & Health at Work, its related expenses are about 20 billion Euros per year [8]. It is also considered a real mental health threat as it is a main cause of Burn-Out (BO) especially in the healthcare sector [9]. In fact, the risk of burnout in areas of high occupational stress is seven times greater than that in areas of low occupational stress [10].
Reported for the first time in 1974 by Freudenberger, the BO describes a state of exhaustion and internal void observed in individuals who are involved in aid relationship, such as medical and paramedical staff [11,12]. The operating theatre staff is particularly concerned by this condition [9] as it is commonly exposed to various constraints related to heavy technical platform, excessive working hours, severe medical conditions and dreadful consequences in case of malpractice [11].
Thus, preventive measures should be elaborated to help health personnel cope with existing stressors. Many procedures have been proposed such as music therapy [13,14]. This non pharmacological technique is defined by the American Music Therapy association [15] as ‘the clinical and evidence-based use of music interventions to accomplish individualized goals within a therapeutic relationship by a credentialed professional who has completed an approved music therapy program’.
Its effectiveness has been proven in the management of physical and mental stress, anxiety, depression and pain related to some neuropsychiatric conditions, cancer and surgical intervention [16–20]. According to a new literature review enrolling the impact of musical interventions on stress and anxiety was reported by the majority of enrolled studies [21].
Recently, it has been assessed in the operating room by several studies focusing mainly in its effects on patients [22–25]. Its impact on the operating room staff is not well established and results remain controversial. While performance and accuracy could be improved for surgeons, vigilance, attention and alarms perception may be disrupted for anesthetists [22]. In addition, its effects on stress levels have not been assessed yet [13].
In this context, this study was conducted to evaluate the effects of a music therapy program on the level of stress and burnout risk among the operating room staff of urology and maxillofacial surgery in an academic hospital.
2. Methods
After the approval of the institutional ethics committee, this pragmatic quasi-experimental study with pre-post measures was conducted in the operating theatre of urology and maxillofacial surgery of Sahloul Academic Hospital (Sousse, Tunisia), over a six weeks period (from January 2nd to 16 February 2017). This central operating theatre is composed of 5 functional operating rooms.
All the staff members with an occupational seniority of more than 1 year, exercising the mornings and who had expressed their oral consent to participate, were enrolled in this study. Criteria for non-inclusion were refusal to participate to the study, drugs affecting the central nervous system, psychiatric or hearing disorders, trainees and non-titular staff members. Participants who did not assist to the intervention or who were unreachable during data collection were excluded from the study.
Collected data was based on a pre established questionnaire including socio-professional characteristics of the participants, their lifestyle, their level of stress and their BO risk. Two validated tools were considered: the Perceived Stress Scale in its version PSS-10 and the Maslash Burn out Inventory (MBI) in its French version.
The PSS-10 was used to measure the stress level of our population. This scale is composed of 10 items divided into 2 groups. The first group has 6 negative items measuring ‘perception of stress’, while the second group has 4 positive items measuring ‘coping’ or adaptation to stress. A high level of perceived stress is defined by a score greater than 27 [26,27].
The MBI was used to assess BO. It is a self-questionnaire consisting of 22 items assessing three dimensions: emotional exhaustion (9 items), depersonalization (5 items) and personal accomplishment (8 items). Emotional exhaustion is considered high if the score is greater than 30. For depersonalization, it is considered high for a total greater than 12. Finally, the impairment of personal achievement is considered high for a score less than 33. In our survey a high level of burnout was defined by the association of a high score of emotional exhaustion and depersonalization and a low score of professional achievement [12,28,29].
Our study consisted of three phases. The first phase started January the 2 nd and lasted one week. It was an initial assessment of the stress and BO level using the pre-established questionnaire. Questionnaires were distributed by the investigator through direct contact with staff members. During these contacts, the investigator explained the interest of the study and clarified the content of the different items to the participants.
The second phase consisted of a one-month intervention (from January 9th to February 9th). Three sessions of music therapy of 30 minutes each were provided daily to the operating room staff during working days. These sessions had the same hours during the whole study period (from 8:00 am to 8:30 am, from 10:00 am to 10:30 am and from 12:00 pm to 12:30 pm) unless a patient-related incident occurred during a session. In this case, the current session was shifted. The same type of generic brand CD player was used in all operating rooms. The musical repertoire used was varied to satisfy all the participants’ preferences. Indeed several types of music have been used namely oriental, occidental and Tunisian music. In order to avoid noise pollution, music volumes were set below 60 dB using a mobile application (Sound meter, Smart tools Co) [13,16].
The third phase of the study began at the end of the music therapy program and lasted a week. The initial investigation was redone. The same questionnaire was redistributed. One question was added concerning the opinion of the participants regarding this intervention.
The data was analyzed using the SPSS.20.0 software. Qualitative variables were expressed in numbers and percentages. Continuous variables were expressed as means, standard deviations, medians and extent of extreme values, according to their distribution. For the comparison of the means, Student’s T-Test was used to compare two independent series averages and the Snedecor ‘f’ test for parametric variance analysis (one-way ANOVA) was used to compare several averages. Frequency comparison was performed with the Pearson Chi-square test. The study of the relationship between two quantitative variables was done using the Pearson correlation coefficient. For all statistical tests, the significance level p was set at 0.05.
3. Results
Of the 49 staff assigned to the operating room of urology and maxillofacial surgery, inclusion criteria were retained in 46 participants. Twelve members were subsequently excluded, corresponding to a final population of 34, with a participation rate of 73.9% (Figure 1).
Figure 1.
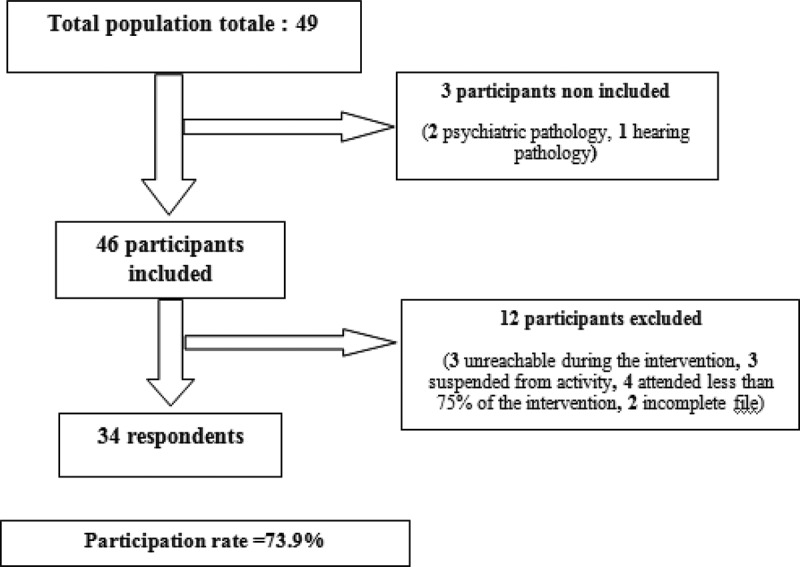
Flowchart.
The mean age of our study population was 37.8 ± 7.7 years. A female predominance was noted with a sex ratio of 0.54. The study population was divided between 10 medical professionals (29.4%) and 24 paramedics (70.6%). Average occupational seniority was 13.1 ± 8.9 years.
Fourteen participants went around urology and maxillofacial surgery operating rooms (41.2%). The average number of surgeries performed per participant per day during the last week was 7.5 ± 4.1 interventions.
Table 1 summarizes the socio-professional characteristics and lifestyle habits of the study population.
Table 1.
Socio-professional characteristics and lifestyle habits of the study population.
| Variables | Number | Percentage (%) |
|---|---|---|
| Marital status | ||
| Married | 29 | 85.3 |
| Single | 3 | 8.8 |
| Divorced | 2 | 5.9 |
| Tobacco smoking | ||
| Yes | 5 | 14.7 |
| No | 29 | 85.3 |
| Alcohol consumption | ||
| Yes | 10 | 29.4 |
| No | 24 | 71.6 |
| Physical activity | ||
| Yes | 10 | 29.4 |
| No | 24 | 70.6 |
| Coffee consumption | ||
| Neither or rarely | 39 | 26.4 |
| Frequently | 14 | 41.2 |
| Occupational status | ||
| Surgeon | 8 | 23.5 |
| Anesthetist doctor | 21 | 5.9 |
| Anesthetist technician | 5 | 35.3 |
| Nurse | 6 | 14.7 |
| Instrumentalist | 6 | 17.6 |
| Caregiver | 1 | 2.9 |
| Operating theatre | ||
| Urology | 11 | 32.4 |
| Maxillofacial surgery | 9 | 26.5 |
| Both | 14 | 41.2 |
| Another occupational activity | ||
| Yes | 8 | 23.5 |
| No | 26 | 76.5 |
| Effect size | 34 | 100 |
Statical methods: numbers and percentages
At the first evaluation, 14 participants (41.2%) had high levels of perceived stress. A high score was noted in 38.2% of cases for emotional exhaustion, in 50% for depersonalization and in 58.8% for professional achievement. Of the 29 participants affected by this syndrome, 5 (17.2%) had a high level of burnout (Table 2).
Table 2.
Burnout evaluation.
| Settings of burnout | Number | Percentage (%) | |
|---|---|---|---|
| Emotional exhaustion | Low | 7 | 20,6 |
| Moderate | 14 | 41,2 | |
| High | 13 | 38,2 | |
| Depersonalization | Low | 11 | 32,4 |
| Moderate | 6 | 17,6 | |
| High | 17 | 50 | |
| Professional achievement | Low | 6 | 17,6 |
| Moderate | 8 | 23,5 | |
| High | 20 | 58,8 | |
| Burnout level (High) | Yes | 5 | 17,2 |
| No | 24 | 82,8 | |
Statical methods: numbers and percentages
At the end of our intervention, the mean perceived stress score decreased significantly from 22 ± 8.9 to 16 ± 7.9 (p = 0.006). Only 4 patients (22.2%) had kept a high level of stress (Table 3).
Table 3.
Evolution of perceived stress after intervention.
| Variables | Before intervention Effect size (34) |
After intervention Effect size (30) |
p | |
|---|---|---|---|---|
| Number (percentage) | Number (percentage) | |||
| Stress level | Low | 9 (37,5%) | 15 (62,5%) | 0,033 |
| Moderate | 11 (50%) | 11 (50%) | ||
| High | 14 (77,8%) | 4 (22,2%) | ||
| Average score of perceived stress | Mean± Standard Deviation | |||
| 22 ± 8,8 | 16 ± 7,9 | 0,006 | ||
Statical methods: Snedecor ‘f’ test/Pearson Chi-square test
For burnout, only the mean score of emotional exhaustion decreased significantly from 27 ± 10.8 pre-intervention to 19.2 ± 9.5 post-intervention (P = 0.004) (Table 4).
Table 4.
Evolution of burnout after intervention.
| Variables | Before intervention Effect size (34) |
After intervention Effect size (30) |
p | |
|---|---|---|---|---|
| Number (percentage) | Number (percentage) | |||
| Emotional exhaustion | <17 | 7 (29,2%) | 17 (70,8%) | 0,011 |
| 18–29 | 14 (70%) | 6 (30%) | ||
| ≥ 30 | 13 (65%) | 7 (35%) | ||
| Depersonalization | < 5 | 11(57,9%) | 8 (42,1%) | 0,5 |
| 6–11 | 6 (40%) | 9 (60%) | ||
| ≥ 12 | 17 (56,7%) | 13 (43,3% | ||
| Professional achievement | ≥ 40 | 6 (46,2%) | 7 (53,8%) | 0,73 |
| 34–39 | 8 (61,5%) | 5 (38,5%) | ||
| ≤ 33 | 20 (52,6%) | 18 (47,4%) | ||
| Burnout level | High | 5 (17,2%) | 3 (15%) | 0,98 |
| Low-Moderate | 24 (82,8%) | 17 (85%) | ||
Statical methods: Pearson Chi-square test
The majority of participants (73.5%) felt that this intervention was beneficial.
4. Discussion
The music Therapy program assessed in our study allowed a significant improvement in perceived stress as the Perceived Stress Scale average score decreased from 22 ± 8.9 to 16 ± 7.9 (p = 0.006). Concerning the burnout, only the average score of emotional exhaustion decreased significantly from 27 ± 10.8 to 19.2 ± 9.5 (p = 0.004).
Similar results have been reported by other studies that have considered various tools in stress assessment and a wide variety of studied populations.
In fact, a music therapy program had decreased the average perceived stress score from 6.7 in pre-intervention to 2.98 in post-intervention (p < 0.001), in a study enrolling 54 nurses. Results suggested also a significant improvement of heart rate, blood pressure, and cortisol levels [30].
Horst M [31] assessed the impact of music therapy on stress levels in 36 caregivers. The intervention consisted of a music therapy program of 1 to 5 sessions of 20 min. Repeated assessments showed a decrease in the stress level after each of the 5 music therapy sessions compared to the pre-interventional values (p < 0.05). Relative stress reductions were statistically significant for each of the received sessions (1–5) (p < 0.001).
De Cunto Taets G et al [13] also found a significant decrease in the staff stress levels in a Brazilian private clinic after a program of 12 music therapy sessions. In the study of Watanabe K [32] assessing the effect of music on stress in nurses via a questionnaire and heart rate measurement, a significant decrease was noted for heart rate, but not for self-reported data.
Beck BD et al [33] assessed the impact of a psychotherapy intervention including relaxation, music listening, and imagery, on biopsychosocial measures of work related stress. Twenty workers on sick leave were randomized into two groups: individual music therapy versus waitlist control. Outcome criteria included salivary cortisol, testosterone, melatonin, self-reported data on psychological stress symptoms and job return. After nine weeks of music therapy, a significant improvement was found in well-being, mood disturbance, physical distress, and cortisol concentrations. Results were also in favour of an early intervention as related to the onset of sick leave, as evidenced by a faster job return and a significant improvement in stress levels.
Similar findings were reported by Khalfa B et al [34] in a study focusing in the effects of relaxing music on salivary cortisol level after a psychologically stressful task (Trier Social Stress Test). Patients were allocated into two groups (group music therapy and group silence) and salivary cortisol levels were regularly monitored. Results showed a stabilization of salivary cortisol level in intervention group, versus its increase during the 30 minutes following the stressor in the control group.
However, contradictory results have also been reported in the literature. Thoma MV et al [35] assessed the effect of a music intervention on pre-treatment anxiety and stress in healthy patients waiting for dental hygiene treatment. Ninety two patients were randomly allocated to either an experimental (listening to music for 10 min) or a control group (waiting in silence). Although the intervention decreased anxiety levels, no effects were found on subjective stress or mood variables.
These discrepancies cannot rule out the beneficial effects of music therapy on stress levels and anxiety. In fact, besides the characteristics of prescribed music, patients’ preferences and their experiences with music may have a crucial effect on positive behavior changes related to music [36]. According to the meta-analysis of Pelletier CL [37], the amount of stress reduction was significantly different when considering age, type of stress, music assisted relaxation technique, musical preference, previous music experience, and type of intervention.
Regarding BO, only the average score of emotional exhaustion decreased significantly from 27 ± 10.8 to 19.2 ± 9.5 (p = 0.004). Our results are consistent with those of Bittman B et al [38] who noted a significant decrease in emotional exhaustion after a 6-week music therapy intervention in first year associate degree nursing students (from 25.9 to 23.2; p = 0.01).
In another study enrolling 112 health care workers, a music therapy intervention for 6 weeks significantly reduced emotional exhaustion scores (from 16.3 to 13.2, p = 0.03) and significantly increased professional achievement scores (from 35 to 36.8, p = 0.003) [39].
Similarly, Horst M [31] reported that the BO rate among nurses significantly decreased after 5 music therapy sessions (p = 0.02).
Several studies have shown that musical entertainment activities in the workplace, such as choir songs [40], drums group [39,41], discussion song [42] and listening to music [30,33], can reduce chronic stress including BO, increase social support and improve immune system and health factors.
Brandes V et al [43] evaluated a musical intervention protocol that included listening to one of two specially designed music programs (P1 or P2) twice a day for 30 minutes, 5 days a week, for duration of 5 weeks. The control group was randomized to listen to either sounds of nature (PN) or a list of their own choice (K). The authors concluded that there was a significant reduction in burnout symptoms for the P1 and P2 intervention groups. Similarly, participants reported a persistence of the degree of stabilization and the maintenance of psychological resilience.
On the other hand, Brooks D et al [44] found contradictory results. Indeed, no significant change was found in BO dimensions after music therapy sessions, which may be explained by the fact that participants received only 2 to 4 sessions.
Since 1946, the literature has provided consistent data on the effects of music in the operating room on both patients and staff. In our study, this therapy was found beneficial by 73.5% of participants.
Similar results were reported by Faraj AA et al [45] in their study assessing the attitude of healthcare professionals to music in the operating theatre. According to this study, working while listening to music was more appreciated by 78.9% of the medical staff and by 66.7% of nurses. Similarly, the performance was rated better by 66% of medical staff and 57% of nurses. Another study found that 63% of operating room staff believe that music has a positive effect and 77% of them believe that it makes them more effective and calmer [23]. Several authors have reported that music should be played in the operating theater because of its benefits such as relaxation, well-being, and mood enhancement [25,46].
The impact of the music in the operating room should be analyzed according to the effects on the patient, the surgeon and the rest of the staff.
As for the surgeon, music seems to have several advantages over performance and efficiency by improving accuracy, concentration and speed during the performance of tasks. Endurance also seems to be improved by the effects of music on muscle recruitment [47–51].
Several interviews about music effect on surgeons have been published. The majority attributed a positive effect on communication between staff, and nearly 80% of participants believe that music made people calmer and more effective [23].
However, regarding other operating room staff, especially anesthesiologists, music can potentially lead to poor communication and even distract them from various monitoring alarms and reduce their level of alertness [52].
According to other studies based on simulations, music increases the time needed to acquire skills (especially for trainees), slows the overall completion time of procedures and increases general irritation [24].
Some authors have also reported that for anesthetists, operating room noise can impair their ability to provide a stable level of sedation for patients undergoing surgery under local anesthesia. They also report that noise can decrease the effectiveness of sedation itself [53,54].
The type of music and volume was also a subject of debate. The literature emphasizes that the most appropriate music in the operating theater seems to be classical music because it is known to elicit mental alertness, which is necessary to perform surgical tasks and have a positive effect on surgical memory consolidation, thus improving surgical learning. This type of music also induces relaxing emotions that seem to be beneficial for controlling surgical tension, reducing anxiety and improving the efficiency and depth of anesthesia [22].
Regarding the volume of music, the majority of authors agree that the staff prefers a low volume [46]. Indeed, a high volume of music hinders communication and cooperation between the surgical team and the rest of the staff. In addition, it interferes with the audible alarms of monitoring devices [22].
Several hypotheses have been put forward to explain the effects of music therapy on stress and mood disorders. An analysis of 400 studies found that music positively affects the neurochemicals of four systems: the reward system, the social system, the immune system and the stress system [55].
Neuroimaging studies using PET scan and functional MRI found that pleasurable music perception increases regional cerebral blood flow within the structures that comprise the meso-cortico-limbic system, also known as the reward system or dopaminergic system [56,57]. This results in dopamine secretion, with central opioid receptor activation inhibiting pain sensation [58]. Strong deactivations were also observed in the amygdala, hippocampus and parahippocampal gyrus modulating defensive behaviors in response to stress because of a decrease in cortisol, which is a key hormone in the pathophysiology of stress [57].
Music has also an effect on the pituitary gland resulting in the release of growth hormone. This effect may be secondary to the central sedative actions of the music, an indirect inhibitory effect on the sympathetic nervous system or a liberation hypothalamic GHRH which is also present in immune cells thus suggesting an immunomodulatory role for this neuropeptide [59].
Some studies report an inverse correlation between the release of GHRH and the release of IL-6 from mononuclear peripheral blood cells [60]. In addition, the secretion of growth hormone induced by music could promote the immune response via the inhibition of apoptosis induced by activated T and B lymphocytes [61].
According to several studies, the effects of music on the hypothalamic-pituitary-adrenal axis seem to be dominant, since the ACTH and cortisol concentrations during music therapy have not changed significantly, while the adrenaline have actually decreased. As a result of its GH inhibition, the secretion of stress hormones, such as adrenaline and its metabolites, is suppressed and, consequently, a significant drop in blood pressure and heart rate [62].
Other data attribute effects to the neurohormonal pathway mediated by adrenocorticotropic hormone (ACTH) and cortisol [62]. Studies assensing [63] the neurophysiological response to music found a decrease in plasma norepinephrine, epinephrine, growth hormone, prolactin, ACTH, cortisol and β-endorphin concentrations [64].
Recent studies clearly indicate a fine two-way interaction between the neuroendocrine and immune systems. Hypothalamic hormones, apart from their neuroendocrine role, have influences on immune function. The release of growth hormone, for example, is not only produced by the neurosecretory cells of the hypothalamic-pituitary system, but also synthesized by immunocompetent cells. Interleukin-6 (IL-6) and other cytokines play a central role in immune modulation and also have demonstrated effects on the neuroendocrine system [62].
Several studies have investigated the effects of music on the production of salivary immunoglobulin A (s-IgA), a first line of defense against bacterial and viral infections [65], and a reliable marker of functional status of the entire mucosal immune system [66]. The studies of Knight WEJ et al [67] have shown an increase in the concentration of salivary immunoglobulin A compared to its baseline value when listening to relaxing music. However, this effect has not been proven for plasma IgA concentrations [68].
This study focusing in music therapy as a preventive procedure can easily be considered as a part of a workplace health improvement plan. It evaluates a particularly interesting tool as it is economic, non invasive and does not require any apprenticeship or prior training. However, some limitations must be considered before results interpretation such as the limited sample size and the relatively short time period for reassessment.
In addition, this study enrolled only staff members of urology and maxillofacial Surgery operating theatre resulting in a selected population. Thus, results generalization to others staffs may be absurd. However, this selectivity facilitates data analysis by reducing the studied population heterogeneity.
Furthermore, the use of self-report questionnaires which is a widely used approach in medical researches because of its speed and low cost may expose to the risk of participants subjectivity because of its declarative character. To remedy this deficiency, validated and standardized tools were used to evaluate stress and BO.
In our study, screening for auditory and psychiatric disorders which can interfere with the intervention impact, was based solely on anamnesis, whose sensitivity and specificity remain limited. A specialized ENT examination with audiometry and an assessment of mental status by validated tests should have been performed for all participants. In addition, the communication between the various members of the operating room and the noise of the devices could be a nuisance annoying the musical listening.
Finally, the choice of music should also be analyzed. The freedom of choice given to the participants would allow a better adherence to the study at the expense of a bias of confusion between the effects directly related to music properties and the effects related to other dimensions including emotional and nostalgic ones.
5. Conclusion
In our study, music therapy had significantly improved the stress levels of the operating theater staff suggesting a wide use of this non-pharmacological, simple, economical and non-invasive therapy as a preventive measure. However, many points must be previously specified such as the characteristics of the music to prescribe and the timing of its administration. Thus, randomized studies with larger samples, and phsyiological measures are needed before any definitive conclusion.
Disclosure statement
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
- [1].Légeron P. Le stress au travail. Paris: Odile Jacob; 2003. [Google Scholar]
- [2].Siang YT, Hans Selye YA. (1907–1982): founder of the stress theory. Singapore Med J. 2018;59(4):170–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Pauline M, Grégory M. L’inventaire de stress professionnel adapté aux Métiers de l’Urgence et corrélats psychopathologiques. An Med Psychol. 2015;173:704–710. [Google Scholar]
- [4].Malagris L. Burnout: o profissional em chamas. In: Sobrinho FPN, Nassaralla I, editors. Pedagogia Institucional: fatores humanos nas organizacoes. Rio de Janeiro: ZIT; 2004. p. 196–213. [Google Scholar]
- [5].Pafaro RC. Estudo do estresse do enfermeiro com dupla jornada de trabalho em um hospital de oncologia pediatrica de Campinas. Campinas: Dissertacao [Mestrado em Enfermagem] - Universidade Estadual de Campinas; 2002. [DOI] [PubMed] [Google Scholar]
- [6].Agency for Safety and Health at Work . Calculating the cost of work-related stress and psychosocial risks European Risk Observatory Literature Review. Luxembourg: Publications Office of the European Union; 2014. [Google Scholar]
- [7].Bernaldo-De-Quiro´s M, Piccini AT, Gomez MM, et al. Psychological consequences of aggression in pre-hospital emergency care: cross-sectional survey. Int J Nurs Stud. 2015;52:260–270. [DOI] [PubMed] [Google Scholar]
- [8].European Agency for safety and health at work . Calcul des coûts du stress et des risques psychosociaux liés au travail 2014. Available from: https://osha.europa.eu/fr/tools-and-publications/publications/literature_reviews/calculating-the-cost-of-work-related-stress-and-psychosocial-risks
- [9].Travers V, Watrelot A, Cuche H. Évaluation du niveau de stress et de ses principaux indicateurs chez les praticiens de bloc opératoire. Presse Med. 2012;41:e577–e585. [DOI] [PubMed] [Google Scholar]
- [10].Khalid A, Pan F, Li P, et al. The impact of occupational stress on job burnout among bank employees in Pakistan, with psychological capital as a mediator. Front Public Health. 2019;7:410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Freudenberger HJ. Staff burn-out. J Social Issues. 1974;30:159–165. [Google Scholar]
- [12].Kacem I, Kalboussi H, Ayoub N, et al. Burnout chez les jeunes médecins: étude réalisée dans la région de Sousse. Ann Med Psy. 2017;175(4):332–338. [Google Scholar]
- [13].De Cunto Taets G, Borba-Pinheiro CJ, Almeida de Figueiredo NM, et al. Impact of a music therapy program on the stress level of health professionals. Rev Bras Enferm. 2013;66(3):385–390. [DOI] [PubMed] [Google Scholar]
- [14].Linnemanna A, Ditzenb B, Strahlera J, et al. Music listening as a means of stress reduction in daily life. Psychoneuroendocrinology. 2015;60:82–90. [DOI] [PubMed] [Google Scholar]
- [15].American Music Therapy association. [cited 2020 April15]. Available from: https://www.musictherapy.org/.
- [16].Kahloul M, Mhamedi S, Nakhli MS, et al. Effects of music therapy under general anesthesia in patients undergoing abdominal surgery. Libyan J Med. 2017;12(1):1260886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Magee WL, Clark I, Tamplin J, et al. Music interventions for acquired brain injury. Cochrane Database Syst Rev. 2017;1:CD006787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Maratos A, Gold C, Wang X, et al. Music therapy for depression. Cochrane Database Syst Rev. 2008;1:CD004517. [DOI] [PubMed] [Google Scholar]
- [19].Bradt J, Dileo C, Magill L, et al. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst Rev. 2016;8:CD006911. [DOI] [PubMed] [Google Scholar]
- [20].van der Steen JT, Smaling HJA, van der Wouden JC, et al. Music-based therapeutic interventions for people with dementia. Cochrane Database Syst Rev. 2018;7:CD003477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Martin L, Oepen R, Bauer K, et al. Creative arts interventions for stress management and prevention—a systematic review. Behav Sci. 2018;8(2):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Moris DN, Linos D. Music meets surgery: two sides to the art of “healing”. Surg Endosc. 2013;27(3):719–723. [DOI] [PubMed] [Google Scholar]
- [23].Ullmann Y, Fodor L, Schwarzberg I, et al. The sounds of music in the operating room. Injury. 2008;39(5):592–597. [DOI] [PubMed] [Google Scholar]
- [24].Bosanquet DC, Glasbey JC, Chavez R. Making music in the operating theatre. BMJ. 2014;349:g7436. [DOI] [PubMed] [Google Scholar]
- [25].Makama JG, Ameh EA, Eguma SA. Music in the operating theatre: opinions of staff and patients of a Nigerian teaching hospital. Afr Health Sci. 2010;10(4):386–389. [PMC free article] [PubMed] [Google Scholar]
- [26].Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- [27].Langevin V, Boini S, François M, et al. Perceived Stress Scale (PSS): Échelle de stress perçu. INRS 2015; N 143: 101–104. Disponible sur www.rst-sante-travail.fr/rst/dms/dmt/ArticleDMT/RisquesPsychosociaux/
- [28].Maslach C, Jackson S. Maslash Burnout Inventory: research edition. Palo Alto (CA): Consulting Psychologists Press; 1981. [Google Scholar]
- [29].Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd ed. Palo Alto (CA): Consulting PsychologistsPress; 1996. [Google Scholar]
- [30].Lai HL, Li YM. The effect of music on biochemical markers and self-perceived stress among first-line nurses: A randomized controlled crossover trial. J Adv Nurs. 2011;67(11):2414–2424. [DOI] [PubMed] [Google Scholar]
- [31].Horst M. Evaluation de la musicothérapie sur le stress et le burn-out chez les soignants. Arch Mal Prof Envir. 2018;79:407–477. [Google Scholar]
- [32].Watanabe K The effects of music with abbreviated progressive relaxation tech- niques on occupational stress on femah; nurses in a hospital 2001. Unpublished Master’s Thesis, Florida State University, Tallahassee, FL. In Cori L. Pelletier, MM, MT-BC. The Effect of Music on Decreasing Arousal Due to Stress: A Meta-Analysis. JoumalofMusic Therapy, XU (3), 2004. 192-214. [DOI] [PubMed] [Google Scholar]
- [33].Beck BD, Hansen AM, Gold C. Coping with work-related stress through guided imagery and music (GIM): randomized controlled trial. J Music Ther. 2015;52(3):323–352. [DOI] [PubMed] [Google Scholar]
- [34].Khalfa S, S D Bella, Roy M, Peretz ILupien SJ. Effects of relaxing music on salivary cortisol level after psychological stress. Ann N Y Acad Sci. 2003;999:374-6. [DOI] [PubMed] [Google Scholar]
- [35].Thoma MV, Zemp M, Kreienbühl L, et al. Effects of music listening on pre-treatment anxiety and stress levels in a dental hygiene recall population. Int J Behav Med. 2015;22(4):498–505. [DOI] [PubMed] [Google Scholar]
- [36].Lesiuk T. The effect of preferred music listening on stress levels of air traffic controllers. Arts Psychotherapy. 2008;35(1):1–10. [Google Scholar]
- [37].Pelletier CL. The effect of music on decreasing arousal due to stress: a meta-analysis. J Music Ther. 2004;11(3):192–214. [DOI] [PubMed] [Google Scholar]
- [38].Bittman B, Snydery C, Bruhnz KT, et al. Recreational music-making: an integrative group intervention for redu-cing burnout and improving mood states in first year associate degree nursing students: insights and economic impact. Int J Nurs Educ Scholarship. 2004;1(1):1–29. [DOI] [PubMed] [Google Scholar]
- [39].Bittman B, Bruhn KT, Stevens CK, et al. Recreational Music-making: a cost-effective group interdisciplinary strategy for reducing burnout and improving mood states in long-term care workers - insights and poten-tial economic impact. Adv Mind Body Med. 2003;19(3–4):4–15. [PubMed] [Google Scholar]
- [40].Vaag J, Saksvik P, Theorell T, et al. Sound of well-being: choir singing as an intervention to improve well-being among employees in two Norwegian country hospitals. Arts Health. 2012;5(2):93–102. [Google Scholar]
- [41].Maschi T, MacMillan T, Viola D.. Group drumming and well-being: a promising self-care strategy for social workers. Arts Health. 2013;5(2):142–151. [Google Scholar]
- [42].Cheek J, Bradley L, Parr G, et al. Using music therapy techniques to treat teacher burnout. J Mental Health Couns. 2003;25(3):204–217. [Google Scholar]
- [43].Brandes V, Terris D, Fischer C, et al. Music programs designed to remedy burnout symptoms show signifi-cant effects after five weeks. Ann N Y Acad Sci. 2009;1169:422–425. [DOI] [PubMed] [Google Scholar]
- [44].Brooks D, Bradt J, Eyre L, et al. Creative approaches for reducing burnout in medical personnel. Arts Psychotherapy. 2010;37:255–263. [Google Scholar]
- [45].Faraj WAP, Haneef JHS, Jones A.. Listen while you work? The attitude of healthcare professionals to music in the operating theatre. Clin Feature. 2014;24(9):199–204. [DOI] [PubMed] [Google Scholar]
- [46].Shyjumon G, Shafiq A, Mammen JK, et al. Influence of music on operation theatre staff. J Anaesthesiol Clin Pharmacol. 2011;27(3):354–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Miskovic D, Rosenthal R, Zingg U, et al. Randomized controlled trial investigating the effect of music on the virtual reality laparoscopic learning performance of novice surgeons. Surg Endosc. 2008;22:2416–2420. [DOI] [PubMed] [Google Scholar]
- [48].Allen K, Blascovich J.. Effects of music on cardiovas-cular reactivity among surgeons. JAMA. 1994;272: 882e884. [PubMed] [Google Scholar]
- [49].Siu KC, Suh IH, Mukherjee M, et al. The effect of music on robot-assisted laparoscopic surgical performance. Surg Innov. 2010;17:306e311. [DOI] [PubMed] [Google Scholar]
- [50].Conrad C, Konuk Y, Werner P, et al. The effect of defined auditory conditions versus mental loading on the laparoscopic motor skill performance of experts. Surg Endosc. 2010;24:1347–1352. [DOI] [PubMed] [Google Scholar]
- [51].Pluyter JR, Buzink SN, Rutkowski AF, et al. Do absorp-tion and realistic distraction influence performance of component task surgical procedure? Surg Endosc. 2010;24:902–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Kalyvas AV, Linos D, Moris D.. Concerns about evaluat-ing the effect of noise and music inthe operating room. J Am Coll Surg. 2014;219(5):1097–1098. [DOI] [PubMed] [Google Scholar]
- [53].Newman A, Boyd C, Meyers D, et al. Implementation of music as an anesthetic adjunct during monitored anesthesia care. J Perianesth Nurs. 2010;25:387–391. [DOI] [PubMed] [Google Scholar]
- [54].Kim DW, Kil HY, White PF.. The effect of noise on the bispectral index during propofol sedation. Anesth Analg 2001; 93(5):1170–1173. [DOI] [PubMed] [Google Scholar]
- [55].Chanda ML, Levitin DJ.. The neurochemistry of music. Trends Cogn Sci. 2013;17(4):179–193. [DOI] [PubMed] [Google Scholar]
- [56].Blood AJ, Zatorre RJ.. Intensely pleasurable responses to music correlate with activity in brain regions implicated in reward and emotion. Proc Natl Acad Sci. 2001;98:11818–11823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Koelsch S, Fritz T, Cramon DY, et al. Investigating emo-tion with music: an fMRI study. Hum Brain Mapp. 2006;27(3):239–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Jeffries KJ, Fritz JB, Braun AR.. Words in melody: an h(2) 15o pet study of brain activation during singing and speaking. Neuroreport. 2003;14(5):749–754. [DOI] [PubMed] [Google Scholar]
- [59].Chrousos GP. The hypothalamic-pituitaryadrenal axis and immune-mediated inflammation. N Engl J Med. 1995;332:1351–1362. [DOI] [PubMed] [Google Scholar]
- [60].Siejka A, Stepien T, Lawnicka H, et al. Effect of the growth hormone-releasing hormone [GHRH(1–44) NH2] in IL-6 and IL-8 secretion from human peripheral blood mononuclear cells in vitro. Endocr Regul. 2005;39(1):7–11. [PubMed] [Google Scholar]
- [61].Mitsunaka H, Dobashi H, Sato M, et al. Growth hor-mone prevents Fas-induced apoptosis in lymphocytes through modulation of Bcl-2 and caspase-3. Neuroimmunomodulation. 2001;9(5):256–262. [DOI] [PubMed] [Google Scholar]
- [62].Escher J, Höhmann U, Anthenien L, et al. Music during gastroscopy. Schweiz Med Wochenschr. 1993;123 (26):1354–1358. [PubMed] [Google Scholar]
- [63].Claudius C, Hanno N, Karl-Walter J, et al. Overture for growth hormone: requiem for interleukin-6? Crit Care Med. 2007;35(12):2709–2713. [DOI] [PubMed] [Google Scholar]
- [64].Gerra G, Zaimovic A, Franchini D, et al. Neuroendocrine responses of healthy volunteers to ‘techno-music’: rela-tionships with personality traits and emotional state. Int J Psychophysiol. 1998;28(1):99–111. [DOI] [PubMed] [Google Scholar]
- [65].Woof JM, Kerr MA.. The function of immunoglobulin a in immunity. J Pathol. 2006;208:270–282. [DOI] [PubMed] [Google Scholar]
- [66].Hucklebridge F, Lambert S, Clow A, et al. Modulation of secretory immunoglobulin a in saliva; response to manipulation of mood. Biol Psychol. 2000. May;53(1):25–35. [DOI] [PubMed] [Google Scholar]
- [67].Knight WE, Rickard NS.. Relaxing music prevents stress-induced increases in subjective anxiety, systolic blood pressure, and heart rate in healthy males and females. J Music Ther. 2001;38(4):254–272. [DOI] [PubMed] [Google Scholar]
- [68].Chamorro-Premuzic T, Furnham A.. Personality and music: cantraits explain how people use music in everyday life? Br J Psychol. 2007;98:175–185. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- European Agency for safety and health at work . Calcul des coûts du stress et des risques psychosociaux liés au travail 2014. Available from: https://osha.europa.eu/fr/tools-and-publications/publications/literature_reviews/calculating-the-cost-of-work-related-stress-and-psychosocial-risks
- American Music Therapy association. [cited 2020 April15]. Available from: https://www.musictherapy.org/.
- Langevin V, Boini S, François M, et al. Perceived Stress Scale (PSS): Échelle de stress perçu. INRS 2015; N 143: 101–104. Disponible sur www.rst-sante-travail.fr/rst/dms/dmt/ArticleDMT/RisquesPsychosociaux/


