INTRODUCTION
Coronavirus disease 2019 (COVID-19) has affected more than 14 million individuals and caused more than 600,000 deaths as of July 20, 2020, rapidly spreading across large cities as well as many rural areas. In parallel with rising cases and deaths globally, the situation in local communities fluctuates daily while knowledge about the disease and transmission evolves.
Public health agencies play a critical role in managing disease epidemics. Agencies are on the front lines to conduct disease surveillance; facilitate resource distribution, including personal protective equipment (PPE); establish alternative care sites; and provide diagnostic support through laboratory testing.
The public health response to COVID-19 has been criticized1 , 2 for being too slow, lacking transparency, and being insufficient. This essay examines the reasons behind the sluggish response to COVID-19. The authors then argue for an evolved public health system after the crisis, which is better prepared for emergencies and equipped to support population health for the future.
A WEAK PUBLIC HEALTH SYSTEM
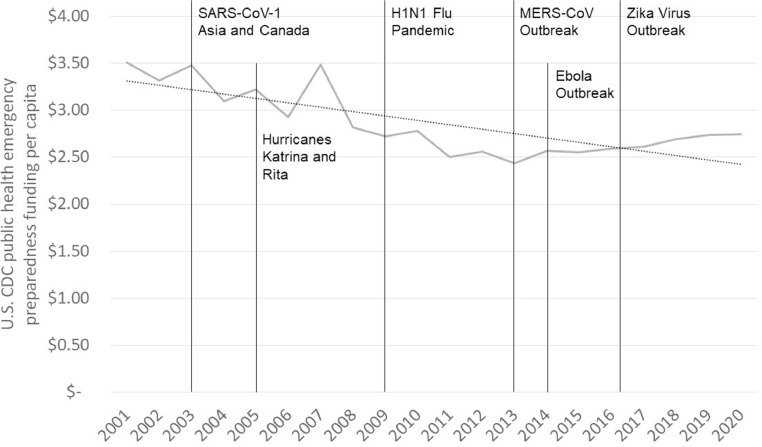
Although emergency funds for COVID-19 have been appropriated, history suggests that after the crisis, the U.S. will return to underinvestment in public health. Public health spending represents just 2.5% of all health spending,3 and reports from the National Academy of Medicine (NAM) over the past 20 years suggest that the public health system lacks the funding, infrastructure, and workforce to respond to regional, national, and international disease outbreaks.4 , 5 Figure 1 summarizes the Centers for Disease Control and Prevention (CDC) per capita funding, adjusted for inflation, for public health emergency preparedness (PHEP) since 2001. These funds are used to support surveillance as well as resilience in communities, including the planning and implementation of mitigation strategies designed to support vulnerable populations during an emergency or natural disaster.6 After major public health events, there is usually a temporary increase in funding followed by reductions that defund PHEP over time. Although recent PHEP funding increased modestly ($0.30 per capita), total spending is down by 27% since 2001. A similar pattern exists with the total CDC budget, which declined by 10% in the past decade.7
Figure 1.
Timeline depicting per capita funding of PHEP in the U.S. in parallel with major public health events between 2001 and 2020.
CDC, Centers for Disease Control and Prevention; MERS-CoV, Middle East respiratory syndrome‒related coronavirus; PHEP, public health emergency preparedness; SARS-CoV-1, severe acute respiratory syndrome coronavirus 1.
When testifying before Congress in April 2020, the Director of CDC Dr. Robert Redfield highlighted that chronic underinvestment was partially to blame for COVID-19 testing challenges.8 Yet, just 11 days after the WHO declaration of COVID-19 as a public health emergency on March 11, 2020, the White House proposed a 16% cut to future (Fiscal Year 2021) CDC funding as well as a 40% reduction in the contribution to WHO.7
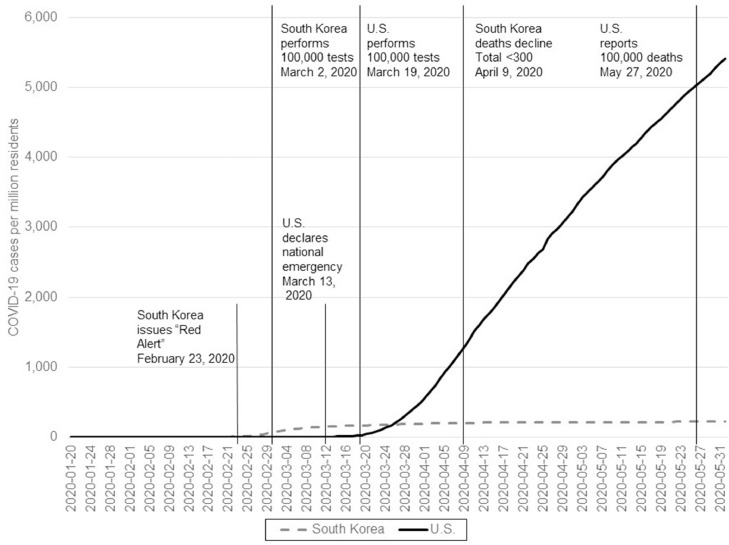
With respect to testing, multiple components of the health system failed. Test development by scientists at CDC ran into challenges. The U.S. Food and Drug Administration enforced usual processes delaying approval for hospitals, private clinics, and companies to deploy additional diagnostic tests. This is a stark contrast to other regions of the world where the private sector mobilized faster to develop and then offer screening tests for tens of thousands of individuals. Figure 2 highlights the differences in response between the U.S. and South Korea.9 Both countries documented their first case of COVID-19 around January 20, 2020. South Korea declared a national emergency 3 weeks before the U.S. Ten days before the U.S. declared COVID-19 an emergency, South Korea had already tested 100,000 individuals. America did not reach this milestone until March 19. By March 26, South Korea had 180 cases per million residents compared with 209 cases in the U.S. Moreover, despite the high rates of disease in many parts of the U.S. on that date, just 21 states had issued stay-at-home orders to enforce social distancing. Over the next 2 months, South Korea's cases would slowly inch to 224 per million residents, whereas America's burden soared to 5,408 cases per million residents by June 1.
Figure 2.
Timeline depicting the number of confirmed COVID-19 cases per million residents in the U.S. and South Korea between January 20, 2020 and May 31, 2020 in parallel with public health milestones reached in each country.
At local and state levels, public health agencies were challenged to coordinate efforts. Part of this stemmed from a lack of coordination initially at the federal level. Yet, a larger issue is the general lack of integrated data and information as well as the inability to rapidly analyze data. In the authors’ state, agency staff as well as volunteers were charged to manually call health facilities for information on their available beds, critical care capacity, ventilators, and PPE. Existing data available through sources such as the American Hospital Association survey were out of date or missing (e.g., ventilator counts). Moreover, there were virtually no data available on nursing home preparedness, institutions that house some of the most vulnerable populations to COVID-19. It quickly became apparent that these facilities were ground 0 for COVID-19 outbreaks and facilities lacked the staff, PPE, and other resources to properly respond.
Public health agencies further lacked access to real-time data on hospitalizations as well as transfers to critical care because hospitals do not share such information until after discharge. Moreover, providers did not use specific COVID-19 diagnostic codes until April 1 because they were not able to charge under these codes before this date. These system dynamics prevented electronic data flow to public health until weeks after the first case was diagnosed.
Beyond healthcare capacity, the U.S. public health system lacks a strong safety net to support the thousands of low-income residents impacted hardest by COVID-19. Data from the Regenstrief Institute highlight what many public health leaders recognized: racial and ethnic minority populations are at least twice as likely to become infected and hospitalized.10 A lack of sick time in many workplaces, including facilities critical to the nation's food supply, forced many individuals to come into work when ill or remain in a home environment where they spread COVID-19 to extended family members. Significant outbreaks in prisons and homeless shelters also highlighted the fragility of the public health system to protect vulnerable populations.
Once data could be assembled by public health authorities, rapidly analyzing information to examine capacity and forecast disease spread as well as resource utilization was limited, especially among local public health agencies. Informatics and data science professionals, although present in state health agencies and many large city health departments, were overwhelmed. Agencies engaged academics as well as private consultants to help. Yet, organizing these efforts took time and contributed to a slower-than-desired response. Moreover, coordination was limited giving rise to varying case definitions and methods to measure COVID-19‒related deaths.
EVOLVING THE PUBLIC HEALTH SYSTEM
The framework for an evolved American public health system exists, referred to as Public Health 3.0.11 The model urges a transformation in which there is a greater focus on building a culture of health, including cross-sector collaboration and an emphasis on health and health equity in all policies. Multisector coalitions that investigate and act to address health issues are led by chief health strategists, a new role for public health officers. Now is the time to begin planning for how to ensure the transition to this model once the COVID-19 pandemic ends. Getting there will require strategic partnerships, effective technology as well as infrastructure, workforce development, flexible and sustainable funding, and strong leadership.
A key tenant of Public Health 3.0 is that public health must engage broadly with partners in multiple sectors. Health system leaders as well as leaders in finance, technology, transportation, real estate, social services, and energy are necessary partners to create a culture that values human health and well-being. To adequately address upstream issues, including the social determinants of health, public health agencies need strategic, bidirectional partnerships that can support addressing complex health and social needs. For example, many states implemented drive-thru testing sites for COVID-19, yet many low-income populations do not have access to a personal vehicle. Community leaders pointed this out during the response, so why were they not consulted ahead of time or represented in state emergency operations centers? Partners should be engaged in decision making, including the assessment of community health needs and the establishment of public health programs to meet those needs.
To ensure that health and equity are present in all policies, public health should be represented in partners’ meetings when decisions are made about where to build the next school as well as plans to redevelop vacant housing sites in low-income neighborhoods. Residential zoning, walking trails, and bus lines can benefit some populations at the expense of others. Decisions by local and state authorities should consider impacts on environmental and social determinants, consulting public health officials regularly. Healthcare organizations should also consult public health partners in various processes, including facility planning and case conferences. For example, engaging public health nurses in case conferences at a federally qualified health center enabled access to needed public services as well as information about living environments and communities that supported addressing the needs of complex and vulnerable patients.12
The U.S. must continue to make progress toward the use of effective information systems and infrastructure across the public health system. Although healthcare policy influenced the adoption of electronic health records in hospitals and clinics, many public health agencies continue to rely on outdated technology and lack connectivity to providers.13 Transition to Public Health 3.0 requires investment in new technologies for public health, including technical interfaces among medicine, public health, and social service agencies. Nascent efforts such as Digital Bridge14 have the potential to transform how data and information are captured on emerging health threats, but many states and local health authorities lack the capacity to establish robust infrastructures. When fully connected, public health will have bidirectional capabilities to receive and send information with our strategic partners. Data sharing can inform community health assessment activities as well as the evaluation of public health programs.
The public health workforce is aging and lacks the key skills necessary to fully transition. In its most recent survey of the public health workforce, the Association of State and Territorial Health Officers found that 70% of state-level public health workers were aged >40 years, and <20% of them possessed formal training in public health.15 Furthermore, 1 in 5 state employees plans to retire by 2023. The survey also found that few health departments employ informatics specialists who can harness the power of advanced computing systems and data science techniques.16 Public Health 3.0 demands training of more public health workers to replace those retiring, and they need to be empowered with the knowledge and skills to lead the transformation of the public health system.
Engagement with partners to address the social determinants, expanded infrastructure to modernize methods as well as tools, and the development of the workforce needed to realize Public Health 3.0 will require significant new investment. Returning to existing or lower levels of funding after the COVID-19 pandemic is a secondary disaster for America. Instead of cutting public health programs or jobs, policymakers need to commit to funding both recovery and sustained public health preparedness, including replenishing the national stockpile. The NAM recommends doubling investment in public health.4 A bill introduced in the U.S. Senate proposes investing $100 million per year for 10 years in the public health infrastructure to modernize information systems and the public health workforce.17
In addition to PHEP, investment is needed in the full range of public health and social programs, including nutrition, housing, immunization, screening, and economic security programs that strengthen communities and address social determinants. There are immense social and mental health needs among individuals impacted by COVID-19, including millions who never became infected. Individuals have lost jobs, and others are on the verge of losing their home or becoming evicted. Although jobs might be regained, stress and suffering will exact a toll on the population for decades. Moreover, vulnerable populations decimated financially will need to rely more heavily on the public health system for care until other insurance options become available.
Finally, evolution will require bold leadership from public health and medicine. The 3 decades after the first NAM report on the future of public health, only half of the nation's state health officers have formal public health training before their appointment,18 requiring a longer learning curve to be effective. The average tenure is 4.1 years (median=2.9 years), and every year, 12 states replace their state health officers.19 If the nation is to achieve the goal of public health leaders serving as chief health strategists as suggested in Public Health 3.011 in which they architect solutions in partnership with healthcare and other sector leaders, the lack of experienced senior leadership must be addressed seriously. This includes applying the Association of State and Territorial Health Officers workforce recommendations to implement leadership training with current and future public health leaders.20
CONCLUSIONS
The U.S. public health system is frail. Response to COVID-19 exposed a myriad of weaknesses. The health system and political leaders must take bold action after COVID-19 to seriously address the challenges. The Public Health 3.0 framework provides a road map for a stronger, evolved public health system. The words of Gostin et al.21 remain valid today, “Achieving a highly functioning governmental public health system is difficult; the necessary tasks are technically within our reach but require political will.”
ACKNOWLEDGMENTS
The authors thank Mrs. Jennifer Williams, MPH, of the Regenstrief Institute for her help in gathering data on public health emergency preparedness data presented in this essay.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Cortez M, Tozzi J, Bloomberg What happened to the CDC? The storied disease agency is taking a back seat in the U.S. response to the coronavirus. Fortune. April 12, 2020 https://fortune.com/2020/04/12/cdc-coronavirus-testing-us-covid-19-response-trump-american-government/ [Google Scholar]
- 2.Stein M. The federal response to Covid-19 we should have expected. Public Health Post. May 6, 2020 https://www.publichealthpost.org/viewpoints/the-federal-response-to-covid-19-we-should-have-expected/ [Google Scholar]
- 3.Trust for America's Health . Trust for America's Health; Washington, DC: Published April 2019. The impact of chronic underfunding on America's public health system: trends, risks, and recommendations, 2019.https://www.tfah.org/wp-content/uploads/2020/03/TFAH_2019_PublicHealthFunding_07.pdf [Google Scholar]
- 4.Institute of Medicine . The National Academies Press; Washington, DC: 2012. For the Public's Health: Investing in a Healthier Future. [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine . The National Academies Press; Washington, DC: 2003. The Future of the Public's Health in the 21st Century. [DOI] [Google Scholar]
- 6.Schroeder J, Bouldin ED. Inclusive public health preparedness program to promote resilience in rural Appalachia (2016-2018) Am J Public Health. 2019;109(suppl 4):S283–S285. doi: 10.2105/AJPH.2019.305086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Devi S. U.S. public health budget cuts in the face of COVID-19. Lancet Infect Dis. 2020;20(4):415. doi: 10.1016/S1473-3099(20)30182-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hirsch L, Dzhanova Y. Coronavirus response hurt by lack of funding for public health labs, CDC director tells Congress. CNBC. March 10, 2020 https://www.cnbc.com/2020/03/10/coronavirus-testing-delays-caused-in-part-by-underfunding-cdc-director-says.html [Google Scholar]
- 9.Statistics and research: coronavirus (COVID-19) testing. Our World in Data.https://ourworldindata.org/coronavirus-testing. Updated June 9, 2020. Accessed June 10, 2020.
- 10.Regenstrief COVID-19 dashboard. Regenstrief Institute.https://www.regenstrief.org/covid-dashboard/. Updated June 9, 2020. Accessed June 10, 2020.
- 11.DeSalvo KB, O'Carroll PW, Koo D, Auerbach JM, Monroe JA. Public health 3.0: time for an upgrade. Am J Public Health. 2016;106(4):621–622. doi: 10.2105/AJPH.2016.303063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vest JR, Caine V, Harris LE, Watson DP, Menachemi N, Halverson P. Fostering local health department and health system collaboration through case conferences for at-risk and vulnerable populations. Am J Public Health. 2018;108(5):649–651. doi: 10.2105/AJPH.2018.304345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dixon BE, Rahurkar S, Apathy NC. Interoperability and health information exchange for public health. In: Magnuson JA, Dixon BE, editors. Public Health Informatics and Information Systems. 3rd ed. Springer; Cham, Switzerland: 2020. pp. 307–324. [DOI] [Google Scholar]
- 14.Black J, Hulkower R, Suarez W, Patel S, Elliott B. Public health surveillance: electronic reporting as a point of reference. J Law Med Ethics. 2019;47(2 suppl):19–22. doi: 10.1177/1073110519857309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bogaert K, Castrucci BC, Gould E. The Public Health Workforce Interests and Needs Survey (PH WINS 2017): an expanded perspective on the state health agency workforce. J Public Health Manag Pract. 2019;25(2 suppl):S16–S25. doi: 10.1097/PHH.0000000000000932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McFarlane TD, Dixon BE, Grannis SJ, Gibson PJ. Public health informatics in local and state health agencies: an update from the Public Health Workforce Interests and Needs Survey. J Public Health Manag Pract. 2019;25(2 suppl):S67–S77. doi: 10.1097/PHH.0000000000000918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.S.1973, 116th Cong. 1st Sess. 2019. Saving Lives Through Better Data Act. [Google Scholar]
- 18.Yeager VA, Menachemi N, Jacinto CM. State health officials: backgrounds and qualifications. J Public Health Manag Pract. 2020;26(1):9–15. doi: 10.1097/PHH.0000000000000937. [DOI] [PubMed] [Google Scholar]
- 19.Halverson PK, Lumpkin JR, Yeager VA, Castrucci BC, Moffatt S, Tilson H. High turnover among state health officials/public health directors: implications for the public's health. J Public Health Manag Pract. 2017;23(5):537–542. doi: 10.1097/PHH.0000000000000639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Becker SJ, Hannan C, Robitscher JW. A win for workforce development: the value of PH WINS for ASTHO affiliates. J Public Health Manag Pract. 2019;25(2 suppl):S177–S179. doi: 10.1097/PHH.0000000000000970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gostin LO, Boufford JI, Martinez RM. The future of the public's health: vision, values, and strategies. Health Aff (Millwood) 2004;23(4):96–107. doi: 10.1377/hlthaff.23.4.96. [DOI] [PubMed] [Google Scholar]