Abstract
An elderly woman underwent hardware removal and total joint replacement (TJR) of her right knee. Ipsilateral total tip replacement was performed 7 years earlier, and 12 months later, a supracondylar fracture of the index femur was successfully treated by open reduction internal fixation (ORIF) of the distal femur with a locking compression plate condylar plate. Hardware removal attempt, prior to the arthroplasty, resulted in fracture of the distal femur. Total knee replacement (TKR) was commenced with temporary reduction and final stabilisation of the femur fracture with a condylar plate. Postoperatively, non-union of the femur fracture developed twice with fatigue failure of the plate fixation device in both instances. Refixation of the femur was performed on both occasions and additional bone healing augmentation measures were performed for each subsequent surgery. Femur union was achieved fourteen months after the last surgery.
Keywords: orthopaedic and trauma surgery, osteoarthritic knww
Background
Primary knee osteoarthritis with history of trauma involving long bone fractures around the knee, inevitably introduces soft tissue scarring, interferes with implanted hardware, and at times, necessitates multiple subsequent surgeries, all of which compounding the clinical complexity in candidates for knee arthroplasty.1 The treatment strategy should be tailored individually since each case is unique. Evaluation of risk factors, surgical technique and morbidity is required to achieve a favourable ‘cost-effective’ clinical result.
Distinguishing patients prescribed for total knee replacement (TKR) with a ‘superimposed condition’ is vital. Whether a primary disease in elderly people with a history of geriatric fracture fixation, or conditions resulting in secondary joint disease associated with extra-articular deformities such as in skeletal dysplasia or post-traumatic arthritis found in ‘mangled limb’, all such conditions pose considerable technical difficulties and increase the potential for joint replacement surgery complications.2 3
Case presentation
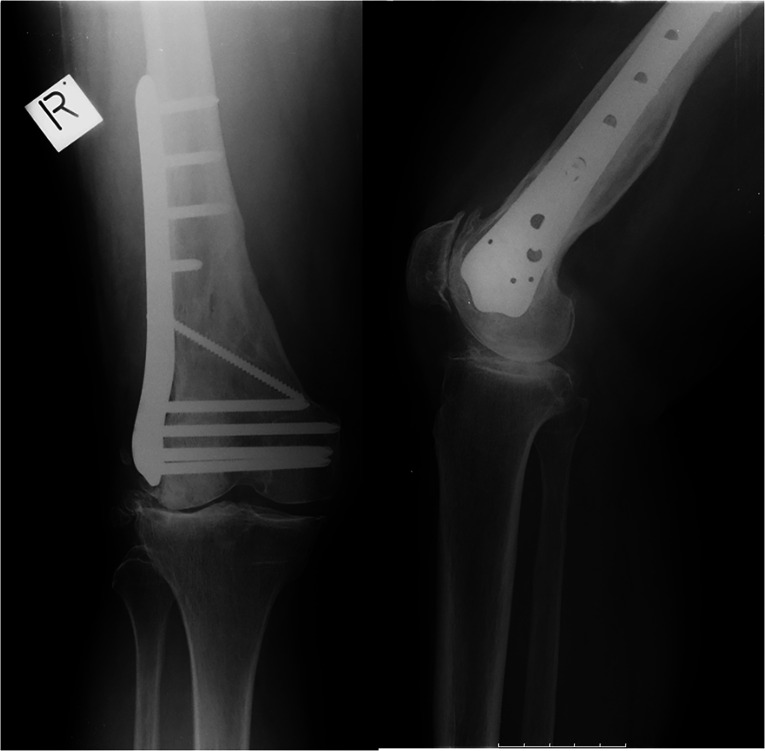
An 80-year-old female patient with constitutional valgus was electively admitted for right knee joint replacement due to aggravated pain due to primary osteoarthritis involving the lateral compartment and patellofemoral joint (figure 1).
Figure 1.
Standing X-ray of knees shortly prior to total knee replacement (TKR).
Seven years earlier, she underwent a right total tip replacement (THR). One year afterward, she fell from a standing position resulting in a supracondylar fracture of the ipsilateral femur; she subsequently underwent open reduction internal fixation (ORIF) with a condylar plate (locking compression plate—LCP, DePuy Synthes, Zuchwil, Switzerland).
Uneventful follow-up with slightly delayed union ensued at 7 months. Review of her medical records indicated that she had been undergoing osteoporosis treatment with bisphosphonates for the 4 years prior to the fracture. After an extensive endocrine workup, her prolonged bisphosphonate treatment was interrupted and had been changed to recombinant parathyroid hormone (teriparatide).4
Numerous risk factors had to be taken into consideration for this patient, related to the surgery itself, healing potential and possible complications due to reduced bone mass, including: gender, eighth decade of life, presence of hardware, type II osteoporosis with recorded lengthy bisphosphonates treatment with possibly superimposed, chronic disuse osteopenia due to delayed long bone fracture healing, and prolonged painful degenerative joint disease. Multiple stress riser holes had been placed in the event of hardware removal from the distal femur. Finally, the presence of the ipsilateral THR stem had to be taken into account, in the event that a stemmed femoral implant was chosen for TKR, which could have an increased stress transfer effect on the intercalating bone segment.
Treatment
During the surgery, a lateral incision that traced the old surgical scar was made in an attempt to remove the LCP plate, for femoral guide rod insertion into the medullary canal for the TKR. Difficulties were encountered via this approach due to a worn hex head screw hole socket; another screw breakage with complete detachment of the screw head necessitated ‘broken screw extractor set’ usage, a carbide drill and special tools for complete hardware removal. These efforts resulted in iatrogenic intraoperative fracture of the femur.
TKR (DePuy Sigma, J&J, Warsaw, Indiana, USA) commenced through a separate midline skin incision and medial parapatellar arthrotomy. The femoral guide rod was initially used to maintain temporary fracture reduction. The rod was introduced just enough into the remaining tubular bone proximal to the fracture site and distal to the femoral stem of the THR, to achieve satisfactory temporary fracture alignment, and to provide the possibility of a measured distal femoral cut for TKR. Finally, the fracture site was reinforced with bone clamps in preparation for the subsequent internal fixation.
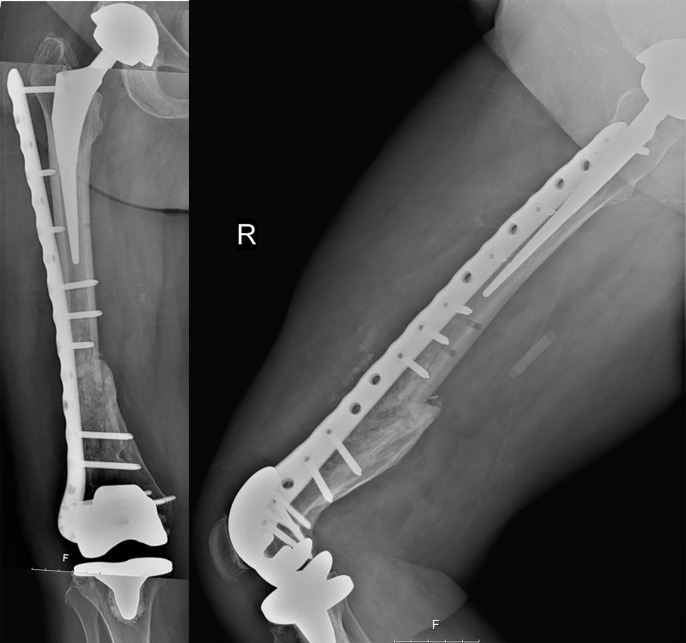
New full draping was necessary before performing the fracture fixation, since the tourniquet had to be removed in order to gain access to the proximal part of the thigh for the osteosynthesis. Refixation of the femur was performed with a periprosthetic condylar plate (non-contact bridging—NCB, Zimmer Biomet, Warsaw, USA) spanning the full femur length from the trochanter, with unicortical screws along the femoral stem of the THR, to the distal femur, augmented with allogenic bone graft (Grafon TBF, France). The X-ray demonstrated good alignment in the coronal plan, but some retroversion of the distal fragment in the lateral view with inadequate reduction and lack of sufficient contact between bone fragments (figure 2). The recorded operating time was 7 hours and 6 min. The patient was instructed to observe restricted weight bearing to ‘toe-touch’ for 6 weeks with a mandatory walker, while permitting range of motion of the knee as tolerated under supervised physiotherapy.
Figure 2.
Postoperative radiograph of right (RT). Femur following simultaneous total knee replacement (TKR) and open reduction internal fixation (ORIF).
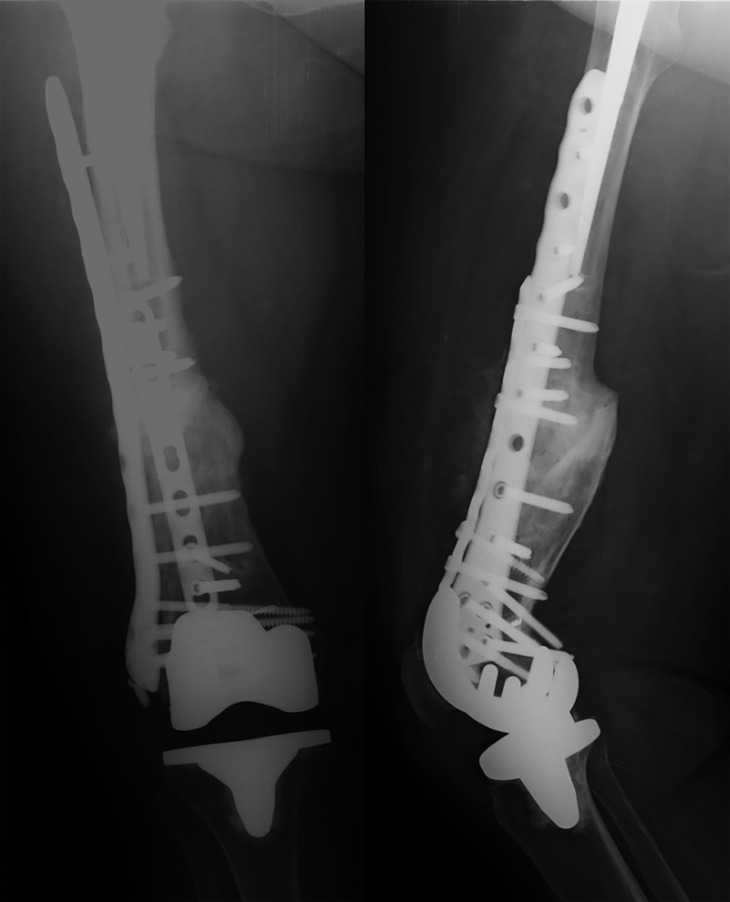
Seven months following surgery, the patient experienced an episode of acute pain. A periprosthetic fracture at a nonunion site of the femur with plate breakage due to fatigue failure was diagnosed. Following removal of the broken plate, refixation of the femur with a new periprosthetic NCB plate augmented with bone marrow aspirate concentrate (BMAC) (Harvest Terumo BCT, USA) was performed (figure 3). Tissue samples sent for culture were all negative.
Figure 3.
Non-union of femur with breakage of the plate at 7 months from surgery.
Ten months later, she experienced another episode of acute pain. X-ray demonstrated a second fatigue breakage of the NCB plate resulting from nonunion of the femur. Removal of the broken plate was followed by refixation of the femur with an LCP plate, additionally augmented with an low contact dynamic compression plate (LC-DCP) plate on the anterior cortex of the femoral shaft. Both BMAC and allogenic bone were supplemented to stimulate callus formation. At 14 months, solidly mineralised callus formation was observed (figure 4).
Figure 4.
Ten months from third and last surgery. Well-observed callus formation.
Finally, in retrospect, a detailed review of the patient’s record revealed a medical consultation by an orthopaedic surgeon, 3 months prior to the index operation, elaborating the rationale and recommending total knee replacement with patient-specific instrumentation (PSI) and hardware retention.
Outcome and follow-up
Substantial callus formation was observed at fourteen months after the final surgery (figure 4). The patient resumed ability to walk with a single crutch and maintains an independent life style including basic outdoor activities.
At 4 years follow-up, during which three major operations were performed within 2.5 years, the patient was fully independent and able to walk freely around the house. She demonstrated a leg length discrepancy of 1.5 cm with a very slight limp and active range of knee motion of 0°–100°. Walking aids were in use intermittently in the house.
Discussion
It is essential to be alert to the warning signs that can present in elderly patients with a history of old, well fixed, healed and properly aligned fracture of the distal femur with retained hardware, who are scheduled for conventional TKR due to relentless painful osteoarthritis.5
In itself, intraoperative fracture of the femur is a major complication and marks a dramatic shift of events. This is even more so when the inherent basic conditions are strained by poor bone quality, a single possible surgical option—plating, and the presence of proximal THR and distal TKR. However, regardless of the surgical hardship, anatomic reduction and quality osteosynthesis is ever more important and less forgiving when absent. Malreduction, poor bone quality, extensive exposure and inadequate reduction and fixation, all represent biological and biomechanical deficiencies, which increase non-union risk.6 The outcome of fatigue metal failure, as eventually occurred repeatedly in the case analysed herein, is inevitable. Fracture healing, in hindsight, was obtained only on the second revision when the LCP was further supplemented with an anterior plate, assuming better stability with a so-called ‘strut effect,’ augmented massively with bone growth stimulants. Biological healing was achieved with sagittal plane malunion.7
Furthermore, the risk factors pertaining to an individual patient are clearly of key importance during preoperative planning, particularly when involving advanced age, female gender, the presence of hardware from previous surgery and type II osteoporosis under lengthy treatment with bisphosphonates, all of which have a compounding influence on risk in a single stage conventional TKR approach.8 Hardware removal is recognised as potentially difficult and time consuming due to cold welding, metal breakage and screw head stripping, with a reported average increased operating time of 71.3 min per procedure.6 9 Multiple screw holes remaining in an already weakened bone, as well as the presence of THR stem concomitantly, may synergistically act as stress riser on the intercalating bone segment endangering structural integrity.10 The presence of so many risk factors makes it mandatory to anticipate potential problems prior to surgery to ensure adequate risk management planning. Careful preplanning, access to special tools, extramedullary femoral guide,7 backup fluoroscopy and alternative plans such as the readily available possibility for upgrading the constraint level of the implant are elementary ‘bail out’ requirements in such complex patients and projected difficulties.11
Undertaking a conventional approach to knee arthroplasty, where hardware removal is mandatory, even a flawless procedure inherently increases the magnitude of the operation in terms of surgery time, morbidity, infection, blood loss, pain duration pain and potential postoperative complications.12 13
In complex cases, risk–benefit options should be weighed and solutions should be tailored. A staged procedure with hardware removal, and second-stage arthroplasty, is safe, although it involves two operations with the resulting prolonged discomfort. The use stemmed femoral implants to bridge stress rising holes, following plate removal with or without bone graft, is possible in a single operation; however, medullary canal preparation for stem insertion could be prolonged and not entirely risk free. Furthermore, in the case of a stemmed femur in TKR, attention to stress elevation created by ‘tip-to-tip’ proximity of both TKR and ipsilateral THR should be noted, as the risk for structural failure increases with the elevated forces exerted on the intercalating bone segment, with its resistance dependent on the length of the intercalating bone segment and its tissue quality.10 Alternatively, the possibility for metal removal and primary simple TKR in favour of reduced operating time remain applicable but highly risky.14 An extramedullary femoral aiming device is an option for avoiding hardware removal. Although well described as being as efficient as intramedullary devices in restoring TKA alignment,15 it has not achieved widespread routine practice.16 Nowadays, advanced technologies offer the possibility to perform TKR with primary implants and hardware retention. It is well established that hardware retention is possible, without negatively impacting knee arthroplasty.17 Restoring lower limb mechanical alignment by neutralising (bypassing) instead of correcting extra-articular deformities by osteotomy or removing hardware is a prominent feature of modern preplanning technologies. In either case, extending the operation in order to gain access to the medullary canal of the femur, as would be required in a conventional setup, is redundant,9 thereby minimising risk of undue complications.5
Preoperative planning tools vary from computer-aided design software to PSI,3 computer navigation (CAS),18 and robotic arms, all subject to availability and surgeon’s experience.
Of the technologies available, in our view, CT three-dimensional (3-D) imaging reconstruction followed by high-quality dynamic graphical presentation is a powerful tool in the hand of the surgeon. It offers a high predictive value, displaying ideal sizing, positioning, possible collision points between retained hardware and implant alignment restoration, making it an ideal tool for implantation planning.
Translated by rapid prototyping technology (3-D printing) into operating jigs, PSI is currently the safest approach to complex TKR.19 20 Finally, with PSI the entire preplanning is outside the operating theatre in neutral conditions, unlike computer assisted surgery (CAS) or robotic arms, where calibrations and resolving dilemmas occur in real time intraoperative activity.
Patients with extensive medical and surgical backgrounds who are candidates for knee arthroplasty due to osteoarthritis must undergo detailed evaluation, since the knee joint is often deformed, the periarticular structures are inaccessible, and bone and soft tissue quality is poor.
A single-stage conventional approach in these patients requires careful planning and foresight with preparation of backup strategies to avoid and resolve complications so as to provide successful results under unfavourable conditions.
The question of whether such complications are preventable is critical. In most similar cases, such as the one looked at herein, the answer is yes. PSI would have provided useful information and practical solutions to many of the problems encountered herein. Therefore, we recommend considering PSI as a first-line treatment for patients presenting with extra-articular problems compounding the degenerative joint disease.
Learning points.
Preoperative planning is paramount where individual tailored solutions are necessary.
Patient’s general (osteoporosis), regional (total tip replacement + distal plate) and local (knee) risk factors are equally important when challenging surgery is expected.
Hardware removal should be avoided or minimised.
Patient-specific instrumentation is recommended as a useful tool for similar cases.
Footnotes
Contributors: GN: chief knee reconstruction surgeon; reporting; concept and design of manuscript. AAE: reporting; data acquisition. EK: junior trauma surgeon; concept and design of manuscript; editing; follow-up. DN: chief trauma surgeon; reporting; follow-up. All authors made a substantial contribution to the debriefing of this complicated case and bringing this case report and paradigm analysis to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Volpin G, Dowd GS, Stein H, et al. Degenerative arthritis after intra-articular fractures of the knee. long-term results. J Bone Joint Surg Br 1990;72:634–8. [DOI] [PubMed] [Google Scholar]
- 2.Bala A, Penrose CT, Seyler TM, et al. Outcomes after total knee arthroplasty for post-traumatic arthritis. Knee 2015;22:630–9. 10.1016/j.knee.2015.10.004 [DOI] [PubMed] [Google Scholar]
- 3.Mattei L, Pellegrino P, Calò M, et al. Patient specific instrumentation in total knee arthroplasty: a state of the art. Ann Transl Med 2016;4:126. 10.21037/atm.2016.03.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koh A, Guerado E, Giannoudis PV. Atypical femoral fractures related to bisphosphonate treatment. Bone Joint J 2017;99-B:295–302. 10.1302/0301-620X.99B3.BJJ-2016-0276.R2 [DOI] [PubMed] [Google Scholar]
- 5.Shearer DW, Chow V, Bozic KJ, et al. The predictors of outcome in total knee arthroplasty for post-traumatic arthritis. Knee 2013;20:432–6. 10.1016/j.knee.2012.12.010 [DOI] [PubMed] [Google Scholar]
- 6.Ebraheim NA, Kelley LH, Liu X, et al. Periprosthetic distal femur fracture after total knee arthroplasty: a systematic review. Orthop Surg 2015;7:297–305. 10.1111/os.12199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peschiera V, Staletti L, Cavanna M, et al. Predicting the failure in distal femur fractures. Injury 2018;49:S2–7. 10.1016/j.injury.2018.10.001 [DOI] [PubMed] [Google Scholar]
- 8.Benazzo F, Rossi SMP, Ghiara M, et al. Total knee replacement in acute and chronic traumatic events. Injury 2014;45:S98–104. 10.1016/j.injury.2014.10.031 [DOI] [PubMed] [Google Scholar]
- 9.Veltman ES, van Wensen RJA, Defoort KC, et al. Single-Stage total knee arthroplasty and osteotomy as treatment of secondary osteoarthritis with severe coronal deviation of joint surface due to extra-articular deformity. Knee Surg Sports Traumatol Arthrosc 2017;25:2835–40. 10.1007/s00167-015-3889-9 [DOI] [PubMed] [Google Scholar]
- 10.Krbec M, Motycka J, Lunácek L, et al. [Osteosynthesis for periprosthetic supracondylar fracture above a total knee arthroplasty using a locking compression plate]. Acta Chir Orthop Traumatol Cech 2009;76:473–8. [PubMed] [Google Scholar]
- 11.Bohm ER, Tufescu TV, Marsh JP. The operative management of osteoporotic fractures of the knee. J Bone Joint Surg Br 2012;94-B:1160–9. 10.1302/0301-620X.94B9.28130 [DOI] [PubMed] [Google Scholar]
- 12.Birjandinejad A, Ebrahimzadeh MH, Sayyed-Hosseinian S-H, et al. Prognostic factors affecting the results of modified thompson Quadricepsplasty for the treatment of extension contracture of the knee. Arch Bone Jt Surg 2017;5:109–13. [PMC free article] [PubMed] [Google Scholar]
- 13.Böstman OM. Refracture after removal of a condylar plate from the distal third of the femur. J Bone Joint Surg Am 1990;72:1013–8. 10.2106/00004623-199072070-00009 [DOI] [PubMed] [Google Scholar]
- 14.Suzuki T, Smith WR, Stahel PF, et al. Technical problems and complications in the removal of the less invasive stabilization system. J Orthop Trauma 2010;24:369–73. 10.1097/BOT.0b013e3181c29bf5 [DOI] [PubMed] [Google Scholar]
- 15.Tang Q, Shang P, Zheng G, et al. Extramedullary versus intramedullary femoral alignment technique in total knee arthroplasty: a meta-analysis of randomized controlled trials. J Orthop Surg Res 2017;12:82. 10.1186/s13018-017-0582-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Phillips AM, Goddard NJ, Tomlinson JE. Current techniques in total knee replacement: results of a national survey. Ann R Coll Surg Engl 1996;78:515. [PMC free article] [PubMed] [Google Scholar]
- 17.Manzotti A, Pullen C, Cerveri P, et al. Post traumatic knee arthritis: navigated total knee replacement without hardware removal. Knee 2014;21:290–4. 10.1016/j.knee.2012.06.008 [DOI] [PubMed] [Google Scholar]
- 18.Batash R, Rubin G, Lerner A, et al. Computed navigated total knee arthroplasty compared to computed tomography scans. Knee 2017;24:622–6. 10.1016/j.knee.2017.03.006 [DOI] [PubMed] [Google Scholar]
- 19.Thienpont E, Bellemans J, Victor J, et al. Alignment in total knee arthroplasty, still more questions than answers…. Knee Surg Sports Traumatol Arthrosc 2013;21:2191–3. 10.1007/s00167-013-2622-9 [DOI] [PubMed] [Google Scholar]
- 20.Thienpont E, Paternostre F, Pietsch M, et al. Total knee arthroplasty with patient-specific instruments improves function and restores limb alignment in patients with extra-articular deformity. Knee 2013;20:407–11. 10.1016/j.knee.2013.07.001 [DOI] [PubMed] [Google Scholar]