Abstract
Intra-articular steroid injections are widely prescribed for management of osteoarthritis when oral medication or physiotherapy treatment fails to relieve patient’s pain. Septic arthritis is an uncommon side effect of steroid injection. Common causal micro-organisms are bacterial with Staphylococcus aureus being the most frequent. Fungal septic arthritis is rare and does not usually present beyond the neonatal period. We present a rare case of septic arthritis secondary to fungal infection.
Keywords: infections, musculoskeletal and joint disorders, degenerative joint disease, osteoarthritis, orthopaedic and trauma surgery
Background
The risk of acquiring septic arthritis post intra-articular injection has been reported 1 in 3000 to 1 in 50 000.1 The risk of acquiring infection post steroid intra-articular injection has not increased however, the incidence has increased. Due to a growing ageing population, more patients are being treated for osteoarthritis. When conservative treatment such as painkillers and physiotherapy fails, physicians often prescribe intra-articular steroid injection as part of the stepwise management. We present a rare case of septic arthritis post intra-articular injection in native joint caused by Candida albicans, to increase awareness among physicians and evaluate current management given limited data.
Case presentation
A 66-year-old woman with no significant medical history presented with right hip pain. The patient’s body mass index was 33 but she did not suffer from diabetes mellitus. A recent glycosylated haemoglobin measured 38 mmol/mol which was within normal range. She presented with increasing right hip pain despite physiotherapy and oral painkillers. She was reviewed by rheumatology who diagnosed her with osteoarthritis. A pelvis radiograph, showed mild narrowing of both hip joints with subchondral sclerosis(white arrow) suggestive of background mild osteoarthritis (figure 1). Given lack of response to oral painkillers, she was referred for intra-articular steroid injection. The procedure was performed under strict aseptic technique and prior to injection, the skin overlying the hip joint was visually inspected and no evidence of intertrigo or clinical redness was detected. The skin surface was then cleaned with copious amounts of 0.5% chlorhexidine.
Figure 1.
Pelvis radiograph shows slight asymmetrical narrowing of the right hip joint with associated subchondral sclerosis suggestive of osteoarthritis.
Under fluoroscopic imaging, her right hip joint was marked and 5 mL of 1% lidocaine was administered locally, followed by a non-compounded intra-articular injection of 40 mg triamcinolone diluted with 6 mL of 0.25% bupivacaine drawn from a single vial. Approximately 2 months after the intra-articular steroid injection, patient attended the emergency department with the symptoms of increasing severity of pain, extending to the groin and ankle.
Patient was afebrile with no clinical evidence of joint swelling or erythema. She had no history of candida infection; skin, mucosal or vaginal. Blood results revealed normal levels of peripheral white cell count; however, C reactive protein (CRP) was elevated at 54 mg/L. Given lack of clinical sepsis, patient was treated with painkillers only and sent home. However, the pain worsened making the patient represent with debilitating pain. On the second visit to emergency, a pelvis radiograph was performed.
Investigations
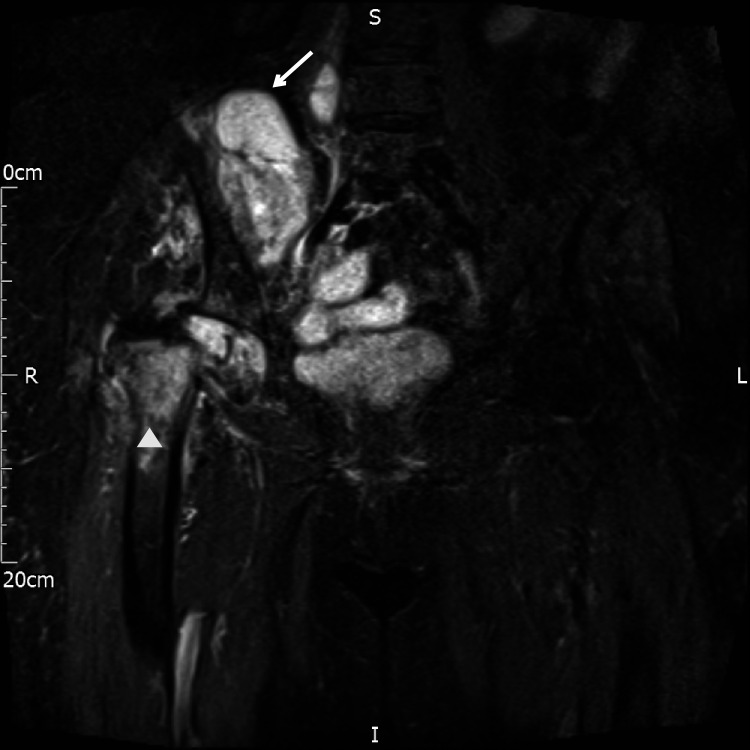
Based on raised inflammatory markers and increasing joint pain, a repeat pelvis radiograph was performed which revealed complete destruction of the right femoral head with superolateral migration of the proximal femur (figure 2). Subsequently a CT abdomen and pelvis was performed which confirmed findings of destruction of the right femoral head(white arrow) and revealed a large, loculated collection within the right hip with a calcified focus within the right iliopsoas bursa consistent with migrated fractured component of the right femoral head (figure 3). MRI pelvis demonstrated extensive destruction of the right femoral head with marrow changes in the intertrochanteric region of the proximal femur and acetabulum consistent with septic arthritis (figure 4).
Figure 2.
Follow-up pelvis radiograph shows destruction of the right femoral head with superolateral migration of the proximal femur.
Figure 3.
Coronal view of CT demonstrates the extent of the rim enhancing right iliopsoas collection (arrow) with remnant femoral head (arrowhead).
Figure 4.
MRI pelvis coronal Turbo inversion recovery magnitude sequence reveals marrow changes in the intertrochanteric region of the proximal femur and acetabulum (arrowhead). The right femoral head is collapsed and loculated right iliopsoas collection (arrow).
Treatment
Patient had percutaneous drainage of the right hip and iliopsoas collection followed by radical hip debridement with insertion of a temporary antibiotic loaded cement spacer. Purulent aspirates taken when the drainage was inserted while debrided material and bone scrapings attained during the surgery, were both sent for microbiology and culture. However, only debrided material and bone scrapings were positive for fungal infection.
Based on initial diagnostic imaging of septic arthritis, she was empirically treated for bacterial infection with 4 weeks of vancomycin 15 mg/kg intravenous four times a day and piperacillin-tazobactam 4.5 mg intravenous three times a day. However, candida was cultured from the surgical biopsy samples. Based on multidisciplinary discussion and microbiology advise, patient was treated with 400 mg oral fluconazole for 6 months.
Outcome and follow-up
Patient is currently being treated with 6 months oral fluconazole and is having monthly bloods checking her inflammatory markers; CRP which have been running low at 15. On completion of her antifungals she will be treated in an expectant manner for her pending hip replacement.
Discussion
The incidence of septic arthritis secondary to intra-articular intervention is low and stands at approximately 0.002%–0.01% per annum.1 However, the total number of septic arthritis has increased as intra-articular injections are currently more widely prescribed although the risk of infection per injection has remain unchanged.2
Patients who are at risk of septic arthritis include those with chronic medical conditions such as diabetes, chronic renal disease, pre-existing prosthesis, intravenous drug users, rheumatoid arthritis, osteoarthritis including those who are pharmacologically suppressed.3
The most common causal pathogen is gram positive bacteria, notably Staphyloccocus aureus.1 Fungal infections are rare particularly in native joints. The most common fungal pathogens are Candida and Aspergillus.4 5 Unlike bacterial infection which typically presents with an acute infection such as increased inflammatory markers and raised white cell count. The clinical course of fungal septic arthritis is variable and can be indolent in up to a third of cases.6 Such indolent cases are difficult to diagnose, as inflammatory markers can be normal. Usually, the main presenting symptom is worsening pain. The absence of fever and septicaemia does not exclude septic arthritis.7 8
Given its insidious presentation, fungal septic arthritis should be excluded in patients who have had recent joint intervention as the hip particularly is susceptible to contiguous spread rather than haematogenous spread.
Management of septic arthritis, particularly fungal in aetiology, often requires a combined approach of pharmacology and surgery. Surgical debridement is dependent on severity of infection. Debridement is important to remove necrotic and disease bone to reduced organism burden and improve efficacy of antifungals. It is paramount to check susceptibility to ensure the best antifungal treatment is given. Most C. albicans isolates are susceptible to fluconazole and amphotericin B.8 Data on length of treatment is limited with few guidelines for management of such infections and is very much institution based and case basis.
Patient’s perspective.
I was reviewed in A&E on three separate occasions but on each occasion the doctors diagnosed my condition as sciatica and gave me stronger pain killers and failed to realise the worsening pain was a complication of the steroid injection I had received. Obviously, mine is a rare case but given increased prevalence of infections from intra-articular injections, awareness of this complication should be emphasize as early detection is of utmost importance and will prevent debilitating conditions.
Learning points.
Despite low risk involved in intra-articular steroid injections, clinicians have to recognise the increasing prevalence of septic arthritis post injection and be aware of the insidious clinical presentation of fungal septic arthritis.
Patients presenting with osteoarthritis, categorically have immunocompromised status similar to other conditions such as rheumatoid arthritis, diabetes, trauma and iatrogenic procedures. All these patients categorically have increased risk of developing of septic arthritis post procedure.
Aetiology of hip pain can be elusive, other causes such as muscle injury or tendinopathy needs to be excluded.
Footnotes
Contributors: SLC: drafted manuscript, acquisition, interpretation of data for the work and imaging data. Final approval of the version to be published; agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. JP: substantial contribution. Reported on patient initial imaging and followed patient up. Reviewed the manuscript. Final approval of the version to be published; agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. DJ: orthopaedic specialist that reviewed patient and managed care from time of diagnosis. Involved in revising manuscript critically for important intellectual content; final approval of the version to be published; and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. DM: substantial contributions to the conception of the work; or the acquisition of imaging, and critically revising the manuscript for important intellectual content; and final approval of the version to be published; and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.McGarry JG, Daruwalla ZJ. The efficacy, accuracy and complications of corticosteroid injections of the knee joint. Knee Surg Sports Traumatol Arthrosc 2011;19:1649–54. 10.1007/s00167-010-1380-1 [DOI] [PubMed] [Google Scholar]
- 2.Helito CP, Teixeira PRL, Oliveira PRde, et al. Septic arthritis of the knee: clinical and laboratory comparison of groups with different etiologies. Clinics 2016;71:715–9. 10.6061/clinics/2016(12)07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Geirsson AJ, Statkevicius S, Víkingsson A. Septic arthritis in Iceland 1990-2002: increasing incidence due to iatrogenic infections. Ann Rheum Dis 2008;67:638–43. 10.1136/ard.2007.077131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bariteau JT, Waryasz GR, McDonnell M, et al. Fungal osteomyelitis and septic arthritis. J Am Acad Orthop Surg 2014;22:390–401. 10.5435/JAAOS-22-06-390 [DOI] [PubMed] [Google Scholar]
- 5.Kohli R, Hadley S. Fungal arthritis and osteomyelitis. Infect Dis Clin North Am 2005;19:831–51. [DOI] [PubMed] [Google Scholar]
- 6.Mathews CJ, Coakley G. Septic arthritis: current diagnostic and therapeutic algorithm. Curr Opin Rheumatol 2008;20:457–62. 10.1097/BOR.0b013e3283036975 [DOI] [PubMed] [Google Scholar]
- 7.Tong SYC, Davis JS, Eichenberger E, et al. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev 2015;28:603–61. 10.1128/CMR.00134-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pappas PG, Kauffman CA, Andes DR, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the infectious diseases Society of America. Clin Infect Dis 2016;62:civ933. 10.1093/cid/civ933 [DOI] [PMC free article] [PubMed] [Google Scholar]