Abstract
While aneurysms of the internal mammary artery (IMA) complicate occasionally surgical procedures employing median sternotomy, or are associated with direct thoracic trauma, mycotic pseudoaneurysms of the vessel are rarely reported in the literature. We herein report a case of a 22-year-old man who developed a mycotic internal mammary artery pseudoaneurysm secondary to staphylococcal chest wall abscesses and was effectively treated by coil embolization. Additionally, the report provides a brief review focusing on the current state of treatment options for internal mammary artery aneurysms.
Keywords: Aneurysm, Coil embolization, Internal mammary artery
INTRODUTION
Medical literature provides scant reports of internal mammary artery (IMA) aneurysms, especially if they are of infectious origin. In general those vessel deformities have been described in patients with connective tissue disorders, infection, vasculitis, thoracic trauma and following median sternotomy or attempted subclavian venous puncture. Due to the risk of increasing in size and eventually pseudoaneurysmatic sac rupturing, treatment including various approaches is always recommended [1]. We report one case of staphylococcal left IMA pseudoaneurysm in a 22-year-old man, treated successfully by coil embolization.
The patient described here has consented to publication of all case details and associated images.
CASE REPORT
A 22-year-old man was admitted to our emergency department suffering of blunt thoracic trauma due to traffic accident. Clinical examination and performed radiological studies revealed fractures of multiple left-sided ribs, the sternum as well the Th11 and Th12 vertebral bodies. The patient was initially treated conservatively, but on the fifth day, he developed a left-sided pleural effusion, necessitating a thoracostomy tube. Additionally, there were subpectoral chest wall abscesses, which were surgically incised and drained. Blood as well pus cultures from the abscess cavities revealed the growth of Staphylococcus aureus; therefore, intravenous antistaphylococcal antibiotics were administered. However, in the further course, a control contrast-enhanced computed tomography (CT) scan demonstrated a big left IMA pseudoaneurysm (Fig. 1: white arrow) accompanied by an ipsilateral localized hemothorax (Fig. 1A–C). The effusion was drained again, and concerning the aneurysm, we preferred a minimally invasive treatment via coil embolization in order to avoid a potential extensive mobilization of the patient, contraindicated by his spinal injuries, while the positioning on the operating table in case of a surgical treatment through a lateral thoracotomy.
Figure 1.
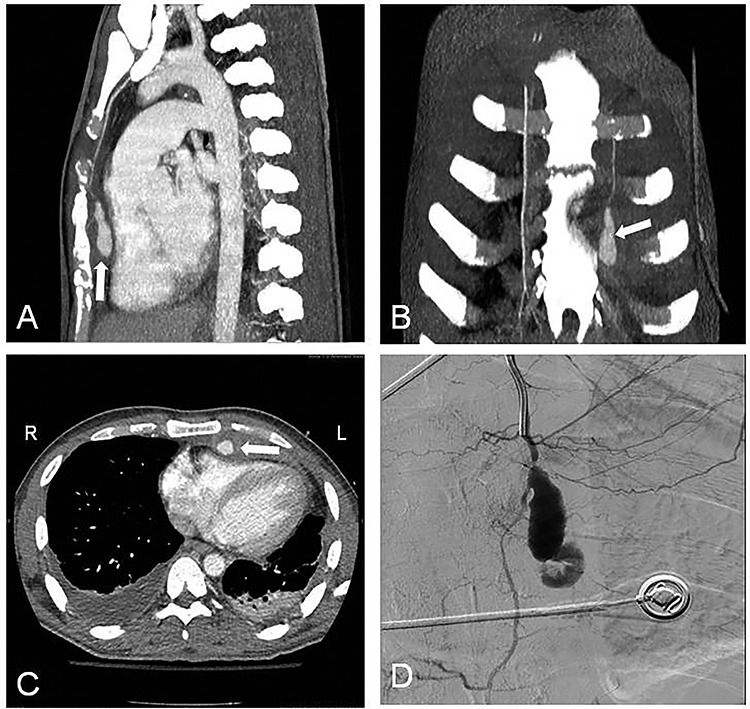
Contrast-enhanced CT with LIMA pseudoaneurysm (white arrow). (A) Sagittal plane; (B) coronal plane; (C) transverse plane with LIMA pseudoaneurysm (white arrow) and bilateral pleural effusions; (D) selective LIMA angiography demonstrating the aneurysm.
The embolization was performed after obtaining three consecutive negative blood cultures accompanied by a significant decrease of the laboratory infection parameters. The angiographic approach was done through the left brachial artery (Fig. 1D), and a microcatheter was placed into the aneurysm neck. Through coiling we aimed to occlude the IMA distally and proximally adjacent to the aneurysmatic sac, but attempts to cannulate the vessel distal to the aneurysm were unsuccessful. Therefore multiple (5x) coils were placed (VortX™ 35 (3×) and Complex Helical 18 (2×); Boston Scientific; Boston, MA, USA) into the aneurysmatic neck and sac (Fig. 2A).
Figure 2.
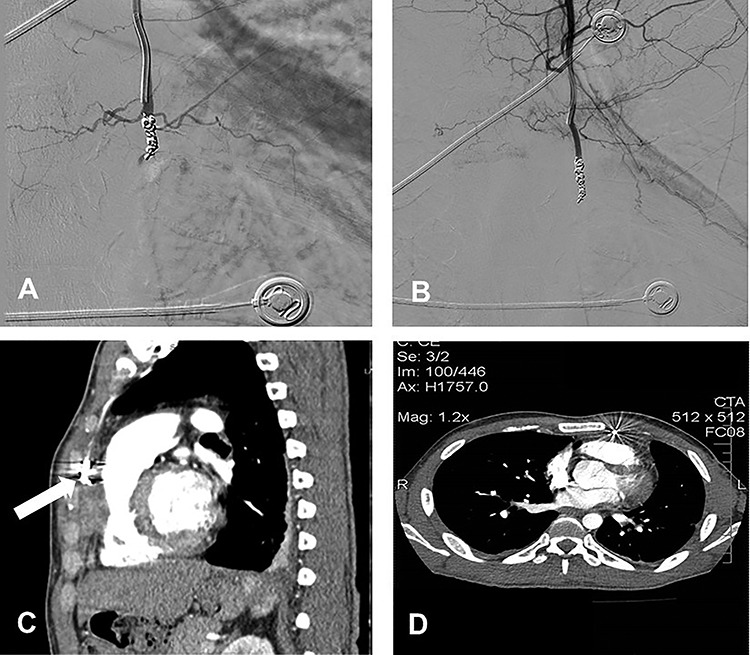
(A) Coil embolization of the aneurysm; (B) postembolization completion angiogram; (C) follow-up contrast-enhanced CT scan at 3 weeks after the embolization with complete regression of the pseudoaneurysm without flow into it (white arrow); (D) follow-up contrast-enhanced CT scan at 6 months after the embolization.
The completion angiogram demonstrated no filling in the coiled pseudoaneurysmal sac (Fig. 2B), while at follow-up 1, 3 weeks and 6 months after the procedure, CT scans showed initially shrinkage and finally complete regression of the pseudoaneurysm with no flow into it (Fig. 2C and D; white arrow). Early post-interventional course was unremarkable, and the patient was discharged after completing an intravenous antibiotic treatment over 6 weeks.
DISCUSSION
Although IMA aneurysms are occasionally observed secondary to thoracic trauma, cardiac surgical procedures including sternotomy, connective tissue disorders, vasculitis, fibromuscular hyperplasia and atherosclerotic disease [1], mycotic pseudoaneurysms of the vessel are even rarely reported in the literature [2, 3].
In general aneurysms may rupture and lead to arterial bleeding with subsequent hemomediastinum or hemothorax. In order to avoid these potentially catastrophic complications, treatment is mandatory in all cases once the diagnosis is established. Unspecific clinical signs indicating the presence of an IMA aneurysm are dyspnea, cough or hemoptysis accompanying usually a bulging chest mass. CT angiography with MDCT scan of the thorax represents the cornerstone in the diagnosis enabling exact size assessment and anatomical allocation of the aneurysm [4], while selective vessel angiography is on the one hand essential to localize the source of bleeding, in case of sac rupture, and on the other an important prerequisite for endovascular treatment [5].
In our patient the close vessel proximity to the concomitant subpectoral chest wall abscesses, as well as a potential traumatic insult during the abscess drainage and the history of blunt thoracic injuries, may have forced through hematogenous spreading an IMA wall involvement with subsequent pseudoaneurysm formation.
Reviewing the literature regarding the management of non-iatrogenic, non-traumatic IMA aneurysms and pseudoaneurysms (Table 1), there is a shift from the traditional surgical repair toward minimally invasive endovascular techniques including coil embolization [1–3, 5] and recently stent-graft repair [6, 7].
Table 1.
Literature review of case reports regarding non-iatrogenic/non-traumatic IMA aneurysms
| Author, year, [reference-citation] | Aneurysm location | Etiology | Treatment | Outcomes |
|---|---|---|---|---|
| Otter GD, 1978 | LIMA | Unknown | Exploratory thoracotomy and ligation of aneurysm | Uneventful recovery |
| Sanchez FW, 1985 | LIMA | CGD | Angiographic embolization | Uneventful recovery |
| Giles JA, 1990 | BL IMA | Polyarteritis nodosa | Thoracotomy with bilateral aneurysmectomy | Uneventful recovery |
| Wildhirt S, 1994 | RIMA | Atherosclerosis | Open ligation and resection | Uneventful recovery |
| Chan LW, 1996 | LIMA | No risk factors | Angiographic embolization, thoracotomy for hematoma evacuation | Uneventful recovery |
| Phan TG, 1998 | LIMA | Ehlers–Danlos syndrome | Thoracotomy with ligation of the LIMA, drainage of hemothorax | Uneventful recovery |
| Common AA, 1999 | LIMA | Marfan syndrome, previous MVC | Coil embolization | Uneventful recovery; died years later from type A dissection |
| Deshmukh H, 2001 [2] |
n: two pts LIMA RIMA |
Staphylococcal chest wall infection Tuberculous chest wall abscess |
Coil embolization Coil embolization |
Uneventful recovery Uneventful recovery; at 3-month follow-up successful aneurismal obliteration |
| Kim SJ, 2005 | LIMA | NF type I | Urgent coil embolization | Uneventful recovery; 2-month follow-up unremarkable |
| Dell’Amore A, 2006 | LIMA | Atherosclerosis | Surgical repair via median sternotomy due to interventional approach failure | Uneventful recovery |
| Urso S, 2007 | RIMA | NF type I | Emergent surgery with CPB due to rupture | Pt died during operation |
| Wani NA, 2010 [3] | LIMA | Pulmonary actinomycosis | Surgical repair planed | Pt died prior surgery |
| Rose JF, 2011 | LIMA | Marfan syndrome | Coil embolization | Uneventful recovery 4- and 9-month follow-up unremarkable |
| Ohman JW, 2012 | RIMA | Loeys–Dietz syndrome | Coil embolization | Uneventful recovery; At 24-month follow-up complete thrombosis of aneurysm |
| Okura Y, | RIMA | Idiopathic CMD | Surgical ligation and removal | Uneventful recovery; 1-year follow-up unremarkable |
| Sareli AE, 2012 | RIMA | NF type I | Emergent surgery due to rupture | Pt died due to anoxic brain injury |
| Lindblom RPF, 2013 | LIMA | Idiopathic or possibly very late post-traumatic | Emergent coil embolization | Uneventful recovery |
| Heyn J, 2014 | LIMA | Idiopathic | Open surgical resection | Uneventful recovery, at 6 months unremarkable |
| Burke C, 2015 | LIMA | SMAD3 mutation | Coil embolization | Uneventful recovery |
| Piffaretti G, 2015 [6] | LIMA | Sneddon’s syndrome | Stent-graft repair | Uneventful recovery, at 6 months: exclusion of aneurysm, patent ITA, absence of endoleak or edge stenosis |
| Ouldsalek EH, 2016 | LIMA | Unknown | Surgical resection | Uneventful recovery |
| Kwon OY, 2016 | RIMA | NF type I | Emergent staged management: coil embolization, and a subsequent VATS procedure | At 6 months: clinically asymptomatic |
| Alhawasli H, 2016 | BL IMA | Marfan syndrome | Endovascular stent-graft repair | Uneventful recovery, at 2-year follow-up: unremarkable |
| Nevidomskyte D, 2017 [7] | n: two pts (siblings) LIMA, RIMA | SMAD3 Mutation | Endovascular stent-graft repair | Uneventful recovery |
| Wong WJ, 2017 | RIMA | Idiopathic | Coil embolization | Uneventful recovery |
| Kim DW, 2017 | LIMA | NF type I | Emergent coil embolization | Uneventful recovery, at 18 months unremarkable |
| Almerey T, 2017 | RIMA | Idiopathic in the setting of aberrant subclavian artery | Coil embolization | Uneventful recovery, at 18 days unremarkable |
| Fujiyoshi T, 2018 | BL IMA | Marfan syndrome | Coil embolization | Uneventful recovery, 7-year follow-up completed |
| Ho K, 2018 | RIMA | Immunoglobulin G4-related | Hybrid surgical approach: open ligation of IMA origin and VAT-aneurysmectomy | Uneventful recovery |
| Miyazaki M, 2019 | RIMA | Related to previous DeBakey III acute aortic dissection | Surgical thoracoscopic resection | Uneventful recovery |
| Chen JF, 2019 | BL IMA | Heterozygous missense variant of unknown significance in COL5A1-gene and fibromuscular dysplasia | Coil embolization | Uneventful recovery |
| Mertens RA, 2020 | BL IMA | Marfan syndrome | Coil embolization, stent grafting of the left subclavian artery | Uneventful recovery |
Transcatheter embolization is performed using predominantly steel coils placed either within the aneurismal sac or in the feeding vessel [5], while IMA embolization distally to the pathology precludes retrograde collateral flow into the aneurysm [8]. Although this method is rapidly becoming the treatment of choice for arteriovenous fistulas and small aneurysms, some authors still advocate the classical surgical repair especially in bigger, wall-thinned, non-iatrogenic aneurysms, which enables complete ablation of the aneurysm, ensures long-term patient survival and provides histological information. Adjacent infective processes like anterior chest wall abscesses should be treated aggressively to prevent transthoracic infection spreading with subsequent vascular complications [2].
Nevertheless, indications for embolic coiling in case of mycotic aneurysms like in the presented case remain controversial and still under debate. The major concern is either the persistent infection or a reinfection of the coil fabric, constituting an unresolved issue in patients with ongoing bacterial inflammation [9]. As long as the reported post-embolic infectious complications in noninfected arteries are very low, below 1% [10], one would predict a much higher infection incidence in cases of infected aneurysms. In our case, we avoided the surgical approach through a lateral thoracotomy with the required positioning on the operating table, due to the patient’s coexisting spine injuries. We proceeded therefore with a transcatheter treatment after controlling the infection. Aiming to minimize the infection recurrence risk, the patient was set for 6 weeks postoperatively on intravenous broad-spectrum antibiotics. The literature provides only a few reports of coiling in mycotic IMA pseudoaneurysms, with a maximum follow-up of 3 months in one case [2], while our patient was closely observed radiologically over 6 and clinically over 12 months.
In conclusion IMA aneurysms are rare but potentially morbid. Percutaneous transcatheter coil embolization of a mycotic IMA pseudoaneurysm may offer under circumstances a safe, efficient and minimally invasive therapeutic alternative to the standard treatment of open surgical repair.
Adjacent infective processes like anterior chest wall abscesses should be treated aggressively to prevent transthoracic infection spreading with subsequent vascular complications.
Funding
There is no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing Interests
The authors declare that they have no competing interests.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Contributor Information
Kyriakos Spiliopoulos, Department of Thoracic and Cardiovascular Surgery, Faculty of Medicine, School of Health Sciences, University of Thessaly, Larissa, Greece.
Dimitrios E Magouliotis, Department of Surgery, Faculty of Medicine, School of Health Sciences, University of Thessaly, Larissa, Greece.
Konstantinos Spanos, Department of Vascular Surgery, Faculty of Medicine, School of Health Sciences, University of Thessaly, Larissa, Greece.
Nikolaos S Salemis, Breast Unit, Army General Hospital, Athens, Greece.
Angeliki Tsantsaridou, Department of Thoracic and Cardiovascular Surgery, Faculty of Medicine, School of Health Sciences, University of Thessaly, Larissa, Greece.
Georgios Karagiorgas, Department of Radiology, Faculty of Medicine, School of Health Sciences, University of Thessaly, Larissa, Greece.
Athanasios D Giannoukas, Department of Vascular Surgery, Faculty of Medicine, School of Health Sciences, University of Thessaly, Larissa, Greece.
Christos Rountas, Department of Radiology, Faculty of Medicine, School of Health Sciences, University of Thessaly, Larissa, Greece.
References
- [1]. Nasir A, Viola N, Livesey SA. Iatrogenic pseudoaneurysm of internal mammary artery: case report and literature review. J Cardiovasc Surg 2009;24:355–6. [DOI] [PubMed] [Google Scholar]
- [2]. Deshmukh H, Prasadb SR, Patankara T, Zankara M. Internal mammary artery pseudoaneurysms complicating chest wall infection in children. Diagnosis and endovascular therapy. Clin Imaging 2001;25:396–9. [DOI] [PubMed] [Google Scholar]
- [3]. Wani NA, Rawa IA, Pala NA, Kosar T. Pseudoaneurysm of internal mammary artery caused by pulmonary actinomycosis. Br J Radiol 2010;83:e235–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Kamath S, Unsworth-White J, Wells IP. Pseudoaneurysm of the internal mammary artery as an unusual cause of post-sternotomy hemorrhage: the role of multislice computed tomography in the diagnosis and treatment planning. Cardiovasc Interv Radiol 2005;28:246–8. [DOI] [PubMed] [Google Scholar]
- [5]. Saad NE, Saad WE, Davies MG, Waldman DL, Fultz PJ, Rubens DJ. Pseudoaneurysms and the role of minimally invasive techniques in their management. Radiographics 2005;25:S173–89. [DOI] [PubMed] [Google Scholar]
- [6]. Piffaretti G, Carrafiello G, Franchin M, Ierardi AM, Mariscalco G, Castelli P, et al. Stent-graft repair of a true internal thoracic artery aneurysm. Case Reports Ann Vasc Surg 2015;29:1452.11–5. [DOI] [PubMed] [Google Scholar]
- [7]. Nevidomskyte D, Shalhub S, Aldea GS, Byers PH, Schwarze U, Murray ML, et al. Endovascular repair of internal mammary artery aneurysms in 2 sisters with SMAD3 mutation. Case Reports Ann Vasc Surg 2017;41:283.5–9. [DOI] [PubMed] [Google Scholar]
- [8]. Husted JW, Stock JR, Manella WJ. Traumatic anterior mediastinal hemorrhage: control by internal mammary artery embolization. Cardiovasc Intervent Radiol 1982;5:268–70. [DOI] [PubMed] [Google Scholar]
- [9]. Falagas ME, Nikou SA, Siempos II. Infections related to coils used for embolization of arteries: review of the published evidence. J Vasc Interv Radiol 2007;18:697–701. [DOI] [PubMed] [Google Scholar]
- [10]. Angle JF, Siddiqi NH, Wallace MJ, Kundu S. Quality improvement guidelines for percutaneous transcatheter embolization. J Vasc Interv Radiol 2010;21:1479–86. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors declare that data supporting the findings of this study are available within the article.


