Abstract
A 2-year-old boy was brought by his parents with complaints of difficulty in mouth opening for the past one and half years. He had difficulty in chewing and was malnourished, with developing facial asymmetry. He was diagnosed with right side temporomandibular joint ankylosis. We planned for surgical removal of the ankylotic mass. But we modified the treatment protocol. Instead of doing coronoidectomy after aggressive excision of the ankylotic mass as advocated by Kaban, we did a ‘coronoidoplasty’ after aggressive excision of the ankylotic mass. Coronoidotomy or coronoidectomy is one of the rungs in the treatment ladder that is followed in surgical management of temporomandibular joint ankylosis. But one of the postoperative complications after coronoidectomy is the open bite. The difficulty to close the mouth becomes more pronounced when bilateral coronoidectomy is done. However, ‘coronoidoplasty’, as we have done for this patient retains the action of the temporalis muscle on the mandible in closing the mouth, yet removes the mechanical interference of the coronoid process. Postoperatively the patient was able to clench his teeth well, chew properly and there was no open bite.
Keywords: dentistry and oral medicine, oral and maxillofacial surgery
Background
Temporomandibular joint (TMJ) ankylosis, which is the fusion of condyle of the mandible with the skull base results in very limited or no mobility of the joint.1 This results in almost nil mouth opening. Prevalence is more in the developing countries, around 0.46 in 1000, than the developed countries.2 The most common cause for a TMJ ankylosis is trauma resulting in the fracture of the condylar head of the mandible followed by infections resulting in ankylosis.3 Coronoidectomy becomes inevitable when the coronoid tip is elongated causing mechanical obstruction while opening the mouth, even after the ankylotic mass has been surgically removed. Surgeons operating on TMJ ankylosis will very well acknowledge this and recommend a coronoidectomy as advocated by Kaban.4 But the problem associated with the coronoidectomy is the open bite,5 6 due to the loss of temporalis muscle action on the mandible. This becomes more pronounced when bilateral cornoidectomy is performed. Some cases improve with time but in our experience we have had long-standing cases of inability to close the mouth postbilateral coronoidectomies. While the patient presents with difficulty in opening the mouth, after the procedure, the patient develops difficulty in closing the mouth! Chewing the food becomes extremely difficult, which further leads to nutritional deficiencies. It becomes a sad state of affairs, training the patient postoperatively to close the mouth. This inability further leads to psychological and social problems, particularly in young female patients. Hence, it is important to preserve temporalis action on the mandible and therefore we decided to do this new technique ‘coronoidoplasty’ instead of coronoidectomy.
Case presentation
A 2-year-old boy was brought to our outpatient department by his parents. Their complaint was that he was not able to open his mouth. This problem had initially started when he was about 7 months old, as difficulty to open or reduced mouth opening and gradually worsened to the present condition, where he is not able to open his mouth. He had difficulty in eating as he could not open his mouth and his chewing was impaired. This had a negative impact on his nourishment. His parents could not recall any particular event or fall, which led to this condition. They gave no history of ear infection. On clinical examination, the boy had a maximal interincisal mouth opening of 3 mm. His chin was deviated to the right side and there was evidence of retrognathia (figures 1 and 2). With the available history and the clinical presentation, we arrived at a provisional diagnosis of right side TMJ ankylosis.
Figure 1.

Preoperative frontal view.
Figure 2.
Preoperative right lateral view.
Investigations
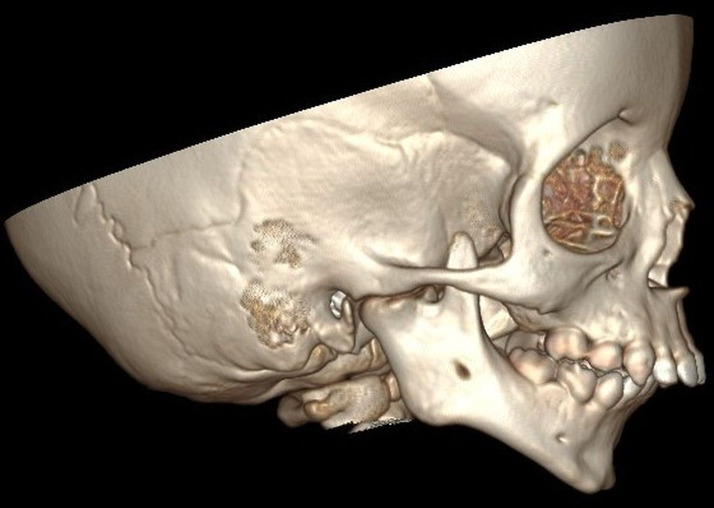
We did a CT scan to evaluate his bilateral TMJ. The CT scan revealed evidence of bony ankylosis in the right TMJ. It also revealed the coronoid process of mandible in the right side was elongated (figure 2). The left side TMJ and the coronoid process were unaffected (figure 3). His other blood parameters were within normal range.
Figure 3.
Preoperative left lateral view.
Procedure
Under general anaesthesia, through right preauricular and right submandibular incisions (figures 4 and 5), we excised the ankylotic mass and we checked the mouth opening. He had about 21 mm of interincisal mouth opening after removal of the ankylotic mass. There was mechanical obstruction of the coronoid, preventing further mouth opening. We proceeded to do ‘coronoidoplasty’. We marked a centimetre of the base of coronoid along the ascending ramus. This was done close to the internal angle region. The temporalis attachment along the lateral and anterior surface of coronoid was released, preserving the medial and superior attachments. We fixed a two-hole plate to the would be proximal segment of the coronoid with a screw and secured the plate with ties, before doing the osteotomy. Osteotomy was done and we removed 1 cm of the ascending ramus. A molar tooth bud in the region was also removed. We pulled down the proximal segment of the resected coronoid and fixed to the distal part of the remaining ascending ramus at the internal angle region with the two-hole plate. The mouth opening after this procedure was about 35 cm interincisally (figures 6–11). We achieved adequate mouth opening, we proceeded to do pterygomasseteric muscle interposition to prevent reankylosis, and also preserved the temporalis attachment to the mandible through the ‘coronoidoplasty’.
Figure 4.
Osteotomy through submandibular incision.
Figure 5.
Osteotomy through preauricular incision.
Figure 6.
Securing coronoid before osteotomy.
Figure 7.
Segment of resected ascending ramus.
Figure 8.
Coronoidoplasty fixation.
Figure 9.
Resected ankylotic mass and ramus.
Figure 10.

Immediate post Operative.
Figure 11.

Immediate post-OP opening.
Outcome and follow-up
His postoperative period was uneventful, and on the seventh day we removed the sutures and his mouth opening was around 25 cm interincisally (figures 12 and 13). We followed up him for 10 days postoperatively and the outcome of this procedure ‘coronoidoplasty’ was evident. The boy could well clench his teeth on both sides. He could open his mouth well, so could he chew well on both sides. He did not have any difficulty while closing his mouth in the form of open bite. Four months postoperatively, we did a teleconsultation. He had good mouth opening, with no evidence of TMJ reankylosis. We could not measure the mouth opening but his mouth opening had not decreased as is evident in the photographs sent later. He was able to chew well on both sides and the surgical sites had healed well with minimal scarring. Because of the lockdown imposed due to SARS COV2 the patient could not travel to our hospital as he belonged to another state in India. Close to 6 months postoperatively, the father of the patient sent the photographs that he took at their home and it was evident he did not have reankylosis (figures 14–18).
Figure 12.

Seventh day post OP.
Figure 13.
Mouth opening seventh day post OP.
Figure 14.
Mouth opening close to 6 months post OP.
Figure 15.

Deviation to the right side but adequate opening.
Figure 16.

Mouth opening adequate to protrude tongue.
Figure 17.

Frontal view mouth closed.
Figure 18.

Healing with minimal scarring.
Discussion
Coronoidectomy for TMJ ankylosis is done when gap arthroplasty alone is not enough to achieve adequate mouth opening. Preoperatively radiographic evidence of elongated coronoid process is an indication for coronoidectomy as it causes physical obstruction in the opening of mandible. To remove the obstruction caused by the elongated coronoid, the coronoid process is surgically removed. In certain cases, Gap arthroplasty would eliminate the coronoid process, where the ankylotic mass is so massive that it involves the sigmoid notch and extending to the coronoid process. Thus, Gap arthroplasty with the removal of coronoid process would result in loss of temporalis attachment to the mandible. The temporalis muscle helps in elevating the mandible, resulting in closure of the mouth. The loss of temporalis action is more pronounced when bilateral coronoidectomy is done and becomes even more worse when bilaterally, medial pterygoid and masseter muscles are used for interposition to prevent reankylosis. This would result in inaction of both the muscles responsible for elevating the mandible on both sides. Postoperatively the patient would have adequate mouth opening, but would start complaining about inability to close the mouth and difficulty in chewing food. Some patients end up having mouth open unable to close or have an anterior open bite.
The undesirable effects of Gap arthroplasty in various scenarios such as (1) anterior open bite, (2) posterior open bite and (3) malocclusion due to posterior premature contact have been well documented in multiple articles.5–7 This is because of the combination of the following factors: (1) absence of a posterior stop or articulating surface at the glenoid fossa resulting in loss of fulcrum, (2) uncountered, anterosuperior direction of pull exerted by the medial pterygoid and masseter muscles and (3) absence of the action of temporalis muscle which is posterosuperior in direction. In a normal functioning mandible, the condyle acts as the fulcrum, and the medial pterygoid and masseter muscles exert an anterosuperior pull, which is countered by the temporalis, with a posterosuperior pull on the mandible. The forces exerted by the pterygo-masseteric muscles and the temporalis, balance out each other to place the mandible at the exact anteroposterior position in relation to the maxilla resulting in occlusion. This is evident in the direction of the muscle fibres (figures 19 and 20).
Figure 19.

Direction of masseter and temporalis muscle fibres. This illustration was drawn by the author (DSSS).
Figure 20.

Direction of pull. Copyright by AO Foundation, Switzerland. Source: AO Surgery Reference, https://surgeryreference.aofoundation.org.
As TMJ ankylosis surgery has progressed from simple removal of the ankylosis resulting in mere opening of the mouth, to also restoration of form and function through procedures like distraction osteogenesis and placement of condylar analogues, it is important to preserve the action of temporalis muscle on the mandible.
Considering the physics of TMJ function, when the fulcrum, which is the condyle, is restored with a condylar analogue or any interpositional graft, the upward and backward pull of the temporalis is essential to prevent anterior open bite. Otherwise, the unopposed anterosuperior action of the medial pterygoid and masseter muscles will cause premature posterior occlusal contact resulting in anterior open bite. Thus, ‘coronoidoplasty’ done during ankylosis release will be of immense help when at a later stage total joint replacement is planned to restore the function.
The procedure that we have done removes the obstruction caused by elongated coronoid process as well as restores the action of the temporalis muscle on the mandible. This would result in closure of the mouth without an anterior open bite. Coronoidectomy is permanent removal of temporalis action on the mandible. There are articles about other modifications of coronoidectomy.8 9 But ‘coronoidoplasty’ is more preservative, eliminating only the obstruction, but retaining the temporalis action on the mandible.
Reankylosis is a major concern in the treatment of TMJ ankylosis, whichever technique is adopted.10 Even so, ‘coronoidoplasty’ causing reankylosis is a concern. We would like to treat it, as we would address any other concern causing reankylosis. We feel the usual precautions taken to prevent reankylosis like adequate removal of bone, good interpositional graft11 12 and vigorous mouth opening exercises during the postoperative period would prevent reankylosis.13
In this present case, assessing the postoperative CT scan (figures 21 and 22), we noted that there is room for some improvements in executing this surgical procedure. We felt that the repostioning of the coronoid should have been a little more anterior, flush to the ascending ramus. That would have taken the coronoid tip more further away from the ankylosis site, further reducing chances of reankylosis. We also noticed that it is preferable to use a four-hole plate without bar, for more stability and thereby preventing rotational movements of the plate with one screw as an axis, while opening and closure of the jaw, though it may not be possible all the times.
Figure 21.

Postoperative frontal view.
Figure 22.
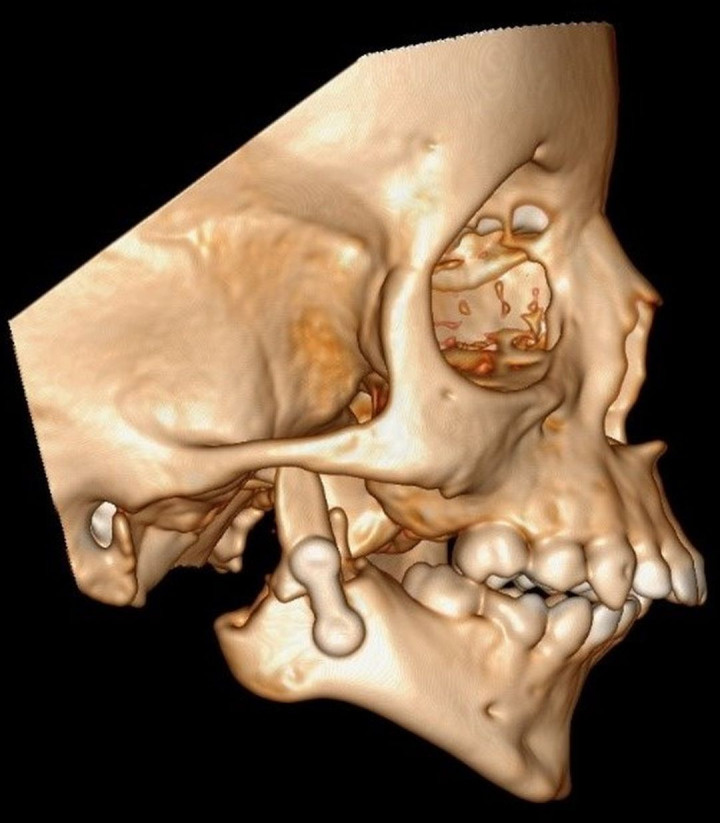
Postoperative right lateral view.
With adequate efforts taken to prevent reankylosis, we propose ‘coronoidoplasty’ can be included in the treatment protocol for TMJ ankylosis especially for patients with bilateral TMJ ankylosis.14
Since this is a case report highlighting the surgical technique, we acknowledge the limitation of having done only one case using this technique. Though we regard this outcome successful at close to 6 months of postoperative period, we would like to state that the results need to be firmly established with (1) a series of cases, (2) cases involving bilateral TMJ ankylosis and (3) a longer follow-up, which we are planning to do. Results from other centres following this technique will help validate our results.
Learning points.
‘Coronoidoplasty’ definitely addresses the postoperative open bite problem.
It is a more preservative procedure than coronoidectomy.
Avoids the adverse side effects of a coronoidectomy without compromising on the intended outcome of the surgery, which is adequate mouth opening.
Footnotes
Contributors: The concept, planning and execution of the surgery of this new technique was conceived by DSSS. He also wrote the manuscript. AGO assisted in the surgery, and did literature review and article search. JE edited the manuscript and finalised it for submission and he was also a scientific adviser.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Parental/guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Vibhute PJ, Bhola N, Borle RM. TMJ Ankylosis: multidisciplinary approach of treatment for Dentofacial Enhancement—A case report. Case Rep Dent 2011;2011:1–7. 10.1155/2011/187580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta VK, Mehrotra D, Malhotra S, et al. An epidemiological study of temporomandibular joint Ankylosis. Natl J Maxillofac Surg 2012;3:25–30. 10.4103/0975-5950.102146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Roo N, Van Doorne L, Troch A, et al. Quantifying the outcome of surgical treatment of temporomandibular joint Ankylosis: a systematic review and meta-analysis. J Craniomaxillofac Surg 2016;44:6–15. 10.1016/j.jcms.2015.08.019 [DOI] [PubMed] [Google Scholar]
- 4.Kaban LB, Bouchard C, Troulis MJ. A protocol for management of temporomandibular joint ankylosis in children. J Oral Maxillofac Surg 2009;67:1966–78. 10.1016/j.joms.2009.03.071 [DOI] [PubMed] [Google Scholar]
- 5.Jagannathan M, Munoli AV, Amarnath V. Unfavourable results in temporomandibular joint Ankylosis surgery. Indian J Plast Surg 2013;46:235–8. 10.4103/0970-0358.118598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cho J-W, Park J-H, Kim J-W, et al. The sequential management of recurrent temporomandibular joint ankylosis in a growing child: a case report. Maxillofac Plast Reconstr Surg 2016;38:39. 10.1186/s40902-016-0083-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Danda AK, S R, Chinnaswami R. Comparison of gap arthroplasty with and without a temporalis muscle flap for the treatment of Ankylosis. J Oral Maxillofac Surg 2009;67:1425–31. 10.1016/j.joms.2008.12.049 [DOI] [PubMed] [Google Scholar]
- 8.Prabhu S. Wedge subcoronoid ostectomy: an alternative to coronoidotomy. Int J Oral Maxillofac Surg 2010;39:1127–9. 10.1016/j.ijom.2010.06.022 [DOI] [PubMed] [Google Scholar]
- 9.Mohanty S, Kohli S, Dabas J, et al. Fate of the coronoid process after Coronoidotomy and its effect on the Interincisal opening: a clinical and radiologic assessment. J Oral Maxillofac Surg 2017;75:1263–73. 10.1016/j.joms.2017.01.012 [DOI] [PubMed] [Google Scholar]
- 10.KeqianZhi MD. Management of temporomandibular joint ankylosis: 11 years’ clinical experience. Oral Surg Oral Med Oral Pathol 2009;108:687–92. [DOI] [PubMed] [Google Scholar]
- 11.Bayat M, Badri A, Moharamnejad N. Treatment of temporomandibular joint Ankylosis: gap and interpositional arthroplasty with temporalis muscle flap. Oral Maxillofac Surg 2009;13:207–12. 10.1007/s10006-009-0174-4 [DOI] [PubMed] [Google Scholar]
- 12.Dimitroulis G. The interpositional dermis-fat graft in the management of temporomandibular joint Ankylosis. Int J Oral Maxillofac Surg 2004;33:755–60. 10.1016/j.ijom.2004.01.012 [DOI] [PubMed] [Google Scholar]
- 13.Park MW, Eo MY, Seo BY, et al. Gap arthroplasty with active mouth opening exercises using an interocclusal splint in temporomandibular joint Ankylosis patients. Maxillofac Plast Reconstr Surg 2019;41:18. 10.1186/s40902-019-0200-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Uppal N, Baliga M, Ramanathan A. Is a modification of Kaban's protocol in treating temporomandibular joint Ankylosis appropriate? J Oral Maxillofac Surg 2010;68:706–7. 10.1016/j.joms.2009.09.115 [DOI] [PubMed] [Google Scholar]