Abstract
PURPOSE
The objectives of this study were to evaluate the fracture strength and fracture patterns of provisional crowns fabricated from different materials and techniques after receiving stress from a simulated oral condition.
MATERIALS AND METHODS
A monomethacrylate-based resin (Unifast Trad) and a bis-acryl-based (Protemp 4) resin were used to fabricate provisional crowns using conventional direct technique. A milled monomethacrylate resin (Brylic Solid) and a 3D-printed bis-acrylate resin (Freeprint Temp) were chosen to fabricate provisional crowns using the CAD/CAM process. All cemented provisional crowns (n=10/group) were subjected to thermal cycling (5,000 cycles at 5°–55℃) and cyclic occlusal load (100 N at 4 Hz for 100,000 cycles). Maximum force at fracture was tested using a universal testing machine.
RESULTS
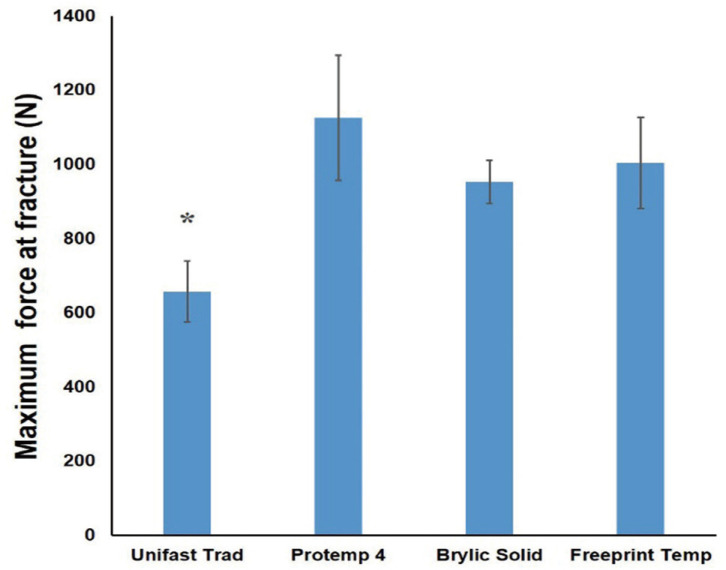
Maximum force at fracture (mean ± SD, N) of each group was 657.87 ± 82.84 for Unifast Trad, 1125.94 ± 168.07 for Protemp4, 953.60 ± 58.88 for Brylic Solid, and 1004.19 ± 122.18 for Freeprint Temp. One-way ANOVA with Tamhane post hoc test showed that the fracture strength of Unifast Trad was statistically significantly lower than others (P<.01). No statistically significant difference was noted among other groups. For failure pattern analysis, Unifast Trad and Brylic Solid showed less damage than Protemp 4 and Freeprint Temp groups.
CONCLUSION
Provisional crowns fabricated using the CAD/CAM process and the conventionally fabricated bis-acryl resins exhibited significant higher fracture strength compared to conventionally fabricated monomethacrylate resins after the aging regimen. Therefore, CAD/CAM milling and 3D printing of provisional restorations may be good alternatives for long term provisionalization.
Keywords: Computer-aided design/computer-aided manufacturing (CAD/CAM), 3D printing, Fracture strength, Provisional restorations
INTRODUCTION
Provisional restoration is an important and almost unavoidable part of fixed prosthodontic treatment until the definitive prosthesis is placed. Currently, two popular groups of custom-fabricated provisional materials are monomethacrylates or acrylic resins, which comprise polymethylmethacrylate (PMMA), polyethyl/butyl methacrylate (PEMA), and other types or combination of methacrylate resins, and dimethacrylates or bis-acryl composite resins, namely bisphenol A-glycidyl dimethacrylate (Bis-GMA) and urethane dimethacrylate (UDMA, the visible light-polymerized resin).1
The provisional restoration should be able to withstand oral conditions, including sharp rises and drops in temperature, saturated humidity and repeated occlusal force, for a reasonable amount of time.2 It is preferable for provisional materials to have adequate strength to avoid breakage, since repairing inevitably requires an extra visit. The type of material plays important roles in the fracture strength outcome.3 Many studies reported that bis-acryl resins are stronger than conventional PMMA and PEMA resins.4,5,6,7 However, Haselton et al.2 concluded that the fracture property depended on each material, rather than the material category, since some bis-acryl groups had high mean fracture force while others performed poorly even when compared with PMMA resins.
Recently, the availability of computer-aided design/computer-aided manufacturing (CAD/CAM) technology in dental use had made a novel way of provisional restoration possible. CAD/CAM fabrication can be categorized as subtractive manufacturing or milling, which is processed by cutting out the unwanted parts from a block of solid material, and additive manufacturing or three-dimensional (3D) printing, which is processed by adding small parts of the material layer by layer.8,9 The CAD/CAM milling process allows for the use of high density and pre-polymerized polymer, hopefully to improve the mechanical properties of previously used chemically cured resins.10 Several studies suggested that CAD/CAM-milled PMMA had higher strength than autopolymerized PMMA and conventional bis-acrylic based materials, with or without thermocycling.5,11,12 In contrast, Karaokutan et al.13 showed that the fracture strength of bisacryl-based resins and CAD/CAM-milled PMMA was higher than that of conventional PMMA-based materials after thermocycling.
Studies on fracture strength of 3D printed provisional restorations are still limited.10,14 Tahayeri et al.14 found that provisional resins produced with 3D printing process can sustain a peak stress at a comparable level with bis-acryl materials, with both performing significantly better than monomethacrylate resins. Digholkar et al.10 reported that the flexural strength value of the CAD/CAM 3D-printed visible-light-cured microhybrid-filled composite resin was statistically significantly lower than those of the CAD/CAM-milled PMMA resin and the conventional heat-cured PMMA resin.
As previously mentioned, studies about provisional restoration strength are still in controversy. Additionally, most studies used thermocycling or water storage to test material properties, which might not represent the oral condition that involved both thermocycling and cyclic occlusal loading.7,11,12,13,15 To date, there has been little study on the examination of the properties of provisional restorative materials fabricated using the latest 3D printing technology.10,14
Therefore, the main objective of this study is to evaluate the fracture strength of provisional crowns made from different materials and fabrication methods after simulating a thermo-mechanical aging process. The failure mode of provisional crowns was also examined. The tested null hypothesis was that maximum force at the fracture of different materials and fabrication techniques used for provisional restoration after simulated aging would be similar.
MATERIALS AND METHODS
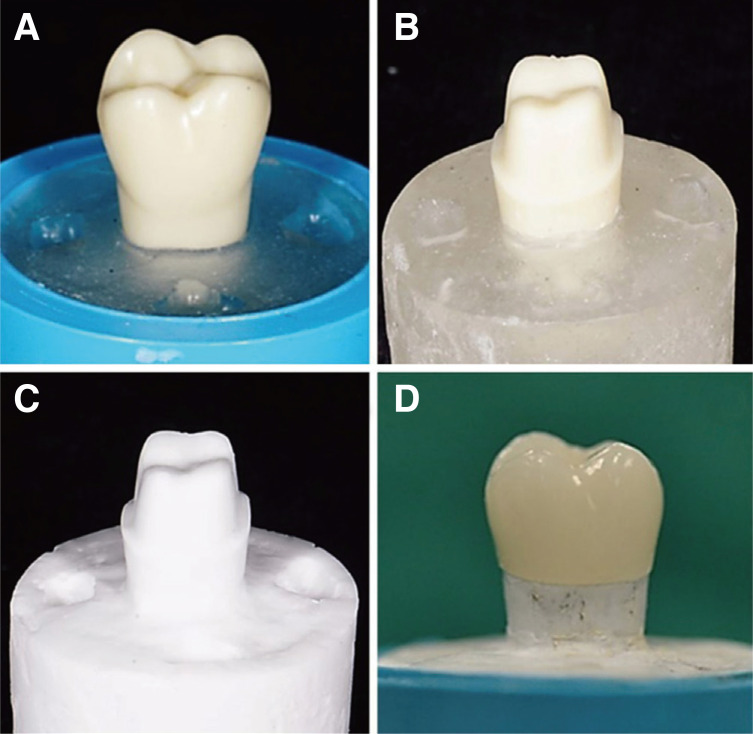
A maxillary right first molar dentoform tooth (Nissin Dental Product Inc., Tokyo, Japan) was positioned and embedded in a polyvinyl chloride (PVC) tube with self-cured clear PMMA (Ortho-jet, Lang Dental, Wheeling, IL, USA) (Fig. 1A). After completed setting, three indices were marked on the resin to assist the re-positioning of silicone index in the fabrication of direct provisional crowns, as well as the superimposing position during the scanning and fabrication of the CAD/CAM provisional crowns. Another dentoform tooth was similarly positioned and embedded with the aid of a silicone index to imitate the axis and position of the PVC tube and to replicate the index from the first tooth. This tooth was then used as a die for the preparation of ceramic crown. The preparation included 2 mm occlusal reduction, 1 mm round chamfer finishing line at 1 mm above the cemento-enamel junction with a 6-degree convergence angle (Fig. 1B). The prepared tooth, along with its resin base, was used as a template for die fabrication. Duplication of the prepared tooth was then carried out with a 1:1 mixture of bisphenol-A epoxy resin (Epotec YD128 Aditya Birla Chemicals Ltd., Bangkok, Thailand) reinforced with 50 µm alumina particles (Loxley, Bangkok, Thailand) and poured into a condensation silicone mold material (RA-320, Rungart Co., Bangkok, Thailand). Each completely polymerized epoxy resin die (Fig. 1C) was carefully inspected under 2.5× magnification dental loupes (HR, HEINE Optotechnik, Herrsching, Germany). If any defects were found, the epoxy die was excluded from this study. Finally, 40 dies were selected and randomly divided into four experimental groups. Different types of materials and fabrication methods were assigned to each group, as shown in Table 1. The sample size of the present study is 10 per group, calculated using the mean and the standard deviation of the fracture resistance data provided by Abdullah et al.16
Fig. 1. Die preparation and provisional crown. (A) Pre-preparation dentoform tooth embedded in a polyvinyl chloride tube with self-cured resin, (B) prepared tooth for all ceramic crown, (C) epoxy die replicated from prepared tooth, (D) provisional crown cemented on an epoxy die.
Table 1. Provisional materials used in this study.
| Material | Type | Fabrication technique | Manufacturer |
|---|---|---|---|
| Unifast Trad | Methylmethacrylate | Conventional Direct | GC chemicals, Tokyo, Japan |
| Protemp 4 | Bis-acryl | Conventional Direct | 3M ESPE, Seefeld, Germany |
| Brylic Solid | Highly polymerized PMMA | CAD/CAM milling | Sagemax bioceramics, WA, USA |
| Freeprint Temp | Photo-polymerized bis-acrylate resin | CAD/CAM printing | Detax GmbH, Ettlingen, Germany |
CAD/CAM, computer-aided design/computer-aided manufacturing; PMMA, polymethylmethacrylate
For the conventional direct technique, a thin layer of petroleum jelly was applied on each die. A self-cured PMMA provisional restoration material (Unifast Trad, GC chemicals, Tokyo, Japan) and a self-cured bis-acryl material (Protemp 4, 3M ESPE, Seefeld, Germany) were then mixed according to the manufacturer's recommendations and loaded into the special tray-supported silicone mold (Provil novo, Kulzer GmbH, Wehrhiem, Germany), which imitates the outer surface of the unprepared tooth, until completely set. The excess material at the crown margin was marked and removed under 2.5× magnification loupes using carbide bur followed by polishing with a Sof-Lex disc (3M ESPE) and a slurry of pumice. After finishing and polishing, the provisional crown was tried-in on each respective die to ascertain fit and adaptability.
For the provisional crowns fabricated with the CAD/CAM method, each die was scanned using an intraoral scanner (3Shape TRIOS, Copenhagen, Denmark) to attain a 3D model of the prepared tooth. The pre-preparation scan of the model was obtained on the same die with a provisional crown template fabricated with a similar technique to the previous groups. The pre-preparation scan was applied as an outer surface template. The adjustments were minor, made as necessary to achieve the accurate dimensions of the provisional crowns as compared to the template fabricated from the unprepared tooth. A cement space of 50 µm for each specimen was set.17 The subtractive CAD/CAM-fabricated provisional crowns were milled from the CAD/CAM PMMA bank (Brylic Solid, Sage bioceramics, WA, USA) using a 5-axis milling machine (CORiTEC 250i, imesicore GmbH, Eiterfeld, Germany). No further adjustment or finishing was done on the provisional crowns from the CAD/CAM milling process, except for the removal of the supporting struts. A light-polymerized resin (Freeprint Temp, Detax GmbH, Ettlingen, Germany) was used to construct the additive CAD/CAM fabricated provisional crowns using digital light processing printer (Asiga Max, Asiga, Sydney, Australia). After removing the supporting struts, another thin layer of printing resin was applied over the printed crowns and light cured to glaze the external surface.
Each crown was cemented on an individual die with Temp-bond NE (Kerr Dental, Brea, CA, USA) under 50 N constant pressure from a metal pendulum for six minutes until a complete set of temporary cement was obtained. Excess cement was then removed with a dental explorer (Fig. 1D).
The cemented provisional crowns were thermocycled for 50,000 cycles between baths held at 5 and 55℃, with a dwell time of 60 seconds and transfer time of five seconds using the thermocycling machine (TC-301, KMITL, Bangkok, Thailand), to represent approximately six months of oral environment.12 One hundred thousand rounds of 100 N at 4 Hz frequency were then applied to the central pit of provisional crown along the long axis of each tooth, using a 5 mm diameter stainless steel ball fixed on the dynamic testing instrument (Electroplus E1000, Instron, Norwood, MA, USA) in a 37℃ electric water tank to represent a six-month oral condition.18
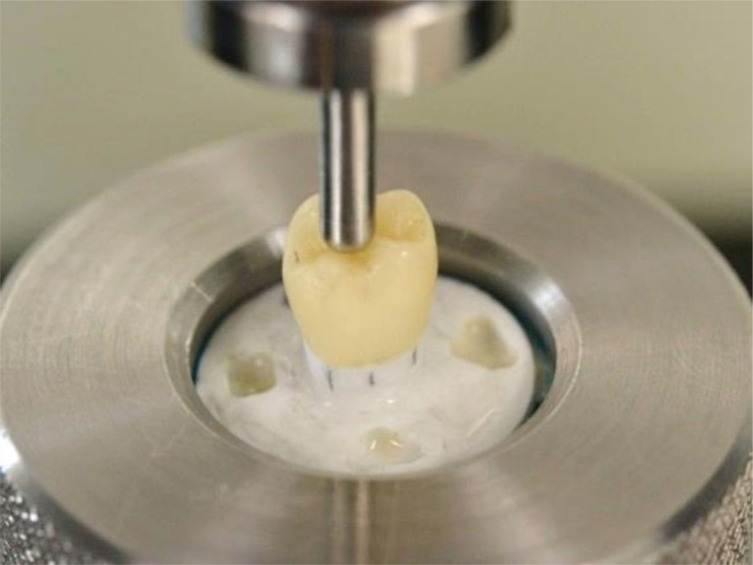
Subsequently, all cemented provisional crowns were subjected to the universal testing machine (Lloyd LR10K, Ametek, FL, USA) under an axial load at a crosshead speed of 1 mm/min with 30 kN load cells, using a metal ball of 5 mm diameter at the central pit parallel to the long axis of the tooth until failure occurred (Fig. 2). Maximum force at fracture was recorded. The type of failure of each sample was then classified according to Burke19 (Table 2).
Fig. 2. Specimen mounted on universal testing assembly for the compressive load test.
Table 2. Classification of restoration failure according to Burke19.
| Classification | Pattern of fracture |
|---|---|
| Class I | Minimal fracture or crack in crown |
| Class II | Less than half of crown lost |
| Class III | Crown fracture through midline; half of crown displaced or lost |
| Class IV | More than half of crown lost |
| Class V | Severe fracture of tooth and/or crown |
All fracture strength data were analyzed by one-way ANOVA with Tamhane post hoc test using IBM SPSS Statistics 20 (IBM, Armonk, NY, USA). All statistical tests were conducted at a significance level of 0.05.
RESULTS
The minimum, maximum, mean and standard deviation values, along with a 95% interval of the maximum force of each group, were shown in Table 3. The fracture strength of Unifast Trad group was statistically lower than that of the other groups (P < .01), while no significant difference were found among other groups (P > .05) (Fig. 3).
Table 3. The maximum force at the fracture (N) of each group.
| Material | Minimum | Maximum | Force at fracture | 95% Confidence Interval | ||
|---|---|---|---|---|---|---|
| Mean | SD | Lower bound | Upper bound | |||
| Unifast Trad | 540.20 | 769.81 | 657.87 | 82.84 | 598.61 | 717.13 |
| Protemp 4 | 783.78 | 1338.51 | 1125.94 | 168.07 | 1005.71 | 1246.16 |
| Brylic Solid | 873.17 | 1084.46 | 953.60 | 58.88 | 911.47 | 995.72 |
| Freeprint Temp | 744.02 | 1149.05 | 1004.19 | 122.18 | 916.79 | 1091.59 |
Fig. 3. The fracture strength of provisional crowns. Graph representation of maximum force (N) at the fracture point of provisional crowns in each group.
Data were presented as mean ± SD. *indicates statistically significant value (P < .01).
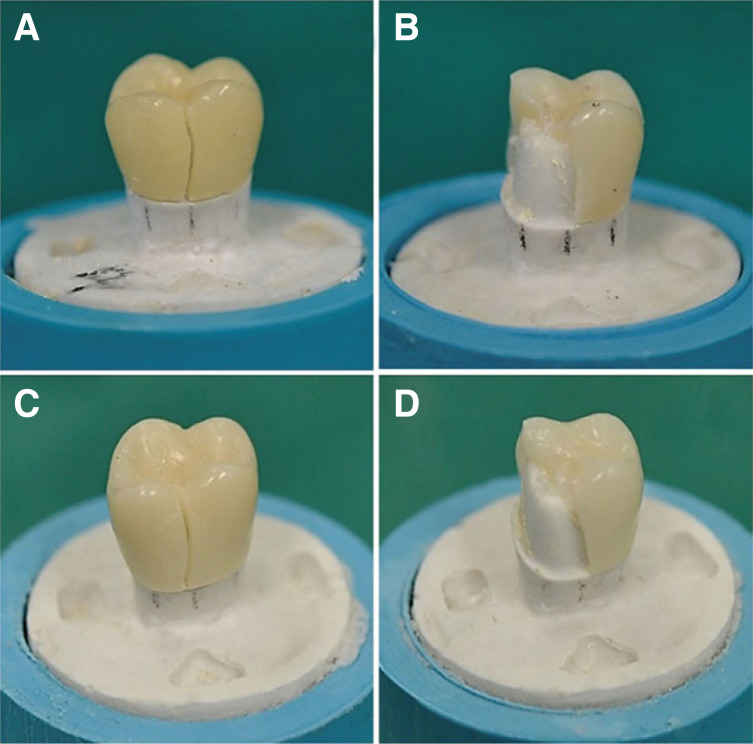
All samples in the Protemp 4 and Freeprint Temp groups had the same fracture pattern, with the crack at mesiobuccal cusp, a small part of mesiolingual cusp and crack lines in other areas, which were classified as class II failure. On the other hand, the monomethacrylate groups, namely Unifast Trad and milled Brylic Solid, exhibited class I failure with a crack line running from the central fossa along the buccal groove to the margin (Fig. 4).
Fig. 4. The fracture pattern of provisional crowns. (A) Unifast Trad, (B) Protemp 4, (C) Brylic Solid, (D) Freeprint Temp.
DISCUSSION
In this study, the fracture strength and pattern of provisional restoration made with different materials and fabrication technique after simulated thermo-mechanical aging were evaluated. The null hypothesis was rejected as different fracture strengths were found among groups. Provisional restoration should be able to sustain dynamic oral condition and occlusion forces for a certain period of time, especially in full mouth rehabilitation or dental implant treatment. The appropriate strength and stability of materials are quite critical to support its function.2 Stress from intraoral functions generated by both thermal and mechanical stimulants could weaken the mechanical properties of provisional restorations.6,12,15,20 However, only a few studies have been carried out to evaluate the strength of provisional restorations that received mechanical fatigue loading.6 By using both of thermocycling process (5,000 cycles, at 5 – 55℃) and occlusal fatigue loading (100,000 cycles of 100 N at 4 Hz frequency occlusal load), we tried to simulate the oral environment as much as possible.
In this study, maximum force at the fracture point was evaluated and the results were corresponded to many previous studies. With or without the aging regimen, the chemically cured PMMA resin has inferior mechanical properties when compared to the auto-mixed bis-acryl and CAD/CAM milling materials.3,5,6,13,15,21 Inferior mechanical properties in hand-mixed self-cured monomethacrylate provisional restorations might be from the nature of the material preparation and molecular structure.3,7 Difficulty in controlling air bubbles and porosity during the manual mixing of monomethacrylate resins may lead to compromised mechanical strength, whereas the self-mixing cartridge delivery system of the bis-acryl resin provides better control to its component proportions and to minimal air entrapment.3,13
The monomethacrylate resin has a much lower monomer molecular weight compared to bis-acryl resin, which contains a large aromatic ring in the monomer that increases rigidity and reduces tendency of the polymer chain to slip or move, which causes deformation of materials.3,22 As with other monomethacrylates, PMMA contains only one functional group, which does not allow the cross-linking of each polymer chain, while a bi-functional monomer bis-acryl is capable of cross-linking and branching with other monomers and therefore strengthens the material bulk.3,7 Moreover, most of the auto-mixed bis-acryl resins, including Protemp 4, are reinforced with fillers that help enhance their mechanical properties.22
Although monomethacrylate was found to be mechanically inferior to bis-acryl, as mentioned earlier, the CAD/CAM-milled restoration that utilized a PMMA block did not exhibit significantly lower fracture strength in the same way as the conventionally fabricated PMMA group. This finding was similar to many of other studies that compared CAD/CAM resin with hand-mixed chemically cured chair-sided PMMA resin and auto-mixed chemically cured bis-acryl resin.5,11,15,21 The provisional material used for CAD/CAM milling in this study is a highly polymerized PMMA polymer based on highly cross-linked resins, which are manufactured in an industrial process with a well-controlled environment that can minimize flaw and contamination while maintaining the pressure during the polymerization process.23,24 This may be impossible when using conventional hand-mixed techniques. Accordingly, the CAD/CAM PMMA blocks exhibited superior qualities when compared to the conventional hand-mixed PMMA, supporting the results of this study.
It has been reported that the provisional resin tends to absorb water, leading to the degradation of polymeric chains by hydrolysis of the monomer, which causes a decrease in the mechanical properties of the resin.1,3 The PMMA resin has a linear polymer network structure, with the high polarity of its molecules and the air bubbles embedded in its structure. As a result, PMMA resin tends to absorb more water than bis-acryl resin.3,6 This was in agreement with a study by Abdulmohsen et al.,4 which found that the monomethacrylate resin had significantly higher water absorption than the dimethacrylate resin after immersion in both artificial saliva and distilled water for up to one and a half months. Several authors proposed that water absorption, which is generated from storage in water or artificial saliva and thermocycling, seriously influences the strength of provisional restorations.12,15,20 Balkenhol et al.25 noted that the fracture toughness of provisional materials depends on the storage times and that methacrylate resin had lower mechanical properties than bis-acrylate resin. Nejatidanesh et al.7 evaluated the flexural strength of provisional materials stored in artificial saliva and thermocycling condition (2,500 cycles at 5 – 55℃) and revealed that bis-acryl-based resins had higher flexural strength than monomethacrylate-based resins. Lang et al.6 found that after storage in distilled water for 24 hours, the fracture resistance value in bis-acryl composite provisional materials was higher than PMMA resins. They also found that upon receiving a mechanical load to simulate intraoral conditions, conventional PMMA also performed poorly and rarely passed the 100,000 cycles of occlusal load when fabricated as 3-unit provisional bridges, while most of the bis-acryl provisional bridges survived as much as 480,000 cycles of occlusal load of 50 N at 1.6 Hz frequency.
As stated earlier, industrial CAD/CAM PMMA-based polymers have more homogeneous structure, fewer free monomers and lower porosity. Therefore, the water absorption of these materials was lower than that of the handmixed self-cured PMMA resins.26 This could explain the superior mechanical properties of CAD/CAM PMMA-based polymers over conventional PMMA resins. These data were similar to the study by Alt et al.,15 stating that CAD/CAM fabricated of the same materials yielded better results than conventional technique. Flaws and inconsistent mixing processes, which are commonly found in conventional methods, could be the major causes of this inferior outcome. They also concluded that the fracture toughness of CAD/CAM PMMA was significantly affected by thermocycling but to a lesser degree than the directly fabricated PEMA and UDMA resins.15
There is little information on the mechanical properties of CAD/CAM 3D printing materials. The present study noted that fracture strength of 3D-printed bis-acrylate resin was similar to milled PMMA resin and conventional bisacryl resin but was significantly higher than chemically-cured PMMA resin. These results were consistent with the study of Tahayeri et al.,14 which revealed that the peak stress for 3D-printed PMMA resins was comparable to the conventional bis-acryl resins and was significantly higher than conventional PMMA. In Contrast, Digholkar et al.'s10 work found that a 3D-printed microhybrid-filled composite resin showed significantly lower flexural strength when compared to milled PMMA and conventional heat-cured PMMA resins. These conflicting results may be partly due to differences in the aging protocols, experimental methods, material types and fabrication processes.
The failure pattern of all monomethacrylate samples (Unifast Trad and Brylic Solid), which were classified as class I, showed less damage than the bis-acryl samples (Protemp 4 and Freeprint Temp), which were classified as class II. The consistency of this finding may be explained by the different chemical construction of the two resins. Balkenhol et al.20 explored the fracture behavior and fracture resistance of monomethacrylates and dimethacrylates and found a substantial difference between the two in terms of patterns of failure. While the stress-strain graphs in all bisacryl groups exhibited linear patterns before the failures occurred, the monomethacrylate groups showed long nonlinear patterns before failure with a maximum point far outside the 95% interval. These findings indicated that monomathacrylates behaved like a ductile material that underwent a considerable degree of plastic deformation before fracture while dimethacrylates were more brittle. This might partly explain the different failure behaviors found in this study.
At present, CAD/CAM technology is popular in dentistry because it is easy and accessible. Furthermore, the CAD/CAM fabrication processes could support a rapid workflow in the fabrication of provisional restoration. For example, in dental implant treatment, oral scan can be made during the surgical visit or even during the treatment planning visit, and provisional restoration can be made ready for immediate provisionalization following implant placement surgery, which is beneficial for soft tissue preservation.27 In the present study, fracture strength of CAD/CAM milling and 3D printing provisional restorations were not different from conventional bis-acryl provisional restoration. Thus, CAD/CAM provisional restorations may be a good alternative for long term provisionalization.
Nonetheless, studies relating to the properties of 3D printing provisional materials are still limited. Moreover, for clinical application, other factors such as dimensional stability during and after fabrication, color stability, and ease of relining and repair should also be considered when choosing provisional materials. Further studies are needed to provide more information.
CONCLUSION
Within the limitations of the present in vitro study, the following conclusions can be drawn. After aging protocol, the conventionally fabricated monomethacrylate (Unifast Trad) represented the lowest fracture strength of all groups. No significant difference of fracture strength was observed among the provisional crowns fabricated from dimethacrylate using conventional techniques (Protemp 4), CAD/CAM-milled monomethacrylate (Brylic Solid) and CAD/CAM 3D-printed dimethacrylates (Freeprint Temp). All monomethacrylate groups (Unifast Trad and Brylic Solid) exhibited class I failure mode, whereas the dimethacrylates groups (Protemp 4 and Freeprint Temp) showed class II failure mode. The results indicated that CAD/CAM fabricated provisional restoration could be used as a promising long-term provisionalization.
Footnotes
This work was partially supported by Faculty of Dentistry, Khon Kaen University.
References
- 1.Burns DR, Beck DA, Nelson SK Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. J Prosthet Dent. 2003;90:474–497. doi: 10.1016/s0022-3913(03)00259-2. [DOI] [PubMed] [Google Scholar]
- 2.Haselton DR, Diaz-Arnold AM, Vargas MA. Flexural strength of provisional crown and fixed partial denture resins. J Prosthet Dent. 2002;87:225–228. doi: 10.1067/mpr.2002.121406. [DOI] [PubMed] [Google Scholar]
- 3.Astudillo-Rubio D, Delgado-Gaete A, Bellot-Arcís C, Montiel-Company JM, Pascual-Moscardó A, Almerich-Silla JM. Mechanical properties of provisional dental materials: A systematic review and meta-analysis. PLoS One. 2018;13:e0193162. doi: 10.1371/journal.pone.0196264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abdulmohsen B, Parker S, Braden M, Patel MP. A study to investigate and compare the physicomechanical properties of experimental and commercial temporary crown and bridge materials. Dent Mater. 2016;32:200–210. doi: 10.1016/j.dental.2015.11.025. [DOI] [PubMed] [Google Scholar]
- 5.Alp G, Murat S, Yilmaz B. Comparison of flexural strength of different CAD/CAM PMMA-based polymers. J Prosthodont. 2019;28:e491–e495. doi: 10.1111/jopr.12755. [DOI] [PubMed] [Google Scholar]
- 6.Lang R, Rosentritt M, Behr M, Handel G. Fracture resistance of PMMA and resin matrix composite-based interim FPD materials. Int J Prosthodont. 2003;16:381–384. [PubMed] [Google Scholar]
- 7.Nejatidanesh F, Momeni G, Savabi O. Flexural strength of interim resin materials for fixed prosthodontics. J Prosthodont. 2009;18:507–511. doi: 10.1111/j.1532-849X.2009.00473.x. [DOI] [PubMed] [Google Scholar]
- 8.van Noort R. The future of dental devices is digital. Dent Mater. 2012;28:3–12. doi: 10.1016/j.dental.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 9.Alghazzawi TF. Advancements in CAD/CAM technology: options for practical implementation. J Prosthodont Res. 2016;60:72–84. doi: 10.1016/j.jpor.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Digholkar S, Madhav VN, Palaskar J. Evaluation of the flexural strength and microhardness of provisional crown and bridge materials fabricated by different methods. J Indian Prosthodont Soc. 2016;16:328–334. doi: 10.4103/0972-4052.191288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rayyan MM, Aboushelib M, Sayed NM, Ibrahim A, Jimbo R. Comparison of interim restorations fabricated by CAD/ CAM with those fabricated manually. J Prosthet Dent. 2015;114:414–419. doi: 10.1016/j.prosdent.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 12.Yao J, Li J, Wang Y, Huang H. Comparison of the flexural strength and marginal accuracy of traditional and CAD/CAM interim materials before and after thermal cycling. J Prosthet Dent. 2014;112:649–657. doi: 10.1016/j.prosdent.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 13.Karaokutan I, Sayin G, Kara O. In vitro study of fracture strength of provisional crown materials. J Adv Prosthodont. 2015;7:27–31. doi: 10.4047/jap.2015.7.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tahayeri A, Morgan M, Fugolin AP, Bompolaki D, Athirasala A, Pfeifer CS, Ferracane JL, Bertassoni LE. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent Mater. 2018;34:192–200. doi: 10.1016/j.dental.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alt V, Hannig M, Wöstmann B, Balkenhol M. Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations. Dent Mater. 2011;27:339–347. doi: 10.1016/j.dental.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 16.Abdullah AO, Tsitrou EA, Pollington S. Comparative in vitro evaluation of CAD/CAM vs conventional provisional crowns. J Appl Oral Sci. 2016;24:258–263. doi: 10.1590/1678-775720150451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nakamura T, Tanaka H, Kinuta S, Akao T, Okamoto K, Wakabayashi K, Yatani H. In vitro study on marginal and internal fit of CAD/CAM all-ceramic crowns. Dent Mater J. 2005;24:456–459. doi: 10.4012/dmj.24.456. [DOI] [PubMed] [Google Scholar]
- 18.Heintze SD, Cavalleri A, Zellweger G, Büchler A, Zappini G. Fracture frequency of all-ceramic crowns during dynamic loading in a chewing simulator using different loading and luting protocols. Dent Mater. 2008;24:1352–1361. doi: 10.1016/j.dental.2008.02.019. [DOI] [PubMed] [Google Scholar]
- 19.Burke FJ. Fracture resistance of teeth restored with dentin-bonded crowns constructed in a leucite-reinforced ceramic. Dent Mater. 1999;15:359–362. doi: 10.1016/s0109-5641(99)00057-3. [DOI] [PubMed] [Google Scholar]
- 20.Balkenhol M, Köhler H, Orbach K, Wöstmann B. Fracture toughness of cross-linked and non-cross-linked temporary crown and fixed partial denture materials. Dent Mater. 2009;25:917–928. doi: 10.1016/j.dental.2009.01.099. [DOI] [PubMed] [Google Scholar]
- 21.Stawarczyk B, Ender A, Trottmann A, Özcan M, Fischer J, Hämmerle CH. Load-bearing capacity of CAD/CAM milled polymeric three-unit fixed dental prostheses: effect of aging regimens. Clin Oral Investig. 2012;16:1669–1677. doi: 10.1007/s00784-011-0670-4. [DOI] [PubMed] [Google Scholar]
- 22.Mei ML, So SYC, Li H, Chu CH. Effect of heat treatment on the physical properties of provisional crowns during polymerization: an in vitro study. Materials (Basel) 2015;8:1766–1777. doi: 10.3390/ma8041766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Edelhoff D, Beuer F, Schweiger J, Brix O, Stimmelmayr M, Guth JF. CAD/CAM-generated high-density polymer restorations for the pretreatment of complex cases: a case report. Quintessence Int. 2012;43:457–467. [PubMed] [Google Scholar]
- 24.Giordano R. Materials for chairside CAD/CAM-produced restorations. J Am Dent Assoc. 2006;137:14S–21S. doi: 10.14219/jada.archive.2006.0397. [DOI] [PubMed] [Google Scholar]
- 25.Balkenhol M, Knapp M, Ferger P, Heun U, Wöstmann B. Correlation between polymerization shrinkage and marginal fit of temporary crowns. Dent Mater. 2008;24:1575–1584. doi: 10.1016/j.dental.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 26.Liebermann A, Wimmer T, Schmidlin PR, Scherer H, Löffler P, Roos M, Stawarczyk B. Physicomechanical characterization of polyetheretherketone and current esthetic dental CAD/ CAM polymers after aging in different storage media. J Prosthet Dent. 2016;115:321–328.e2. doi: 10.1016/j.prosdent.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 27.Mandelaris GA, Vlk SD. Guided implant surgery with placement of a presurgical CAD/CAM patient-specific abutment and provisional in the esthetic zone. Compend Contin Educ Dent. 2014;35:494–504. [PubMed] [Google Scholar]