Abstract
PURPOSE
This study aimed to fabricate provisional crowns at varying build directions using the digital light processing (DLP)-based 3D printing and evaluate the marginal and internal fit of the provisional crowns using the silicone replica technique (SRT).
MATERIALS AND METHODS
The prepared resin tooth was scanned and a single crown was designed using computer-aided design (CAD) software. Provisional crowns were printed using a DLP-based 3D printer at 6 directions (120°, 135°, 150°, 180°, 210°, 225°) with 10 crowns in each direction. In total, sixty crowns were printed. To measure the marginal and internal fit, a silicone replica was fabricated and the thickness of the silicone impression material was measured using a digital microscope. Sixteen reference points were set and divided into the following 4 groups: marginal gap (MG), cervical gap (CG), axial gap (AG), and occlusal gap (OG). The measurements were statistically analyzed using one-way ANOVA and Dunnett T3.
RESULTS
MG, CG, and OG were significantly different by build angle groups (P<.05). The MG and CG were significantly larger in the 120° group than in other groups. OG was the smallest in the 150° and 180° and the largest in the 120° and 135° groups.
CONCLUSION
The marginal and internal fit of the 3D-printed provisional crowns can vary depending on the build angle and the best fit was achieved with build angles of 150° and 180°.
Keywords: Crowns, Printing, Three-dimensional, Dental marginal adaptation, Dental internal fit
INTRODUCTION
Recently in dentistry, various dental prostheses are being fabricated using an additive manufacturing technique called ‘3D printing.’ Since the technique builds the form by stacking the material layer by layer, it can be used to make more complex forms of prosthesis than using subtractive manufacturing.1 In addition, the amount of material used can be reduced and details finer than the width of a cutting bur can be fabricated.2
The method of additive manufacturing varies depending on the material employed, among which the digital light processing (DLP) method involves the layering of a liquid photopolymer by light to produce the final form.3 Compared to the stereolithography (SLA) method, in which each layer is made up of fine lines produced by a laser beam, the DLP method allows faster fabrication time as each layer is created with a single lighting step.4
The direct technique of fabricating temporary crowns using polymethyl methacrylate(PMMA) has been frequently used for convenience and low costs of production, but it has the drawbacks of polymerization shrinkage, marginal discrepancy, and heat production.5 Today, indirect fabrication is possible using computer-aided design/computer-aided manufacturing (CAD/CAM), which facilitates remaking provisional crowns that were lost or fractured during long-term use due to orthodontic treatment or altered vertical dimension.6 Digholkar et al.7 reported that provisional crowns made by 3D printing show higher microhardness than those made by conventional methods. Furthermore, several studies have reported that using an indirect rather than a direct technique to fabricate the provisional crown yields better internal fit.8
For 3D printing, a CAD model is stored as a standard tessellation language (STL) file and then placed on the build platform once the build direction has been determined. Cheng et al.9 reported that choosing the right build direction enhances the volumetric accuracy, reduces the time and cost of production, and minimizes the supports needed for printing. In previous studies, provisional crowns were fabricated in only one build direction to evaluate internal and marginal fit.10,11 Other studies have evaluated the dimensional accuracy of provisional crowns by three-dimensional superimposition method based on various build directions.12,13 However, few studies have evaluated marginal and internal fit for various build directions.
There are various methods of measuring the marginal and internal fit of a prosthesis, of which the silicone replica technique (SRT), unlike other methods, allows directly fitting of the crown to the tooth intraorally to assess the fit.14 SRT has also been reported to show no difference from the cross-section method, in which a cross-section is cut from the specimen and directly observed,15 and has been actively employed in research as a relatively simple method that requires no cutting of prosthesis.14
The present study aims to print provisional crowns at varying build directions using a DLP-based 3D printer and evaluate the marginal and internal fit of the printed crowns using SRT. The null hypothesis is that the build directions have no effect on the marginal and internal fit of the provisional crowns.
MATERIALS AND METHODS
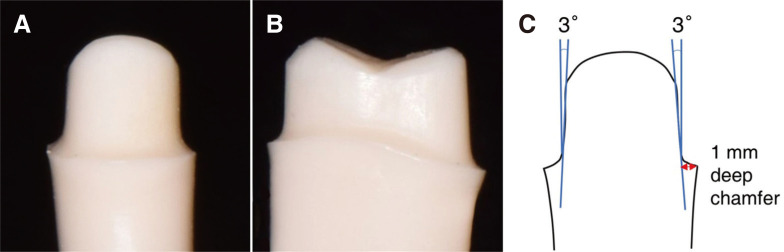
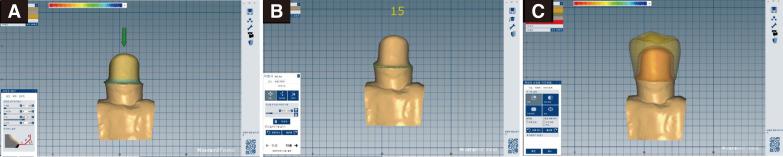
A maxillary second premolar resin tooth (A5AN-500, Nissin Dental Products Inc., Kyoto, Japan) was prepared by reducing 2 mm on the occlusal surface and a total of 6° convergence angle with a 1 mm circumferential deep chamfer finish line (Fig. 1). The prepared resin tooth was then scanned using a model scanner (Ceramill Map 400, Amann Girrbach, Koblach, Austria). After converting the scan data into STL format, a single premolar crown was designed using CAD software (Ceramill Mind, Amann Girrbach, Koblach, Austria). A 30 µm cement gap was set at 1 mm above the finish line (Fig. 2).16
Fig. 1. Preparation of maxillary second premolar resin tooth. (A) Buccal view, (B) mesial view, (C) axial reduction of 6-degree convergence angle with circumferential 1 mm deep chamfer finish line.
Fig. 2. Designing single crown with CAD software. (A) Virtual cement gap of 30 µm set at 1 mm above finish line, (B) finish line of abutment delicated, (C) designed crown.
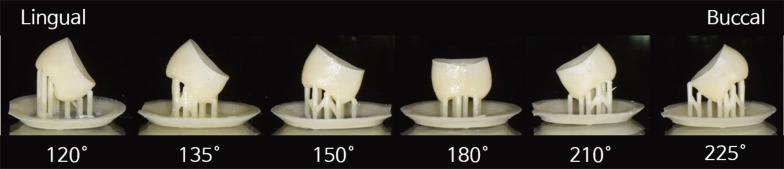
The designed crown was exported into a 3D printer software (Flashprint, Flashforge, Jinhua, China). Ten crowns were placed on a platform in the 3D printer software and rotated according to each build direction. The 120° direction was defined as the orientation after positioning the lingual surface of the crown parallel to the build platform and rotating it 30° on the Y-axis. The crown was rotated 15° or 30° in the direction of the Y-axis until the support was placed on the buccal surface. The support was to be automatically positioned only on the surface that formed an angle of ≥ 30° with the Z-axis.
Provisional crowns were printed using a DLP-based 3D printer (Hunter, Flashforge Corp., Jinhua, China) at 6 directions (120°, 135°, 150°, 180°, 210°, 225°) with 10 crowns in each direction (Fig. 3). In total, sixty crowns were printed. In each build direction, the crowns were printed using a liquid photopolymer (NextDent C&B, 3D systems, Soesterberg, Netherlands) with the layer thickness set to 50 µm. Complying with the manufacturer's instruction, the prints were washed for 5 minutes using 96% 2-propanol (Merck, Emsure, Darmstadt, Germany) and cured for 45 minutes using light-curing unit (LC-3D Print Box, 3D systems, Soesterberg, Netherlands).
Fig. 3. Provisional crowns were printed at 6 build directions (120°, 135°, 150°, 180°, 210°, 225°) using 3D printer.
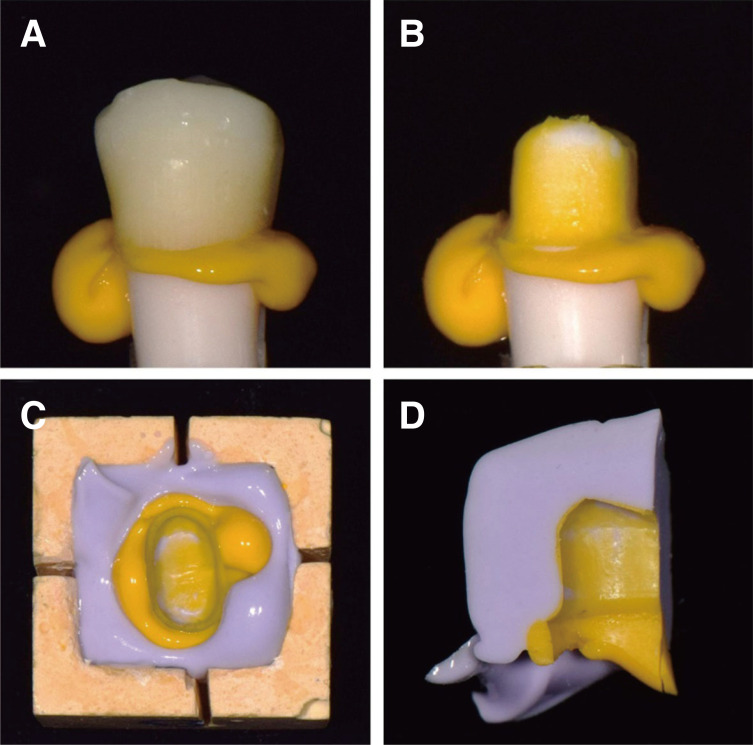
The marginal and internal fit was measured using SRT. Low-viscosity silicone impression material (Honigum light, DMG, Hamburg, Germany) was applied to the inner surface of the crown and fitted to a resin dental model. The crown was pressed until final polymerization was complete and removed after 3 minutes and 30 seconds as instructed by the manufacturer. To cut out the low-viscosity silicone more easily, a silicone interocclusal recording material (Regisil Rigid, Dentsply Sirona, York, PA, USA) was applied around the remaining impression material in the dental model. After removing the fabricated silicone replica from the dental model, it was sectioned evenly in the buccopalatal and mesiodistal direction within the pre-made frame (Fig. 4).
Fig. 4. Fabrication of silicone replica. (A) Low viscosity silicone impression material was applied to the inner surface of the crown and fitted to resin tooth model, (B) crown was removed and bite registration material was applied on low viscosity silicone, (C) silicone replica was sectioned in buccopalatal and mesiodistal directions, (D) sectioned silicone replica.
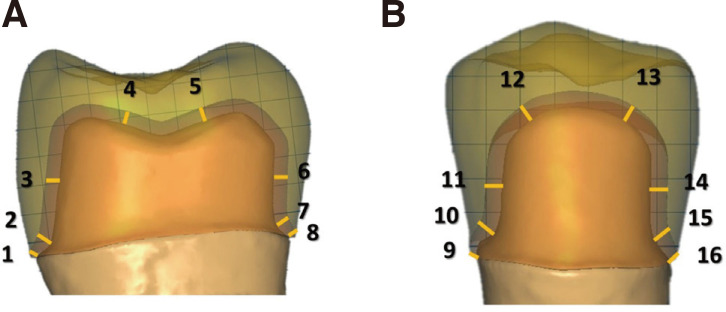
According to the method proposed by Holmes et al.,17 16 reference points were set and divided into the following 4 groups: marginal gap (MG), cervical gap (CG), axial gap (AG), and occlusal gap (OG). MG was defined as absolute marginal discrepancy.17 The internal fit was evaluated and divided into CG, AG, and OG. The vertical distance from the deepest of the margin to the inner surface of the crown was measured as CG. In the cross-section, the middle of the axial wall was defined as AG and the middle of the occlusal surface was defined as OG (Fig. 5). Each point was observed at 160× using a digital microscope (KH-7700, Hirox, Tokyo, Japan) and the thickness of the low-viscosity silicone was measured at each point.
Fig. 5. Sixteen measuring points for the marginal and internal gap of the crown. (A) Buccopalatal section, (B) Mesiodistal section. Marginal gap (MG): 1, 8, 9, 16; cervical gap (CG): 2, 7, 10, 15; axial gap (AG): 3, 6, 11, 14; occlusal gap (OG): 4, 5, 12, 13.
The measurement results were statistically analyzed with one-way ANOVA using SPSS for Windows (SPSS v20.0, IBM, Chicago, IL, USA). For post-hoc analysis, the Dunnett T3 method was used, since homogeneity was not assumed and the sample size was less than 50. The data was evaluated at a significance level of P < .05.
RESULTS
The measurement results of the marginal and internal gaps for each direction group are presented in Table 1. The gap in each group is the average of the 4 measuring points (buccal, palatal, mesial, and distal). One-way ANOVA indicated that the build directions have a significant influence on MG, CG, and OG. The post-hoc test was conducted to see if there were any significant differences between build angles in MG, CG, and OG.
Table 1. One-way ANOVA for marginal and internal gaps in 6 build direction groups.
| Group (°) | Mean (μm) | Standard deviation (SD) | F | P value | |
|---|---|---|---|---|---|
| MG | 120 | 113.66 | 78.30 | 6.467 | .000* |
| 135 | 73.13 | 48.48 | |||
| 150 | 58.52 | 32.32 | |||
| 180 | 65.18 | 36.04 | |||
| 210 | 69.86 | 39.32 | |||
| 225 | 75.41 | 40.45 | |||
| CG | 120 | 150.74 | 75.70 | 3.914 | .002* |
| 135 | 116.72 | 56.30 | |||
| 150 | 101.27 | 47.96 | |||
| 180 | 113.82 | 32.49 | |||
| 210 | 118.36 | 44.64 | |||
| 225 | 125.92 | 50.99 | |||
| AG | 120 | 52.37 | 28.79 | 1.532 | .181 |
| 135 | 57.50 | 32.94 | |||
| 150 | 57.36 | 31.26 | |||
| 180 | 69.03 | 32.86 | |||
| 210 | 55.97 | 23.81 | |||
| 225 | 55.50 | 24.78 | |||
| OG | 120 | 153.00 | 58.14 | 19.326 | .000* |
| 135 | 142.18 | 56.45 | |||
| 150 | 75.05 | 28.18 | |||
| 180 | 76.10 | 16.85 | |||
| 210 | 105.99 | 43.47 | |||
| 225 | 115.31 | 60.03 |
MG, Marginal gap; CG, Cervical gap; AG, Axial gap; OG, Occlusal gap.
*Differences significant at P < .05
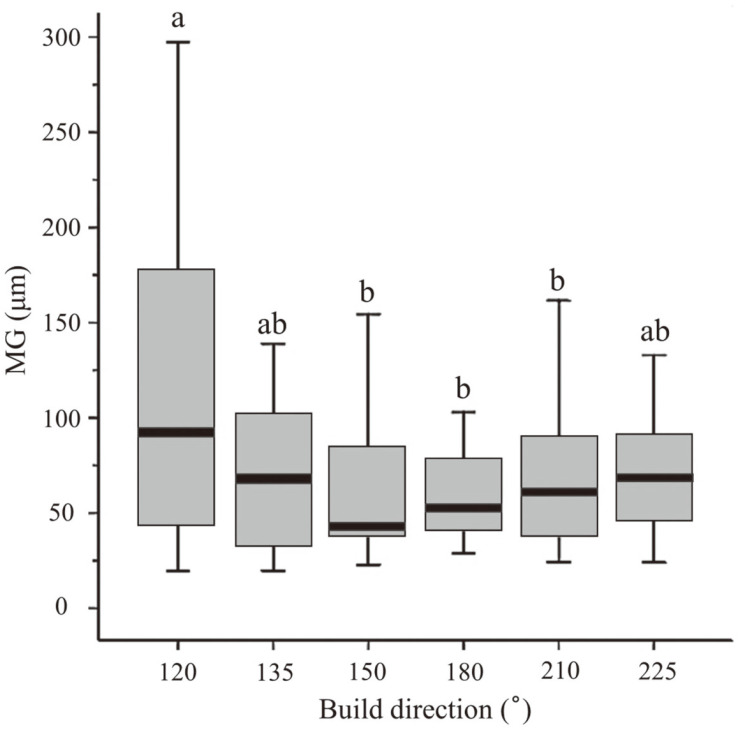
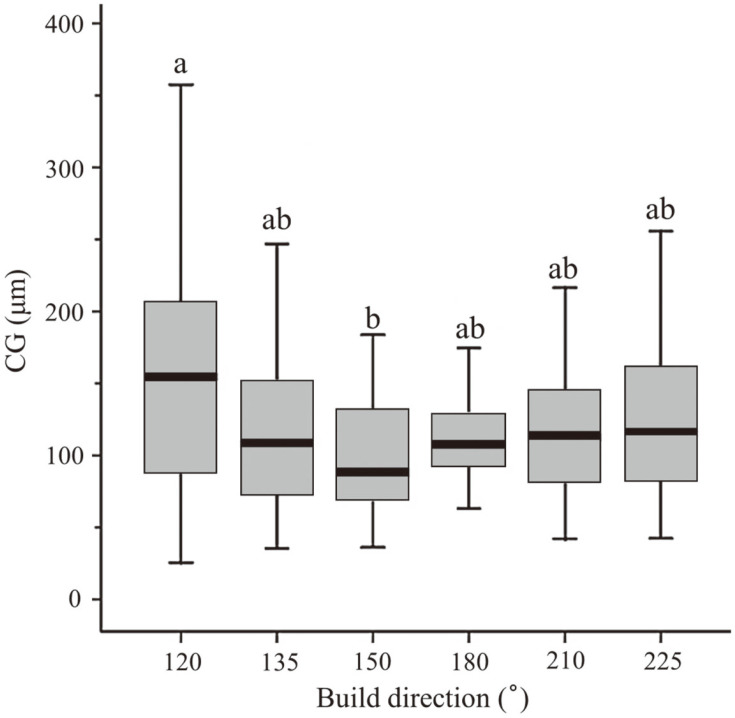
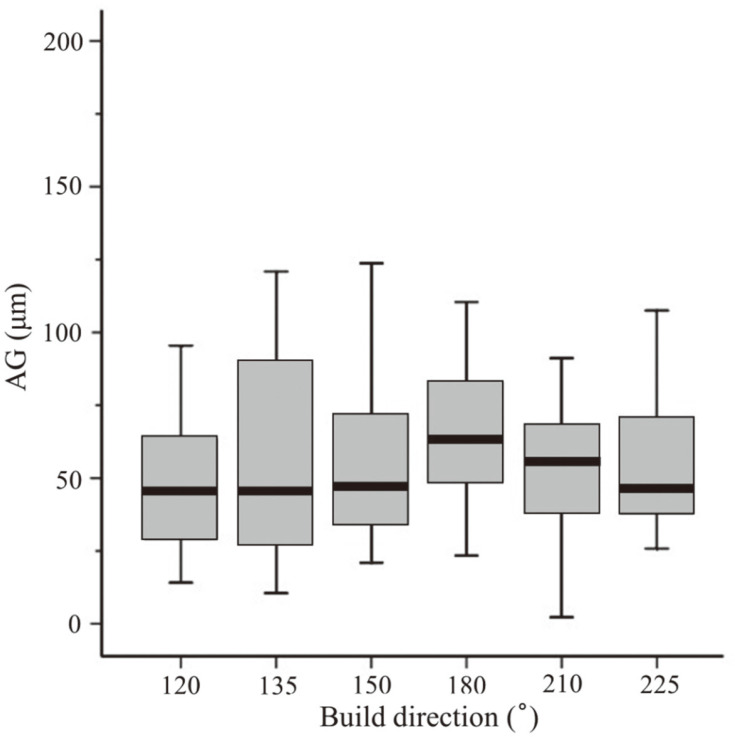
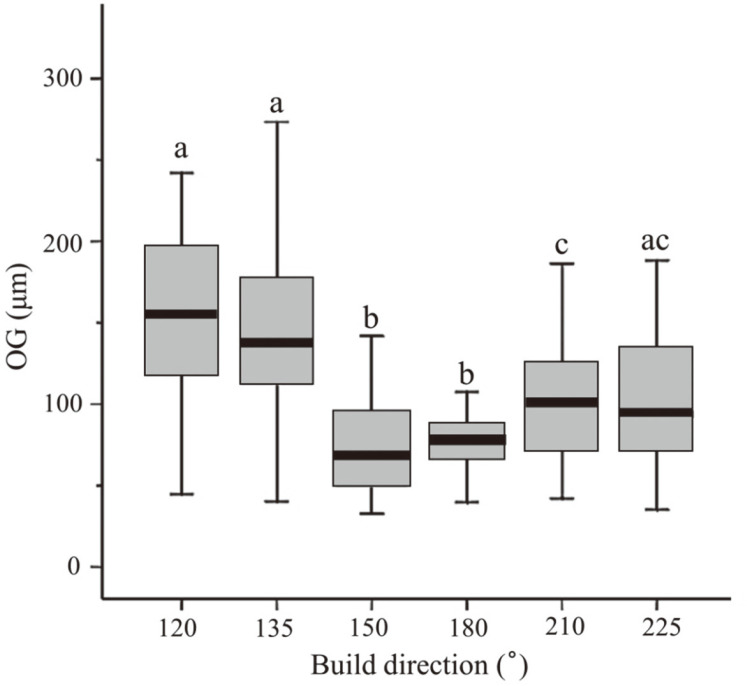
MG was significantly larger in the 120° group (113.6 ± 78.3 µm) than in the 150° (58.5 ± 32.3 µm), 180° (65.1 ± 36.0 µm), and 210° (69.8 ± 39.3 µm) groups (P < .05). There was no significant difference between the 150°, 180°, and 210° groups (P > .05). There was no significant difference from any build angle in the 135° and 225° groups in MG (P > .05) (Table 1, Fig. 6). CG was significantly larger in the 120° group (150.7 ± 75.6 µm) than in the 150° group (101.2 ± 47.9 µm) (P < .05). There was no significant difference between the 135°, 180°, 210°, and 225° groups (P > .05) (Table 1, Fig. 7). AG was not significantly different across all the build directions, showing a P-value of 0.181 (P > .05) (Table 1, Fig. 8). OG was the smallest in the 150° (75.0 ± 28.1 µm) and 180° (76.1 ± 16.8 µm) groups, followed by the 210° group (105.9 ± 43.4 µm), while it was the largest in the 120° (152.9 ± 58.1 µm) and 135°(142.1 ± 56.4 µm) groups. In addition, the OG was significantly larger in the 225° group (115.3 ± 60.0 µm) compared to the 150° and 180° groups (P < .05). The 225° group showed no significant difference from the 120°, 135°, and 210° group (P > .05) (Table 1, Fig. 9).
Fig. 6. Mean values of marginal gap in six build direction groups. Different letters indicate statistically significant differences among 6 groups (P < .05).
Fig. 7. Mean values of the cervical gap in six build direction groups. Different letters indicate statistically significant differences among 6 groups (P < .05).
Fig. 8. Mean values of axial gap in six build direction groups (P = .181).
Fig. 9. Mean values of occlusal gap in six build direction groups. Different letters indicate statistically significant differences among 6 groups (P < .05).
DISCUSSION
This study was conducted to evaluate the effect of build directions on the marginal and internal fit of the provisional crowns using SRT. As a result, there was a difference in the marginal and internal fit according to build directions. Thus, the null hypothesis was rejected.
In a previous study, Abdullah et al.18 evaluated a MG of provisional crowns made with 4 types of resin using low-viscosity silicone impression material and reported a mean MG of 47 – 193 µm. Yao et al.19 reported a MG of 150 – 280 µm, after fabricating provisional crowns using 4 resin types and attaching using glass ionomer cement. Belser et al.20 asserted that the clinically permissible MG in the final prosthesis was 120 µm, while Beuer et al.21 reported a range of 100 – 150 µm. In the present study, the MG was shown to be 58 – 113 µm, which falls within the clinically permissible range.
Internal fit affects the retention and resistance of the crown,22 in which OG is often the largest measured gap than CG or AG.23 According to Boitelle et al.,24 the internal fit of CAD/CAM prostheses made with various materials was 45 – 219 µm in the OG. Alharbi et al.11 reported an incisal gap of 169 µm in the 3D-printed anterior provisional crown, which was 1.5 times greater than the assigned cement gap. Kokubo et al.25 reported an incisal gap of 170 µm, which was 3 – 4 times greater than the cement gap. In this study, the cement gap was set to be 30 µm and the measured OG was 75 – 152 µm, which was 2.5 – 5 times greater. The AG shows a different pattern. Alharbi et al.11 reported an AG of 41 µm, which is smaller than the defined cement gap of 60 µm. In this study, the AG was 52 – 69 µm, which was smaller than OG and CG. This was due to the errors in STL file splitting, thus it is necessary to increase the cement gap in the axial wall to enhance the fit.11
Park et al.26 studied 3D-printed 3-unit fixed partial dentures using resin in 5 build angles (0°, 30°, 45°, 60°, 90°) and found a significant difference in the marginal and internal fit, in which the optimal build angles were 45° and 60°, corresponding to 135° and 120° in our study. Alharbi et al.12 compared the three-dimensional accuracy of resin crowns 3D-printed at 9 different angles using superimposition software and concluded that the optimal build angle was 120°, considering the position of support and time needed for finishing and polishing. In addition, Osman et al.13 compared the three-dimensional accuracy of DLP-printed resin crowns and reported 135° as the optimal angle. In this study, MG and CG were significantly larger in the 120° group than in other groups, while OG was the smallest in the 150° and 180° and the largest in the 120° and 135° groups. Therefore, considering the marginal and internal fit, 150° and 180° are recommended as the optimal build angles.
There are various reasons for the differences in the marginal and internal fit based on the build angle. First, the form of the layer created by the 3D printer differs according to the build angle. Since a DLP-based 3D printer polymerizes one layer at a time, any change in the layer form entails changes in the form and degree of polymerization shrinkage.27,28 For example, in the case of a hollow cylindrical object, there is a part that is consistently exposed to light, which affects the internal fit.13 Moreover, the position of support attachment changes with the build angle. Errors can arise from the unsupported section. If support is attached close to the crown margin, then unwanted damage can be incurred during the removal of the support.12 Although supports were attached symmetrically in the 150° and 210° groups, OG was significantly larger in the 210° group whose support was located more buccally. The number of supports was 13 in the 150° group and 11 in the 210° group, which explains the error in the 210° group by its relatively fewer supports.
Osman et al.13 fabricated and scanned provisional crowns in 9 different angles using a DLP-based method and obtained a color map by superimposing with original data, which showed a positive change in the internal surfaces of the supported area and the opposite area when build angles of 90°, and 270° were used. This can be explained by the gravitational effects on the liquid medium as the platform moves up and down during printing. In the preliminary experiments of this study, 90°, 240°, and 270° were excluded from the experimental group for imperfect fit, which can be explained by the same reason. Furthermore, AG was smaller in the 120° group than in other groups, while OG and CG were larger, suggesting that fit was imperfect in the axial plane.
Attempts have been made in many studies to reduce the area of support by changing the build angle.4,29,30,31 Attaching support to the object increases the printing time and the amount of material used, while removing the support requires a considerable amount of manual work and time and can degrade surface quality.32 Here, the build angle is selected manually, semi-automatically or automatically. In the manual mode, the user can directly set the build angle on the platform. In the semi-automatic mode, the angle is determined based on the feedback information on printing time and support area. In the automatic mode, it is determined by a specific algorithm that takes the printing time, as well as the amount and area of support into account.33 Previous studies have proposed various algorithms to find the optimal build angle.34,35 The differences in fit after applying various algorithms must be further studied.
In this study, when the provisional crowns were printed at an build direction of 120° to 225° using a DLP 3D printer, the optimal build angles were 150° and 180°. However, the limitation is that the cement thickness to which the crown was suitable at all angles was not set. As a result, the difference in the fit according to the position of the support was not comparable in all build angles. Also, further studies are needed to evaluate the influence of various parameters such as layer thickness, support type and location on the platform that should be considered during crown printing.
CONCLUSION
When provisional crowns were fabricated using a DLP-based 3D printer within the limits of this study, the marginal fit was shown to be clinically permissible across all build angles. The internal fit was shown to be different in the cervical and occlusal surfaces depending on the build angle. Considering the marginal and internal fit, 150° and 180° are recommended as the optimal build angles.
Footnotes
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government(MSIT) (No. NRF-2017R1C1B5018275).
References
- 1.Berman B. 3-D printing: The new industrial revolution. Bus Horiz. 2012;55:155–162. [Google Scholar]
- 2.Azari A, Nikzad S. The evolution of rapid prototyping in dentistry: a review. Rapid Prototyp J. 2009;15:216–225. [Google Scholar]
- 3.Andersen UV, Pedersen DB, Hansen HN, Nielsen JS. Inprocess 3D geometry reconstruction of objects produced by direct light projection. Int J Adv Manuf Technol. 2013;68:565–573. [Google Scholar]
- 4.Mitteramskogler G, Gmeiner R, Felzmann R, Gruber S, Hofstetter C, Stampfl J, Ebert J, Wachter W, Lanubersheimer J. Light curing strategies for lithography-based additive manufacturing of customized ceramics. Addit Manuf. 2014;1:110–118. [Google Scholar]
- 5.Duke ES. Provisional restorative materials: a technology update. Compend Contin Educ Dent. 1999;20:497–500. [PubMed] [Google Scholar]
- 6.Hamza TA, Rosenstiel SF, El-Hosary MM, Ibraheem RM. Fracture resistance of fiber-reinforced PMMA interim fixed partial dentures. J Prosthodont. 2006;15:223–228. doi: 10.1111/j.1532-849X.2006.00110.x. [DOI] [PubMed] [Google Scholar]
- 7.Digholkar S, Madhav VN, Palaskar J. Evaluation of the flexural strength and microhardness of provisional crown and bridge materials fabricated by different methods. J Indian Prosthodont Soc. 2016;16:328–334. doi: 10.4103/0972-4052.191288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monday JJ, Blais D. Marginal adaptation of provisional acrylic resin crowns. J Prosthet Dent. 1985;54:194–197. doi: 10.1016/0022-3913(85)90285-9. [DOI] [PubMed] [Google Scholar]
- 9.Cheng W, Fuh J, Nee A, Wong Y, Loh H, Miyazawa T. Multiobjective optimization of part-building orientation in stereolithography. Rapid Prototyp J. 1995;1:12–23. [Google Scholar]
- 10.Park JY, Kim HY, Kim JH, Kim JH, Kim WC. Comparison of prosthetic models produced by traditional and additive manufacturing methods. J Adv Prosthodont. 2015;7:294–302. doi: 10.4047/jap.2015.7.4.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alharbi N, Alharbi S, Cuijpers VMJI, Osman RB, Wismeijer D. Three-dimensional evaluation of marginal and internal fit of 3D-printed interim restorations fabricated on different finish line designs. J Prosthodont Res. 2018;62:218–226. doi: 10.1016/j.jpor.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Alharbi N, Osman RB, Wismeijer D. Factors influencing the dimensional accuracy of 3D-printed full-coverage dental restorations using stereolithography technology. Int J Prosthodont. 2016;29:503–510. doi: 10.11607/ijp.4835. [DOI] [PubMed] [Google Scholar]
- 13.Osman RB, Alharbi N, Wismeijer D. Build angle: Does it influence the accuracy of 3D-printed dental restorations using digital light-processing technology? Int J Prosthodont. 2017;30:182–188. doi: 10.11607/ijp.5117. [DOI] [PubMed] [Google Scholar]
- 14.Laurent M, Scheer P, Dejou J, Laborde G. Clinical evaluation of the marginal fit of cast crowns-validation of the silicone replica method. J Oral Rehabil. 2008;35:116–122. doi: 10.1111/j.1365-2842.2003.01203.x. [DOI] [PubMed] [Google Scholar]
- 15.Son K, Lee S, Kang SH, Park J, Lee K, Jeon M, Yun BJ. A comparison study of marginal and internal fit assessment methods for fixed dental prostheses. J Clin Med. 2019;8:785. doi: 10.3390/jcm8060785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu JC, Wilson PR. Optimal cement space for resin luting cements. Int J Prosthodont. 1994;7:209–215. [PubMed] [Google Scholar]
- 17.Holmes JR, Bayne SC, Holland GA, Sulik WD. Considerations in measurement of marginal fit. J Prosthet Dent. 1989;62:405–408. doi: 10.1016/0022-3913(89)90170-4. [DOI] [PubMed] [Google Scholar]
- 18.Abdullah AO, Tsitrou EA, Pollington S. Comparative in vitro evaluation of CAD/CAM vs conventional provisional crowns. J Appl Oral Sci. 2016;24:258–263. doi: 10.1590/1678-775720150451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yao J, Li J, Wang Y, Huang H. Comparison of the flexural strength and marginal accuracy of traditional and CAD/CAM interim materials before and after thermal cycling. J Prosthet Dent. 2014;112:649–657. doi: 10.1016/j.prosdent.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 20.Belser UC, MacEntee MI, Richter WA. Fit of three porcelain-fused-to-metal marginal designs in vivo: a scanning electron microscope study. J Prosthet Dent. 1985;53:24–29. doi: 10.1016/0022-3913(85)90058-7. [DOI] [PubMed] [Google Scholar]
- 21.Beuer F, Neumeier P, Naumann M. Marginal fit of 14-unit zirconia fixed dental prosthesis retainers. J Oral Rehabil. 2009;36:142–149. doi: 10.1111/j.1365-2842.2008.01908.x. [DOI] [PubMed] [Google Scholar]
- 22.Nakamura T, Dei N, Kojima T, Wakabayashi K. Marginal and internal fit of Cerec 3 CAD/CAM all-ceramic crowns. Int J Prosthodont. 2003;16:244–248. [PubMed] [Google Scholar]
- 23.Scherrer SS, de Rijk WG, Belser UC, Meyer JM. Effect of cement film thickness on the fracture resistance of a machinable glass-ceramic. Dent Mater. 1994;10:172–177. doi: 10.1016/0109-5641(94)90028-0. [DOI] [PubMed] [Google Scholar]
- 24.Boitelle P, Mawussi B, Tapie L, Fromentin O. A systematic review of CAD/CAM fit restoration evaluations. J Oral Rehabil. 2014;41:853–874. doi: 10.1111/joor.12205. [DOI] [PubMed] [Google Scholar]
- 25.Kokubo Y, Nagayama Y, Tsumita M, Ohkubo C, Fukushima S, Vult von Steyern P. Clinical marginal and internal gaps of In-Ceram crowns fabricated using the GN-I system. J Oral Rehabil. 2005;32:753–758. doi: 10.1111/j.1365-2842.2005.01506.x. [DOI] [PubMed] [Google Scholar]
- 26.Park GS, Kim SK, Heo SJ, Koak JY, Seo DG. Effects of printing parameters on the fit of implant-supported 3D printing resin prosthetics. Materials (Basel) 2019;12:2533. doi: 10.3390/ma12162533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tahayeri A, Morgan M, Fugolin AP, Bompolaki D, Athirasala A, Pfeifer CS, Ferracane JL, Bertassoni LE. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent Mater. 2018;34:192–200. doi: 10.1016/j.dental.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Unkovskiy A, Bui PH, Schille C, Geis-Gerstorfer J, Huettig F, Spintzyk S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent Mater. 2018;34:e324–e333. doi: 10.1016/j.dental.2018.09.011. [DOI] [PubMed] [Google Scholar]
- 29.Frank D, Fadel G. Expert system-based selection of the preferred direction of build for rapid prototyping processes. J Intell Manuf. 1995;6:339–345. [Google Scholar]
- 30.Pham D, Dimov S, Gault R. Part orientation in stereolithography. Int J Adv Manuf Technol. 1999;15:674–682. [Google Scholar]
- 31.Strano G, Hao L, Everson R, Evans K. A new approach to the design and optimisation of support structures in additive manufacturing. Int J Adv Manuf Technol. 2013;66:1247–1254. [Google Scholar]
- 32.Jiang J, Xu X, Stringer J. Support structures for additive manufacturing: A review. J Manuf Mater Process. 2018;2:64 [Google Scholar]
- 33.Pandey PM, Reddy NV, Dhande SG. Slicing procedures in layered manufacturing: a review. Rapid Prototyp J. 2003;9:274–288. [Google Scholar]
- 34.Pandey PM, Thrimurthulu K, Reddy NV. Optimal part deposition orientation in FDM by using a multicriteria genetic algorithm. Int J Prod Res. 2004;42:4069–4089. [Google Scholar]
- 35.Paul R, Anand S. Optimization of layered manufacturing process for reducing form errors with minimal support structures. J Manuf Syst. 2015;36:231–243. [Google Scholar]