Abstract
During the development of the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV2), a myriad of complications has emerged and although rare, several genitourinary complications have been reported. The bulk of these complications have been secondary to hypercoagulable states, such as priapism. Previous SARS family infections have caused orchitis, though no adult cases of orchitis have been reported. We describe a novel case of SARS-CoV2 bilateral orchitis in a previously healthy 37-year-old male who presented for testicular pain with constitutional symptoms. Additionally, there was no epididymitis associated with the bilateral orchitis. Based on both data in SARS-CoV2 infected males and previous data from prior SARS infections, spermatocyte function may be compromised secondary to this infection. With the various symptoms associated with this virulent pathogen, we characterize the potential complications and importance of fertility follow up.
Keywords: COVID-19, Orchitis, SARS-CoV2
1. Introduction
Occurring in both pediatric and adult males, orchitis presents in a bimodal distribution [1]. Sexually transmitted infections and orthomyxoviruses account for the younger age group of 16 to 30 years old while bacterial urinary pathogens predominate the older distribution of 51–70 years old, especially if benign prostatic hypertrophy is present [[1], [2], [3]]. Bacterial orchitis rarely occurs without concomitant epididymitis [1]. Mumps is the most common virus to cause orchitis and of the prepubertal males that develop mumps, 20% will develop this complication [4]. While many viruses may account for orchitis in both the immunocompetent and immunocompromised state, we present a novel cause of coronavirus disease 2019 (COVID-19) orchitis.
2. Case presentation
A 37-year-old previously healthy male presented to the emergency department (ED) complaining of bilateral testicular warmth and discomfort as well as fevers, anorexia, myalgias, fatigue, and non-productive cough. He noted that these constitutional symptoms progressed for the past 10 days, with the bilateral testicular pain developing over the past 3 days. The patient was diagnosed with COVID-19 by nasopharyngeal polymerase chain reaction at an outpatient clinic 15 days prior to presentation to the ED. His review of systems was otherwise unremarkable and he had no recent travel or high-risk SARS-CoV2 contacts.
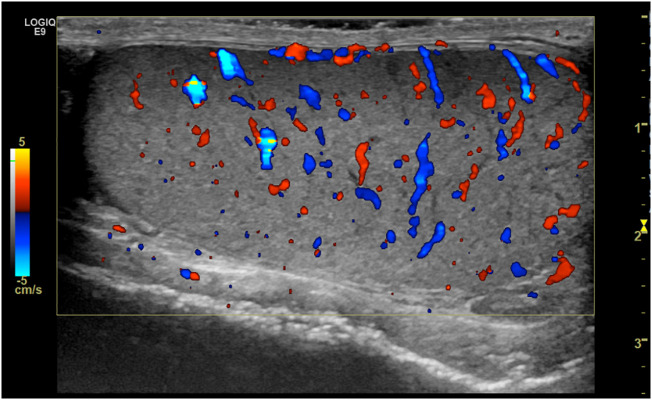
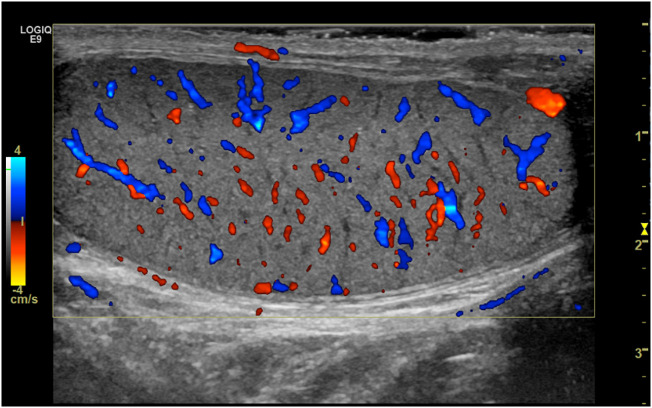
The patient's initial vital signs were blood pressure of 119/69, heart rate 97, respiratory rate 20, oxygen saturation 96% on room air with a temperature of 100.8 degrees Fahrenheit. Physical exam was notable for mild rhonchi in bilateral lung bases as well as scrotal erythema and mild bilateral testicular discomfort without epididymal tenderness or abnormal lay. Laboratory evaluation demonstrated a complete blood count with lymphopenia, a normal compreshensive metabolic panel, unremarkable urinalysis, Procalcitonin of 0.15 ng/mL, a positive nasopharyngeal polymerase chain reaction for SARS-CoV2, non-reactive Syphilis, non-reactive T. pallidum antibody, negative urine nucleic amplification assay for N. gonorrhea and C. trachomatis and a urine culture without growth. Chest radiograph and computed tomography without contrast revealed peripheral mid to lower hazy pulmonary opacities (Fig. 1 ) consistent with COVID-19 infection. On testicular ultrasound, bilateral non-specific increased blood flow was present consistent with orchitis (Fig. 2, Fig. 3 ). The patient received 1000 mg of Acetaminophen as well as 1000 mg of cefepime intravenously and 1000 mg orally of azithromycin. The patient was admitted to the hospitalist with a stable clinical course not requiring supplemental oxygen and was discharged home on hospital day 2 with mildly improved testicular pain.
Fig. 1.
Non-contrasted computed tomography with axial slice showing bilateral interstitial infiltrates without consolidation consistent with SARS-CoV2 infection.
Fig. 2.
Transverse color Doppler ultrasound of the right testis demonstrating increase bilateral testicular flow.
Fig. 3.
Transverse color Doppler ultrasound of the left testis demonstrating increase bilateral testicular flow.
3. Discussion
As the SARS-CoV2 pandemic continues to affect the population worldwide, rare complications should be characterized in order better recognize associated symptoms. Similar to the proposed mechanism for pulmonary virulence, the pathophysiology for SARS-CoV2 orchitis relies on the primary receptor on Leydig cells in the testis being the ACE2 receptor, facilitating cellular entry [5]. While SARS-CoV2 has not been cultured in urine samples, semen in males infected with SARS-CoV2 demonstrates impaired spermatocyte quality, potentially having a future impact on male fertility [6].
Similarly, previous SARS virus family infections have caused orchitis and epididymitis with subsequent spermatogenic tubule destruction as well as oligospermia and azoospermia [7]. This novel case of bilateral adult orchitis without epididymitis may potentially follow suit. One case of epididymo-orchitis secondary to SARS-CoV2 has been reported in a previously healthy 14-year-old male [8]. This pattern of concomitant epididymitis with orchitis is more typical as compared to the above case of isolated viral orchitis. Additionally, thrombotic complications of SARS-CoV2 may affect the genitourinary system as well, with priapism reported in a critically ill patient with acute respiratory distress syndrome and coagulopathic complications [9].
4. Conclusion
With the progression of the SARS-CoV2 pandemic, rare reproductive complications should be characterized. Identification of infrequent genitourinary effects may help emergency physicians identify this disease at the earliest junction and trigger appropriate treatment, quarantine, and fertility follow-up.
Disclaimer
The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, the Department of the Air Force and Department of Defense or the U.S. Government.
Presentations
None.
Publications (Print and Online)
None.
Funding
None.
Declaration of Competing Interest
None.
Acknowledgements
None.
References
- 1.Manavi K., Turner K., Scott G.R., Stewart L.H. Audit on the management of epididymo-orchitis by the Department of Urology in Edinburgh. Int J STD AIDS. 2005;16(5):386–387. doi: 10.1258/0956462053888853. [DOI] [PubMed] [Google Scholar]
- 2.Redfern T.R., English P.J., Baumber C.D., McGhie D. The aetiology and management of acute epididymitis. Br J Surg. 1984;71(9):703–705. doi: 10.1002/bjs.1800710921. [DOI] [PubMed] [Google Scholar]
- 3.Delavierre D. Orchi-epididymitis. Ann Urol (Paris) 2003;37(6):322–338. doi: 10.1016/j.anuro.2003.01.002. [DOI] [PubMed] [Google Scholar]
- 4.Gazibera B., Gojak R., Drnda A., et al. Spermiogram part of population with the manifest orchitis during an ongoing epidemic of mumps. Med Arh. 2012;66(3 Suppl. 1):27–29. doi: 10.5455/medarh.2012.66.s27-s29. [DOI] [PubMed] [Google Scholar]
- 5.Douglas G.C., O’Bryan M.K., Hedger M.P., et al. The novel angiotensin-converting enzyme (ACE) homolog, ACE2, is selectively expressed by adult leydig cells of the testis. Endocrinology. 2004;145(10):4703–4711. doi: 10.1210/en.2004-0443. [DOI] [PubMed] [Google Scholar]
- 6.Holtmann N., Edimiris P., Andree M., et al. Assessment of SARS-CoV-2 in human semen—a cohort study. Fertil Steril. 2020;114(2) doi: 10.1016/j.fertnstert.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu J., Qi L., Chi X., et al. Orchitis: a complication of severe acute respiratory syndrome (SARS) Biol Reprod. 2006;74(2):410–416. doi: 10.1095/biolreprod.105.044776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gagliardi L., Bertacca C., Centenari C., et al. Orchiepididymitis in a boy with COVID-19. Pediatr Infect Dis J. 2020;8:200–202. doi: 10.1097/inf.0000000000002769. [DOI] [PubMed] [Google Scholar]
- 9.Lamamri M., Chebbi A., Mamane J., et al. Priapism in a patient with coronavirus disease 2019 (COVID-19): a case report. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]