Abstract
This themed issue on global health research has come at an opportune time in the middle of the ongoing global public health crisis arising from the coronavirus disease (COVID-19) pandemic which has claimed nearly 756,000 lives in 210 countries and territories around the world as of August 15, 2020. The public health crisis underscores the importance of global health research partnerships and collaborations to develop and evaluate the requisite health technologies to assist in containing COVID-19, other diseases, and health-related concerns that defy national borders. The 17 Sustainable Development Goals (SDGs), adopted by the member countries of the United Nations in September 2015, provide a framework for global development efforts including global health research. SDG3, which promotes health and well-being for the world populations across the age spectrum, highlights disease areas for special focus which can be adapted in specific global health research programs to serve local health needs. SDG17 promotes partnerships between high income (HIC) and low and middle-income countries (LMIC) for sustainable and equitable global development. However, given the wide disparities in fiscal and overall capacity for research between researchers in HIC and their counterparts in LMIC as well as the greater vulnerabilities of the LMIC communities when serving as research locations, a spotlight on the nature of such global health research partnerships in the context of the SDGs is desirable. This is to ensure that they are meaningful and mutually-beneficial partnerships which address local health concerns and promote long-term value for the communities involved.
The objective of this commentary is, therefore, to provide a brief overview of the SDGs by way of context; explore the power differences at play when researchers from HIC are seeking research opportunities in LMIC; examine the social determinants of health and the disproportionate burden of global diseases carried by populations in LMIC to establish their vulnerability; discuss global research partnerships; and attempt to make a case for why community-based participatory research may be the preferred type of global health research partnership in the context of the SDGs.
Keywords: Sustainable development goals, SDGs, Agenda for sustainable development, Global health research, Research partnerships, Global health research partnerships, Community-based participatory research, CBPR
Introduction
This themed issue on global health research is particularly timely during the ongoing COVID-19 pandemic which has claimed nearly 756,000 lives globally from the over 21 million confirmed cases as of August 15, 2020.1 Since COVID-19 transcends national borders, global partnerships and collaborations are needed towards the development and assessment of technologies, including vaccines and therapeutics, required to contain this and other health threats in order to benefit global health and the economy.2 The importance of such partnerships in this era of globalization has been reinforced by the 17 Sustainable Development Goals (SDGs) which provide the framework for promoting sustainable and equitable development, including global health research, for the next 15 years (2015–2030).3, 4, 5, 6 SDG 17 is the goal for development partnerships and seeks to promote inter-country partnerships aiming to reduce the disparities gap between the high income countries (HIC) and their counterparts in low and middle-income countries (LMIC) through strategies that include information sharing, technology transfer, and opportunities for research.3, 4, 5, 6 SDG3 focuses on the promotion of health of people across the age spectrum and may, thus, provide the starting point for the discussion and identification of priority research areas of focus to meet the needs of communities in LMIC where global health research may be located.3, 4, 5, 6 However, given the wide health disparities along with the disparities in fiscal aspects and overall capacity for research between researchers in HIC and their counterparts in LMIC and the greater vulnerabilities of the communities in the latter countries when serving as research locations,7 , 8 a spotlight on the nature of such global health research partnerships in the context of the SDGs is desirable. This is to ensure that such global health research partnerships are meaningful and mutually-beneficial by addressing local health concerns and promoting long-term value for the communities involved.
The objective of this commentary is, therefore, to contextualize this discussion on global health research partnerships with an overview of the SDGs; explore the power differences at play when researchers from HIC are seeking research opportunities in LIMC; examine the social determinants of health and the disproportionate burden of global diseases carried by populations in LMIC to establish their vulnerability; discuss global research partnerships; and attempt to make a case for why community-based participatory research may be the preferred type of global health research partnership in the context of the SDGs.
Overview of the Sustainable Development Goals (SDGs)
“Transforming our World: The 2030 Agenda for Sustainable Development” was adopted by the Heads of State and Government at a special summit of the United Nations (UN) on September 25, 20153, 4, 5, 6 to complete the global developmental agenda began by its predecessor, the Millennium Development Goals (MDGs).9, 10, 11 The Agenda for Sustainable Development with its 17 Sustainable Development Goals (SDGs) [Table 1 ]3, 4, 5, 6 and their 169 targets were meant to continue the work began by the MDGs,9, 10, 11 but with a much greater focus on environmental, social, and economic sustainability.3, 4, 5, 6 Unlike the MDGs which had three separate health-related goals, SDG3 (Ensure healthy lives and promote well-being for all at all ages) is the only direct health-related goal; however, the other SDGs also impact health, although indirectly.3, 4, 5, 6 The 13 targets for SDG3 provide an effective umbrella for all the major global health concern areas.3, 4, 5, 6
Table 1.
The Sustainable Development Goals (SDGs).4
| The Sustainable Development Goals (SDGs) | Goal Description |
|---|---|
| SDG1 | No Poverty |
| SDG2 | Zero Hunger |
| SDG 3 | GOOD HEALTH & WELL-BEINGa |
| SDG4 | Quality Education |
| SDG5 | Gender Equality |
| SDG6 | Clean Water & Sanitation |
| SDG7 | Affordable and Clean Energy |
| SDG8 | Decent Work & Economic Growth |
| SDG9 | Industry, Innovation, Infrastructure |
| SDG10 | Reduced Inequalities |
| SDG11 | Sustainable Cities & Communities |
| SDG12 | Responsible Consumption, Production |
| SDG13 | Climate Action |
| SDG14 | Life Below Water |
| SDG15 | Life on Land |
| SDG16 | Peace, Justice & Strong Institutions |
| SDG17 | Partnerships for the Goals |
SDG3: Ensure healthy lives and promote well-being for all at all ages.
The core global health focus areas to be addressed under SDG3 can be summarized as follows:3, 4, 5, 6
-
•
End the global epidemics of HIV/AIDS, TB, Malaria, and other communicable diseases
-
•
Reduce by one-third premature mortality by non-communicable diseases
-
•
Reduce infant and under 5 mortality ratios
-
•
Reduce maternal mortality ratios
-
•
Promote universal access to safe, effective, quality, and affordable essential medicines and vaccines for all.
SDGs and global health research
The importance of the SDGs in the context of global health research is that SDG3 may provide a reference point from which research partners can start their discussions to identify and reach consensus regarding their priorities, particularly with respect to research located in LMIC.3, 4, 5, 6 Even though these countries carry the global burden of many diseases, studies have shown that researchers from them may not be the major recipients of grant funding for global health research.12 A systematic review has pointed out the disproportionate concentration of first and coauthors on health inequalities scientific literature in HIC, effectively eclipsing researchers from LMIC.12 This calls for a closer look at global health research partnerships and collaborations and how these may be developed, implemented, monitored, and evaluated to ensure greater and more sustainable benefits to the local communities in which these research studies are located.
In the context of this theme issue on global health research, attention is being drawn to another goal in the Sustainable Development Goals, i.e. SDG 17-“Partnerships for the Goals,” that is, partnerships for achieving the other 16 SDGs including the health-related SDG3.13 The global community recognizes the fact that the SDGs can only be achieved through strong global partnerships and collaborations; hence, SDG17 identifies five target areas for focus, namely: finance, technology, capacity building, trade, and systemic issues.13 In particular, the goal calls for improving access to technology and knowledge to facilitate the sharing of ideas and innovation; global health research partnerships hence falls under this purview.13
Power differences at play when researchers from HIC are seeking research opportunities in LMIC
Availability of grant funding for researchers in HIC has been reported as a major source of disparity between potential partners in LMIC and provides the former with undue power advantage over the latter with whom they seek to collaborate.8 It has been estimated that the total funding available for research from private and public sources is in the region of $73 billion/year.8 However, the concept of the “10/90 gap” which refers to the availability of only 10% of global health research funding for diseases with the highest global prevalence in LMIC and 90% to those affecting populations in HIC has been described in the biomedical literature.8 , 12 , 14, 15, 16
Apart from the greater availability of funding for researchers in HIC, they also have access to better educational, training, and other resources for research, higher socioeconomic and developmental status, and more stable sociopolitical systems that provide them with the relative mental stability and the freedom to focus on higher level human pursuits including research. On the other hand, their counterparts in LMIC may need to be dealing with everyday stresses including inadequate health and educational resources, unstable sociopolitical systems, and other constraints that may not provide the optimum environmental and systemic support that facilitates research activities. These disparities, working in the favor of researchers from HIC, may make it easier for them to dictate the terms of the “partnership” or collaboration with those in LMIC including the research agenda setting, priorities, and authorship since the former holds the research funding purse, among other resources.16
Social determinants of health and disease burdens in LMIC countries serving as locations for global health research
To put the reported wide disparities in research funding availability between HIC and LMIC into context, a discussion of the social determinants of health in the latter countries is needed since they frequently serve as global health research locations. Social Determinants of Health according to WHO, describe the “circumstances in which people grow, live, work, and age, and the systems put in place to deal with illness.17 , 18 These conditions are in turn shaped by the prevailing political, social, and economic forces at work.17 , 18 The SDGs provide a framework by which countries around the globe can be objectively evaluated with respect to their prevailing social determinants of health.3, 4, 5, 6
The importance of the social determinants of health is better understood when seen through the lens of the global burden of disease that LMIC carry. WHO data indicates that in year 2018, the number of people living with HIV/AIDS (PLWHA) globally was 37.9 million, along with 770,000 AIDS-related deaths; over 66% of PLWHA were living in LMIC particularly in Africa.19 Similarly, over 50% of the estimated 10 million/year global TB cases and the 1.5 million deaths in 2018 occurred in 8 LMIC,20 and the 228 million cases of malaria and 405,000 deaths in 2018 occurred mostly in sub-Saharan Africa.21 LMIC are also increasingly shouldering the greater burden of noncommunicable diseases (NCDs) and their associated premature mortality; 75% of the global 16 million NCD deaths in 2018 occurred in LMIC.22
Hence, the combination of low research funds, relatively poorer social determinants of health (including weaker healthcare systems and infrastructure),23 and higher burden of diseases of global health importance, increases the vulnerability of countries and communities in LMIC for potential exploitation by researchers from HIC. Thus, there is a need to highlight the nature of global health research partnerships and collaborations between HIC and LMIC in the context of the SDGs.
Global health research partnerships
Dr. Margaret Chan, Director General of the World Health Organization (WHO)[2007–2017] had this to say about global health partnerships and collaborations in 2006 during her acceptance speech; “Today, collaboration to achieve public health goals is no longer simply an asset. It is a critical necessity. WHO needs to develop an approach to collaboration that emphasizes management of diversity and complexity.“ 24 The current WHO Director-General Dr. Tedros Adhanom Ghebreyesus has also expressed the following vision, “I envision a world in which everyone can live healthy, productive lives, regardless of who they are or where they live. I believe the global commitment to sustainable development-enshrined in the Sustainable Development Goals-offers a unique opportunity to address the social, economic, and political determinants of health and to improve the health and well-being of people everywhere.“25 Taken together, these two statements from the global health leadership point to the need for global health research partnerships to be developed taking full cognizance of the differences in the social determinants of health of the partners, including the sociocultural and political contextual environment of the research location. These considerations should ideally assist in prioritizing research focus area(s) to meet the specific needs and aspirations of LMIC communities, increase research relevance, and optimize the long-term impact of findings. This would be a win-win situation for the partners as they are bound to strengthen the research partnership and collaboration over the long term.
However, historically, and until recently, the type of research collaborations based in the poorer countries of the world, mostly in Africa, Asia, and Latin America (i.e. LMIC), and those from the richer countries in North America, Europe, Japan, Australia, and New Zealand (HIC) had followed what had been referred to as “north-south” collaborations, where those from the “north” were perceived as the “givers” and those from the “south” as the “receivers.“26, 27, 28, 29 Given this historical context, the types of research collaborations located in LMIC communities between individuals and institutions from HIC and LMIC used to be described by some as “scientific colonialism,” since the fund holders from the HIC often dictated the research agenda, and benefits accruing to them were frequently not known by LMIC partners as they were often packaged as “development aid” for which the latter were expected to receive with gratitude.26, 27, 28, 29
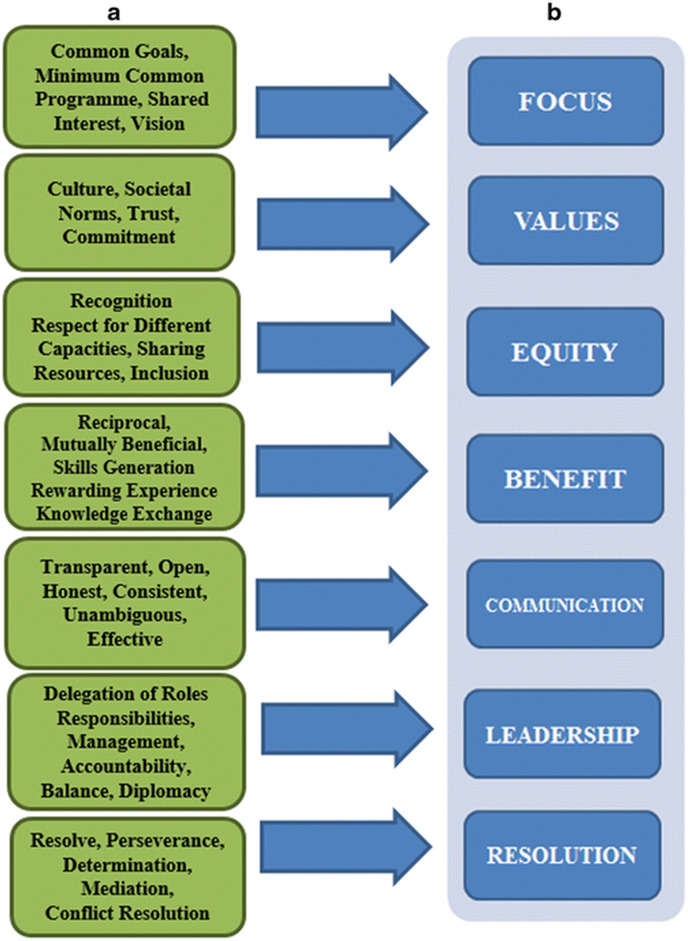
Fortunately, global health research partnerships have been evolving since the adoption of the global development frameworks embodied by the MDGs9, 10, 11 and currently the SDGs,3, 4, 5, 6 as being reflected by the global health leadership.24 , 25 Partnerships for the goals and for sustainable development, including global health research, are key components of both frameworks.3, 4, 5, 6 , 9, 10, 11 To support the ongoing evolvement of global health research partnerships, Larkan et al. have developed a framework for successful partnerships.30 These researchers from the Centre for Global Health, Trinity College, Dublin, have defined health partnerships as “contextually relevant peer-to-peer collaborations which offer a platform for sharing knowledge and growing expertise globally, working towards a common goal, across disciplines and perspectives.“30 Based on primary research data collected from 22 of their 40 global partnerships and collaborators around the world, Larkan et al. have outlined a framework of seven core principles and their attributes for developing, implementing, monitoring, and evaluating successful global health partnerships (Fig. 1 ).30 These core principles-focus, values, equity, benefit, communication, leadership, and resolution-were found to cut across all partnership types globally, irrespective of context.30 The researchers found no evidence of hierarchy with respect to the relative importance of these core concepts/principles and, therefore, recommended all to be accorded equal importance for successful global health research partnerships.30
Fig. 1.
Consolidated sets of attributes (a) and derived core concepts (b) for successful research partnerships in Global Health.27
Making a case for community-based participatory research: A viable option for global health research partnership
Having established the vulnerability of the communities in which global health research is frequently located, attention is increasingly being drawn to the important role that the community as a whole can play in such research undertakings.31 Some have identified such greater community awareness and involvement as the most important recent development in biomedical ethics.31 These developments have given rise to research partnerships commonly referred to as community-based participatory research (CBPR).31, 32, 33, 34, 35, 36, 37
CBPR approaches are particularly suited for global health research because they take into account the prevailing social determinants of health which have been identified frequently as the root causes of global health disparities17 , 18; and they also are in line with the vision of the WHO for global health partnerships.24 , 25 CBPR recognizes that individuals are “embedded within social, political, and economic systems that shape behaviors and access to resources necessary to maintain health.31, 32, 33, 34, 35, 36, 37
Proponents of CBPR describe it as a research approach that depends on equitable partnership involving the sharing of expertise, responsibilities, and ownership of the research process between academic research partners and their non-academic community partners in order to enhance the understanding of a given phenomenon; in global health research, it may be to address an identified health problem(s).31, 32, 33, 34, 35, 36, 37 This partnership allows earlier integration of knowledge gained with action to improve the health and well-being of a community.31, 32, 33, 34, 35, 36, 37 CBPR may involve partnerships between individual researchers or institutions and vulnerable communities inside HIC or in LMIC.31, 32, 33, 34, 35, 36, 37 It is important to make a distinction between CBPR and “community-placed research,” since the latter is researcher-driven with little involvement of the community people.31, 32, 33, 34, 35, 36, 37
Several advantages of CBPR have been identified, including greater relevance and value to all parties concerned, shared responsibilities, and expertise to solve complex community-specific problems.34 This process improves the quality and validity of the research by engaging local knowledge and theory based on the experience of the people involved.34 It also breaks down existing distrust of community members toward academic institutions, researchers, and research because of their experience.34 Through the CBPR approach, the health and well-being of communities are improved – directly by examining and addressing identified needs and indirectly through increasing power and control over the research process.31, 32, 33, 34, 35, 36, 37
Weiner and McDonald have described three of the different CBPR models/approaches available.36 These include the single-theme model collaboration between a university-based center and a community organization. An example is the environmental protection work being undertaken by the University of Pennsylvania through its Center for Excellence in Environmental Toxicology (CEET) in partnership with the Chester Environmental Partnership (CEP).36 The second CBPR model is described as the targeted, area-based collaboration between academic researchers and a small group of community organizations.36 A good example is the Triumphant Living Collaborative (TCL)-a partnership between the University of Pennsylvania Center for Community-Based Research and Health Disparities (CCRDHD) and community organizations to identify community health problems and implement interventions to promote community health.36 The third CBPR model described consists of a broad-based coalition of two or more academic institutions with multiple stakeholder organizations in a given geographical area working on a long-term basis and on on-going multiple projects towards improving the health status of the target communities.36 An example given in the literature is the Philadelphia Area Research Community Coalition (PARCC) consisting of 22 organizations and three academic institutions.36
Across all three CBPR models, the authors have found that a successful partnership/collaboration is one that leaves something of value in the community even after the grant funding has ceased, stressing the importance of community sustainability.36 Secondly, although the ideal CBPR stresses the importance of the active participation of all parties in all aspects of the research activity, studies have shown that the community's priority is not to become research experts but to create sustainable programs to improve the community's health and well-being.36 Hence, community members at the barest minimum, need to be involved in selecting the research focus/topic, advising on and interpreting results, and in community dissemination of the research findings.36 The greatest barriers to CBPR identified by the community were lack of trust and a history of racism and classism, whereas time constraints and lack of infrastructure were the most important from the perspective of academic partners.36
Adams et al. have also reported the work of the Great Lakes Native American Research Center for Health; this is a National Institutes of Health (NIH)/Indian Health Service-funded collaboration between the University of Wisconsin, the Mayo Clinic, and community leaders including the Great Lakes Inter-Tribal Council and others; the goal is to address Native American community health problems such as child obesity, cancers, and reproductive health-associated issues.37 Promoting trust and building capacity within the community by facilitating the training of community members in the health professions have also been an important component of the efforts at building long-term community sustainability and reduce health disparities.37
Conclusion
The Sustainable Development Goals (SDGs) provide the framework for global sustainable environmental, social, and economic growth, while seeking to protect the planet for future generations. While SDG3 focuses directly on promoting, improving, and sustaining health globally, the other SDGs do the same albeit indirectly. SDG17 is important in calling for global partnerships to facilitate the achievement of the other 16 goals including SDG3.
This paper has provided an overview of the SDGs, explored the power differences at play between potential research partners from HIC and LMIC, examined the social determinants for health and global disease burdens of LMIC, discussed global health research partnerships, and attempted to make a case for community-based participatory research (CBPR) as a viable option for global health research partnerships in the context of the SDGs.
Acknowledgement
Fig. 1 is used with permission from the following open access article:
Larkan F, Uduma O, Lawal SA, van Bavel B. Developing a framework for successful research partnerships in global health. Globalization and Health, 2016; 12:17 DOI 10.1186/s12992-016-0152-1.
Published by Springer Nature, 1 New York Plaza, Suite 4600, New York, NY 10004, U.S.A.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sapharm.2020.08.015.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.World Health Organization WHO coronavirus disease (COVID-19) dashboard. https://covid19.who.int/
- 2.World Health Organization Global leaders unite to ensure everyone everywhere can access new vaccines, tests and treatments for COVID-19. 2020. https://www.who.int/news-room/detail/24-04-2020-global-leaders-unite-to-ensure-everyone-everywhere-can-access-new-vaccines-tests-and-treatments-for-covid-19
- 3.United Nations Development Programme (UNDP) Sustainable development goals. http://www.undp.org/content/undp/en/home/sustainable-development-goals.html
- 4.United Nations Sustainable development goals: about the sustainable development goals. https://www.un.org/sustainabledevelopment/sustainable-development-goals/
- 5.UNDP Sustainable development goals. Goal 3: good health and well-being. http://www.undp.org/content/undp/en/home/sustainable-development-goals/goal-3-good-health-and-well-being.html
- 6.Sustainable Development Report SDG index dashboard. 2018. https://www.sdgindex.org/reports/sdg-index-and-dashboards-2018/
- 7.World Health Organization 10 facts on health inequities and their causes. https://www.who.int/features/factfiles/health_inequities/en/
- 8.Stevens P. Diseases of poverty and the 10/90 gap. https://www.who.int/intellectualproperty/submissions/InternationalPolicyNetwork.pdf
- 9.United Nations Statistics Division Millennium development goals indicators. http://mdgs.un.org/unsd/mdg/Default.aspx
- 10.United Nations The Millennium development goals report. 2015. http://www.undp.org/content/dam/undp/library/MDG/english/UNDP_MDG_Report_2015.pdf
- 11.United Nations Millennium development goals and beyond 2015. https://www.un.org/millenniumgoals/
- 12.Cash-Gibson L., Rojas-Gualdrón D., Pericàs J.M., Benach J. Inequalities in global health inequalities research: a 50-year bibliometric analysis. PloS One. 1966-2015;13(1) doi: 10.1371/journal.pone.0191901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.UNDP Sustainable development goals. Goal 17: partnerships for the goals. https://www.undp.org/content/undp/en/home/sustainable-development-goals/goal-17-partnerships-for-the-goals.html
- 14.Ramsey S. No closure in sight for the 10/90 health research gap. Lancet. 2001;358:1348. doi: 10.1016/S0140-6736(01)06465-0. [DOI] [PubMed] [Google Scholar]
- 15.Doyal L. Gender and the 10/90 gap in health research. Bull World Health Organ. 2004;82:3. Genebra March 2004. [PMC free article] [PubMed] [Google Scholar]
- 16.Smith E., Hunt M., Master Z. Authorship ethics in global health research partnerships between researchers from low or middle income countries and high income countries. BMC Med Ethics. 2014;15:42. doi: 10.1186/1472-6939-15-42. http://www.biomedcentral.com/1472-6939/15/42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO Commission on Social Determinants of Health Social determinants of health, final report: executive summary. http://whqlibdoc.who.int/hq/2008/WHO_IER_CSDH_08.1_eng.pdf
- 18.Marmot M. Social determinants of health inequities. Lancet. 2005;365:1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization HIV/AIDS: facts sheet. https://www.who.int/news-room/fact-sheets/detail/hiv-aids
- 20.World Health Organization Tuberculosis: facts sheet. https://www.who.int/health-topics/tuberculosis#tab=tab_1
- 21.World Health Organization Malaria: facts sheet. https://www.who.int/malaria/en/
- 22.World Health Organization Noncommunicable diseases: facts sheet. https://www.who.int/health-topics/noncommunicable-diseases#tab=tab_1
- 23.World Health Organization The world health report 2008-primary health care (now more than ever) https://www.who.int/whr/2008/en/
- 24.Sixty-third World Health Assembly Policy on WHO engagement with global health partnerships and hosting arrangements. 2010. https://www.who.int/docs/default-source/documents/partnerships/partnerships-63rd-wha-agenda-item-18-1-21-may-2010.pdf?sfvrsn=a9b06d88_2
- 25.World Health Organization WHO Director-General https://www.who.int/dg
- 26.Binka F. North-South research collaboration: a move towards a true partnership? Trop Med Int Health. 2005;10(5):207–209. doi: 10.1111/j.1365-3156.2004.01373.x. [DOI] [PubMed] [Google Scholar]
- 27.Edejer T. North-south research partnerships: the ethics of carrying out research in developing countries. BMJ. 1999;319:438–441. doi: 10.1136/bmj.319.7207.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gallard J.F. North-south research partnership: is collaboration possible between unequal partners? Knowl Pol. 1994;7:2. [Google Scholar]
- 29.Wollfers I., Adjei S., van der Drift R. Health research in the tropics. Lancet. 1995;351:1652–1654. doi: 10.1016/S0140-6736(97)10237-9. 1995. [DOI] [PubMed] [Google Scholar]
- 30.Larkan F., Uduma O., Lawal S.A., van Bavel B. Developing a framework for successful research partnerships in global health. Glob Health. 2016;12:17. doi: 10.1186/s12992-016-0152-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wallwork E. Ethical analysis of research partnerships with communities. Kennedy Inst Ethics J. 2008;18(1):57–85. doi: 10.1353/ken.0.0000. (Article) [DOI] [PubMed] [Google Scholar]
- 32.Israel B.A., Eng E., Schulz J., Parker E.A. second ed. Jossey Bass, A Wiley Imprint; San Francisco, CA: 2013. Methods for Community-Based Participatory Research for Health. [Google Scholar]
- 33.US Department of Health and Human Services Community-based participatory research (CBPR) https://www.nimhd.nih.gov/programs/extramural/community-based-participatory.html
- 34.The Detroit Community-Academic Urban Research Center Community-based participatory research principles. https://www.detroiturc.org/cbpr-principles.html
- 35.School of Public Health U.C. Berkeley. Community-based participatory research: a strategy for building healthy communities and promoting health through policy change. https://www.policylink.org/sites/default/files/CBPR.pdf
- 36.Weiner J., McDonald J.A. Three models of community-based participatory research. Leonard Davis Institute (LDI) Issue Brief. 2013;18(5):1–8. [PubMed] [Google Scholar]
- 37.Adams A., Miller-Korth N., Brown D. Learning to work together: developing academic and community research partnerships. Wis Med J. 2004;103(2):15–19. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.