Dear Editor:
Healthcare workers (HCWs) in the emergency departments (EDs) are at high risk to contract COVID-19. There is consensus in the medical community that universal masking reduces infection rates of HCWs [[1], [2], [3]]. N-95 respirator masks or surgical masks, eye protection, and physical distancing of >1 m or more have all been shown to decrease transmission of SARS-CoV-2 and the related coronaviruses SARS-CoV-1 (SARS) and Middle East respiratory syndrome (MERS) [1]. There has only been one report thus far adding eye protection to universal masking, with no transmission to HCWs who added face shields in India during home visits [4]. The goal of our study was to determine if frontline emergency clinicians contracted COVID-19 at a rate different from that predicted by community spread when implementing mandatory eye protection (in addition to masks).
We conducted a retrospective multicenter study in 14 EDs across a large Midwest integrated healthcare system with >500,000 ED visits annually to assess the effectiveness of mandatory eye protection (goggles) by 352 frontline emergency clinicians (defined as physicians and physician assistants) in conjunction with universal masking. The study was performed as a quality improvement project.
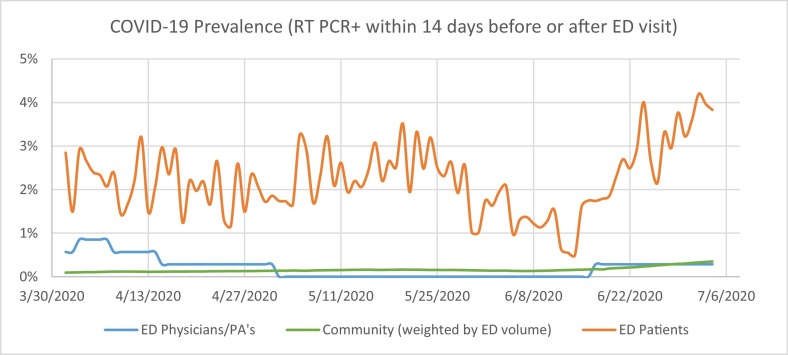
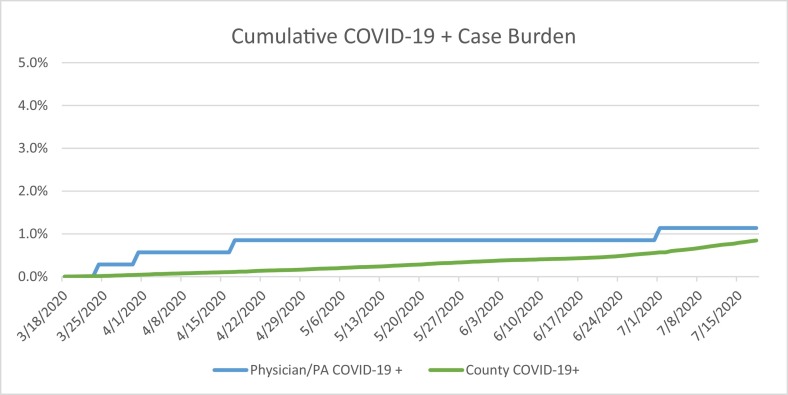
Data was retrieved for a 4-month period, (March 18 to July 18, 2020). Beginning on March 18, goggles purchased by the institution were required to be worn by all frontline emergency clinicians during ED clinical shifts. Additionally, a universal masking policy of all HCWs and all ED patients arriving to the ED was put in place. ED patient COVID-19 prevalence rate was calculated from total daily ED encounters, as defined as the proportion of patients during the study period who tested RT-PCR COVID-19 + within the preceding or trailing 14 days. Frontline emergency clinician prevalence was calculated by tracking the proportion of all clinicians who had tested RT-PCR COVID-19 + within the same period. State databases allowed for calculation of RT-PCR + COVID-19 cases by county across the state. For each county, a prevalence figure was obtained by including those who tested RT-PCR COVID-19 + within the same period and dividing by the county population. County prevalence values were weighted by our annual ED volumes to obtain the community prevalence of COVID-19. More than 80% of healthcare system ED volume is in one county, and we used that county to compare COVID-19 + cumulative case burden between our frontline ED clinicians and community. Significance was calculated using pooled two-proportion Z-test.
Fig. 1 depicts the prevalence of COVID-19 over time in ED patients, frontline ED clinicians, and the community. Fig. 2 shows the cumulative percentage of frontline ED clinicians and representative county residents who tested COVID-19 + over time. During the 4-month study period, 1.14% (4/352) frontline ED clinicians contracted COVID-19, as compared to 0.85% residents of the county with 80% of our healthcare system's collective ED annual volume. When using a two-proportion Z-test, pooled, there was not a significant difference in the populations (p = 0.55).
Fig. 1.
COVID-19 prevalence in emergency departments across the healthcare system.
Fig. 2.
COVID-19 + cumulative case burden in ED frontline clinicians and Main ED.
COVID-19 infection occurred among our frontline ED clinicians at a rate more comparable to community spread than to the prevalence in our ED patient population. Adding eye protection to universal masking appears effective in curbing HCW acquisition of COVID-19. This is the first study examining frontline ED clinicians to determine the effects of eye protection in conjunction with universal masking. These findings parallel known data from SARS and MERS, in which goggle use was associated with a 0.34 (0.22–0.52) relative risk of transmission [1].
Eye protection, in addition to universal masking, was effective in the prevention of COVID-19 transmission. Frontline ED clinicians should consider wearing eye protection at all times in clinical settings. Further studies should examine the addition of eye protection in larger cohorts, and potentially examine the potential benefits of wearing eye protection in the community. Our study can reassure frontline workers in the ED of the safety of universal masking and eye protection to prevent transmission of COVID-19 among HCWs.
References
- 1.Chu D.K., Akl E.A., Duda S., et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang X., Ferro E.G., Zhou G., Hashimoto D., Bhatt D.L. Association between universal masking in a health care system and SARS-CoV-2 positivity among health care workers [published online ahead of print, 2020 Jul 14] JAMA. 2020 doi: 10.1001/jama.2020.12897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study [published online ahead of print, 2020 Jul 31]. Lancet Public Health. https://www.thelancet.com/pdfs/journals/lanpub/PIIS2468-2667(20)30164-X.pdf [DOI] [PMC free article] [PubMed]
- 4.Bhaskar ME, Arun S. SARS-CoV-2 infection among community health workers in India before and after use of face shields [published online ahead of print, 2020 Aug 17]. JAMA. 2020; 10.1001/jama.2020.15586. doi: 10.1001/jama.2020.15586 [DOI] [PMC free article] [PubMed]