Abstract
A 75-year-old man was admitted to our hospital for treatment of esophageal cancer (EC) in March 2017. Esophagogastroduodenoscopy revealed Barrett’s esophagus and superficial, distal EC (type 0-IIc). Tumor biopsy showed esophageal adenocarcinoma. Computed tomography revealed no lymph node metastasis but did reveal a 19-mm tumor on the right side of the urinary bladder. Bladder cancer (BC) was also suspected, and the patient underwent endoscopic submucosal dissection for EC and transurethral resection of the bladder tumor. The pathological diagnosis of EC was moderately to poorly differentiated adenocarcinoma (tub2), pT1b (SM), ly0, v0. The pathological horizontal margin was negative and the vertical margin was positive. Additional esophagectomy and lymph node dissection were indicated for curability. Esophagectomy was difficult because the patient had severe cardiovascular disease, so follow-up observation was adopted. BC was classified as urothelial carcinoma Ta, ly0, v0. After 32 months, multiple tumors were found in the bladder, and BC recurrence was suspected. Transurethral resection of the bladder was performed again for seven tumors, and pathological diagnosis was poorly differentiated adenocarcinoma (tub2). The immunohistochemical features matched those of EC. We diagnosed EC metastasis in the urinary bladder. Bladder adenocarcinoma is difficult to distinguish from metastasis from other organs, especially the upper gastrointestinal tract, and cytomorphological features and appropriate clinical history are required.
Keywords: Esophageal cancer, Metastasis, Urinary bladder
Introduction
Esophageal cancer (EC) is a common but fatal malignancy [1, 2]. The high mortality is attributed to local invasion and distant spread, and metastasis usually occurs to lymph nodes, lungs, liver and bone [3, 4]. The urinary bladder is a rare site of metastasis, and, to our knowledge, this is the first report of urinary bladder metastasis from EC after treatment for primary urothelial carcinoma.
Case report
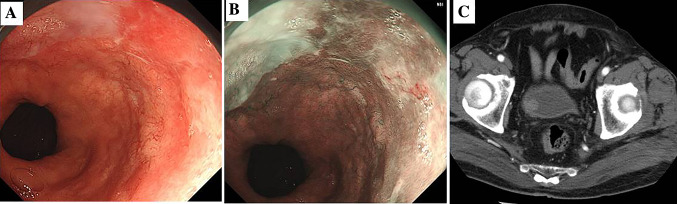
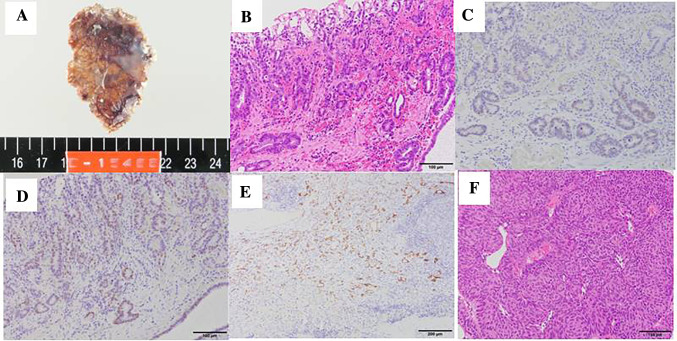
A 75-year-old man was admitted to our hospital for treatment of EC in March 2017. Esophagogastroduodenoscopy revealed Barrett’s esophagus and superficial, distal EC (type 0-IIc + IIa) (Fig. 1a, b). Tumor biopsy showed esophageal adenocarcinoma. Computed tomography (CT) revealed no lymph node metastasis but did reveal a 19-mm tumor on the right side of the urinary bladder (Fig. 1c). Bladder cancer (BC) was also suspected. First, he underwent transurethral resection of the bladder tumor (TURBT) that was diagnosed as urothelial carcinoma Ta, ly0, v0 (Fig. 2f). After 1 month, he underwent endoscopic submucosal dissection for EC. The pathological diagnosis of EC was moderately to poorly differentiated adenocarcinoma (tub2), pT1b (SM), ly0, v0. The pathological horizonal margin was negative and the vertical margin was positive (Fig. 2a). Additional esophagectomy and lymph node dissection were indicated for curability. However, this treatment was difficult because he had severe cardiovascular disease, so follow-up observation was adopted. After surgery, CT scan was performed every 3 months and gastrointestinal endoscopy every 5 months to check for recurrence. Cystoscopy was also performed every 4 months. Thirty-two months after TURBT, multiple tumors were observed in the bladder and BC recurrence was suspected. TURBT was performed again for seven tumors and pathological diagnosis was poorly differentiated adenocarcinoma (por2) (Fig. 3a). The immunohistochemical (IHC) features matched those of EC (CK7+, CK20−, CDX2+, MUC5AC+, p53 mutation+) (Figs. 2c–e, 3b–d). Esophagogastroduodenoscopy revealed no tumor regrowth in the esophagus, and plane CT showed no metastases. However, positron emission tomography revealed multiple bone metastases. We diagnosed EC metastasis and the patient was started on first-line chemotherapy with S-1 plus oxaliplatin.
Fig. 1.
a Endoscopic imaging revealed distal esophageal carcinoma (type 0-IIc). b Esophageal carcinoma was revealed by narrow band imaging. c Computed tomography showed the tumor on the right side of the bladder
Fig. 2.
a Endoscopic submucosal dissection specimen. b Hematoxylin and eosin (HE) staining. Moderately to poorly differentiated adenocarcinoma (tub2), pT1b (SM), ly0, v0. Pathological horizontal margin was negative and vertical margin was positive. The bottom of the specimen contained poorly differentiated adenocarcinoma. c Positive stain for CDX-2. d Positive stain for MUC5AC. e Positive stain for p53 mutation. f HE staining of transurethral resection of the bladder specimen. Urothelial carcinoma Ta, ly0, v0
Fig. 3.
a Hematoxylin and eosin staining of bladder tumor, which was poorly differentiated adenocarcinoma (por2). b Positive stain for CDX-2. c Positive stain for MUC5AC. d Positive stain for p53 mutation
Discussion
We have reported a case of esophageal adenocarcinoma with urinary bladder metastasis. EC can spread even at an early stage and 74.5% of patients have been reported to have lymph node metastasis during initial diagnosis [5]. The most common sites of metastases of EC are lymph nodes, lungs, liver, stomach, and bone [3, 4], but bladder metastasis is rare.
Differentiation of bladder metastasis of EC from primary bladder cancer is important because the prognosis of recurrent EC is poor compared with that of primary bladder adenocarcinoma [6]. However, distinction between primary bladder adenocarcinoma and metastatic adenocarcinoma from other organs is often difficult because of their histological similarity, especially in poorly differentiated cases [7].
In the present case, abrupt appearance of multiple bladder adenocarcinomas and bone metastases after R1 resection for esophageal adenocarcinoma suggested metastasis from EC, and the IHC status of the bladder tumor matched that of esophageal adenocarcinoma.
We searched PubMed for cases of esophageal adenocarcinoma with urinary bladder metastasis using the keyword “esophageal cancer urinary bladder.” This search yielded two detailed case reports (Table 1). Schuurman et al. [8] reported a 53-year-old man who was diagnosed with esophageal adenocarcinoma after presenting with difficulty swallowing. Metastatic workup showed no obvious distant metastasis, but a thickened dorsal bladder wall was noted and biopsy showed esophageal adenocarcinoma. Heather et al. [9] reported a 49-year-old woman who presented with vomiting, and workup revealed advanced esophageal adenocarcinoma with liver metastases. She completed six cycles of cisplatin, 5-fluorouracil, and trastuzumab; however, she had hematuria. Cystoscopy revealed that the patient had undergone TURBT. Pathology was compared with the previous biopsy of liver and was thought to be morphologically similar.
Table 1.
Previous reports of esophagus carcinoma with bladder metastasis including our case
| Author | Our case | Heather et al. [9] | Schuurman et al. [8] |
|---|---|---|---|
| Year | 2020 | 2017 | 2009 |
| Age | 78 | 49 | 52 |
| Sex | Male | Male | Male |
| Location | Ae | Ae | Ae |
| cStage (first visit) | T1bN0M0 Stage I | T3N4M1 Stage IVb | T3N0M1 Stage IVb |
| Pathological findings | Adenocarcinoma | Adenocarcinoma | Adenocarcinoma |
| IHC status of esophagus | CK7+, CK20−, CDX2+, MUC5AC+, p53+ | CK7+, CK20+, CDX2+ | CK7+, CK20+, CDX2+ |
| IHC status of bladder | CK7+, CK20−, CDX2+, MUC5AC+, p53+ | CK7+, CK20+, CDX2+ | CK7+, CK20+, CDX2+ |
The above two cases [8, 9] were diagnosed by IHC staining (Table 1). Immunohistochemistry can be of value in reaching a final diagnosis, although its efficacy is sometimes limited. Torenbeek et al. [7] noted 93% overall correct classification of bladder adenocarcinoma from the prostate using prostate-specific antigen, and 91% correct classification of endometrial cancer using vimentin. However, adenocarcinomas from esophagus have no specific IHC features. Previous authors have emphasized CDX-2 [8, 9], a homeobox gene that is sensitive and specific for gastrointestinal tumors. CDX-2 was also positive in our case but Werlling et al. [10] reported that patients with bladder adenocarcinoma can be positive for CDX-2. In fact, criteria have not been established for confident distinction between bladder metastasis from esophageal adenocarcinoma and primary bladder adenocarcinoma. We performed immunohistochemistry for MUC5AC and p53 mutation as an aid. They were both positive in primary esophageal adenocarcinoma and bladder adenocarcinoma. This matching of IHC status was helpful for diagnosis; however, we thought that either status alone was not sufficiently specific for proof of metastasis. Bardales et al. [11] stated that cytomorphological features and appropriate clinical history are required for distinction. In this case, we diagnosed metastasis from EC on the basis of IHC status as well as clinical history. The abrupt appearance of multiple bladder adenocarcinomas and bone metastases after R1 resection for esophageal adenocarcinoma in short terms (4 months) made it difficult to diagnose primary bladder adenocarcinoma. Moreover, the resection stump of the endoscopic submucosal resection specimen contained poorly differentiated adenocarcinoma, and it seemed to match with similar tumor in the bladder.
Conclusion
We presented a case of multiple urinary bladder metastases from EC after treatment for primary urothelial carcinoma diagnosed by cytomorphological features in association with appropriate clinical history. Bladder adenocarcinoma is difficult to distinguish from metastasis from other organs, especially the upper gastrointestinal tract. Further follow-up and study is required.
Author contributions
Study conception: YK. Data collection: YM, YK, ST. Writing: ST. Critical review and revision: YK, EO. Final approval of the article: All Authors. Accountability for all aspects of the work: All Authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Napier K, Scheerer M, Misra S. Esophagus cancer: a review of epidemiology, pathologenesis, staging work up and treatment modalities. World Gastrointest Oncol. 2014;6(5):112–120. doi: 10.4251/wjgo.v6.i5.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pohl H, Sirovich B, Welch HG. Are we reaching the peak? Cancer Epidemiol Biomark Prev. 2010;19(6):1468–1470. doi: 10.1158/1055-9965.EPI-10-0012. [DOI] [PubMed] [Google Scholar]
- 3.Maller J, Karki N, Sapkota B, Niazi M, Remy P. Rare presentation of gastroesophageal carcinoma with rectal metastasis; a case report. Am J Case Rep. 2016;17:611–615. doi: 10.12659/AJCR.898534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Velcheti V, Govindan R. Metastatic cancer involving bladder; a review. Can J Urol. 2007;14(1):3443–3448. [PubMed] [Google Scholar]
- 5.Mandard AM, Chasle J, Marnay J. Autopsy findings in 111 cases of esophageal cancer. Cancer. 1981;48:329–335. doi: 10.1002/1097-0142(19810715)48:2<329::AID-CNCR2820480219>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 6.Raitane MP, et al. Diagnostic and therapeutic aspects of adenocarcinoma of urinary bladder. Ann Chir Gynaecol. 1993;206:20–27. [PubMed] [Google Scholar]
- 7.Torenbeek R, et al. Value of a panel of antibodies to identify the primary origin of adenocarcinomas presenting as bladder carcinoma. Histopathology. 1998;32:20–27. doi: 10.1046/j.1365-2559.1998.00328.x. [DOI] [PubMed] [Google Scholar]
- 8.Schuurman JP, et al. Urinary bladder metastasis from an esophageal adenocarcinoma: a case report. Am J Gastroenterol. 2009;104(6):1603–1604. doi: 10.1038/ajg.2009.113. [DOI] [PubMed] [Google Scholar]
- 9.Heather K, Rahoma E, Krista D, Toni P. A rare case of esophageal adenocarcinoma with urinary bladder metastasis. Case Rep Gastrointest Med. 2017 doi: 10.1155/2017/9343896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Werling RW, et al. CDX2, a highly sensitive and specific marker of adenocarcinomas of intestinal origin: an immunohistochemical survey of 476 primary and metastatic carcinomas. Am J Surg Pathol. 2003;27(3):303–310. doi: 10.1097/00000478-200303000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Bardales RH, et al. Urine cytology of primary and secondary urinary bladder adenocarcinoma. Cancer. 1998;84(6):335–343. doi: 10.1002/(SICI)1097-0142(19981225)84:6<335::AID-CNCR4>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]