ABSTRACT
Irritation fibroma is a benign, exophytic reactive oral lesion that develops secondary to injury. Its recurrence rate is rare but may happen in case of repeated trauma at the same site. This case report describes a recurrent fibroma in the anterior region of the hard palate in a 13-year-old male patient, which recurred in less than 1 year of surgical excision of the previous lesion. Through a detailed case history and clinical examination, the etiological factor of the same was found to be trauma from occlusion by the lower incisors. A multidisciplinary treatment approach was, therefore, undertaken, which included surgical excision of the lesion and correction of the underlying deep bite to prevent recurrence of the lesion. Thus, this article highlights the significance of a multidisciplinary approach for holistic dental treatment.
How to cite this article
Lalchandani CM, Tandon S, Rai TS, et al. Recurrent Irritation Fibroma—“What Lies Beneath”: A Multidisciplinary Treatment Approach. Int J Clin Pediatr Dent 2020;13(3):306–309.
Keywords: Holistic treatment, Irritational fibroma, Multidisciplinary approach, Recurrent fibroma
INTRODUCTION
Fibroma, a benign neoplasm of fibroblastic origin, represents a reactive hyperplasia of fibrous connective tissue in response to local irritation or trauma.1 These traumatic irritants could range from calculi and foreign bodies to iatrogenic factors like overhanging margins, restorations, etc.
Traumatic fibromas are frequently observed outgrowths in the oral cavity and comprise 4.5% of all oral mucosal lesions.2
The most common clinical aspect is the growth of a well-limited smooth-surfaced tissue, usually of a normal colored mucosa, having a sessile or pedunculated base, hard consistency, and smaller than 1.5 cm at its highest diameter.3 It is usually characterized by a slow, painless growth accumulated over a period of months or years.4
Treatment of fibromas traditionally involves complete surgical excision of the lesion. While the recurrence of traumatic fibromas is rare, it may occur if the irritant or the etiological factor has not been removed.3
In the present case report, recurrence of a traumatic fibroma on the anterior palatal region was suspected to be due to failure of addressing the irritant in the previous treatment procedure of the lesion. Therefore, this article accentuates the necessity of a multidisciplinary treatment plan to prevent recurrence and ensure successful and thorough dental care.
CASE DESCRIPTION
A 13-year-old male patient reported to the Department of Pediatric and Preventive Dentistry with a chief complaint of an uncomfortable growth inside his mouth. He described it to be a slow-growing mass on the anterior palatal region that appeared roughly 1 month ago. It was painless but created an obstruction during mastication and speech.
Dental history revealed that the patient underwent prior surgery for excision of the same lesion less than a year ago.
On intraoral examination, a large, smooth-surfaced, and pedunculated growth was observed in the incisive papillary region of the hard palate, just behind the central incisors. It was about 1.5 × 1 cm in size, soft, nontender, and attached to the palatal mucosa with a stalk (Fig. 1).
Fig. 1.

Preoperative palatal view showing fibrous outgrowth at incisive papillary region
Further clinical examination revealed a deep bite of about 7.5 mm anteriorly, which was suspected to be the etiological factor for this fibrous outgrowth due to irritation from the lower anteriors on the incisive papillary region (Fig. 2). It was, thus, concluded that neglect toward this irritational factor in the previous surgical procedure could have been the reason for recurrence of the lesion in less than a year's time.
Fig. 2.

Preoperative frontal view showing deep bite of 7.5 mm
An occlusal radiograph was done to rule out the presence of calcifications.
After obtaining an informed consent, routine blood investigations were carried out before undertaking the patient for surgery.
Based on all the findings, the provisional diagnosis was made to be irritation fibroma on the hard palate due to trauma from occlusion from the mandibular incisors. Possible differential diagnoses included giant cell granuloma, pyogenic granuloma, neurofibroma, or a benign salivary gland tumor, which would further be investigated by the biopsy.
The treatment was thus planned to surgically excise the lesion completely followed by correction of the underlying deep bite to prevent further recurrence of the lesion.
Phase I therapy involved supragingival scaling and rinses with chlorhexidine mouthwash twice daily for 1 week.
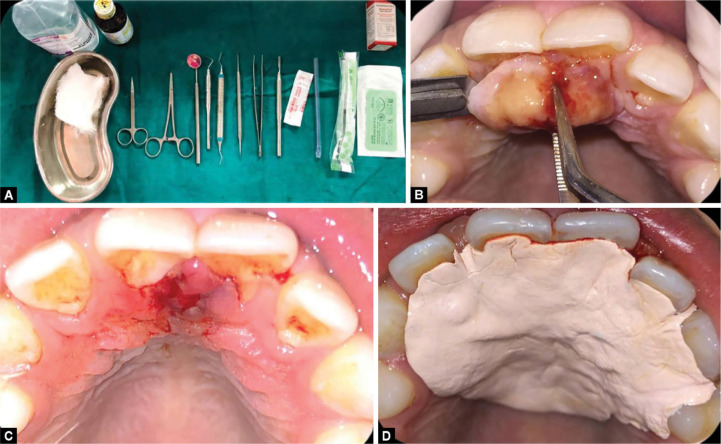
The surgical procedure was then carried out wherein the lesion was completely excised using a BP blade after administering local anesthesia. Bleeding from the region was controlled using a hemostat after which a Coe-Pak (GC America) dressing was given for a week's duration (Figs 3 and 4).
Figs 3A to D.
(A) Armamentarium for surgical excision of the lesion; (B) Surgical excision of the lesion; (C) Immediate postoperative image; (D) Postoperative Coe-Pak (GC America) dressing
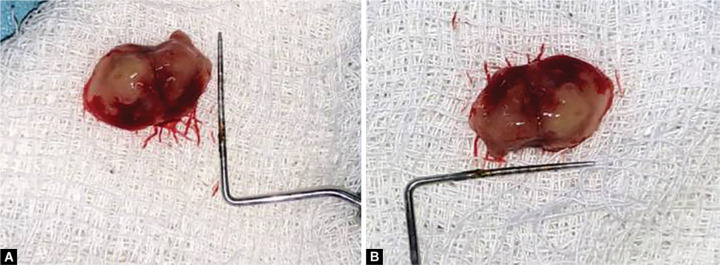
Figs 4A and B.
Dimensions of the lesion (1.5 × 1 cm)
The histopathological report of the excisional biopsy showed orthokeratinized stratified squamous epithelium with short rete pegs. The connective tissue stroma consisted of abundant collagen fiber bundles with proliferating fibroblasts, chronic inflammatory cells, and blood vessels, all of which were suggestive of a fibroma (Fig. 5).
Fig. 5.
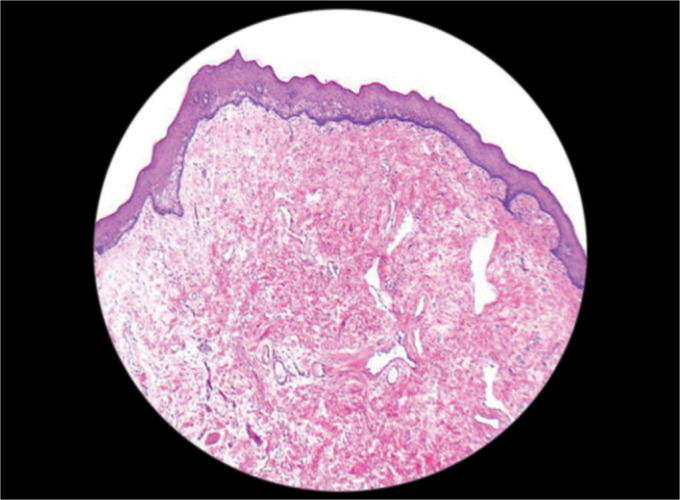
Histopathological section of the lesion
After an uneventful healing of the lesion, the deep bite was addressed. A removable anterior bite plane was given to relieve the bite anteriorly. The bite plane was designed to decrease the overbite by 2 mm, and was fabricated using acrylic. The patient was made to wear this appliance for a period of 3 months (Fig. 6).
Figs 6A and B.
(A) Frontal view with removable anterior bite plane; (B) Palatal view with removable anterior bite plane
After completion of the treatment, both healing at the lesion site and decrease in the overbite to 5.5 mm was observed (Figs 7 and 8).
Fig. 7.

Palatal view showing complete healing of the lesion
Fig. 8.

Frontal view showing reduction of overbite to 5.5 mm
The patient was followed up for 9 months since the treatment throughout which he displayed no signs of recurrence.
DISCUSSION
Localized fibrous tissue overgrowths are very common in the oral mucosa. The etiology of an irritational fibroma is usually a source of irritation. According to Barker and Lucas,1 irritational fibromas exhibit a pattern of collagen arrangement depending on the site of the lesion and the amount of irritation. There are two types of patterns: radiating pattern and circular pattern. Thus, they hypothesized that when there is a greater degree of trauma, the former appears in sites that are immobile in nature (e.g., palate), while less trauma induces the latter and it occurs in sites that are flexible in nature (e.g., cheeks).1 Similar such lesions, which may also arise as a result of irritation due to plaque microorganisms and other local irritants, include pyogenic granuloma, peripheral giant cell granuloma, and peripheral ossifying fibroma. All the lesions have a similar clinical appearance.5
The treatment of irritation fibroma consists of elimination of etiological factors, scaling of adjacent teeth, and total aggressive surgical excision to minimize the possibility of recurrence. Any identifiable irritant should be removed.6
Long-term postoperative follow-up is extremely important because of the high growth potential of incompletely removed lesion, which is 8–20%.7 Recurrences are rare and may be caused by repetitive trauma at the same site.8
In this case report, the recurrence of the pathology was attributed to two possible reasons: nonremoval of the irritant and/or incomplete surgical excision of the lesion. A thorough oral examination was essential to point out the previously unnoticed irritant/etiological factor, which was found to be trauma from occlusion on the palate from the lower incisors, owing to the presence of a deep bite. Thus, for complete treatment, a multidisciplinary approach was adopted.
After surgical excision of the lesion, orthodontic management of the deep bite was planned, to prevent further trauma from occlusion on the site of the lesion. Deep overbite can be corrected by many ways like intrusion of anteriors, extrusion of posteriors, combination of anterior intrusion and posterior extrusion, proclination of anteriors or surgically,9 depending on the requirements of the case and patient factors such as financial status, compliance, etc.
In this case, a removable appliance was found suitable to correct the deep bite. Thus, an anterior bite plane was planned to allow supraeruption of the molars, thereby relieving the bite anteriorly. Once the occlusion had stabilized, the treatment was complete, and the patient was followed up at regular intervals.
CONCLUSION
In conclusion, an etiology-directed dental treatment in this case proved to prevent the patient from bearing the brunt of sustained oral health issues and repeated avoidable procedures. Thus, a progress in treatment approach and planning toward holistic and multidisciplinary oral health care is of prime importance—not only while dealing with less commonly seen surgical lesions but also more routinely observed conditions such as dental caries and gingivitis.
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.Barker DS, Lucas RB. Localised fibrous overgrowths of the oral mucosa. Br J Oral Surg. 1967;5(2):86–92. doi: 10.1016/s0007-117x(67)80031-3. DOI: [DOI] [PubMed] [Google Scholar]
- 2.El Toum S, Cassia A, Bouchi N, et al. Prevalence and distribution of oral mucosal lesions by sex and age categories: a retrospective study of patients attending lebanese school of dentistry. Int J Dent. 2018;2018:4030134. doi: 10.1155/2018/4030134. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh N, Bilichodmath S, Sambhashivaiah S. Traumatic fibroma: a case series. J Health Sci Res. 2016;7(1):28–31. doi: 10.5005/jp-journals-10042-1030. DOI: [DOI] [Google Scholar]
- 4.Wood NK, Goaz PW. Differential Diagnosis of Oral and Maxillofacial Lesions. 5th ed., Missouri: Mosby; 2006. pp. 136–138. [Google Scholar]
- 5.Kolte AP, Kolte RA, Shrirao TS. Focal fibrous overgrowths: a case series and review of literature. Contemp Clin Dent. 2010;1(4):271–274. doi: 10.4103/0976-237X.76400. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jain G, Arora R, Sharma A, et al. Irritation fibroma: report of a case. J Curr Res Sci Med. 2017;3(2):118–121. doi: 10.4103/jcrsm.jcrsm_53_17. DOI: [DOI] [Google Scholar]
- 7.Eversole LR, Rovin S. Reactive lesions of the gingiva. J Oral Pathol. 1972;1(1):30–38. doi: 10.1111/j.1600-0714.1972.tb02120.x. DOI: [DOI] [PubMed] [Google Scholar]
- 8.Esmeili T, Lozada-Nur F, Epstein J. Common benign oral soft tissue masses. Dent Clin North Am. 2005;49(1):223–240. doi: 10.1016/j.cden.2004.07.001. DOI: [DOI] [PubMed] [Google Scholar]
- 9.Daokar S, Agrawal G. Deep bite its etiology, diagnosis and management: a review. J Orthod Endod. 2016;2(04):4. doi: 10.21767/2469-2980.100029. DOI: [DOI] [Google Scholar]