Abstract
The still escalating COVID-19 pandemic also has a substantial impact on energy structure, requirements and related emissions. The consumption is unavoidable and receives a lower priority in the critical situation. However, as the pandemic continues, the impacts on energy and environment should be assessed and possibly reduced. This study aims to provide an overview of invested energy sources and environmental footprints in fighting the COVID-19. The required energy and resources consumption of Personal Protection Equipment (PPE) and testing kits have been discussed. The protecting efficiency returned on environmental footprint invested for masks has been further explored. The main observation pinpointed is that with a proper design standard, material selection and user guideline, reusable PPE could be an effective option with lower energy consumption/environmental footprint. Additional escalated energy consumption for aseptic and disinfection has been assessed. This includes the energy stemming from emergency and later managed supply chains. The outcomes emphasised that diversifying solutions to achieve the needed objective is a vital strategy to improve the susceptibility and provide higher flexibility in minimising the environmental footprints. However, more comprehensive research proof for the alternative solution (e.g. reusable option) towards low energy consumption without compromise on the effectiveness should be offered and advocated.
Keywords: COVID-19 fighting measures, Energy consumption, Environmental footprints, PPE, Disinfection, Supply chains
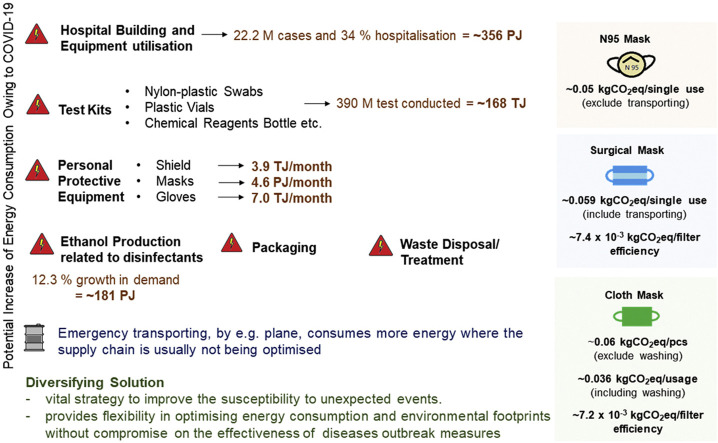
Graphical abstract
Highlights
-
•
COVID-19 pandemic impacts on energy structure, energy requirements and related emissions.
-
•
Overview of the invested energy sources and environmental footprints increased.
-
•
Required energy and resources consumption of Personal Protection Equipment (PPE) and testing kits.
-
•
An assessment of intensive energy consumption for aseptic and disinfection.
-
•
The outcomes emphasised that diversifying solutions are a vital strategy needed.
1. Introduction
The world population has been facing an unprecedented challenge, which has not been experienced from the time of Spanish flu [1] after the First World War. COVID-19, which was seen as another SARS epidemic at the beginning, escalated into worldwide pandemics. When this communication was finalised (19 August 2020), the number of infected was reaching 23 M [2] infected with no sign of halting. Table 1 summarises the different characteristics of epidemic and pandemic diseases. The information related to SARS-CoV-2 is still subjected to changes, including the reproduction number. The rapid spreading of this novel virus stresses the healthcare system and capacity, causing around 800 k lost lives [2] as the insufficient understanding of the mutating virus hinders the effective measures to be taken at the earliest instant. The sudden outbreak induces insufficient supply in term of manpower, raw materials/resources, production rate and disruption in supply chain/logistics to fulfil the surging demand. Flattening the curve [3] has been promoted to slow down the infection rate allowing healthcare services to have better management. A series of protective measures are introduced in the effort to suppress the outbreak. COVID-19 is expected to result in behaviour and structural changes, including the impacts on the economic, environmental and energy sustainability. The effect to the economic [4] is generally apparent; however, the impacts on the energy consumption and consequently, environmental footprint [5] are yet to be fully understood.
Table 1.
Comparison of the different epidemic and/or pandemic.
During the earlier stage of the crisis, lockdown or movement restriction at different stringency has been implemented. The implementation has been directly contributed to the cleaner environment due to the temporary limitation in mobility and the reduction of industrial activities. For example, Le Quéré et al. [12] shows the reduction in daily global CO2 emission. Kanniah et al. [13] reported the reduction of PM, NOx, SO2 and CO in Malaysia. Cleaner sky and cleaner river have also been the headline of different news outlets. Similar positive results to the air pollution are observed in Brazil [14], India [15], Italy [16] and China [17] but with an increased in O3 due to the reduction in NOx. Adams [18], however, suggested that there is a reduction in O3 and NOX during the state of emergency in Ontario, Canada. Almond et al. [19] stated that a relative deterioration in air quality near the epicentre of pandemic (Hubei) is observed, concluding that the impact on pollution is ambiguous. Wang et al. [20] highlighted that the emission reduction in transportation and a slight reduction in industrial would not help avoid severe air pollution, especially when meteorology is not favourable. This suggests the crucial role of energy sectors to the environment. The long-running impacts and the indirect impacts are still to be assessed for an overall picture of environmental sustainability.
The lockdown, which directly impacts the cleaner air, is just a temporary measure. Many countries have started to lift the restriction to support the growth of the economy as soon as considered acceptable. Gilingham et al. [21] stated that the implication of COVID-19 in the long term is deeply uncertain and could be outweighed the short term “silver lining” environmental benefit. During the peak of the crisis, the environmental considerations were understandably side-lined. However, as the pandemics seem to be around for some time yet, the humankind should be fully aware that the environment needs to be kept hand in hand in this long-running battle. The presented study aims to provide an overview of the extra energy consumption that potentially increases the environmental footprint during the COVID-19 crisis. The focus is given to the activities to support the healthcare system, including the hospital consumptions to the public. One of the essential and frequently used PPE, masks, is assessed where the filter efficiency returned on environmental footprint invested is discussed. Although environmental protection could not be the priority in the most critical moment, it is still important to recognise the problem. The additional production (e.g. PPE, test kits, disinfectants) and resultant waste to be handled later as well as the supply chain/logistic issues should be alerted. The issues summarised in this study could serve as a starting point to discuss and optimise possible pathways/solutions with lower energy consumption and environmental impacts in facing a similar future crisis.
2. The energy and environmental footprints of healthcare systems, PPE usage and logistics
Healthcare systems have been under the most unprecedented pressure in the crisis of COVID-19. There had been a struggle in term of PPE and medical supply as well as the bed capacity. For example, Northern Italy, the European Union (EU) resourced health system, was reported to approach its breaking point, see McCarthy [22]. Hospital is regarded as one of the building sectors with high energy consumption, see Bawaneh et al. [23]. Healthcare sector was reported to be responsible for 4.4% of global net GHG emissions [24] and received considerable attention to shrink the carbon emissions even before the COVID-19 crisis. The high energy intensity is mainly contributed by the constant need for power supply, medical equipment usage, requirements for air quality (ventilation) and disease control. Several studies suggested that energy consumption is ranging from 8.9 to 17 MWh/bed, depending on the hospital size according to the annual consumption [25]. By considering the consumption by activities, it represents 0.20 MWh/hospitalisation stay, 1.60 MWh/surgery and 0.07 MWh/emergency action [25]. It is expected that the energy usage and environmental footprint (vast use of resources) of the hospital are increased in this period of time. The rate of hospitalisation and ICU admission were estimated to be 20.7–31.4%, and 4.9–11.5% of the reported cases [26]. By considering 34.25% (26.05% + 8.2%) of hospitalisation stay and 22.2 M reported cases globally, the rough estimation shows that the energy consumption is 99 TWh (22.2 M × 0.345 × 12.95 MWh/bed), equivalent to 356 PJ, still depending on the number of stays. The top emergency measures, such as building new temporary hospital buildings, have not been included; however, the construction needs considerable energy consumption and emissions released.
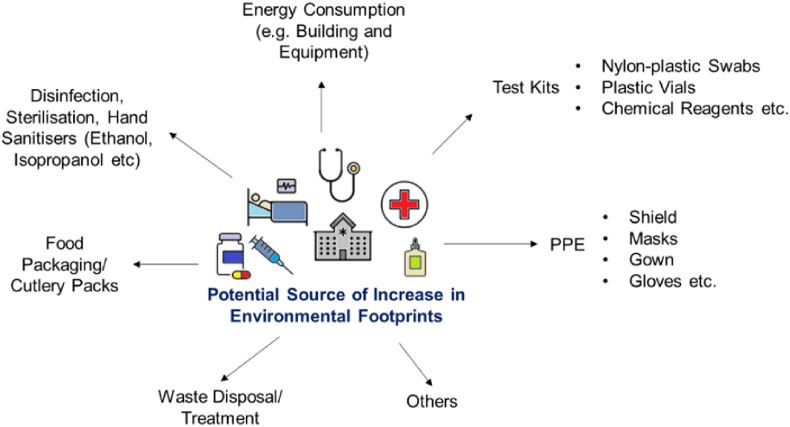
Fig. 1 summarises the potential increase in environmental footprints related to healthcare services. The increase of hospitalisation, working shift and hygiene requirement trigger the increase of energy, food packaging [27] and disinfectants demand. Due to the infectivity of SARS-CoV-2 causing COVID-19, massive testing is required (viral tests or antibody tests) to contain and understand the disease outbreak [28]. By extracting the countries data reported in Wordometer [2], the conducted tests are as high as 390 M (by 18 August 2020). The viral testing, either molecular test, e.g. RT-PCS or antigen tests [29] is with an embodied environmental footprint, including from intranational or international transporting. The global trade network and disruption of PPE supply chain have been discussed by the Asian Development Bank (ADB) [30]. It should be noted that the energy consumption and environmental footprint of transporting could be quite different depending on the situation. For example, in the normal scenario, ship (∼0.1–1.9 MJ/tkm [31]) is utilised. However, in the emergency situation, plane (∼8.2–26 MJ/tkm [31]) is a better option even the cost and emission are higher, with an average of 17.1 times increases in energy consumption. The utilisation of test kits is also associated with the consumption of resources, e.g. swabs, bottle/vials (plastic), chemical reagents, where proper waste treatment and disposal are required to minimise the environmental footprint. The estimated demand and energy consumption of PPE and test kits are summarised in Table 2 . The largest proportion of materials for the PPE are plastics [32]. A part of the energy can be recovered, and the footprint can be mitigated if being treated appropriately. This aftermath of COVID-19, in consumption and waste management, has been still developing and is yet to be evaluated and dealt with as it is not a direct impact which could be quantified in a short run.
Fig. 1.
The increase in the environmental footprints of healthcare during the COVID-19 pandemic.
Table 2.
The PPE Demand and The Energy Consumption (estimated amounts are subject to fluctuations, mostly grows).
| PPE/Devices and Weight | Estimated Demand | Estimated Energy Consumption |
|---|---|---|
Mask 12–13 g/pcsa |
129 G/monthb | 1.29 TWh/month = ∼4.6 PJ/month (By considering the energy consumption for masks production is 0.000792–0.0342 kWh/pcsc, taking 0.01 kWh/pcs for the estimation). Refer to Section 3 for further discussion on emissions |
Gloves ∼7 g/paird |
65 G/monthb | 1.95 GWh/month = ∼7.02 TJ/month (by considering the energy consumption for gloves production is 3 × 10−5 kWh/pairg) |
Fast Test kit (without gloves) ∼14 g/testd |
390 Me (18 August 2020) | 168 TJ (By considering the energy consumption of plastics production is 30.82 MJ/kgf) |
Shield ∼81 g/pcsd |
1.59 M/monthb | 3.9 TJ/month (By considering the energy consumption of plastics production is 30.82 MJ/kgf) |
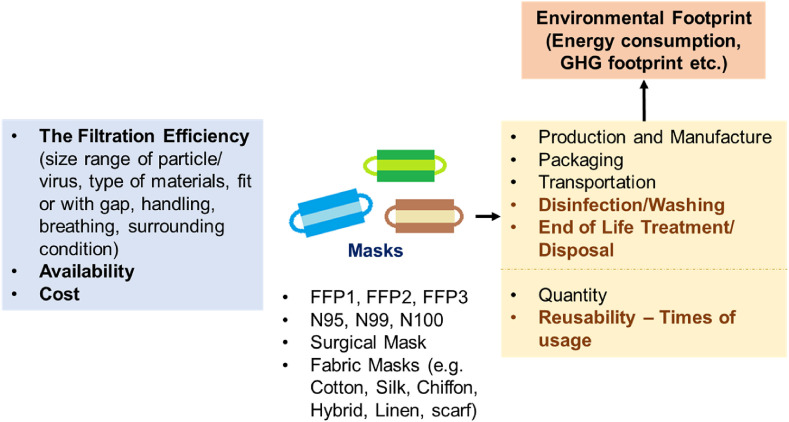
3. The filtration efficiency and environmental footprint of masks
Masks have been an essential PPE in this crisis. It is not privileged to use masks in hospital but common/mandatory in current daily mobility. There was a serious shortage in the supply where the demand cannot be fulfilled in a short time. This highlights the importance of diversifying to minimise dependency or threats. Fig. 2 summarises the selection criteria of masks and the source of environmental footprint. The approaches of washing or disinfection, times of usage and the end-of-life treatment could change the overall environmental footprint significantly. This aspect is discussed later based on Fig. 3 . The main selection criterion for a mask is the protection efficiency (i.e. filtration efficiency), which is usually reported by quantitative percentage numbers. However, a high percentage does not necessarily suggest high protection from infection where the assessed size for filtration efficiency and experimental settings needs to be referred. The penetrating particle size, which is usually applied in the certification test of a mask is 300 nm (SARS-CoV-2 < 300 nm, see Table 1).
Fig. 2.
The selection criteria of masks and the source of environmental footprint.
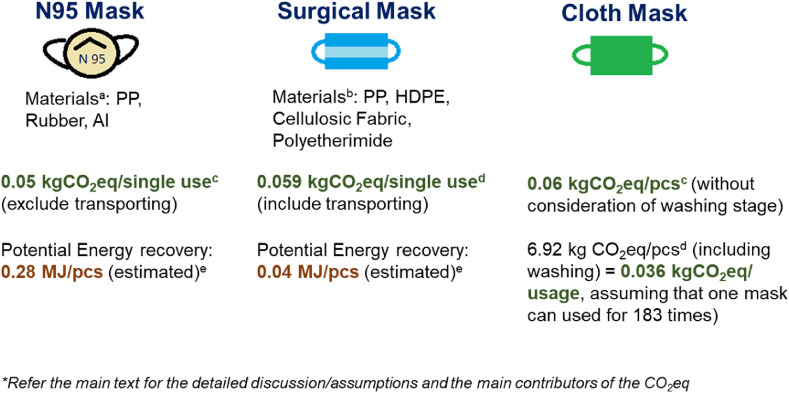
Fig. 3.
Comparison of environmental (GHG) footprint and potential energy recovery of different masks/respiratory. a [33], b [35], c [33], d [35], eCalculated based on the low heating value of plastic based on Klemeš et al. [36]. PP = polypropylene. Al = Aluminium. HDPE = High-density polyethylene.
Table 3 summarises the available results on the filtration efficiency of masks in different materials. In general, reusable masks have a lower filtration efficiency than N95 masks and surgical masks. However, it is not an absolute case where exceptional cases are observed (Table 3). This highlighted that cloth masks are competitive and have the potential to serve as an effective PPE. The type of cloth (e.g. hybrid material), fitting design and proper usage play the key role in promoting reliability. Cloth material with combined effects of electrostatic and physical filtering by layering can enhance the filtration efficiency [38]. There has different contradiction observation on top of the reported filtration efficiency summarised in Table 3. Smith et al. [39] summarised that there are insufficient data to conclusively suggest N95 masks are superior to surgical masks in the clinical setting, although the results for laboratory setting is positive. Lee et al. [40] suggested that filtering facepiece (FFP) respirators provide 11.5–15.9 times better protection than surgical masks. Long et al. [41] concluded that the use of N95 is not associated with a lower risk of laboratory-confirmed influenza compared to surgical masks. This highlights that more studies are needed to achieve a consensus regarding the efficiency of masks (including reusable mask, e.g. cloth) as well as improving the standard guideline for production and usage. Despite the initial confusing information on the use of masks in mitigating COVID-19, WHO has recently recommended the usage of three layers fabric masks for healthy people and provided the information on the filtration efficiency [42].
Table 3.
The filtration efficiency of masks in different materials.
| Konda et al. [38], <300 nm | Davies et al. [43], 23 nm |
Robertson [44] 20 - 1000 nm |
|
|---|---|---|---|
| N95 (No gap) | 85 ± 15 | – | 98.9 |
| N95 (with gap) | 34 ± 15 | – | – |
| Surgical mask (no gap) | 76 ± 22 | 89.52 ± 2.65 | 80–96.4 |
| Surgical mask (with a gap) | 50 ± 7 | – | – |
| Cotton (80 TPI), 1 layer | 9 ± 13 | – | – |
| Cotton (80 TPI), 2 layer | 38 ± 11 | – | – |
| Cotton (600 TPI), 1 layer | 79 ± 23 | 50.85 ± 16.81 (100% cotton T-shirt) | 50–69.4 |
| Silk | 54 ± 8 | 54.32 ± 29.49 | – |
| Scarf | – | 48.87 ± 19.77 | – |
| Hybrid (e.g. cotton/chiffon or cotton/silk) (no gap) | >90 | – | – |
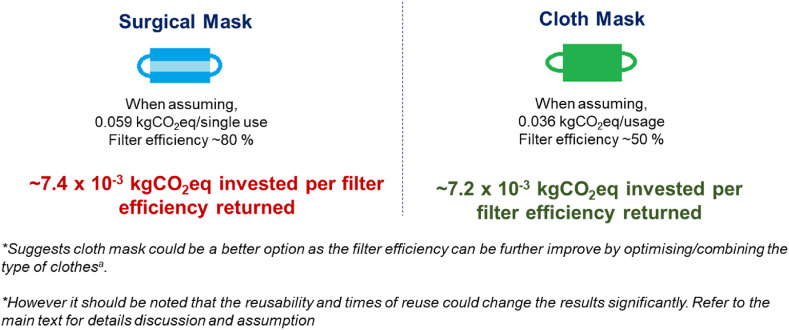
Fig. 3 illustrates the environmental performance related to different choices of masks. Without the consideration of transportation, the reported embodied GHG of N95 is 0.05 kg CO2eq/single-use [33], for which the main contributor is the Polypropylene (PP) materials. Allison et al. [35] reported that, based on an assessment in the UK, the high share of GHG emission embodied in surgical masks is from transportation. By considering the GHG emission of producing the masks, cloth masks have the highest emission at 0.06 kg CO2eq/pcs [33] or 6.92 kg CO2eq/pcs [35] when washing is considered. It shows the high share of GHG emission from the cleaning of masks. However, waste products can be reduced, and the emission can be lower by increasing the times of reuses. For example, the emission could reduce to 0.036 kgCO2eq if it was used 183 times. The filtering efficiency returned on GHG emission invested is proposed in this study as an index or indicator in evaluating the effectiveness and environmental footprint of masks in the future development (e.g. the advanced reusable masks). Based on the existing data, the cloth mask is suggested to have a reasonable index compared to the surgical mask (Fig. 4 ). The user phase assessment is challenging and needs further accounting as it is affected by behaviours, varying from person to person. For single disposal masks, proper waste treatment is required to minimise the impacts through energy recovery.
Fig. 4.
The filtering efficiency returned on GHG emission invested in surgical and cloth mask. The estimation is based on the information in Fig. 3 and Table 3.
4. The increased energy consumption of disinfection alternatives for public
During the COVID-19 pandemic, massive antiseptics and disinfectants are being produced, consumed, stockpiled and utilised for personal or public disinfection to prevent SARS-CoV-2 infection. On 13 February 2020 (near the peak of disease pandemic in China), the manufacturers of disinfection products in China produced antiseptics 205 t/d, disinfectants 4,597 t/d and medical-use ethanol 906 t/d [45]. The big e-commerce data showed that the sales of hand sanitiser spiked by 2,315% on the Suning e-commerce platform during the COVID-19 pandemic compared to the same period in 2019 [46]. Similar sale surge with more than 1,000% elevation was observed on the Taobao e-commerce platform in China [46]. In Japan, the Kao company increased the production of alcohol disinfectants by 2,000% in April 2020 to fight the shortage [47]. The increased demand and supply of antiseptics and disinfectants were also apparent in the EU and the USA. For example, in March 2020, sales of multipurpose cleaners in the USA spiked by 166% and aerosol disinfectants 343% from a year ago, which disrupted the supply chains of disinfectants [48]. Due to the disease pandemic, a total of 1,963.58 t of disinfectants were used in sewage systems in Wuhan, China from 29 January to 18 February 2020 [49]. The overuse of antiseptics and disinfectants with corrosive chemical compounds for the COVID-19 control could not only pose great threat to the urban environment [50] and ecosystems [51] but also lead to massive energy waste.
Energy consumption and environmental footprint are regarded as important criteria for disinfection technologies [52]. For effective disinfection of SARS-CoV-2, the conventional surface disinfectants were recommended to contain 62–71% ethanol or 0.1% sodium hypochlorite [53]. Compared to non-alcoholic products, alcoholic sanitisation products are chosen as a first-line measure for infection prevention due to their high efficacy and broader spectrum [54]. The usage of antiseptics and disinfectants during the COVID-19 pandemic increases energy and environment footprints significantly. Based on the currently available data, some rough estimations are presented for the extra energy consumption and environmental emissions related to the disinfectants used in 2020 due to the COVID-19 pandemic. On 18 June 2020, Technavio [55] estimated that the global surface disinfectants market would post a compound annual growth rate of 12.0% during 2020–2024. Such an estimation was based on a detailed analysis of the disinfection type of liquids, steam sprays and wipes over the EU, North America, Asia-Pacific, Middle East and South America. Due to the COVID-19 pandemic, Technavio [55] expected the impact to be apparent in the first quarter of 2020 but gradually lessen in the following quarters. China, the EU and North America are three regions having the largest share of the global market size. Table 4 shows the historical and estimated data of the disinfection industry in China [56]. The growth rate of the market size in China, i.e. 13.7%, as shown in Table 4, is basically in line with the global growth rate of 12.0%. If the growth rate of market size is used to approximate the overall growth rate of energy consumption and environmental emissions related to the disinfection industry in 2020, the range 12.0%–13.7% might be regarded as an experience-based estimation. However, it is worthy of being emphasised that such an estimated range might only be a lower bound considering the worse progress of global disease pandemic after June 2020. The ethanol production is the most concerning item for the estimation of extra energy demand and environmental emissions. The growth rate of medical-use ethanol in 2020 was 20.0%, as shown in Table 4. From 2015 to 2019, the average growth rate is calculated at 7.7%. By eliminating such an inertial growth trend, the extra growth rate of medical-use ethanol due to disease pandemic is estimated at 12.3%. In 2019, the global fuel ethanol production was 29,100 M gallons (∼110,155 × 106 L) [57]. That means the extra absolute volume of ethanol production in 2020 is 13,549 × 106 L. According to the energy content of ethanol, i.e. 18.4–21.2 MJ/L (mean = 19.8 MJ/L), the energy content in the extra ethanol demand in 2020 is 249.3–287.2 PJ (mean = 268.3 PJ). According to the well-to-pump estimation, the fossil fuel consumption was estimated as 0.51–0.84 MJ/MJ (mean = 0.675 MJ/MJ) of ethanol produced, and the GHG emissions were estimated as 39.44 - 49.97 gCO2eq/MJ (mean = 44.71 gCO2eq/MJ) of ethanol [58]. The extra energy used for ethanol production in 2020 is estimated as ∼181.1 PJ, and the extra GHG emissions in 2020 are estimated as ∼11,993.1 kt CO2eq.
Table 4.
Historical and estimated data of the disinfection industry in China [56].
| Year | Market size (/109 CNY) | Growth rate of market size | Antiseptics (kt) | Disinfectantsb (kt) | 75% medical-use ethanol (kt) | Growth rate of ethanol |
|---|---|---|---|---|---|---|
| 2015 | 85.9 | – | 31.4 | 358 | 52 | – |
| 2016 | 91.2 | 6.2% | 34.0 | 385 | 56 | 7.7% |
| 2017 | 96.2 | 5.5% | 36.9 | 417 | 60 | 7.1% |
| 2018 | 102.8 | 6.9% | 40.1 | 452 | 65 | 8.3% |
| 2019 | 103.4 | 0.6% | 43.7 | 493 | 70 | 7.7% |
| 2020a | 117.6 | 13.7% | 51.0 | 575 | 84 | 20.0% |
Notes.
The projection value in 2020.
Only the ‘84 disinfectant liquid’ was counted.
Besides liquid disinfection, some other disinfection technologies, including heat, radiation, steam and other emerging methods, can be used as the second-line measure for infection prevention. Heating at 85 °C and 30% relative humidity was found to be a useful technique for disinfection and reuse of N95 respirators [59]. Microwave sterilisation is essentially a type pf steam disinfection process. Compared to liquid disinfection, the steam spray was regarded as more environmentally friendly disinfection benefitting from a series of merits, e.g. without chemicals and their residuals, water-saving and wide coverage where manual cleaning is not possible. Table 5 shows the comparison of cost, water use and electricity use between the chemical method and the steam method. Except for the electricity use, the steam method has advantages on the other items. During disease pandemic, the steam can be used for the disinfection of partial medical waste that do not generate toxic volatile organic compounds [52], PPE like N95 masks [60] and public area [61], e.g. workplace, supermarkets and public transport.
Table 5.
Comparison in terms of cost, water use and electricity use between chemical method and steam method [64].
| Cost under classical chemical method (€/m2) | Cost under steam method (€/m2) | |
|---|---|---|
| Chemical products | 0.0009 | ∼0 |
| Gloves | 0.001 | 0.0004 |
| Laundry microfiber clothes | 0.027 | 0.01 |
| Water | 0.00012 | 0.00004 |
| Electricity | 0 | 0.0025 |
| TOTAL | 0.029 | 0.013 |
Steam disinfection is an energy-based sterilisation process. Extra energy consumption by steam disinfection highly depends on the path and conditions during the steam generation process. In the simplest case, 2.63 MJ energy is needed to transform 1 kg water (10 °C) to 1 kg dry steam (100 °C) at atmospheric pressure. There are mobile units used in Europe, consuming about 1,300 L/h and 12 L/h [62]. However, the total amount of steam used has not been readily available.
The extra energy and environment footprints can be estimated based on some online calculators, e.g. Steam Tables [63], when the information of consumption amount is available in future. Although there are merits for the steam disinfection, its effects are sensitive to the temperature setting and the time of disinfection. For reducing energy consumption and environmental footprint, a comprehensive assessment is urgently needed to select the suitable disinfection technologies for different disinfection tasks, e.g. the environmental disinfection, household disinfection, personal disinfection and extended use of PPE. The corresponding WHO standards and national standards on the selection of disinfection technology should be given and explained explicitly to avoid secondary disasters in the energy and environment sector.
The lasting impacts of the disease pandemic on energy efficiency, energy access, energy transition and renewable energy deployment remain to be investigated [65]. The World Bank mentioned several times that the latest statistics in the report are estimated without considering the COVID-19 impacts. This implies that nearly all macro energy planning and strategy should be updated or adjusted based on
-
i)
The projection of COVID-19 impacts during the disease pandemic or
-
ii)
The expected statistics after the disease pandemic.
Decision-makers face considerable challenges to keep progress to the original plans made before the disease pandemic, e.g. the Sustainable Development Goals (SDGs) targets by 2030 [66]. Along with challenges, unprecedented opportunities and motivations, e.g. the global collaboration, the regional synergy and the research and development (R&D) of low-risk non-toxic disinfectants, have existed in the energy and environment sector.
5. Future PPE and environmentally sustainable measures
Liu et al. [67] stated that the trend of the world energy market in the post-COVID-19 era should be given more attention. Environmental sustainability of PPE, under unavoidable usage, highly depends on how PPE is being used and treated at the end-of-life. The environmental friendlier options can overturn the results, creating more GHG footprint, if it is not adequately utilised and disposed of, e.g. the situation when reusable fabric masks are disposed of after single/minimal reuse. It is important that the emergency measures implemented to tackle COVID-19 or other future crises, do not derail the efforts to address pressing environmental challenges [68]. The improvement and development needed for future PPE as well as the healthcare system, are listed as follows.
-
•
Develop a more resilient supply chain and consider the environmental footprint as much as possible.
The resilience of supply chains of PPE and disinfectants needs to be strengthened to confront disruptions prompted by a disease outbreak. For a comparatively recently broken crisis without enough data available, the popular data-driven supply chain management even supported by advanced machine-learning techniques could present a high risk for adequate planning and timely supply. In such a situation, the fusion of expert knowledge may assist in promoting a more resilient supply chain. Golan et al. [69] highlighted that the common goal of supply chain modelling is to optimise efficiency and cost; however, trade-offs of efficiency and resilience is not fully addressed. Remko [70] stated that the COVID-19 crisis shows a lack of preparedness, shortcomings of current response plans. More study is required to minimise the potential risk with adequate concern on environmental performance through minimising energy consumption. Optimal allocation under resources constraints as performed by Sy et al. [71] is also important to support the emergency decision making.
-
•
Diversify the solutions, especially the reusable options
Diversification provides a lower risk of supply disruption and higher flexibility. The wider selection could offer the solution with lower life cycle energy consumptions as possible, even facing the life-threatening crisis. For example, bio-based PPE, e.g. mask [72], utilising 3D printing [73] and reusable device, e.g. bronchoscopes, [74]. Liao et al. [59] assessed the different disinfection treatment for N95, including dry heat, steam, ethanol, chlorine-based, and Ultraviolet Germicidal Irradiation. It can be treated for 10–50 cycles without a significant drop in filtration efficiency. However, energy consumption needs to be quantified. More research and novel technology development supported by verification on the effectiveness and sustainability of these options are needed. Standard user manual and protocol need to be established to avoid misinformation and confusion. A typical example has been the confusion about mask usage and its effectiveness that happened in the earlier stages of the pandemic.
-
•
Assess the burdening footprint of reusing (e.g. washing, sterilisation)
Although reusable PPE or devices reduce the amount of waste, to fully understand the life cycle energy consumptions and environmental sustainability, assessment is a need. A comprehensive assessment framework and quantification method need further development. This is especially the assumption in the number of uses and the approaches of washing/sterilisation/decontamination, which are responsible for up to 90% GHG emissions [75]. Biobased [76] and reusable PPE or devices did not necessarily offer a lower environmental impact. The circumstances/limit where the environmental benefit is no longer valid need to be clearly established.
-
•
Reduce the energy consumption of hospital building
The urge for sustainable practices and reduce the energy consumption of hospital building has been an on-going study [77]. The issues become even apparent with the incident of COVID-19 where the hospital is playing the key role in protecting human health and life. Lights (36%) and biomedical equipment (34%) are the main electrical consumption pathways in a hospital [78]. Buonomano et al. [79] suggested that the adoption of thermostatic valves and Air Handling Unit control system could contribute to high energy savings. Waste heat recovery could also be an option toward sustainability [80]. Research in minimising the energy usage of hospital building should be encouraged. Wang et al. [81] stated that economic incentives and regulation enforcement are important in encouraging the full participation and support of hospital stakeholders.
-
•
Improve the waste sorting and enhance the technology development in handling medical waste sustainably
There have been studies (e.g. Runcie et al. [82]) suggested that the clinical and non-clinical waste is not adequately disposed of due to the lack of waste sorting awareness. Better and detailed sorting could increase the availability of different recycling and treatment options. This is especially important as it is understood that a single disposal device or equipment cannot be completely replaced. Sorting could ensure regular waste in the hospital, especially plastic waste, to be recovered as energy sources to minimise the environmental footprints. Different treatments of medical waste have been discussed by Fang et al. [83], where incineration is seen as the most technically and economically feasible. However, it releases emission and toxic metals. Fang et al. [83] proposed the optimised pyrolysis for mixed medical waste. However, the economic feasibility is yet to be assessed. More options, especially the mobilised equipment and treatment with minimum needs of human operation, are worth for exploration.
-
•
Improve the response of waste management systems under a change in amount, composition and disseminated location
This issue has been recently discussed in Klemeš et al. [36], which appeals to focus on topics related to disaster waste management, especially the optimisation of disaster waste management planning on the regional scale. However, it should be noted that the impacts of COVID-19 on waste management can be diverse, depending on the geographical and sociological factors [84]. The differences in impacts required special attention for a higher practicality response and decision making.
6. Conclusion
Epidemic and pandemic crisis, e.g. COVID-19, is regretfully not likely to be isolated case. The to-date approximate estimations based on reported data of variable accuracy on the additional energy consumption or environmental footprint increase owning to COVID-19 can be assessed as:
-
•
The energy consumption due to hospitalisation = ∼356 PJ (22.2 M cases, 34% hospitalisation)
-
•
The energy consumption in plastic production of 390 M test kits (only the fast tests considered, with more rigorous the numbers will increase) = ∼168 TJ
-
•
The energy consumption of shield production to fulfil the forecasted demand = 3.9 TJ/month
-
•
The energy consumption of masks production to fulfil the forecasted demand = 4.6 PJ/month
-
•
The energy consumption of gloves production to fulfil the forecasted demand = 7.0 TJ/month
-
•
The energy consumption used for ethanol production related to disinfectants in 2020 (with an extra 12.3% growth rate in demand) = ∼181 PJ
-
•
The GHG footprints of N95 and surgical masks are suggested as ∼ 5 × 10−2 - 6 × 10−2 kg CO2eq/single use. The cloth mask is having a GHG footprint of ∼6 × 10−2 kg CO2eq/pcs; however, by considering the usage (with washing stages) is 0.036 kg CO2eq/usage.
-
•
The invested carbon emissions per filter efficiency returned of the surgical mask (80%), and emissions of cloth mask (50%) are ∼ 7.4 × 10−3 kg CO2eq/filter efficiency and ∼7.2 × 10−3 kg CO2eq/filter efficiency.
-
•
The emergency transportation could increase the energy consumption by 17.1 times (e.g. plane instead of a ship) in reducing the delay of transporting the lifesaving resources.
The COVID-19 pandemic has been still widely acting in the world. Its actual consequences could be fully understood after the disease pandemic only. The results in this present study serve as an initial step, summarising some references for a better assessment in the future. The effect of COVID-19 on global energy consumption can be estimated based on different penetration rates in future years. It should be noted that there are significant assumptions in estimating the resulting energy consumption and GHG emission, as stated in this manuscript. The value of this study is mainly to highlight the issues rather than pursuing accurate quantification. The quantitative data quoted in this paper should be used with caution, especially when there exist many uncertainties in the current phase. The overview and insight offered in this study, which, based on the burdening impacts of COVID-19 arises from additional demand for energy and resources, serve as a direction for corrective measures. Reusable PPE are highlighted as an option with lower energy consumption; however, a proper design standard, material selection and user guideline are needed to ensure its effectiveness. The environmentally friendly alternatives in combating infectious disease apparently have to be developed systematically, and there is an urgent need for more research. Diversifying solution is a vital strategy to improve the susceptibility to an unexpected event. It provides flexibility in optimising energy consumption and environmental footprint. If well taken, the lesson could prepare humankind more ready in preventing, containing and mitigating future infectiousness diseases without huge compromise on environmental sustainability. During the crises, the additional energy consumed were mainly offset by reductions caused by the decrease of production, travel and social activities. Although COVID-19 offers temporary environmental benefit and reduction of energy demand in some of the non-essential sectors/services during the lockdown, the impact on the structural and behavioural changes should not be underestimated. The society is now facing a period when the recovery is strongly economically supported; however, pandemic fighting measures should be still in place. A proper restructure on various existing systems, e.g. production, energy, supply chain, waste management, in new norms during and after COVID-19 is required.
CRediT author statement
Jiří Jaromír Klemeš: Conceptualisation, Original draft, Supervision, Writing-revising and editing, Funding Acquisition. Yee Van Fan: Conceptualisation, Original draft, Writing-revising and editing, Data Curation, Visualisation. Peng Jiang: Conceptualisation, Original draft, Data collection and curation, Writing-revising and editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
The authors gratefully acknowledge financial support from the EU project Sustainable Process Integration Laboratory – SPIL, funded as project No. CZ.02.1.01/0.0/0.0/15_ 003/0000456, by Czech Republic Operational Programme Research and Development, Education, Priority 1: Strengthening capacity for quality research.
References
- 1.WHO . 2020. Influenza: are we ready?www.who.int/influenza/spotlight [Google Scholar]
- 2.Worldometer . 2020. Coronavirus cases.www.worldometers.info/coronavirus/#countries [Google Scholar]
- 3.Akiyama M.J., Spaulding A.C., Rich J.D. Flattening the curve for incarcerated populations—covid-19 in jails and prisons. N Engl J Med. 2020;382(22):2075–2077. doi: 10.1056/NEJMp2005687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Atkeson A. Rough estimates of disease scenarios (No. w26867) National Bureau of Economic Research; 2020. What will be the economic impact of COVID-19 in the US? [DOI] [Google Scholar]
- 5.Čuček L., Klemeš J.J., Kravanja Z. A review of footprint analysis tools for monitoring impacts on sustainability. J Clean Prod. 2012;34:9–20. [Google Scholar]
- 6.Goel S., Hawi S., Goel G., Thakur V.K., Pearce O., Hoskins C., Pearce O., Hussain T., Upadhyayay H.M., Cross G., Barber A.H. Resilient and agile engineering solutions to address societal challenges such as coronavirus pandemic. Materials Today Chemistry. 2020;100300 doi: 10.1016/j.mtchem.2020.100300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Business Insider . 2020. One key figure helps countries decide when their coronavirus outbreaks are over-but scientists say it’s a moving target.www.businessinsider.com/how-countries-decide-to-lift-coronavirus-lockdowns-basic-reproduction-number-2020-4 27 July 2020 [Google Scholar]
- 8.Vajda J., Weber D., Brekel D., Hundt B., Müller E. Size distribution analysis of influenza virus particles using size exclusion chromatography. J Chromatogr A. 2016;1465:117–125. doi: 10.1016/j.chroma.2016.08.056. [DOI] [PubMed] [Google Scholar]
- 9.Yu I.M., Oldham M.L., Zhang J., Chen J. Crystal structure of the severe acute respiratory syndrome (SARS) coronavirus nucleocapsid protein dimerization domain reveals evolutionary linkage between corona-and arteriviridae. J Biol Chem. 2006;281(25):17134–17139. doi: 10.1074/jbc.M602107200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.AABB . 2013. Middle East respiratory syndrome coronavirus.www.aabb.org/tm/eid/Documents/middle-east-respiratory-syndrome-coronavirus [Google Scholar]
- 11.Baylor College of Medicine Ebola Virus. www.bcm.edu/departments/molecular-virology-and-microbiology/emerging-infections-and-biodefense/specific-agents/ebola-virus# :∼:text=Ebola%20viruses%20belong%20to%20a,a%20diameter% 20of%2080%20nanometers.
- 12.Le Quéré C., Jackson R.B., Jones M.W., Smith A.J., Abernethy S., Andrew R.M., Friedlingstein P. Temporary reduction in daily global CO 2 emissions during the COVID-19 forced confinement. Nat Clim Change. 2020:1–7. [Google Scholar]
- 13.Kanniah K.D., Zaman N.A.F.K., Kaskaoutis D.G., Latif M.T. COVID-19’s impact on the atmospheric environment in the Southeast Asia region. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.139658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nakada L.Y.K., Urban R.C. COVID-19 pandemic: impacts on the air quality during the partial lockdown in São Paulo state, Brazil. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.139087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma S., Zhang M., Gao J., Zhang H., Kota S.H. Effect of restricted emissions during COVID-19 on air quality in India. Sci Total Environ. 2020;728:138878. doi: 10.1016/j.scitotenv.2020.138878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collivignarelli M.C., Abbà A., Bertanza G., Pedrazzani R., Ricciardi P., Miino M.C. Lockdown for CoViD-2019 in Milan: what are the effects on air quality? Sci Total Environ. 2020;732:139280. doi: 10.1016/j.scitotenv.2020.139280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen H., Huo J., Fu Q., Duan Y., Xiao H., Chen J. Impact of quarantine measures on chemical compositions of PM2. 5 during the COVID-19 epidemic in Shanghai, China. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.140758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adams M.D. Air pollution in Ontario, Canada during the COVID-19 state of emergency. Sci. Total Environ. 2020:140516. doi: 10.1016/j.scitotenv.2020.140516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Almond D., Du X., Zhang S. Did COVID-19 improve air quality near hubei? (No. w27086) National Bureau of Economic Research. 2020 doi: 10.3386/w27086. [DOI] [Google Scholar]
- 20.Wang P., Chen K., Zhu S., Wang P., Zhang H. Severe air pollution events not avoided by reduced anthropogenic activities during COVID-19 outbreak. Resour Conserv Recycl. 2020;158:104814. doi: 10.1016/j.resconrec.2020.104814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gillingham K.T., Knittel C.R., Li J., Ovaere M., Reguant M. The short-run and long-run effects of covid-19 on energy and the environment. Joule. 2020;4(7):1337–1341. doi: 10.1016/j.joule.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCarthy N. Statista; 2020. The countries with the most critical care beds per capita.www.statista.com/chart/21105/number-of-critical-care-beds-per-100000-inhabitants [Google Scholar]
- 23.Bawaneh K., Ghazi Nezami F., Rasheduzzaman M., Deken B. Energy consumption analysis and characterization of healthcare facilities in the United States. Energies. 2019;12(19):3775. [Google Scholar]
- 24.HCWH (Health Care Without Harm) 2019. Health care’s climate footprint: how the health sector contributes to the global climate crisis and opportunities for action. noharm-global.org/sites/default/files/documents-files/5961/HealthCaresClimate Footprint_090619.pdf. [Google Scholar]
- 25.García-Sanz-Calcedo J., Gómez-Chaparro M., Sanchez-Barroso G. Electrical and thermal energy in private hospitals: consumption indicators focused on healthcare activity. Sustainable Cities and Society. 2019;47:101482. [Google Scholar]
- 26.CDC (Centers for Disease Control and Prevention) Severe outcomes among patients with coronavirus disease 2019 (COVID-19) — United States, 12 february–16 March, 2020. MMWR (Morb Mortal Wkly Rep) 2020;69:343–346. doi: 10.15585/mmwr.mm6912e2. 10.15585/mmwr.mm6912e2external icon. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gallego-Schmid A., Mendoza J.M.F., Azapagic A. Environmental impacts of takeaway food containers. J Clean Prod. 2019;211:417–427. [Google Scholar]
- 28.Walensky R.P., Del Rio C. From mitigation to containment of the COVID-19 pandemic: putting the SARS-CoV-2 genie back in the bottle. Jama. 2020;323(19):1889–1890. doi: 10.1001/jama.2020.6572. [DOI] [PubMed] [Google Scholar]
- 29.FDA . 2020. Coronavirus testing basics.www.fda.gov/consumers/consumer-updates/coronavirus-testing-basics [Google Scholar]
- 30.ADB . 2020. Global shortage of personal protective equipment amid COVID-19: supply chains, bottlenecks, and policy implication.www.adb.org/sites/default/files/publication/579121/ppe-covid-19-supply-chains-bottlenecks-policy [Google Scholar]
- 31.LISPASTO . 2017. Unit emissions.lipasto.vtt.fi/yksikkopaastot/indexe.htm [Google Scholar]
- 32.Klemeš J.J., Fan Y.V., Jiang P. Plastics: friends or foes? The circularity and plastic waste footprint, energy sources, Part A: recovery. Utilization, and Environmental Effects. 2020 doi: 10.1080/15567036.2020.1801906. [DOI] [Google Scholar]
- 33.Ecochain The rise of the face mask: what’s the environmental impact of 17 million N95 masks? 2020. ecochain.com/knowledge/footprint-face-masks-comparison
- 34.Prata J.C., Patrício Silva A.L., Walker T.R., Duarte A.C., Rocha Santos T. COVID-19 pandemic repercussions on the use and management of plastics. Environ Sci Technol. 2020;54(13):7760–7765. doi: 10.1021/acs.est.0c02178. [DOI] [PubMed] [Google Scholar]
- 35.Allison A.L., Ambrose-Dempster E., T Aparsi D., Bawn M., Casas Arredondo M., Chau C., Chandler K., Dobrijevic D., Hailes H., Lettieri P., Liu C., Medda F., Michie S., Miodownik M., Purkiss D., Ward J. UCL Press; 2020. The environmental dangers of employing single-use face masks as part of a COVID-19 exit strategy. [DOI] [Google Scholar]
- 36.Klemeš J.J., Fan Y.V., Tan R.R., Jiang P. Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew Sustain Energy Rev. 2020;127:109883. doi: 10.1016/j.rser.2020.109883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goorej . 2020. Case study – glove manufacturing.www.godrejcas.com/case-studies/pharmaceutical-industry/glove-manufacturing [Google Scholar]
- 38.Konda A., Prakash A., Moss G.A., Schmoldt M., Grant G.D., Guha S. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano. 2020;14(5):6339–6347. doi: 10.1021/acsnano.0c03252. [DOI] [PubMed] [Google Scholar]
- 39.Smith J.D., MacDougall C.C., Johnstone J., Copes R.A., Schwartz B., Garber G.E. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis. CMAJ (Can Med Assoc J) 2016;188(8):567–574. doi: 10.1503/cmaj.150835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee S.A., Hwang D.C., Li H.Y., Tsai C.F., Chen C.W., Chen J.K. Particle size-selective assessment of protection of European standard FFP respirators and surgical masks against particles-tested with human subjects. Journal of Healthcare Engineering. 2016;2016 doi: 10.1155/2016/8572493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Long Y., Hu T., Liu L., Chen R., Guo Q., Yang L., Du L. Effectiveness of N95 respirators versus surgical masks against influenza: a systematic review and meta-analysis. J Evid Base Med. 2020;13(2):93–101. doi: 10.1111/jebm.12381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.WHO . 2020. Advice on the use of masks in the context of COVID-19. Interim Guidance 5 June 2020.apps.who.int/iris/rest/bitstreams/1279750/retrieve [Google Scholar]
- 43.Davies A., Thompson K.A., Giri K., Kafatos G., Walker J., Bennett A. Testing the efficacy of homemade masks: would they protect in an influenza pandemic? Disaster Med Public Health Prep. 2013;7(4):413–418. doi: 10.1017/dmp.2013.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Robertson P. Can masks capture coronavirus particles? – SmartAir. 2020. smartairfilters.com/en/blog/diy-homemade-mask-protect-virus-coronavirus
- 45.China News . 2020. Ministry of Industry and Information Technology: the operating rate of disinfection products is gradually increasing, and the supply can meet the demand.www.chinanews.com/gn/2020/02-13/9090354.shtml [Google Scholar]
- 46.Allison The hand sanitizer market in China - demand after COVID-19. 2020. daxueconsulting.com/hand-sanitizer-market-in-china
- 47.Kyodo News Japan breweries answer call for strong alcohol amid sanitizer shortage. 2020. english.kyodonews.net/news/2020/04/5e47d5018f49-feature-japan-breweries-answer-call-for-strong-alcohol-amid-sanitizer-shortage.html
- 48.Guynn J. 2020. Looking for Lysol spray and Clorox wipes? COVID-19 wiped out disinfectants, but here’s when you can buy again.www.usatoday.com/story/money/2020/04/09/coronavirus-clorox-lysol-shortages-walmart-costco-publix-winco-lowes/2961818001 [Google Scholar]
- 49.Xinhua net . 2020. Nearly 2,000 t of disinfectants were used to promote enhanced disinfection of urban drainage and sewage facilities in Wuhan.www.xinhuanet.com/fortune/2020-02/20/c_1125600148.htm [Google Scholar]
- 50.Nabi G., Wang Y., Hao Y., Khan S., Wu Y., Li D. Massive use of disinfectants against COVID-19 poses potential risks to urban wildlife. Environ Res. 2020;188:109916. doi: 10.1016/j.envres.2020.109916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang H., Tang W., Chen Y., Yin W. Disinfection threatens aquatic ecosystems. Science. 2020;368(6487):146–147. doi: 10.1126/science.abb8905. [DOI] [PubMed] [Google Scholar]
- 52.Wang J., Shen J., Ye D., Yan X., Zhang Y., Yang W., Li X., Wang J., Pan L. Disinfection technology of hospital wastes and wastewater: suggestions for disinfection strategy during coronavirus Disease 2019 (COVID-19) pandemic in China. Environ. Pollut. 2020:114665. doi: 10.1016/j.envpol.2020.114665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Berardi A., Perinelli D.R., Merchant H.A., Bisharat L., Basheti I.A., Bonacucina G., Palmieri G.F. Hand sanitisers amid CoViD-19: a critical review of alcohol-based products on the market and formulation approaches to respond to increasing demand. Int J Pharm. 2020 doi: 10.1016/j.ijpharm.2020.119431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Technavio . 2020. COVID-19 impact and recovery analysis- global surface disinfectants market 2020-2024.www.businesswire.com/news/home/20200618005734/en/COVID-19-Impact-Recovery-Analysis--Global-Surface-Disinfectants [Google Scholar]
- 56.FIRI . 2020. Research report of the disinfection industry in China 2020.pdf.dfcfw.com/pdf/H3_AP202003181376603847 _1.pdf Forward Industry Research Institute (FIRI) [Google Scholar]
- 57.Garside M. 2020. Ethanol fuel production in top countries 2019.www.statista.com/statistics/281606/ethanol-production-in-selected-countries [Google Scholar]
- 58.Wang Y., Cheng M.H., Wright M.M. Lifecycle energy consumption and greenhouse gas emissions from corncob ethanol in China. Biofuels, Bioproducts and Biorefining. 2018;12(6):1037–1046. [Google Scholar]
- 59.Liao L., Xiao W., Zhao M., Yu X., Wang H., Wang Q., Cui Y. Can N95 respirators be reused after disinfection? How many times? ACS Nano. 2020;14(5):6348–6356. doi: 10.1021/acsnano.0c03597. [DOI] [PubMed] [Google Scholar]
- 60.Carrillo I.O., Floyd A.C., Valverde C.M., Tingle T.N., Zabaneh F.R. Immediate-use steam sterilisation sterilizes N95 masks without mask damage. Infect Contr Hosp Epidemiol. 2020:1–2. doi: 10.1017/ice.2020.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Steamericas, Inc. 2020. Incorporating dry vapor steam into disinfection processes against SARS-CoV-2.www.foodsafetymagazine.com/signature-series/incorporating-dry-vapor-steam-into-disinfection-processes-against-sars-cov-2/#References [Google Scholar]
- 62.Karcher www.karcher.cz/cz/?cid=cz-SEA-ESlZRh_TXkmzfScrJK15pg
- 63.Sarco-Spirax . 2020. Steam Tables.www.spiraxsarco.com/resources-and-design-tools/steam-tables/dry-saturated-steam-line#article-top [Google Scholar]
- 64.SaniVap . 2013. Steam biocleaning: the hygienic solution for healthcare establishments.www.sanivap.fr/en/health/le-bionettoyage-vapeur [Google Scholar]
- 65.World Bank . 2020. Tracking SDG 7: the energy progress report 2020.trackingsdg7.esmap.org/data/files/download-documents/tracking_sdg_7_ 2020-full_report_-_web_0.pdf Washington, DC. [Google Scholar]
- 66.WHO . 2020. COVID-19 intensifies the urgency to expand sustainable energy solutions worldwide.www.who.int/news-room/detail/28-05-2020-covid-19-intensifies-the-urgency-to-expand-sustainable-energy-solutions-worldwide [Google Scholar]
- 67.Liu, H., Zhang Z., Zhang T., Wang L., 2020. Revisiting Chian’s provincial energy efficiency and its influencing factors. DOI: 10.1016/j.energy.2020.118361. [DOI] [PMC free article] [PubMed]
- 68.OEDC 2020. www.oecd.org/coronavirus/policy-responses/from-containment-to-recovery-environmental-responses-to-the-covid-19-pandemic-92c49c5c
- 69.Golan M.S., Jernegan L.H., Linkov I. Trends and applications of resilience analytics in supply chain modeling: systematic literature review in the context of the COVID-19 pandemic. Environment Systems & Decisions. 2020;40:222–243. doi: 10.1007/s10669-020-09777-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Remko, V. H., 2020. Research opportunities for a more resilient post-COVID-19 supply chain-closing the gap between research findings and industry practice. International Journal of Operations & Production Management. ISSN: 0144-3577.
- 71.Sy C.L., Aviso K.B., Cayamanda C.D., Chiu A.S.F., Lucas R.I.G., Promentilla M.A.B., Ubando A.T. Process integration for emerging challenges: optimal allocation of antivirals under resource constraints. Clean Technol Environ Policy. 2020:1–12. doi: 10.1007/s10098-020-01876-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Das O., Neisiany R.E., Capezza A.J., Hedenqvist M.S., Försth M., Xu Q., Ramakrishna S. The need for fully bio-based facemasks to counter coronavirus outbreaks: a perspective. Sci. Total Environ. 2020:139611. doi: 10.1016/j.scitotenv.2020.139611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tino R., Moore R., Antoline S., Ravi P., Wake N., Ionita C.N., Chepelev L.L. COVID-19 and the role of 3D printing in medicine. 3D Print Med. 2020;6(1):11. doi: 10.1186/s41205-020-00064-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sohrt A., Ehlers L., Udsen F.W., Mærkedahl A., McGrath B.A. Cost comparison of single-use versus reusable bronchoscopes used for percutaneous dilatational tracheostomy. PharmacoEconomics-open. 2019;3(2):189–195. doi: 10.1007/s41669-018-0091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hofheinz E. 2020. Environmental impact of disposable vs reusable instruments.ryortho.com/breaking/environmental-impact-of-disposable-vs-reusable-instruments [Google Scholar]
- 76.Walker S., Rothman R. Life cycle assessment of bio-based and fossil-based plastic: a review. J Clean Prod. 2020:121158. [Google Scholar]
- 77.Eckelman M.J., Sherman J.D., MacNeill A.J. Life cycle environmental emissions and health damages from the Canadian healthcare system: an economic-environmental-epidemiological analysis. PLoS Med. 2018;15(7) doi: 10.1371/journal.pmed.1002623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Saidur R., Hasanuzzaman M., Yogeswaran S., Mohammed H.A., Hossain M.S. An end-use energy analysis in a Malaysian public hospital. Energy. 2010;35(12):4780–4785. [Google Scholar]
- 79.Buonomano A., Calise F., Ferruzzi G., Palombo A. Dynamic energy performance analysis: case study for energy efficiency retrofits of hospital buildings. Energy. 2014;78:555–572. [Google Scholar]
- 80.Bujak J.W. Production of waste energy and heat in hospital facilities. Energy. 2015;91:350–362. [Google Scholar]
- 81.Wang T., Li X., Liao P.C., Fang D. Building energy efficiency for public hospitals and healthcare facilities in China: barriers and drivers. Energy. 2016;103:588–597. [Google Scholar]
- 82.Runcie H. Sort your waste! an audit on the use of clinical waste bins and its implications. Future Healthcare Journal. 2018;5(3):203. doi: 10.7861/futurehosp.5-3-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fang S., Jiang L., Li P., Bai J., Chang C. Study on pyrolysis products characteristics of medical waste and fractional condensation of the pyrolysis oil. Energy. 2020;195:116969. [Google Scholar]
- 84.Fan Y.V, Jiang P., Hemzal M., Klemeš J.J. An update of COVID-19 influence on waste management. Sci Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.142014. [DOI] [PMC free article] [PubMed] [Google Scholar]