Abstract
Background
Rising telehealth capabilities and improving access to older adults can aid in improving health outcomes and quality of life indicators. Telehealth is not being used ubiquitously at present.
Objective
This review aimed to identify the barriers that prevent ubiquitous use of telehealth and the ways in which telehealth improves health outcomes and quality of life indicators for older adults.
Methods
This systematic review was conducted and reported in accordance with the Kruse protocol and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Reviewers queried the following four research databases: Cumulative Index of Nursing and Allied Health Literature (CINAHL), PubMed (MEDLINE), Web of Science, and Embase (Science Direct). Reviewers analyzed 57 articles, performed a narrative analysis to identify themes, and identified barriers and reports of health outcomes and quality of life indicators found in the literature.
Results
Reviewers analyzed 57 studies across the following five interventions of telehealth: eHealth, mobile health (mHealth), telemonitoring, telecare (phone), and telehealth video calls, with a Cohen κ of 0.75. Reviewers identified 14 themes for barriers. The most common of which were technical literacy (25/144 occurrences, 17%), lack of desire (19/144 occurrences, 13%), and cost (11/144 occurrences, 8%). Reviewers identified 13 medical outcomes associated with telehealth interventions. The most common of which were decrease in psychological stress (21/118 occurrences, 18%), increase in autonomy (18/118 occurrences, 15%), and increase in cognitive ability (11/118 occurrences, 9%). Some articles did not report medical outcomes (18/57, 32%) and some did not report barriers (19/57, 33%).
Conclusions
The literature suggests that the elimination of barriers could increase the prevalence of telehealth use by older adults. By increasing use of telehealth, proximity to care is no longer an issue for access, and thereby care can reach populations with chronic conditions and mobility restrictions. Future research should be conducted on methods for personalizing telehealth in older adults before implementation.
Trial Registration
PROSPERO CRD42020182162; https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020182162.
International Registered Report Identifier (IRRID)
RR2-10.2196/15490
Keywords: telehealth, telemedicine, older adults, barriers, health outcomes
Introduction
Background
A demographic shift has been evident globally since 2015. Specifically, the aging population has been growing at a rapid rate and has been predicted to reach 22% by the year 2050 [1]. In fact, the World Health Organization (WHO) estimates that during 2020, adults aged 60 years or older will outnumber children aged 5 years or younger [1]. The United States Census Bureau published a graphic on March 13, 2018, depicting the population pyramid from 1960 and comparing it with the 2060 prediction [2]. The graphic demonstrated the gradual change of the US population pyramid to a pillar shape [2]. This graphic is key to understanding the demands on the health care system in the area of geriatric, long-term, and end-of-life care, because it highlights the larger number of older adults living longer lives. By 2030, 60 million people in the “baby boomer” generation (born between 1946 and 1964) will have reached 65 years of age or older and will be eligible for age-related state entitlements in most countries [3,4]. This demographic shift is an impending issue facing health care, as geriatric, long-term, and end-of-life care will experience a surge in demand. Health care organizations and their providers must find ways to effectively allocate resources and provide the right care at the right time and at the right place [5].
Telemedicine has the potential to increase access among elderly people and relieve the stress regarding care for the unusually large number of elderly people. The WHO defines telemedicine as “healing from a distance.” More specifically, it is healing through the use of information and communication technologies “to improve patient outcomes by increasing access to care and medical information” [6]. The WHO also does not differentiate between the terms telemedicine and telehealth.
There has not been much work on the use of telehealth based on age; however, we know that a technology gap or digital divide exists. It is established by tiers of race, age, and economic disparities [7]. In the United States, for instance, the elder-care entitlement Medicare imposes restrictions on the use of telehealth for the primary population [8]. The Coronavirus Aid, Relieve, and Economic (CARES) Act provides a regulatory waiver to extend reimbursements to telemedicine, but this is only a relief act and not permanent legislation [9]. Previous reviews have investigated facilitators and barriers to the adoption of telehealth, the use of eHealth and mobile health (mHealth) tools in health promotion and primary prevention among older adults, and patient satisfaction with telehealth interventions [10-12]. A narrative analysis on mHealth solutions for the aging population used a generational analysis that included culture and trust of other people and a distrust of technology [13]. This work noted an increase in the use of technology for health purposes and an increase in the use of the internet for health purposes. It also noted concerns of security and privacy and technical troubleshooting. A review from 6 years ago spanned 10 years, analyzed 14 articles, and focused on older adults over 65 years old [10]. The most recent review on a topic most like this work was published 5 years ago, spanned 10 years, analyzed 45 articles, and focused on older adults aged over 50 years [11].
With an aging population, telehealth services are becoming more common to aid in independent living and health management [14]. An example of telehealth is virtual home health care, where health care providers provide guidance in specific procedures while the patients are in the comfort of their home. Telehealth programs can improve access to health care and have a positive effect on patients’ medical outcomes, especially for the treatment of chronic illnesses in vulnerable populations, such as elderly people [15]. Utilizing age-friendly technology could improve the care providers give to older adults through telehealth services and improve the usability of telehealth for older adults [16]. It is essential to first understand the barriers that affect the usability of telehealth services among older adults in order to find opportunities for improving health outcomes. Barriers to using telehealth can affect the accessibility of health services to older adults. When it comes to technology, older adults are often stereotyped as laggards in technology adoption [7]. However, owing to rising telehealth capabilities, improvement of access, especially to older adults, can aid in improving health outcomes [15]. Understanding the perspectives of older adults is important when evaluating telehealth barriers because older adults generally develop different perspectives compared with those of other age demographics [16]. Other studies on this topic have focused on conditions like depression, heart failure, and falls [17-19]. However, no review has looked at medical outcomes, including indicators of quality of life, that come as a benefit of using telehealth and the barriers that exist to the use of telehealth internationally. This review intends to examine these issues and what has changed in telehealth for older adults in the last 5 years.
Objectives
The purpose of this systematic review was to evaluate the current literature to help identify and understand health-related quality of life enhancers and general health outcomes that are commensurate with and barriers to the use of telehealth services by older adults. Health outcomes, including quality of life enhancers, provide the “so what” to the use of telehealth modalities. Recognizing barriers can help develop solutions for broadening the use of telehealth services in older adults. During the COVID-19 crisis, providers and patients alike were thrust into the world of telehealth. An overview of the benefits and barriers would be helpful to those deciding whether to continue the use of telehealth modalities.
Methods
Protocol and Registration
This review used the Kruse protocol published in 2019 and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [20,21]. The review was registered with PROSPERO on May 2, 2020 (ID: CRD42020182162). In accordance with the rules at PROSPERO, the registration was completed before analysis began.
Eligibility Criteria
Studies were eligible for this review if participants were older adults (older than 50 years), if the intervention was some form of telehealth (including mHealth, eHealth, and all forms of telehealth), if the authors reported either barriers to the use of telehealth or health outcomes, and if the article was published in a research journal in the English language in the last 5 years. Adults older than 50 years were chosen out of trial and error. When we initially wrote the methods for this study, we chose a more universal definition of older adults as those over 65 years of age. Once we started filtering articles for analysis, we noticed a large number of articles that were being eliminated, despite the high level of quality of these studies. If we had stuck with age over 65 years as our screening criteria, we would have eliminated more than half of the group of articles for analysis. As a result, we chose age over 50 years, which is supported by other reviews in this field [11]. This is a limitation we list later.
Information Sources
The following four databases were queried: Cumulative Index of Nursing and Allied Health Literature (CINAHL), PubMed (MEDLINE), Web of Science (WoS), and Embase (Science Direct). Additionally, a specific journal search was conducted in the journal of choice for publication (Journal of Medical Internet Research). Databases were filtered for the last 5 years. Database searches occurred between February 2 and 14, 2020. A period of 5 years was chosen because it has been that long since the last review was published on a similar topic. We expect to find advances in technology and advances in adoption by elderly people because younger people who use technology regularly have advanced into the observation group of over 50 years old. We hope to find fewer barriers.
Search
Reviewers carefully analyzed the MEDLINE Medical Subject Headings (MeSH) for key terms related to telehealth and elderly people. Based on the established hierarchy of indexed terms at MeSH and a series of experimental searches, the final search terms were “Telehealth AND ‘older adults.’” This combination of terms yielded the maximum number of results in all four databases. Reviewers used available filters to eliminate other reviews and focus on academic or peer-reviewed journals over the last 5 years.
Study Selection
Reviewers followed the Kruse protocol, which entails a series of three consensus meetings. The results of the first consensus meeting identified the studies for analysis. After filtering the results of the four databases to meet the eligibility criteria, all reviewers screened the abstracts of the results to ensure that articles were germane to the topic, they were actually studies (not protocols), and they contained tangible results to enable analysis toward the review’s objectives. The first consensus meeting discussed whether to keep articles for analysis. The reasons for rejection included opinion article (not a study), protocol (no results), concept or design paper (no results), review, no use of telehealth, and no reporting of either outcomes or barriers. A kappa statistic was calculated from the results of this meeting [20]. Before consensus meeting number two, the group leader assigned workload to ensure that each article was analyzed by at least two reviewers. Reviewers independently analyzed articles using a piloted form. Reviewers collected several standard items used for summary, such as PICOS (Participants, Intervention, Comparison [to the control group], Outcome, Study design), and analysis, such as forms of telehealth interventions, barriers to the use of telehealth by older adults, and the medical outcomes observed in older adults using telehealth solutions [20]. After making a list of observations, reviewers attempted to make sense of the observations using a narrative analysis [22].
Data Collection Process
The group leader divided analysis workload to ensure all articles were reviewed by at least two reviewers. Reviewers independently analyzed articles using a standardized Excel spreadsheet as a piloted form for data extraction.
Data Items
The piloted form collected data, including participants, intervention, study design, results compared to a control group (where applicable), medical outcomes, sample size, bias within studies, effect size, country of origin, statistics used, barriers to the use of telehealth, and quality assessment from the John Hopkins Nursing Evidence-Based Practice (JHNEBP) rating scale, as well as general observations about the article that would help in interpretation of the results [23]. These data items were independently collected and discussed in the second consensus meeting.
Risk of Bias Within and Across Studies
General observations of bias were made about each study, such as selection bias. These observations were independently collected and discussed in the second consensus meeting. The JHNEBP rating scale was used to assess the risk and quality of each study analyzed. Within the JHNEBP rating scale, level I indicates experimental studies, randomized controlled trials (RCTs), or meta analyses of RCTs; level II indicates quasiexperimental studies; level III indicates nonexperimental studies, qualitative studies, or meta-syntheses; level IV indicates opinions of nationally recognized experts based on research evidence or expert consensus panels (systematic reviews or clinical practice guidelines); and level V indicates opinions of individual experts based on nonresearch evidence. There are three levels of quality of evidence, which are listed as A (high quality), B (good quality), and C (low quality or major flaws). Each of these levels define the following four thresholds: research, summative reviews, organizational opinion, and expert opinion. For instance, in level A, studies have consistent results with sufficient sample size, adequate control, and definitive conclusions. In level C, studies have little evidence with inconsistent results and insufficient sample size, and conclusions cannot be drawn. To limit the inherent bias and limitations commensurate with low-quality studies, the ratings from the JHNEBP rating scale serve as screening criteria. Articles with evidence ratings below level IV were not accepted. Quality of evidence ratings below level B were highly suspect.
Summary Measures and Additional Analysis
The review analyzed both qualitative and quantitative methods, so the summary measures sought were not consistent. The preferred summary statistic was the risk ratio, but other summary statistics were also sufficient. The summary statistics were independently collected and discussed in the second consensus meeting.
A narrative analysis summarized themes for barriers, interventions, and medical outcomes. They were reported in summary statistics in affinity matrices. These themes were independently collected and discussed in the third consensus meeting. After themes were identified, interactions between themes were observed using a spreadsheet.
Results
Study Selection
Figure 1 illustrates the study selection process. A kappa statistic was calculated to measure the reliability of article selection between reviewers. The κ value was 0.75, representing moderate agreement [24,25].
Figure 1.
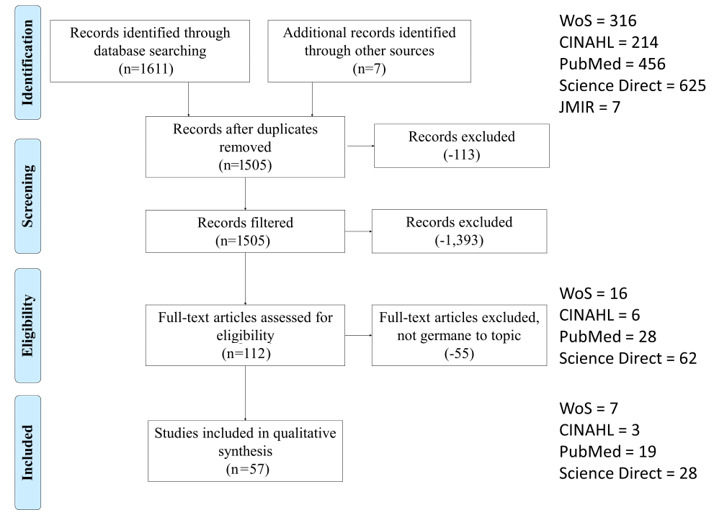
Study selection process.
Study Characteristics
Table 1 lists the ancillary data extracted from the studies analyzed in reverse chronological order as follows: 2020 [26], 2019 [5,26-34], 2018 [4,15,16,35-46], 2017 [14,47-56], 2016 [19,57-63], and 2015 [64-76].
Table 1.
PICOS characteristics.
| Authors, year | Participants | Intervention | Comparator | Medical outcomes reported | Study design |
| Hamilton et al, 2020 [26] | 765 older adults; ≥55 years; Medicare/Medicaid beneficiaries; English 76% (581), Spanish 20% (153), and others 4% (31); low income | Telemonitoring Remote patient monitoring (RPM): blood-pressure cuffs, pulse oximeters, and body weight scales Telehealth Intervention Programs for Seniors, RPM, extensive social wraparound services, care coordination, and intergenerational socialization aimed at improving health care options to assist low-income high health risk older adults who live in subsidized congregate housing or attend local community centers for older adults. A survey instrument was collected each week. |
None | Hospital visits and readmissions | Observational study |
| Theis et al, 2019 [5] | 551 older adults, ≥60 years, 51.3% male and 48.7% female 441 participants (80%) already retired, 109 (19.8%) still working |
eHealth | None | Satisfaction: 64% (353) of older adults were satisfied with the health information they received, 34% (187) were neutral, and 2% (11) were dissatisfied | Analytical observational study |
| Wildenbos et al, 2019 [27] | 13 older adults, ≥50 years, primarily Dutch speaking Additional inclusion criteria for App 2: heart failure (HF) patient and chronic obstructive pulmonary disease |
mHealtha Investigated these interaction issues in two different case studies; an app for older adults facilitating their hospital appointment attendance (App 1) and a self-monitoring app for chronically ill older patients |
None | Cognitive impairment was reported but not compared with a control. | Case study |
| Jakobsson et al, 2019 [28] | 9 older adults, 65-85 years, cognitive impairment of different origin (eg, stroke, dementia, and mild cognitive impairment) | Telehealth, smartphone, computer, and landline | None | Cognitive impairment was reported but not compared with a control. | Qualitative study |
| Karlsen et al, 2019 [29] | 18 older adults, ≥60 years, living in their own homes and having recently received telecare service (within the last 0-3 months), received home care services, Norwegian speaking, no limitations considering disease or chronic conditions | Telemonitoring Personal alarm (16), light sensors (3), stove alarm (4), GPS tracking (3), medication reminders (8), bed sensors (1), door sensor (2), video surveillance (2) |
None | Safety, satisfaction, security, independence, responsibility, mindfulness of failty | Qualitative study |
| Coley et al, 2019 [30] | 341 (quantitative) and 46 (qualitative) older adults; ≥65 years; Finland, France, and Netherlands; response rate 79% (Finland: 81%, France: 72%, Netherlands: 87%, P=.04); 48% (164) male; 51% (174) university-level education | eHealth Participants were randomized to either an interactive internet platform designed to encourage goal setting and lifestyle changes with the remote support of a lifestyle coach or a control platform with basic health information but no interactive features or coach support. Owing to the nature of the intervention, complete double blinding was not possible, but masking was attempted by informing participants that they would be randomized to one of two internet platforms (without further details on the content). |
Control | Not reported | Cross-sectional mixed-methods randomized controlled trial (RCT) |
| Giesbrecht & Miller, 2019 [31] | 18 older adults, ≥50 years, resided in the community, self-propelled using both hands at least 1 hour per day inside and outside their home, English speaking | eHealth The treatment group incorporated two in-person training sessions with a trainer and 4 weeks of monitored home training using a computer tablet (mHealth) wheelchair skills program. The control group did not receive skills training, as is typical practice with this population. |
Control | Skill capacity and safety | RCT |
| Brodbeck et al, 2019 [32] | 110 older adults, >50 years, 79% (87) female | eHealth Internet-based self-help intervention for prolonged grief symptoms after spousal bereavement or separation/divorce |
Control | Grief, depression, psychological distress, embitterment, loneliness, and life satisfaction | Mixed methods, RCT |
| Mosley et al, 2019 [33] | 112 older adults, ≥60 years, 58% (65) female, English speaking | eHealth Etymotic home hearing test compared with traditional manual audiometry |
Control | Not reported | Quasiexperimental study |
| Jensen et al, 2019 [34] | 20 older adults, hip fracture | eHealth “My Hip Fracture Journey” on iPad (provided) education through pictographs, video clips, illustrated exercises, and written information. This was used to augment home visits and subsequent interviews. |
None | Autonomy and self-care | Qualitative study |
| Rasche et al, 2018 [15] | 576 older adults, ≥60 years, 48.7% (280) female, German speaking | eHealth The national survey queried the use of health apps and their perceived usefulness. |
Control | Not reported | Quasiexperimental study |
| Portz et al, 2018 [35] | 30 older adults, ≥60 years, location at the University of Colorado Hospital and the University Hospital Cleveland Medical Center in Cleveland (Ohio), 60% (18) female, 63% (19) black people | mHealth The HF app was developed to allow patients to track their symptoms of HF. Thirty older adults completed an acceptability survey after using the mobile app. The survey used Likert items and open-ended feedback questions. |
None | Awareness of the condition and self-care | Quantitative acceptability survey analysis |
| Castro et al, 2018 [36] | 501 older adults, ≥65 years, Medicare population | eHealth Participants were matched into geographically based small groups with an assigned health coach, and they began the program at the same time. Group members were connected to each other through a private online social forum where they could post comments and questions, engage in health coach–moderated discussions, and provide social support to one another. Using internet-enabled devices (laptop, tablet, or smartphone), program participants were able to asynchronously complete weekly interactive curriculum lessons, reflections, and goal-setting activities in relation to the weekly topic. |
Pretest | Weight: participants lost an average of 13-14 pounds (8%) HbA1c: 0.14% absolute decrease at 6 months and 12 months (P<.001) Cholesterol: mean reduction of -12.92 mg/dL (P<.001). |
Single-arm pretest/posttest design |
| Joe et al, 2018 [37] | 43 older adults, 70% (30) female | eHealth A focus-group method was used to brainstorm designs for telehealth for older adults. |
None | Not reported | Qualitative analysis study (focus groups) |
| Dham et al, 2018 [4] | 134 older adults, 60% (80) female | Telemedicine Telepsychiatry assessments |
None | Not reported | Mixed-methods cross-sectional cohort study with retrospective chart review and prospective feedback survey |
| Paige et al, 2018 [16] | 384 older adults, 74.3% (285) female, 57.7% (222) Caucasian people, 42.3% (162) black people | eHealth eHealth awareness and eHealth literacy scale |
None | Not reported | Qualitative measurement invariance study |
| Cajita et al, 2018 [38] | 10 older adults, ≥65 years, history of HF, spoke English, difficulty with mobile technology | mHealth | None | Not reported | Descriptive exploratory study |
| Harte et al, 2018 [39] | 22 older adults, >65 years, difficulty using smartphones | mHealth Training on a smartphone-based fall detection and prevention system |
None | Not reported | Usability and learnability case study |
| Gordon & Hornbrook, 2018 [40] | 2602 older adults, >65 years, 54% (1,405) female, 79% (2,056) Caucasian people | eHealth Online forms, online tracking systems, and patient portal |
None | Not reported | Mixed-methods cross-sectional study |
| Bao et al, 2018 [41] | 12 older adults, ≥65 years, 75% (8) female | eHealth Online training |
Pretest | Sensory organization test, mini balance evaluation system test, five times sit to stand test, and no statistical significance in other clinical outcomes | Pretest posttest true experiment |
| Egede et al, 2018 [42] | 241 older adults, >63 years, 98% (236) male, 60% (144) Caucasian people, veterans having major depressive disorder | Telemedicine Telepsychotherapy |
Control | Baseline depression severity, generalized anxiety disorder, alcohol misuse, cannabis misuse, and cannabis dependence | RCT |
| Platts-Mills et al, 2018 [43] | 75 older adults, <50 years, musculoskeletal pain | Telecare Telephone call and protocol-guided follow up |
Control | Pain | Randomized controlled pilot study |
| Lopez-Villegas et al, 2018 [44] | 50 older adults, >65 years, 48% (24) women, seen in the cardiology clinic, using a pacemaker | Telemonitoring Pacemakers |
Control | EQ-5D VASb (health-related quality of life) | RCT |
| Dugas et al, 2018 [45] | 27 older adults, >60 years | mHealth DiaSocial for glucose control, exercise, nutrition, and medication adherence |
None | Glucose management and HbA1c | Pilot study |
| Nalder et al, 2018 [46] | 8 older adults, >55 years, type 2 diabetes | eHealth Three internet-based platforms: 1. Chronic disease management 2. Real-world strategy training 3. Learning the ropes |
None | HbA1c, independence, emotional support, and motivation to self-manage | Qualitative pilot program |
| Buck et al, 2017 [47] | 12 older adults, >60 years, 42% (5) female | eHealth PSHA, a web-based tablet-delivered intervention developed internally, which encourages the participant to record daily medication intake, weight, and time spent with a brief exercise program using an aerobic stepper. The tablet records daily information, and the participant watches a short heart health educational video. |
None | Documentation for nutrition and eating and instructional video exposure | Proof-of-concept trial Qualitative semistructured interviews after the study protocol |
| Ware et al, 2017 [14] | 15 older adults, ≥50 years, 73% (11) female | eHealth | None | Not reported | Two focus groups and pragmatic thematic analysis |
| Chang et al, 2017 [48] | 18 older adults, >65 years, diabetes | Telehealth Diabetes management |
None | Self-management and independence | Qualitative research design and 1-1 semistructured interviews |
| Cajita et al, 2017 [49] | 129 older adults, >65 years, 73.6% (95) male, 56.6% (73) Caucasian people | mHealth Simple linear regression was used to test the relationship between the main study variables (eHealth literacy, social influence, perceived financial cost, perceived ease of use, and perceived usefulness) and intention to use mHealth. |
None | Not reported | Cross-sectional correlational study |
| LaMonica et al, 2017 [50] | 221 older adults, ≥50 years, 57.7% (128) female | eHealth Memory aids and mental acuity exercises |
None | Memory | Qualitative study |
| Bahar-Fuchs et al, 2017 [51] | 45 older adults; >65 years; mild cognitive impairment (n=9), mood-related neuropsychiatric symptoms (n=11), or both (n=25) | eHealth Tailored and adaptive computer cognitive training in older adults at risk for dementia |
Control | Memory, global cognition, learning, and mood | RCT |
| Nahm et al, 2017 [52] | 866 older adults, >50 years, bone health issues | eHealth Bone Power program |
Control | Osteoporosis knowledge, self-efficacy/outcome expectations, and exercise behaviors | Two-arm RCT |
| Knaevelsrud et al, 2017 [53] | 47 older adults, >50 years, 64.9% (31) female, posttraumatic stress disorder symptoms, German speaking | eHealth Internet-based therapist-guided intervention |
Control | Comfort (from not being able to see the therapist), satisfaction, motivation, feeling of being understood | RCT |
| Reijnders et al, 2017 [54] | 376 older adults, >50 years, 67.5% female | eHealth Cognitive functioning |
Control | Feelings of stability, memory functioning, and locus of control | RCT |
| Hamblin et al, 2017 [56] | 60 older adults, >85 years | Telemonitoring | None | Autonomy, awareness of danger areas like gardens or staircases, and safety | Mixed-methods study |
| Mageroski et al, 2016 [55] | 25 older adults, >50 years | Telemonitoring Remote sensors in homes of older adults |
None | Not reported | Mixed-methods study |
| Wang et al, 2016 [57] | 29 older adults, >65 years, 71% (21) female | Telemonitoring Wearables, mobile devices, trackers, and in-home telemonitoring |
None | Not reported | Cross-sectional study |
| Gordon & Hornbrook, 2016 [58] | 231,082 older adults for database arm, 2602 older adults for survey arm | eHealth | None | Not reported | Mixed methods, database, and survey study |
| Williams et al, 2016 [59] | 7 older adults, >60 years, dementia | eHealth | None | Not reported | Pilot study |
| Evans et al, 2016 [19] | 41 older adults, >55 years, 57.1% (23) female, English speaking | mHealth Remote monitoring, wrist wearable, and wireless tablet |
Control | Documentation for weight and blood pressure | Single-arm quasiexperimental study |
| Muller et al, 2016 [60] | 43 older adults, ≥55 years, mobile phone use, no regular exercise | mHealth SMS and Physical Activity for Health Study |
Control | Exercise, mood, fitness, health, mindfulness of the importance of exercise, and guilt | Two-arm parallel RCT |
| Quinn et al, 2016 [61] | 118 older adults, >50 years, 66% (78) female, diabetes | mHealth Mobile diabetes intervention study |
Control | HbA1c | True experiment |
| Royackers et al, 2016 [62] | 8 older adults, caring for loved ones in their last days | eHealth Point of care technology through eShift (home-based palliative care) |
None | Comfort, independence, and autonomy | Qualitative pilot study |
| Duh et al, 2016 [63] | 45 older adults, >60 years | Telecare CareMe |
None | Not reported | Qualitative participatory design |
| Depatie & Bigbee, 2015 [64] | 30 older adults, ≥60 years, 80% (24) female | mHealth Mobile health technology for older adults in rural communities |
None | Not reported | Mixed-methods study |
| Moore et al, 2015 [65] | 26 older adults, >55 years, 77% (20) male | eHealth Internet-based hearing health care for older adults |
None | Not reported | Training study |
| Currie et al, 2015 [66] | 168 older adults, ≥60 years, living in rural areas, long-term chronic pain | eHealth | None | Pain | Mixed-methods study |
| Grant et al, 2015 [67] | 762 older adults, >60 years, 67% (511) female, 90% (686) Caucasian people | Telemonitoring LivingWell@Home, sensors (motion, bed, and humidity), emergency response systems, and biometric monitors (heart rate, blood pressure, weight, pulse oximetry, and blood glucose) |
Control | Satisfaction, autonomy, and independence | RCT |
| Brenes et al, 2015 [68] | 141 older adults, ≥60 years, 81% (114) female, living in rural areas, diagnosis of generalized anxiety disorder (GAD) | Telecare Telephone-delivered cognitive behavior therapy and telephone-delivered nondirective supportive therapy |
Control | Worry, GAD, depression, and anxiety | RCT |
| Corbett et al, 2015 [69] | 2192 older adults, ≥60 years | eHealth Online cognitive training package |
Control | Reasoning, verbal learning, and instrumental activities of daily living | RCT |
| Mavandadi et al, 2015 [70] | 1018 older adults, ≥65 years, 83.2% (847) female, community-dwelling, low-income, mental health symptoms | Telecare SUSTAIN care management system (assessment, monitoring, care management, and brief therapies) |
Control | Depressive symptoms, anxiety symptoms, and MH functioning | RCT |
| Egede et al, 2015 [71] | 90 older adults, ≥58 years, 98% (88) male, diagnosis of diabetes | Telemedicine Telepsychotherapy |
Control | Geriatric depression scale, Beck depression inventory, and Diagnostic and Statistical Manual, version 4 symptoms | RCT |
| Chang et al, 2015 [72] | 192 older adults, >60 years, 81% (156) female, cardiology diagnoses | Telemonitoring Remote cardiology management |
None | Cardiac arrhythmias detected and paroxysmal atrial fibrillation detected | Pilot study |
| Boulos et al, 2015 [73] | 27 older adults, 31 caregivers, 43 healthcare professionals | eHealth LiveWell Parkinson intervention and learning modules |
None | Communication of the condition with the provider | Pilot study |
| Dino & deGuzman, 2015 [74] | 82 older adults, demographics not reported | Telemedicine, mHealth, and eHealth | None | Not reported | Structured equation modeling |
| Czaja et al, 2015 [75] | 24 older adults, >60 years, 71% (17) female, 94% (23) Hispanic people, diagnosis of hypertension | Telemonitoring Telehealth system that monitors blood pressure and body weight |
Control | Self-management, health, and independence | Randomized feasibility study |
| Choi et al, 2015 [76] | 42 older adults, ≥60 years, 81% (34) female, low-income, homebound, score of 15 or above on the 24-item Hamilton Rating Scale for Depression | Telecare Video tele-problem-solving therapy (PST) to in-person PST and telephone care calls |
None | Depressive symptoms, understanding of depression, and social interaction | Qualitative |
amHealth: mobile health.
bEQ-5D VAS: European health-related quality of life utility with a visual analogue scale.
Risk of Bias Within Studies
At the study level, reviewers recorded observations of bias. The most frequently observed form of bias was selection bias (asking for volunteers for a research study involving technology will result in volunteers who already gravitate toward technology), which occurred in 7 out of 57 (13%) articles analyzed [15,26,30-32,37,39]. There were six instances of convenience samples from a local population [34,49-52,64]. Both examples of bias limit the external validity of the results.
Results of Individual Studies
Themes that resulted from the narrative analysis are listed in Table 2. Repetition can be observed in a frame of a theme owing to multiple observations from the same article for that theme. Translations from observations to themes for interventions, medical outcomes, and barriers are listed in Multimedia Appendix 1, Multimedia Appendix 2, and Multimedia Appendix 3, respectively. These appendices illustrate the logical inference reviewers made for each theme. For instance, one article listed remote patient monitoring for blood pressure, pulse oximeter, and body weight scales. These were categorized under telemonitoring [26]. The same article listed a decrease in hospital visits and a decrease in readmissions. These were categorized under an increase in hospital metrics. Additional data collected (bias, statistics, country of origin, and quality assessments) are displayed in Multimedia Appendix 4. In consensus meeting number two, we identified general observations, as depicted in the tables [20].
Table 2.
Summary of the analysis of each article.
| Authors, year | Intervention | Medical outcome theme | Theme of barriers |
| Hamilton et al, 2020 [26] | Telemonitoring | Increase in hospital metrics | Not reported |
| Theis et al, 2019 [5] | eHealth | Increase in satisfaction | Medical literacy Trust of the internet Ownership of technologya |
| Wildenbos et al, 2019 [27] | mHealthb | Increase in cognitive ability | Visual acuitya Mental acuity Technical literacy |
| Jakobsson et al, 2019 [28] | mHealth eHealth Telecare (phone) |
Increase in cognitive ability | Social implications Privacy and securitya Technical literacy Lack of desire Ownership of technology Lack of technical support |
| Karlsen et al, 2019 [29] | Telemonitoring | Increase in safety or security Increase in health-related quality of life Increase in safety or securitya Increase in autonomy Increase in mindfulness of the condition |
Mental acuity Visual acuity Social implications |
| Coley et al, 2019 [30] | eHealth | Not reported | Trust of the internet |
| Giesbrecht & Miller, 2019 [31] | eHealth | Increase in cognitive ability Increase in safety or security |
Not reported |
| Brodbeck et al, 2019 [32] | eHealth | Decrease in psychological distressa Increase in health-related quality of life |
Not reported |
| Mosley et al, 2019 [33] | eHealth | Not reported | Cost |
| Jensen et al, 2019 [34] | eHealth | Increase in autonomya | Privacy and security Ownership of technology Lack of desire Lack of technical support Technical literacy |
| Rasche et al, 2018 [15] | eHealth | Not reported | Trust of the internet Technical literacya Privacy and security |
| Portz et al, 2018 [35] | mHealth | Increase in mindfulness of the condition Increase in autonomy |
Technical literacy Medical literacy |
| Castro Sweet et al, 2018 [36] | eHealth | Decrease in medical conditions surrounding diabetesa | Not reported |
| Joe et al, 2018 [37] | eHealth | Not reported | Visual acuitya Hand-eye coordination Technical literacy Lack of desire |
| Dham et al, 2018 [4] | Telehealth video call | Increase in satisfaction | Visual acuity Auditory acuity |
| Paige et al, 2018 [16] | eHealth | Not reported | Technical literacy Trust of the internet |
| Cajita et al, 2018 [38] | mHealth | Not reported | Medical literacy Mental acuity Lack of desire Technical literacy Ownership of technology Cost |
| Harte et al, 2018 [39] | mHealth | Not reported | Technical literacy |
| Gordon & Hornbrook, 2018 [40] | eHealth | Not reported | Cost Technical literacy |
| Bao et al, 2018 [41] | eHealth | Increase in cognitive ability Increase in activity or coordinationa |
Not reported |
| Egede et al, 2018 [42] | Telehealth video call | Decrease in psychological distressa Decrease in medical conditions surrounding paina |
Not reported |
| Platts-Mills et al, 2018 [43] | Telecare (phone) | Decrease in medical conditions surrounding pain | Not reported |
| Lopez-Villegas et al, 2018 [44] | Telemonitoring | Increase in health-related quality of life | Not reported |
| Dugas et al, 2018 [45] | mHealth | Decrease in medical conditions surrounding diabetesa | Not reported |
| Nalder et al, 2018 [46] | eHealth | Decrease in medical conditions surrounding diabetes Increase in autonomy Decrease in psychological distress Increase in autonomy |
Technical literacy |
| Buck et al, 2017 [47] | eHealth | Increase in documentation to give the provider Increase in mindfulness of the condition |
Technical literacy |
| Ware et al, 2017 [14] | eHealth | Not reported | Trust of the internet Medical literacy Technical literacy Social implications Lack of technical support Privacy and security |
| Chang et al, 2017 [48] | mHealth | Increase in autonomya | Cost |
| Cajita et al, 2017 [49] | mHealth | Not reported | Medical literacy Lack of desire Cost Technical literacy Social implications |
| LaMonica et al, 2017 [50] | eHealth | Increase in cognitive ability | Auditory acuity Cost Auditory acuity |
| Bahar-Fuchs et al, 2017 [51] | eHealth | Increase in cognitive abilitya Decrease in psychological distress |
Not reported |
| Nahm et al, 2017 [52] | eHealth | Increase in mindfulness of the condition Increase in autonomy Increase in activity or coordination |
Not reported |
| Knaevelsrud et al, 2017 [53] | eHealth | Increase in safety or security Increase in satisfaction Increase in autonomy Increase in health-related quality of life |
Not reported |
| Reijnders et al, 2017 [54] | eHealth | Increase in activity or coordination Increase in cognitive ability Increase in autonomy |
Not reported Privacy and security |
| Hamblin et al, 2017 [56] | Telemonitoring | Increase in autonomy Increase in mindfulness of the condition Increase in safety or security |
Technical literacy Medical literacy Social implicationsa |
| Mageroski et al, 2016 [55] | Telemonitoring | Not reported | Cost |
| Wang et al, 2016 [57] | Telemonitoring | Not reported | Lack of desire |
| Gordon & Hornbrook, 2016 [58] | eHealth | Not reported | Ownership of technology Lack of technical support Cost Technical literacy Hand-eye coordination Trust of the internet Social implications Lack of desire |
| Williams et al, 2016 [59] | eHealth | Not reported | Technical literacy Lack of technical support Mental acuity Visual acuity Hand-eye coordination |
| Evans et al, 2016 [19] | mHealth | Increase in documentation to give the provider | Lack of desire Technical literacy Lack of desire Ownership of technology |
| Muller et al, 2016 [60] | mHealth | Increase in activity or coordinationa Decrease in psychological distress Decrease in medical conditions surrounding diabetes Increase in mindfulness of the condition Increase in guilt |
Lack of desire |
| Quinn et al, 2016 [61] | mHealth | Decrease in medical conditions surrounding diabetes | Visual acuity Auditory acuity |
| Royackers et al, 2016 [62] | eHealth | Increase in safety or security Increase in autonomya |
Not reported |
| Duh et al, 2016 [63] | Telecare (phone) | Not reported | Mental acuity Lack of desire Lack of technical support Technical literacy Cost |
| Depatie & Bigbee, 2015 [64] | mHealth | Not reported | Cost Lack of desire Social implications Technical literacy Lack of technical support Privacy and security |
| Moore et al, 2015 [65] | eHealth | Not reported | Technical literacy Computer anxiety Lack of technical support |
| Currie et al, 2015 [66] | eHealth | Decrease in medical conditions surrounding pain | Social implications |
| Grant et al, 2015 [67] | Telemonitoring | Increase in health-related quality of life Increase in autonomya |
Lack of desire Cost Privacy and security |
| Brenes et al, 2015 [68] | Telecare (phone) | Decrease in psychological distressa | Not reported |
| Corbett et al, 2015 [69] | eHealth | Increase in cognitive abilitya Increase in health-related quality of life |
Not reported |
| Mavandadi et al, 2015 [70] | Telecare (phone) | Decrease in psychological distressa | Not reported |
| Egede et al, 2015 [71] | Telehealth video call | Decrease in psychological distressa | Not reported |
| Chang et al, 2015 [72] | Telemonitoring | Increase in mindfulness of the conditiona | Not reported |
| Boulos et al, 2015 [73] | eHealth | Increase in documentation to give the provider | Medical literacy Lack of technical support Mental acuity Hand-eye coordination Visual acuity |
| Dino & deGuzman, 2015 [74] | mHealth eHealth Telemonitoring |
Not reported | Lack of desire Lack of technical support |
| Czaja et al, 2015 [75] | Telemonitoring | Increase in autonomya Decrease in medical conditions surrounding diabetes |
Technical literacy |
| Choi et al, 2015 [76] | Telehealth video call | Decrease in psychological distress Increase in mindfulness of the condition Increase in autonomy |
Ownership of technology Lack of desire |
aMultiple uses of this theme in the same article. See Multimedia Appendix 1 for a complete list of individual observations and their translation to themes.
bmHealth: mobile health.
Risk of Bias Across Studies and Quality Assessments
Table 3 summarizes the quality indicators identified by the JHNEBP tool [15]. The most frequent strength rating was III, followed by I, II, and IV. The most frequent evidence rating was A, followed by B and C. No strengths below IV were encountered. A full list of quality assessments is presented in Multimedia Appendix 4. Articles that did not meet the minimum standards of quality were not included in the analysis. This decision was made to limit the bias inherent to nondata-driven opinions or conclusions that do not logically follow the data.
Table 3.
Summary of quality indicators.
| Quality indicator | Value (N=57), n (%) | |
| Strength of evidence |
|
|
|
|
I (experimental study, RCTa, or meta-analysis of RCT) | 18 (32%) |
|
|
II (quasiexperimental study) | 10 (17%) |
|
|
III (nonexperimental, qualitative, or meta-synthesis study) | 28 (49%) |
|
|
IV (opinion) | 1 (2%) |
| Quality of evidence |
|
|
|
|
A (high quality) | 33 (58%) |
|
|
B (good quality) | 23 (40%) |
|
|
C (low quality or major flaws) | 1 (2%) |
aRCT: randomized controlled trial.
Additional Analysis
The results of consensus meeting three identified the themes that corresponded with telehealth interventions, barriers to the use of telehealth, and medical outcomes. These are summarized in Tables 4-6.
Table 4.
Affinity matrix for telehealth interventions.
| Intervention | References | Number of occurrences (N=62) | Probability of occurrence |
| eHealth | [5,14-16,28,30-34,36,37,40,41,46,47,50-54,58,59,62,65,66,69,73,74] | 29 | 47% |
| mHealtha | [19,27,28,35,38,39,45,48,49,60,61,64,74] | 13 | 21% |
| Telemonitoring | [26,29,44,55-57,67,72,74,75] | 10 | 16% |
| Telecare (phone) | [28,43,63,68,70] | 5 | 8% |
| Video call | [4,29,42,71,76] | 5 | 8% |
amHealth: mobile health.
Table 6.
Affinity matrix for barriers to the use of telehealth by older adults.
| Themes of barriers | References | Number of occurrences (N=144) | Probability of occurrence |
| Technical literacy | [14-16,19,27,28,34,35,37-40,46,47,49,56,58,59,63-65,75] | 25 | 17% |
| Not reported | [26,31,32,36,41-45,51-54,62,68-72] | 19 | 13% |
| Lack of desire | [19,28,34,37,38,49,57,58,60,63,64,67,74,76] | 15 | 10% |
| Cost | [33,38,40,48-50,55,58,63,64,67] | 11 | 8% |
| Lack of technical support | [14,28,34,58,63-65,73,74] | 10 | 7% |
| Visual acuity | [4,27,29,37,59,61,73] | 10 | 7% |
| Social implications | [14,28,29,49,56,58,64,66] | 9 | 6% |
| Ownership of technology | [5,19,28,34,38,58,76] | 8 | 6% |
| Privacy and security | [5,19,28,34,38,58,76] | 8 | 6% |
| Medical literacy | [5,14,15,35,38,49,56,73] | 8 | 6% |
| Trust of the internet | [5,14-16,30,58] | 6 | 4% |
| Mental acuity | [27,29,38,59,63,73] | 6 | 4% |
| Hand-eye coordination | [37,58,59,73] | 4 | 3% |
| Auditory acuity | [4,50,61] | 4 | 3% |
| Computer anxiety | [65] | 1 | 1% |
Interventions of Telehealth
Five themes for interventions were identified. Two studies used multiple telehealth interventions. Table 4 lists the interventions with the associated references, number of occurrences, and probability of occurrence in the review. The most common intervention was eHealth (computer driven), followed by mHealth (smart device driven), telemonitoring (remote sensors), telecare (phone), and telehealth video call.
Medical Outcomes and Health-Related Quality of Life Enhancers
Thirteen themes and one observation that did not correspond with a theme for medical outcomes and quality of life factors were reported. Table 5 lists the outcomes with their associated references, number of occurrences, and probability of occurrence in this review. The most common theme for medical outcomes associated with telehealth interventions was decrease in psychological distress (decrease in anxiety symptoms, decrease in depressive symptoms, decrease in embitterment, decrease in grief, decrease in worry, decrease in loneliness, increase in emotional support, and increase in mood), with 21 of 118 (18%) occurrences [32,42,46,51,60,68,70,71,76]. The theme associated with quality of life factors was listed as an increase in autonomy (increase in locus of control, increase in autonomy, increase in responsibility, increase in motivation to self-manage, and increase in independence), with 18 of 118 (15%) occurrences [29,34,35,46,48,52-54,56,62,67,75,76]. One theme was associated with an increase in cognitive ability (increase in skill ability, increase in sensory organization, increase in memory, increase in cognitive activity, and increase in reasoning), with 11 of 118 (9%) occurrences [19,20,23,32,41,42,60]. Another theme was associated with a decrease in symptoms surrounding diabetes (decrease in HbA1c, decrease in cholesterol, increase in glucose management, and increase in diabetes health), with 9 of 118 (8%) occurrences [28,36,37,51,52,66]. Another theme was associated with an increase in mindfulness of the condition (increase in medical events detected, increase in education exposure, and more awareness of danger areas for falls like outside or stairwells), with 8 of 118 (7%) occurrences [21,27,38,43,47,51,63,67]. The next theme summarized observations of an increase in the sense of safety, security, or comfort, with 7 of 118 (6%) occurrences [21,23,44,47,53]. The last set of themes comprised 25% of the observations, and they were an increase in health-related quality of life (increase in life satisfaction and increase in the feeling of being understood); increase in activity or coordination (increase in mobility, increase in activity, increase in exercise, decrease in weight, decrease in BMI, increase in balance evaluation, and increase in the feeling of stability); decrease in medical conditions surrounding pain (decrease in alcohol abuse, decrease in cannabis misuse, decrease in cannabis dependence, and decrease in pain); increase in documentation to give to the provider (documentation and communication with the provider); increase in satisfaction (satisfaction with the health care system); and increase in hospital metrics (decrease in readmissions and decrease in hospital visits). The last observation was the only negative outcome. One participant noted that the SMS text messages she received as part of an exercise RCT increased her level of guilt because she was not exercising.
Table 5.
Affinity matrix for medical outcomes and quality of life factors observed by older adults using telehealth.
| Theme or observation | References | Number of occurrences (N=118) | Probability of occurrence |
| Decrease in psychological distress | [32,42,46,51,60,68,70,71,76] | 21 | 19% |
| Increase in autonomy | [29,34,35,46,48,52-54,56,62,67,75,76] | 18 | 16% |
| Not reported | [14-16,30,33,37-40,49,55,57-59,63-65,74] | 18 | 16% |
| Increase in cognitive ability | [27,28,31,41,50,51,54,69] | 11 | 10% |
| Decrease in medical conditions surrounding diabetes | [36,45,46,60,61,75] | 9 | 8% |
| Increase in mindfulness of the condition | [29,35,47,52,56,60,72,77] | 8 | 7% |
| Increase in safety or security | [29,31,53,56,62] | 7 | 6% |
| Increase in health-related quality of life | [29,32,44,53,67,69] | 6 | 5% |
| Increase in activity or coordination | [41,52,54,60] | 6 | 5% |
| Decrease in medical conditions surrounding pain | [42,43,66] | 5 | 4% |
| Increase in documentation to give the provider | [19,47,73] | 3 | 3% |
| Increase in satisfaction | [4,5,53] | 3 | 3% |
| Increase in hospital metrics | [26] | 2 | 2% |
| Increase in guilt | [60] | 1 | 1% |
Barriers
Fourteen themes and one observation that did not fit into a theme for barriers were observed. Table 6 lists the barriers with their associated references, number of occurrences, and probability of occurrence in this review. The barrier that was reported most often was technical literacy (I do not understand technology, I cannot navigate menus, I do not know how, etc) [14-16,19,27,28,34,35,37-40,46,47,49,56,58,59,63-65,75]. The theme noted the second most often was lack of desire (laziness, I do not want to, I am too busy, etc) [19,28,34,37, 38,49,57,58,60,63,64,67,74,76]. Another theme was cost (too expensive, we live off a fixed income, etc) [33,38, 40,48-50,55,58,63,64,67]. The theme lack of technical support included the following: my friends or family are not able to help me, I do not understand the interface, etc [14,28,34,58,63-65,73,74]. The theme visual acuity included the following: fonts or icons are too small, color contrast, etc [4,27,29,37,59,61,73]. The next observation was a surprise to our reviewing team; the theme was social implications of using a telemonitoring device (I do not want to bother a first responder, I do not want a stranger coming to my house, I do not want anyone coming to my house late at night, I had a bad experience the last time I used the telemonitoring device, I do not want my neighbor to overhear me using this thing, I do not have my own email, I do not understand social media, etc) [14,28,29,49,56,58,64,66]. The next theme was ownership of technology (no phone, no computer, no internet access, etc) [5,19,28,34,38,58,76]. The last set of themes and observations comprised less than 25% of the observations, and they were privacy and security concerns, medical literacy (I do not understand terminology, I do not understand test results, etc), trust of the internet, mental acuity (computers confuse me, the interface is too complex, I cannot focus for very long, how did I get to this page? etc), hand-eye coordination (particularly with those who have Parkinson disease, but not exclusively), auditory acuity, and computer anxiety.
Interactions Between Observations
There were several interactions worth discussing. We analyzed the interactions between interventions and barriers. Ten instances of eHealth interventions were mentioned with technical literacy [14-16,30,33,37,40,58,59,65,74]. Eight instances of eHealth interventions were mentioned with lack of technical support [14,28,34,58,59,65,73,74]. There were eight instances of mHealth interventions associated with technical literacy [19,27,28,35,38,39,49,64], but these were hardly mentioned at all with lack of technical support [28,74]. The interventions of mHealth were also associated with the barrier of lack of desire. This occurred six times in the literature [28,38,39,60,64,74]. Contrary to literature on the digital divide, eHealth and mHealth were only marginally associated with ownership of technology, which occurred four [5,28,34,58] and three times [19,28,38], respectively. Commensurate with literature on generational trends, both eHealth and mHealth were associated with privacy and security concerns, which occurred four [14,15,34,35] and two times [28,64], respectively. Both eHealth and mHealth were associated with the barrier medical literacy, which occurred four [5,14,15,73] and three times [35,38,39], respectively. Surprisingly, eHealth was associated with hand-eye coordination, but mHealth was not [37,58,60,73]. Finally, eHealth was associated with lack of trust of the internet, which occurred six times in the literature [5,14-16,30,58].
We also analyzed the interactions between interventions and medical outcomes. eHealth interventions were associated with an increase in cognitive ability. This interaction occurred seven times in the literature [28,31,41,50,51,54,69].
Results Summary
This review identified 13 themes and one lone observation of medical outcomes incident with the adoption of five types of telehealth approaches. This review also identified 14 themes and one observation of barriers to the adoption of telehealth.
Discussion
Common Barriers to Telehealth
In this review, we were able to identify the common barriers associated with older adults utilizing telehealth. The most frequent barriers were lack of desire, cost, lack of technical support, visual acuity, social implications of use, ownership of technology, privacy and security, medical literacy, trust of the internet, mental acuity, hand-eye coordination, auditory acuity, and computer anxiety. Each of these barrier areas could present hurdles for elderly people dealing with telehealth and reasons to not use it. Lack of technical literacy is a large area of concern, as many elderly people have issues using computers to check email or smartphones to make telephone calls [13]. Because this is new to this population, they are also being held back from acceptance by a simple lack of wanting to do it [28,34,37-39,57,58,60,63,64,67,74,76]. It seems to be an easy thing to add to one’s daily tasks, but when one has lived largely without the use of these technologies, it can become an arduous task to “sell” the benefits of the sudden use of new technology and learning how to use new technology. They have the attitude “as it was not needed before, why bother to learn it now?” This can prove to be an uphill battle for providers who are attempting to utilize new technologies in different ways.
The cost of technology is also quite prohibitive, as computers, smartphones, and other devices cost hundreds to thousands of dollars. Those living on fixed incomes are cash strapped and may not be able to afford to purchase or use such new technologies. Not owning such technologies presents its own concerns for the provision of care. Besides cost, there are concerns in this population regarding the ability to actually utilize the modality of telehealth efficiently. Issues with visual acuity [4,27,29,37,59,61,73], mental acuity [27,29,38,59,63,73], hand-eye coordination [37,58,59,73], and auditory acuity [4,50,61] are all relevant concerns for elderly people. Many people, as they become older, experience decreases in the efficiencies of the operations of many body systems, including their senses. Many develop disease processes that can affect their mental status, vision, and hearing, and any or all of these could easily lead to problems with being able to use technology, let alone having a clear understanding of what they need to be doing with the device or even how to interact with it.
The elderly population also has relevant concerns with trust and technology, as they are one of the prime targets for abuse from their use of technology according to popular media [13,78]. This is where lack of technical support for the use of technology can become a very relevant area of concern. There is no affordable and adequate source of “technical support” to simply learn how to use devices [14,28,59,73]. This lack of knowledge and available education can be a very problematic barrier for the use of the modality of telehealth. Furthermore, problems surrounding trust of the internet [5,14-16,30,58], concerns of privacy and security [5,19,28,34,38,58,76], and even computer anxiety [65] can figure into the use of technology. As there are concerns with privacy and security, telehealth could easily cause patients to succumb to some level of anxiety. Not understanding the modality of telehealth or how to use it can add to the level of this anxiety at an exponential rate.
Another consideration with the use of telehealth is that it requires a certain level of user knowledge. The utilization of medical applications requires the user to have some knowledge of medical terms, procedures, etc [5,14,15,35,38,49,56,73]. This is often not the case, as this population was raised without the internet or medical knowledge. Medical knowledge came from physicians during their younger years, and only recently, the approach has changed to the utilization of internet web searches to garner knowledge about symptoms and diagnoses. This is an entirely new world for the elderly population and a relevant barrier to the use of these applications overall. Overcoming this knowledge gap could prove to be an insurmountable task or one that requires any telehealth use to be kept to an absolute minimum for knowledge or know-how on the part of the user.
Common Outcomes Associated With Telehealth Interventions
The research supports strong medical outcomes incident to the use of telehealth as follows: decreased psychological distress [32,42,46,51,60,68,70,71,76], increased autonomy [29,34,35,46,48,52-54,56,62,67,75,76], increased cognitive ability [27,28,31,41,50,51,54,69], and many others. This review supports an increased quality of life for those who adopt telehealth [29,32,44,53,67,69]. The use of telehealth can lead to less psychological distress, as users know that they have a way of communicating their medical concerns to their providers in a much easier and faster way. This could eventually enable better health due to better management, thus allowing for fewer associated medical conditions for those patients who use telehealth for assistance in the management of their care.
The observation of greater documentation for providers demonstrated that the use of telehealth is not all about the patient. It is just as much about practitioners providing care. The use of telehealth allows for much faster accessibility to documentation to provide care or even real-time information about the patient to allow for immediate diagnosis or intervention, based on information being gathered by the used technology. This can make the provision of care easier and much more efficient for the field, which is already seeing more patients than it can comfortably manage.
Interactions Among Outcomes, Barriers, and Types of Interventions
eHealth interventions were the most frequently observed interventions in the literature, and these interventions were most frequently associated with the barriers of technical literacy and lack of technical support. This observation is interesting because general technical support, whether from friends, neighbors, family, or caregivers, or professionally acquired technical support is a control for the barrier of technical literacy. The interaction between eHealth and technical literacy is interesting as well. This could signal that older adults are more adept at mobile technology than computer technology for application of telehealth. This supposition is supported by the literature because many older adults are turning to mobile technology to communicate with children and grandchildren [13]. The interaction between mHealth and lack of desire is noteworthy. This seems to indicate that older adults are willing to interact with mobile technology to communicate with children and grandchildren, but they are not as willing to use it for telehealth interventions.
Study Quality and Literature Bias
The assessment of the quality of the articles studied is worthy of discussion. The majority (27/57, 49%) of the articles analyzed were level III (nonexperimental, qualitative, or meta-synthesis studies). The reviewers would have preferred to analyze only the highest level (level I) (experimental study or RCT), but only 10 (17%) such studies were available. Fortunately, 98% (56/57) of the articles were rated as quality level A (high quality) or B (good quality). The importance of this rating cannot be understated. If the findings from this review were from low-quality articles, the results would not be as strong. By analyzing high-quality articles with strong levels of evidence, readers can be more assured of the results. Research articles with strong study designs and sufficiently large samples are generally accepted in the scientific field for their veracity.
Limitations
The authors identified the low number of articles analyzed as a limitation of this systematic review. If the authors conduct another systematic review on the same topic, they would like to have a larger analysis pool. This could be achieved by broadening the years of study in the selection or by reducing the threshold of quality. However, the additional years of study would only repeat the results from previously published reviews of a similar topic, and lowering the threshold of quality would introduce articles with dubious results.
Although not intentional, the authors realized that selection bias may be present in this article. To combat selection bias, the authors worked to minimize its effects by ensuring each article was reviewed by at least two authors. The authors held consensus meetings after each screening to provide feedback and reach total agreement on the inclusion and exclusion of articles for the analysis.
Another source of bias that could have affected this article is publication bias. To control for publication bias, the authors searched the Boolean search string in Google Scholar. This action was intended to identify articles from lesser-known journals that may not have appeared in MEDLINE or CINAHL.
Another limitation is our inclusion of people aged 50 years or above in the study of older adults. Most studies categorize older adults as those aged 65 years or above. The elderly population currently spans baby boomers and the silent generation. The youngest members of the former group are still working and are most likely using technology fluently. It is possible that our generalizations do not apply to all members of the elderly demographic.
Future Research
Health care systems can utilize knowledge of these barriers to develop solutions for broadening the use of telehealth among older adults. A multidisciplinary approach and culture of collaboration between administrative leadership and providers may be the most effective and immediate manner of implementing solutions to breach these barriers and strengthen the reach of health care services. However, some barriers may be out of the scope of impact, and policy makers should consider supporting the efforts. Future research should be conducted on methods for personalizing telehealth in older adults before implementation.
Conclusion
Providing sufficient health care access to the rapidly growing aging population has been an imminent issue, and telehealth is a useful tool that can provide a solution. While health care systems increase their telehealth efforts to improve access to health care services among vulnerable populations, such as older adults, some health care organizations do not consider the technological, educational, financial, and behavioral barriers before implementing telehealth solutions. It is imperative that health care systems use a multidisciplinary approach and collaborate with health care providers, community partners, and policy makers to address these barriers of utilizing telehealth among older adults and to successfully implement telehealth solutions. This systematic review provides some understanding of older adults’ perspectives and experiences with the barriers of implementing telehealth services.
Abbreviations
- JHNEBP
John Hopkins Nursing Evidence-Based Practice
- MeSH
Medical Subject Headings
- mHealth
mobile health
- RCT
randomized controlled trial
- WHO
World Health Organization
Appendix
Detailed observations on interventions and corresponding themes.
Detailed observations on medical outcomes and corresponding themes.
Detailed observations on barriers and corresponding themes.
Bias, country of origin, statistics, and quality assessments.
Footnotes
Authors' Contributions: Conceptualization: CSK, NW, JF, ENP, and SZ; methodology: CSK, NW, JF, ENP, and SZ; formal analysis: CSK, NW, JF, ENP, SZ, and MM; investigation: CSK, NW, JF ENP, and SZ; writing—original draft preparation: NW, JF, ENP, and SZ; writing—review and editing: JF; visualization: ENP; supervision: NW; project administration: SZ; final draft: CSK and MM.
Conflicts of Interest: None declared.
References
- 1.Ageing and health. World Health Organization. 2018. Feb 05, [2020-04-02]. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
- 2.From Pyramid to Pillar: A Century of Change, Population of the U.S. US Census Bureau. 2018. Mar 13, [2020-04-02]. https://www.census.gov/library/visualizations/2018/comm/century-of-change.html.
- 3.Colby S, Ortman J. The Baby Boom Cohort in the United States: 2012-2060. US Census Bureau. 2014. May 01, [2020-04-02]. https://www.census.gov/library/publications/2014/demo/p25-1141.html.
- 4.Dham P, Gupta N, Alexander J, Black W, Rajji T, Skinner E. Community based telepsychiatry service for older adults residing in a rural and remote region- utilization pattern and satisfaction among stakeholders. BMC Psychiatry. 2018 Sep 27;18(1):316. doi: 10.1186/s12888-018-1896-3. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-018-1896-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Theis S, Schäfer D, Bröhl C, Schäfer K, Rasche P, Wille M, Brandl C, Jochems N, Nitsch V, Mertens A. Predicting technology usage by health information need of older adults: Implications for eHealth technology. Work. 2019;62(3):443–457. doi: 10.3233/WOR-192878. [DOI] [PubMed] [Google Scholar]
- 6.Ryu S. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth 2009 (Global Observatory for eHealth Series, Volume 2) Healthc Inform Res. 2012;18(2):153. doi: 10.4258/hir.2012.18.2.153. [DOI] [Google Scholar]
- 7.Yoon H, Jang Y, Vaughan PW, Garcia M. Older Adults' Internet Use for Health Information: Digital Divide by Race/Ethnicity and Socioeconomic Status. J Appl Gerontol. 2020 Jan;39(1):105–110. doi: 10.1177/0733464818770772. [DOI] [PubMed] [Google Scholar]
- 8.Dorsey ER, Topol EJ. Telemedicine 2020 and the next decade. The Lancet. 2020 Mar;395(10227):859. doi: 10.1016/s0140-6736(20)30424-4. [DOI] [PubMed] [Google Scholar]
- 9.Trump Administration Issues Second Round of Sweeping Changes to Support U.S. Healthcare System During COVID-19 Pandemic. Centers for Medicare & Medicaid Services. 2020. Apr 30, [2020-04-30]. https://www.cms.gov/newsroom/press-releases/trump-administration-issues-second-round-sweeping-changes-support-us-healthcare-system-during-covid.
- 10.Foster MV, Sethares KA. Facilitators and barriers to the adoption of telehealth in older adults: an integrative review. Comput Inform Nurs. 2014 Nov;32(11):523–33; quiz 534. doi: 10.1097/CIN.0000000000000105. [DOI] [PubMed] [Google Scholar]
- 11.Kampmeijer R, Pavlova M, Tambor M, Golinowska S, Groot W. The use of e-health and m-health tools in health promotion and primary prevention among older adults: a systematic literature review. BMC Health Serv Res. 2016 Sep 05;16 Suppl 5:290. doi: 10.1186/s12913-016-1522-3. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-016-1522-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017 Aug 03;7(8):e016242. doi: 10.1136/bmjopen-2017-016242. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=28775188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kruse CS, Mileski M, Moreno J. Mobile health solutions for the aging population: A systematic narrative analysis. J Telemed Telecare. 2017 May;23(4):439–451. doi: 10.1177/1357633X16649790. [DOI] [PubMed] [Google Scholar]
- 14.Ware P, Bartlett SJ, Paré G, Symeonidis I, Tannenbaum C, Bartlett G, Poissant L, Ahmed S. Using eHealth Technologies: Interests, Preferences, and Concerns of Older Adults. Interact J Med Res. 2017 Mar 23;6(1):e3. doi: 10.2196/ijmr.4447. http://www.i-jmr.org/2017/1/e3/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rasche P, Wille M, Bröhl C, Theis S, Schäfer K, Knobe M, Mertens A. Prevalence of Health App Use Among Older Adults in Germany: National Survey. JMIR Mhealth Uhealth. 2018 Jan 23;6(1):e26. doi: 10.2196/mhealth.8619. https://mhealth.jmir.org/2018/1/e26/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paige SR, Miller MD, Krieger JL, Stellefson M, Cheong J. Electronic Health Literacy Across the Lifespan: Measurement Invariance Study. J Med Internet Res. 2018 Jul 09;20(7):e10434. doi: 10.2196/10434. https://www.jmir.org/2018/7/e10434/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Choi N. Telehealth Depression Treatments for Older Adults. ClinicalTrials.gov. 2015. Nov 09, [2020-04-02]. https://clinicaltrials.gov/ct2/show/NCT02600754.
- 18.Scogin F, Lichstein K, DiNapoli EA, Woosley J, Thomas SJ, LaRocca MA, Byers HD, Mieskowski L, Parker CP, Yang X, Parton J, McFadden A, Geyer JD. Effects of Integrated Telehealth-Delivered Cognitive-Behavioral Therapy for Depression and Insomnia in Rural Older Adults. J Psychother Integr. 2018 Sep;28(3):292–309. doi: 10.1037/int0000121. http://europepmc.org/abstract/MED/30930607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evans J, Papadopoulos A, Silvers CT, Charness N, Boot WR, Schlachta-Fairchild L, Crump C, Martinez M, Ent CB. Remote Health Monitoring for Older Adults and Those with Heart Failure: Adherence and System Usability. Telemed J E Health. 2016 Jun;22(6):480–8. doi: 10.1089/tmj.2015.0140. http://europepmc.org/abstract/MED/26540369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kruse CS. Writing a Systematic Review for Publication in a Health-Related Degree Program. JMIR Res Protoc. 2019 Oct 14;8(10):e15490. doi: 10.2196/15490. https://www.researchprotocols.org/2019/10/e15490/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009 Jul 21;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006 Jan;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 23.Dang D, Dearholt S. Johns Hopkins Nursing Evidence-based Practice: Model and Guidelines. Indianapolis, IN: SIGMA Theta Tau International; 2018. [Google Scholar]
- 24.Light RJ. Measures of response agreement for qualitative data: Some generalizations and alternatives. Psychological Bulletin. 1971;76(5):365–377. doi: 10.1037/h0031643. [DOI] [Google Scholar]
- 25.McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 2012;22(3):276–82. http://www.biochemia-medica.com/2012/22/276. [PMC free article] [PubMed] [Google Scholar]
- 26.Hamilton T, Johnson L, Quinn BT, Coppola J, Sachs D, Migliaccio J, Phipps C, Schwartz J, Capasso M, Carpenter M, Putrino D. Telehealth Intervention Programs for Seniors: An Observational Study of a Community-Embedded Health Monitoring Initiative. Telemed J E Health. 2020 Apr;26(4):438–445. doi: 10.1089/tmj.2018.0248. [DOI] [PubMed] [Google Scholar]
- 27.Wildenbos GA, Jaspers MW, Schijven MP, Dusseljee-Peute LW. Mobile health for older adult patients: Using an aging barriers framework to classify usability problems. Int J Med Inform. 2019 Apr;124:68–77. doi: 10.1016/j.ijmedinf.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 28.Jakobsson E, Nygård L, Kottorp A, Malinowsky C. Experiences from using eHealth in contact with health care among older adults with cognitive impairment. Scand J Caring Sci. 2019 Jun;33(2):380–389. doi: 10.1111/scs.12634. [DOI] [PubMed] [Google Scholar]
- 29.Karlsen C, Moe CE, Haraldstad K, Thygesen E. Caring by telecare? A hermeneutic study of experiences among older adults and their family caregivers. J Clin Nurs. 2019 Apr;28(7-8):1300–1313. doi: 10.1111/jocn.14744. [DOI] [PubMed] [Google Scholar]
- 30.Coley N, Rosenberg A, van Middelaar T, Soulier A, Barbera M, Guillemont J, Steensma J, Igier V, Eskelinen M, Soininen H, Moll van Charante E, Richard E, Kivipelto M, Andrieu S, MIND-AD. HATICE groups Older Adults' Reasons for Participating in an eHealth Prevention Trial: A Cross-Country, Mixed-Methods Comparison. J Am Med Dir Assoc. 2019 Jul;20(7):843–849.e5. doi: 10.1016/j.jamda.2018.10.019. [DOI] [PubMed] [Google Scholar]
- 31.Giesbrecht EM, Miller WC. Effect of an mHealth Wheelchair Skills Training Program for Older Adults: A Feasibility Randomized Controlled Trial. Arch Phys Med Rehabil. 2019 Nov;100(11):2159–2166. doi: 10.1016/j.apmr.2019.06.010. [DOI] [PubMed] [Google Scholar]
- 32.Brodbeck J, Berger T, Biesold N, Rockstroh F, Znoj HJ. Evaluation of a guided internet-based self-help intervention for older adults after spousal bereavement or separation/divorce: A randomised controlled trial. J Affect Disord. 2019 Jun 01;252:440–449. doi: 10.1016/j.jad.2019.04.008. [DOI] [PubMed] [Google Scholar]
- 33.Mosley CL, Langley LM, Davis A, McMahon CM, Tremblay KL. Reliability of the Home Hearing Test: Implications for Public Health. J Am Acad Audiol. 2019 Mar;30(3):208–216. doi: 10.3766/jaaa.17092. http://europepmc.org/abstract/MED/30461396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jensen CM, Overgaard S, Wiil UK, Clemensen J. Can Tele-Health Support Self-Care and Empowerment? A Qualitative Study of Hip Fracture Patients’ Experiences With Testing an “App”. SAGE Open Nursing. 2019 Feb 21;5:237796081982575. doi: 10.1177/2377960819825752. http://europepmc.org/abstract/MED/30210796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Portz JD, Vehovec A, Dolansky MA, Levin JB, Bull S, Boxer R. The Development and Acceptability of a Mobile Application for Tracking Symptoms of Heart Failure Among Older Adults. Telemed J E Health. 2018 Feb;24(2):161–165. doi: 10.1089/tmj.2017.0036. http://europepmc.org/abstract/MED/28696832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Castro Sweet CM, Chiguluri V, Gumpina R, Abbott P, Madero EN, Payne M, Happe L, Matanich R, Renda A, Prewitt T. Outcomes of a Digital Health Program With Human Coaching for Diabetes Risk Reduction in a Medicare Population. J Aging Health. 2018 Jun;30(5):692–710. doi: 10.1177/0898264316688791. http://europepmc.org/abstract/MED/28553807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Joe J, Hall A, Chi N, Thompson H, Demiris G. IT-based wellness tools for older adults: Design concepts and feedback. Inform Health Soc Care. 2018 Mar;43(2):142–158. doi: 10.1080/17538157.2017.1290637. [DOI] [PubMed] [Google Scholar]
- 38.Cajita MI, Hodgson NA, Lam KW, Yoo S, Han H. Facilitators of and Barriers to mHealth Adoption in Older Adults With Heart Failure. Comput Inform Nurs. 2018 Aug;36(8):376–382. doi: 10.1097/CIN.0000000000000442. http://europepmc.org/abstract/MED/29742549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harte R, Hall T, Glynn L, Rodríguez-Molinero A, Scharf T, Quinlan LR, ÓLaighin G. Enhancing Home Health Mobile Phone App Usability Through General Smartphone Training: Usability and Learnability Case Study. JMIR Hum Factors. 2018 Apr 26;5(2):e18. doi: 10.2196/humanfactors.7718. https://humanfactors.jmir.org/2018/2/e18/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gordon NP, Hornbrook MC. Older adults' readiness to engage with eHealth patient education and self-care resources: a cross-sectional survey. BMC Health Serv Res. 2018 Mar 27;18(1):220. doi: 10.1186/s12913-018-2986-0. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-018-2986-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bao T, Carender WJ, Kinnaird C, Barone VJ, Peethambaran G, Whitney SL, Kabeto M, Seidler RD, Sienko KH. Effects of long-term balance training with vibrotactile sensory augmentation among community-dwelling healthy older adults: a randomized preliminary study. J Neuroeng Rehabil. 2018 Jan 18;15(1):5. doi: 10.1186/s12984-017-0339-6. https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-017-0339-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Egede LE, Walker RJ, Payne EH, Knapp RG, Acierno R, Frueh BC. Effect of psychotherapy for depression via home telehealth on glycemic control in adults with type 2 diabetes: Subgroup analysis of a randomized clinical trial. J Telemed Telecare. 2018 Oct;24(9):596–602. doi: 10.1177/1357633X17730419. [DOI] [PubMed] [Google Scholar]
- 43.Platts-Mills TF, Hollowell AG, Burke GF, Zimmerman S, Dayaa JA, Quigley BR, Bush M, Weinberger M, Weaver MA. Randomized controlled pilot study of an educational video plus telecare for the early outpatient management of musculoskeletal pain among older emergency department patients. Trials. 2018 Jan 05;19(1):10. doi: 10.1186/s13063-017-2403-8. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-017-2403-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lopez-Villegas A, Catalan-Matamoros D, Lopez-Liria R, Enebakk T, Thunhaug H, Lappegård KT. Health-related quality of life on tele-monitoring for users with pacemakers 6 months after implant: the NORDLAND study, a randomized trial. BMC Geriatr. 2018 Sep 21;18(1):223. doi: 10.1186/s12877-018-0911-3. https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-018-0911-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dugas M, Crowley K, Gao GG, Xu T, Agarwal R, Kruglanski AW, Steinle N. Individual differences in regulatory mode moderate the effectiveness of a pilot mHealth trial for diabetes management among older veterans. PLoS One. 2018;13(3):e0192807. doi: 10.1371/journal.pone.0192807. http://dx.plos.org/10.1371/journal.pone.0192807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nalder E, Marziali E, Dawson DR, Murphy K. Delivering cognitive behavioural interventions in an internet-based healthcare delivery environment. British Journal of Occupational Therapy. 2018 Mar 23;81(10):591–600. doi: 10.1177/0308022618760786. [DOI] [Google Scholar]
- 47.Buck H, Pinter A, Poole E, Boehmer J, Foy A, Black S, Lloyd T. Evaluating the older adult experience of a web-based, tablet-delivered heart failure self-care program using gerontechnology principles. Geriatr Nurs. 2017;38(6):537–541. doi: 10.1016/j.gerinurse.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 48.Chang C, Lee T, Mills ME. Experience of Home Telehealth Technology in Older Patients With Diabetes. Comput Inform Nurs. 2017 Oct;35(10):530–537. doi: 10.1097/CIN.0000000000000341. [DOI] [PubMed] [Google Scholar]
- 49.Cajita MI, Hodgson NA, Budhathoki C, Han H. Intention to Use mHealth in Older Adults With Heart Failure. J Cardiovasc Nurs. 2017;32(6):E1–E7. doi: 10.1097/JCN.0000000000000401. http://europepmc.org/abstract/MED/28248747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.LaMonica HM, English A, Hickie IB, Ip J, Ireland C, West S, Shaw T, Mowszowski L, Glozier N, Duffy S, Gibson AA, Naismith SL. Examining Internet and eHealth Practices and Preferences: Survey Study of Australian Older Adults With Subjective Memory Complaints, Mild Cognitive Impairment, or Dementia. J Med Internet Res. 2017 Oct 25;19(10):e358. doi: 10.2196/jmir.7981. https://www.jmir.org/2017/10/e358/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bahar-Fuchs A, Webb S, Bartsch L, Clare L, Rebok G, Cherbuin N, Anstey KJ. Tailored and Adaptive Computerized Cognitive Training in Older Adults at Risk for Dementia: A Randomized Controlled Trial. J Alzheimers Dis. 2017;60(3):889–911. doi: 10.3233/JAD-170404. [DOI] [PubMed] [Google Scholar]
- 52.Nahm E, Resnick B, Brown C, Zhu S, Magaziner J, Bellantoni M, Brennan PF, Charters K, Brown J, Rietschel M, An M, Park BK. The Effects of an Online Theory-Based Bone Health Program for Older Adults. J Appl Gerontol. 2017 Sep;36(9):1117–1144. doi: 10.1177/0733464815617284. http://europepmc.org/abstract/MED/26675352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Knaevelsrud C, Böttche M, Pietrzak RH, Freyberger HJ, Kuwert P. Efficacy and Feasibility of a Therapist-Guided Internet-Based Intervention for Older Persons with Childhood Traumatization: A Randomized Controlled Trial. Am J Geriatr Psychiatry. 2017 Aug;25(8):878–888. doi: 10.1016/j.jagp.2017.02.024. [DOI] [PubMed] [Google Scholar]
- 54.Reijnders JS, Geusgens CA, Ponds RW, van Boxtel MP. "Keep your brain fit!" Effectiveness of a psychoeducational intervention on cognitive functioning in healthy adults: A randomised controlled trial. Neuropsychol Rehabil. 2017 Jun;27(4):455–471. doi: 10.1080/09602011.2015.1090458. [DOI] [PubMed] [Google Scholar]
- 55.Mageroski A, Alsadoon A, Prasad P, Pham L, Elchouemi A. Impact of wireless communications technologies on elder people healthcare: Smart home in Australia. 13th International Joint Conference on Compouter Science and Software Engineering (JCSSE); 2016; Khon Kaen, Thailand. 2016. pp. 1–6. [DOI] [Google Scholar]
- 56.Hamblin K, Yeandle S, Fry G. Researching telecare: the importance of context. Journal of Enabling Technologies. 2017 Sep 18;11(3):75–84. doi: 10.1108/jet-04-2017-0016. [DOI] [Google Scholar]
- 57.Wang J, Carroll D, Peck M, Myneni S, Gong Y. Mobile and Wearable Technology Needs for Aging in Place: Perspectives from Older Adults and Their Caregivers and Providers. Stud Health Technol Inform. 2016;225:486–90. [PubMed] [Google Scholar]
- 58.Gordon NP, Hornbrook MC. Differences in Access to and Preferences for Using Patient Portals and Other eHealth Technologies Based on Race, Ethnicity, and Age: A Database and Survey Study of Seniors in a Large Health Plan. J Med Internet Res. 2016 Mar 04;18(3):e50. doi: 10.2196/jmir.5105. https://www.jmir.org/2016/3/e50/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Williams K, Pennathur P, Bossen A, Gloeckner A. Adapting Telemonitoring Technology Use for Older Adults: A Pilot Study. Res Gerontol Nurs. 2016;9(1):17–23. doi: 10.3928/19404921-20150522-01. http://europepmc.org/abstract/MED/26020575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Müller AM, Khoo S, Morris T. Text Messaging for Exercise Promotion in Older Adults From an Upper-Middle-Income Country: Randomized Controlled Trial. J Med Internet Res. 2016 Jan 07;18(1):e5. doi: 10.2196/jmir.5235. https://www.jmir.org/2016/1/e5/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Quinn CC, Shardell MD, Terrin ML, Barr EA, Park D, Shaikh F, Guralnik JM, Gruber-Baldini AL. Mobile Diabetes Intervention for Glycemic Control in 45- to 64-Year-Old Persons With Type 2 Diabetes. J Appl Gerontol. 2016 Feb;35(2):227–43. doi: 10.1177/0733464814542611. [DOI] [PubMed] [Google Scholar]
- 62.Royackers A, Regan S, Donelle L. The eShift model of care: informal caregivers’ experience of a new model of home-based palliative care. Progress in Palliative Care. 2016 Apr 13;24(2):84–92. doi: 10.1179/1743291x15y.0000000006. [DOI] [Google Scholar]
- 63.Duh ES, Guna J, Pogačnik M, Sodnik J. Applications of Paper and Interactive Prototypes in Designing Telecare Services for Older Adults. J Med Syst. 2016 Apr;40(4):92. doi: 10.1007/s10916-016-0463-z. [DOI] [PubMed] [Google Scholar]
- 64.Depatie A, Bigbee JL. Rural Older Adult Readiness to Adopt Mobile Health Technology: A Descriptive Study. OJRNHC. 2015 May 29;15(1):150–184. doi: 10.14574/ojrnhc.v15i1.346. [DOI] [Google Scholar]
- 65.Moore AN, Rothpletz AM, Preminger JE. The Effect of Chronological Age on the Acceptance of Internet-Based Hearing Health Care. Am J Audiol. 2015 Sep;24(3):280–3. doi: 10.1044/2015_AJA-14-0082. [DOI] [PubMed] [Google Scholar]
- 66.Currie M, Philip LJ, Roberts A. Attitudes towards the use and acceptance of eHealth technologies: a case study of older adults living with chronic pain and implications for rural healthcare. BMC Health Serv Res. 2015 Apr 16;15:162. doi: 10.1186/s12913-015-0825-0. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-015-0825-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Grant LA, Rockwood T, Stennes L. Client Satisfaction with Telehealth in Assisted Living and Homecare. Telemed J E Health. 2015 Dec;21(12):987–91. doi: 10.1089/tmj.2014.0218. [DOI] [PubMed] [Google Scholar]
- 68.Brenes GA, Danhauer SC, Lyles MF, Hogan PE, Miller ME. Telephone-Delivered Cognitive Behavioral Therapy and Telephone-Delivered Nondirective Supportive Therapy for Rural Older Adults With Generalized Anxiety Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2015 Oct;72(10):1012–20. doi: 10.1001/jamapsychiatry.2015.1154. http://europepmc.org/abstract/MED/26244854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Corbett A, Owen A, Hampshire A, Grahn J, Stenton R, Dajani S, Burns A, Howard R, Williams N, Williams G, Ballard C. The Effect of an Online Cognitive Training Package in Healthy Older Adults: An Online Randomized Controlled Trial. J Am Med Dir Assoc. 2015 Nov 01;16(11):990–7. doi: 10.1016/j.jamda.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 70.Mavandadi S, Benson A, DiFilippo S, Streim JE, Oslin D. A Telephone-Based Program to Provide Symptom Monitoring Alone vs Symptom Monitoring Plus Care Management for Late-Life Depression and Anxiety: A Randomized Clinical Trial. JAMA Psychiatry. 2015 Dec;72(12):1211–8. doi: 10.1001/jamapsychiatry.2015.2157. [DOI] [PubMed] [Google Scholar]
- 71.Egede LE, Acierno R, Knapp RG, Lejuez C, Hernandez-Tejada M, Payne EH, Frueh BC. Psychotherapy for depression in older veterans via telemedicine: a randomised, open-label, non-inferiority trial. Lancet Psychiatry. 2015 Aug;2(8):693–701. doi: 10.1016/S2215-0366(15)00122-4. [DOI] [PubMed] [Google Scholar]
- 72.Chang W, Hou CJ, Wei S, Tsai J, Chen Y, Chen M, Chuech C, Hung C, Huang M, Lee C, Yeh H, Shih S. Utilization and Clinical Feasibility of a Handheld Remote Electrocardiography Recording Device in Cardiac Arrhythmias and Atrial Fibrillation: A Pilot Study. International Journal of Gerontology. 2015 Dec;9(4):206–210. doi: 10.1016/j.ijge.2015.06.002. [DOI] [Google Scholar]
- 73.Boulos M, Ifeachor E, Zhao P, Escudero J, Carroll C, Costa P, Doppler G, Marín LC, Spiru L, Gudmundsdottir KH, Kosem M. LiveWell-Promoting Healthy Living and Wellbeing for Parkinson Patients through Social Network and ICT Training: Lessons Learnt and Best Practices. International Journal of Healthcare Information Systems and Informatics. 2015;10(3):24–41. doi: 10.4018/IJHISI.2015070102. [DOI] [Google Scholar]
- 74.Diño MJ, de Guzman AB. Using Partial Least Squares (PLS) in Predicting Behavioral Intention for Telehealth Use among Filipino Elderly. Educational Gerontology. 2014 Jun 25;41(1):53–68. doi: 10.1080/03601277.2014.917236. [DOI] [Google Scholar]
- 75.Czaja SJ, Lee CC, Arana N, Nair SN, Sharit J. Use of a telehealth system by older adults with hypertension. J Telemed Telecare. 2014 Jun;20(4):184–191. doi: 10.1177/1357633X14533889. http://europepmc.org/abstract/MED/24803275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Choi NG, Wilson NL, Sirrianni L, Marinucci ML, Hegel MT. Acceptance of home-based telehealth problem-solving therapy for depressed, low-income homebound older adults: qualitative interviews with the participants and aging-service case managers. Gerontologist. 2014 Aug;54(4):704–13. doi: 10.1093/geront/gnt083. http://europepmc.org/abstract/MED/23929664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chi N, Demiris G. A systematic review of telehealth tools and interventions to support family caregivers. J Telemed Telecare. 2015 Jan;21(1):37–44. doi: 10.1177/1357633X14562734. http://europepmc.org/abstract/MED/25475220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Knowles B, Hanson Vl. Older Adults’ Deployment of ‘Distrust’. ACM Trans. Comput.-Hum. Interact. 2018 Sep 15;25(4):1–25. doi: 10.1145/3196490. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Detailed observations on interventions and corresponding themes.
Detailed observations on medical outcomes and corresponding themes.
Detailed observations on barriers and corresponding themes.
Bias, country of origin, statistics, and quality assessments.


