Abstract
Objectives:
The aim of this study was to evaluate depression in pancreatic cancer (PC) patients before and after a cancer diagnosis using a US-based healthcare database. We also sought to study the impact of treatment of depression in PC patients on all-cause mortality.
Methods:
Pancreatic cancer patients with comorbid depression in Explorys (1999–2019) were compared with controls using odds ratios with 95% confidence intervals. Rates of depression diagnosed within 6 months, 1 year, and 3 years before and after a PC diagnosis were recorded. Patients who developed depression after a PC diagnosis were further categorized into those treated for depression using mental health professionals (MHPs), pharmacologic treatment, or both (2015–2019).
Results:
Of the 62,450 PC patients, 10,220 (16.4%) were diagnosed with depression before PC and 8130 (13%) were diagnosed with depression after PC. Patients diagnosed with depression after PC had a significantly higher all-cause mortality than patients with PC alone (P < 0.0001). Involvement of MHP significantly improved all-cause mortality (P = 0.0041).
Conclusions:
The majority of post PC depression is diagnosed in the first 6 months after a PC diagnosis. Even though depression significantly increases PC mortality, integrating MHP in the care of PC patients with depression improves outcomes.
Keywords: depression, pancreatic cancer, integrated care, mental health professionals
INTRODUCTION
Up to 30% of cancer patients are diagnosed with clinical depression which is well above the 8% rate of depression in the general population.1,2 Whether depression is diagnosed in the period before or after a cancer diagnosis, this comorbidity is often attributed to the stress of diagnostic workup and the uncertainty of facing a potentially fatal disease.3,4 Among patients with pancreatic cancer, which has a comparatively low 5-year survival rate, understanding the burden of depression is critical to optimizing care. Although pancreatic cancer has virtually no distinctive early symptoms, it has been hypothesized that clinical depression is a potential precursor to the disease.5
Numerous studies have investigated the occurrence of common mental disorders in patients with various cancers.6,7 Although data on the relationship between depression and pancreatic cancer is limited, recent studies have shown that the prevalence of depression in pancreatic cancer patients can range between 38% and 45%.8 However, in spite of a growing research focus on the longstanding theorized relationship between depression and pancreatic cancer, evidence linking the two conditions remains sparse.
Enhancing care for pancreatic cancer patients can have a meaningfully impact on quality of life.9 The National Cancer Comprehensive Network (NCCN) guidelines recommend comprehensive care through a multidisciplinary pancreatic cancer conference (MDPC), in which healthcare providers from gastroenterology, oncology, and radiology come together to form a treatment plan for each patient case.10 Although this approach has proven effective in the diagnosis and management of pancreatic cancer, with shorter times from diagnosis to surgery and greater success in predicting resectability, the impact of integrating a mental health professional into pancreatic cancer patient care has yet to be adequately described in the literature.11 The primary aim of the present study was to determine the burden of depression in pancreatic cancer patients preceding and following cancer diagnosis using a large, US-based healthcare database. The secondary aim was to investigate the impact of integrating mental health professionals into the care of pancreatic cancer patients on all-cause mortality.
MATERIALS AND METHODS
Database
We used a population-based database called Explorys (Explorys Inc, Cleveland, Ohio) to conduct a longitudinal analysis. Started in 1999, Explorys hosts a collection of electronic health records (EHRs) from 26 major integrated health systems over all 50 states, including data from all four United States census regions. Explorys contains aggregated patient health data provided by participating institutions and utilizes a health data gateway server behind the firewall of each participating healthcare organization, collecting de-identified data from various health information systems. Patient diagnoses, procedures, and observations are mapped into Systematized Nomenclature of Medicine-Clinical Terms (SNOMED-CT) and are thus searchable through desired queries. Data aggregation by Explorys meets the compliance standards of the Health Insurance Portability and Accountability Act (HIPAA) and is thus institutional review board (IRB) exempt. Due to the nature of data aggregation, the Explorys database does not report sample sizes less than 10 and rounds dataset points to the nearest 10 patients.
Patient Inclusion and Search Criteria
At the time of data collection, EHRs of over 65 million patients and 300,000 providers, spanning over 360 hospital systems nationally were in this private cloud-based platform. The baseline population included all patients in the database from 1999–2019. An initial search using the terms “malignant tumor of the pancreas” and “depressive disorder” was conducted to identify patients with pancreatic cancer and comorbid depression (SNOMED CT and International Classification of Diseases, ICD 10 codes are linked in Supplementary Table 1). In order to explore the temporal relationship between pancreatic cancer and clinical depression, patients were then categorized into two groups: 1) patients with a diagnosis of a depressive disorder that preceded pancreatic cancer, and 2) those that were diagnosed with a depressive disorder after a pancreatic cancer diagnosis. Data from these two cohorts were compared with their respective control groups. For the cohort that developed pre-pancreatic cancer depression, a control group of patients who were diagnosed with depression alone using the search term “depressive disorder” was established. For the cohort that developed post-pancreatic cancer depression, an additional control group of patients who were diagnosed with pancreatic cancer but not clinical depression, using the search term “malignant tumor of the pancreas” was established.
For the primary outcome measure, rates of depression diagnoses within 6 months, 1 year, and 3 years both before and after a pancreatic cancer diagnosis were recorded. Demographic data from these groups, including sex, age, race, and all-cause mortality were also noted. In addition, associated symptoms of psychiatric or physical symptoms such as anxiety, sleep disorders, agitation, suicidal thoughts, weight loss, and fatigue were documented.
For the secondary outcome measure, all patients with a pancreatic cancer diagnosis and subsequent diagnosis of depression were further categorized into those who were treated for their depression via referral to a mental health professional, pharmacologic treatment, or both. A number of new studies have shown that in recent years there has been an increase in outpatient mental health treatment in US adults and adolescents.12,13 With this emerging data in mind we limited the search interval for the cohort of patients who were treated for their post pancreatic cancer depression with a mental health professional, pharmacologic treatment, or both to the preceding 5 years only (September 2015-September 2019).
Statistical Analysis
Demographics, comorbidities, and associated findings were compared to control cohorts of patients using odds ratio (OR) with 95% confidence intervals (CI). P values were determined using chi-squared testing using the GraphPad Prism software (version 8 for Windows, La Jolla, Calif) and STATA (Version 15, College Station, Texas). A P value of <0.05 was considered statistically significant.
RESULTS
A total of 18,350 patients were identified with pancreatic cancer and comorbid depression. In the control groups, 5,512,400 patients had depression alone and 62,450 patients had pancreatic cancer alone. Among patients with pancreatic cancer and depression, 10,220 (16.4%) were diagnosed with depression before a diagnosis of pancreatic cancer and 8130 (13%) were diagnosed with depression after a diagnosis of pancreatic cancer had been made. Among patients diagnosed with post-pancreatic cancer depression, 1790 were noted as having a mental health referral and 1560 were noted as both having a mental health referral and were treated with antidepressants.
Depression Preceding Pancreatic Cancer
We identified 10,220 patients who were diagnosed with depression in the period before a pancreatic cancer diagnosis (Table 1). Several factors were associated with patients who developed pre-pancreatic cancer depression versus those who had depression alone: male sex (OR, 1.44; 95% CI, 1.38–1.50; P < 0.0001), Caucasians. (OR, 1.21; 95% CI, 1.15–1.27; P < 0.0001), and age 65+ (OR, 4.47; 95% CI, 4.29–4.66; P < 0.0001). Interestingly, although a higher rate of male patients with depression developed pancreatic cancer than female patients with depression, the absolute number of female patients who developed pre-pancreatic cancer depression was significantly higher than the absolute number of male patients (59.3% females vs 40.7% males; P < 0.0001).
TABLE 1.
Depression Diagnosis a Preceding Diagnosis of Pancreatic Cancer
| Diagnosis of Depression Preceding Diagnosis of PC N = 10,220 |
Depression Diagnosis Without Subsequent PC (Control) N = 5,512,400 |
OR (95% CI) | P | |
|---|---|---|---|---|
| Sex, n (%) | ||||
| Male | 4160 (40.7) | 1,781,850 (32.3) | 1.44 (1.3–1.50) | <0.0001 |
| Female | 6060 (59.3) | 3,729,740 (67.7) | 0.70 (0.67–0.72) | <0.0001 |
| Race, n (%) | ||||
| White | 8420 (82.4) | 4,379,100 (79.4) | 1.21 (1.15–1.27) | <0.0001 |
| African American | 1220 (11.9) | 572,690 (10.4) | 1.17 (1.10–1.24) | <0.0001 |
| Hispanic | 90 (0.9) | 46,400 (0.8) | 1.05 (0.85–1.29) | 0.67 |
| Age, n (%) | ||||
| 18–65 | 3480 (34.1) | 3,776,850 (68.5) | 0.24 (0.23–0.25) | <0.0001 |
| >65 | 6710 (65.7) | 1,651,030 (30.0) | 4.47 (4.29–4.66) | <0.0001 |
| Findings, n (%) | ||||
| Anxiety | 4740 (46.4) | 2,319,930 (42.1) | 1.19 (1.15–1.24) | <0.0001 |
| Sleep disorder | 4230 (41.4) | 1,719,030 (31.2) | 1.56 (1.50–1.62) | <0.0001 |
| Agitation | 170 (1.7) | 46,300 (0.8) | 2.00 (1.72–2.33) | <0.0001 |
| Suicidal thoughts | 520 (5.1) | 441,300 (8.0) | 0.61 (0.56–0.67) | <0.0001 |
| Weight loss | 3270 (32.0) | 373,890 (6.8) | 6.49 (6.22–6.76) | <0.0001 |
| Fatigue | 4950 (48.4) | 1,529,270 (27.7) | 2.45 (2.35–2.54) | <0.0001 |
CI indicates confidence intervals; OR, odds ratio; PC, pancreatic cancer.
Additionally, we investigated potential symptoms of psychiatric conditions that might present in patients developing cancer. Comorbid conditions more likely to be seen in depressed patients with subsequent pancreatic cancer included: anxiety (OR, 1.19; 95% CI, 1.15–1.24; P < 0.0001), sleep disorder (OR, 1.56; 95% CI, 1.50–1.62; P < 0.0001), agitation (OR, 2.00; 95% CI, 1.72–2.33; P < 0.0001), weight loss (OR, 6.49; 95% CI, 6.22–6.76; P < 0.0001), and fatigue (OR, 2.45; 95% CI, 2.35–2.54; P < 0.0001).
Depression Following Pancreatic Cancer
A total of 8130 patients were identified with pancreatic cancer and a subsequent diagnosis of depressive disorder (Table 2). Among this group, female patients were more likely to become depressed than male patients (OR, 1.53; 95% CI, 0.73–1.60; P < 0.0001). Consistent with the results of the analysis of patients with pre-pancreatic cancer depression, the absolute number of female patients with post-pancreatic cancer depression was significantly higher than that of male patients (56.9% vs 42.9%; P < 0.0001). Further, depression following a post-pancreatic cancer diagnosis was more common among Caucasians (OR, 1.79; 95% CI, 1.69–2.99; P < 0.0001) and patients aged 18–65 (OR, 1.41; 95% CI, 0.67–1.48; P < 0.0001). Importantly, patients who developed depression following pancreatic cancer had a higher all-cause mortality than pancreatic cancer patients who did not have depression (P < 0.0001).
TABLE 2.
Depression Diagnosis Following a Diagnosis of Pancreatic Cancer
| Diagnosis of PC With Subsequent Diagnosis of a Depressive Disorder N = 8130 |
Diagnosis of PC Without Subsequent Depression (Control) N = 48,650 |
OR (95% CI) | P | |
|---|---|---|---|---|
| Sex, n (%) | ||||
| Male | 3490 (42.9) | 26,080 (53.6) | 0.65 (0.31–0.68) | <0.0001 |
| Female | 4630 (56.9) | 22,560 (46.4) | 1.53 (0.73–1.60) | <0.0001 |
| Race, n (%) | ||||
| White | 6730 (82.8) | 35,410 (72.8) | 1.79 (1.69–2.99) | <0.0001 |
| African American | 900 (11.1) | 6210 (12.8) | 0.85 (0.79–0.97) | <0.0001 |
| Hispanic | 90 (1.1) | 1120 (2.3) | 0.47 (0.38–0.59) | <0.0001 |
| Age, n (%) | ||||
| 18–65 | 2860 (35.2) | 13,540 (27.8) | 1.41 (0.67–1.48) | <0.0001 |
| >65 | 5250 (64.6) | 34,710 (71.3) | 0.73 (0.35–0.77) | <0.0001 |
| All-cause mortality, n (%) | 3360 (41.3) | 18,130 (37.3) | 1.18 (1.13–1.24) | <0.0001 |
CI indicates confidence intervals; OR, odds ratio; PC, pancreatic cancer.
Temporal Relationship Between Depression and Pancreatic Cancer
In the cohort of patients who were diagnosed with depression before pancreatic cancer (n = 10,220), over 70% of depression diagnoses occurred within 6 months before pancreatic cancer (Fig. 1). In the cohort of patients who were diagnosed with depression after pancreatic cancer (n = 8130), the vast majority of depression diagnoses (80.0%) occurred within 6 months after pancreatic cancer, with depression rates falling sharply after 1 year of pancreatic cancer diagnoses. To further compare this data with that of other cancers, we investigated the rates of depression following breast, prostate, lung, and colorectal cancer diagnoses. Among patients who did develop depression after any type of cancer, cases diagnosed within 6 months after cancer diagnoses occurred at significantly higher rates in pancreatic cancer (80.0%) than in breast (50.6%), prostate (52.3%), lung (49.9%), and colorectal (34.1%) (P < 0.0001) cancers.
FIGURE 1.
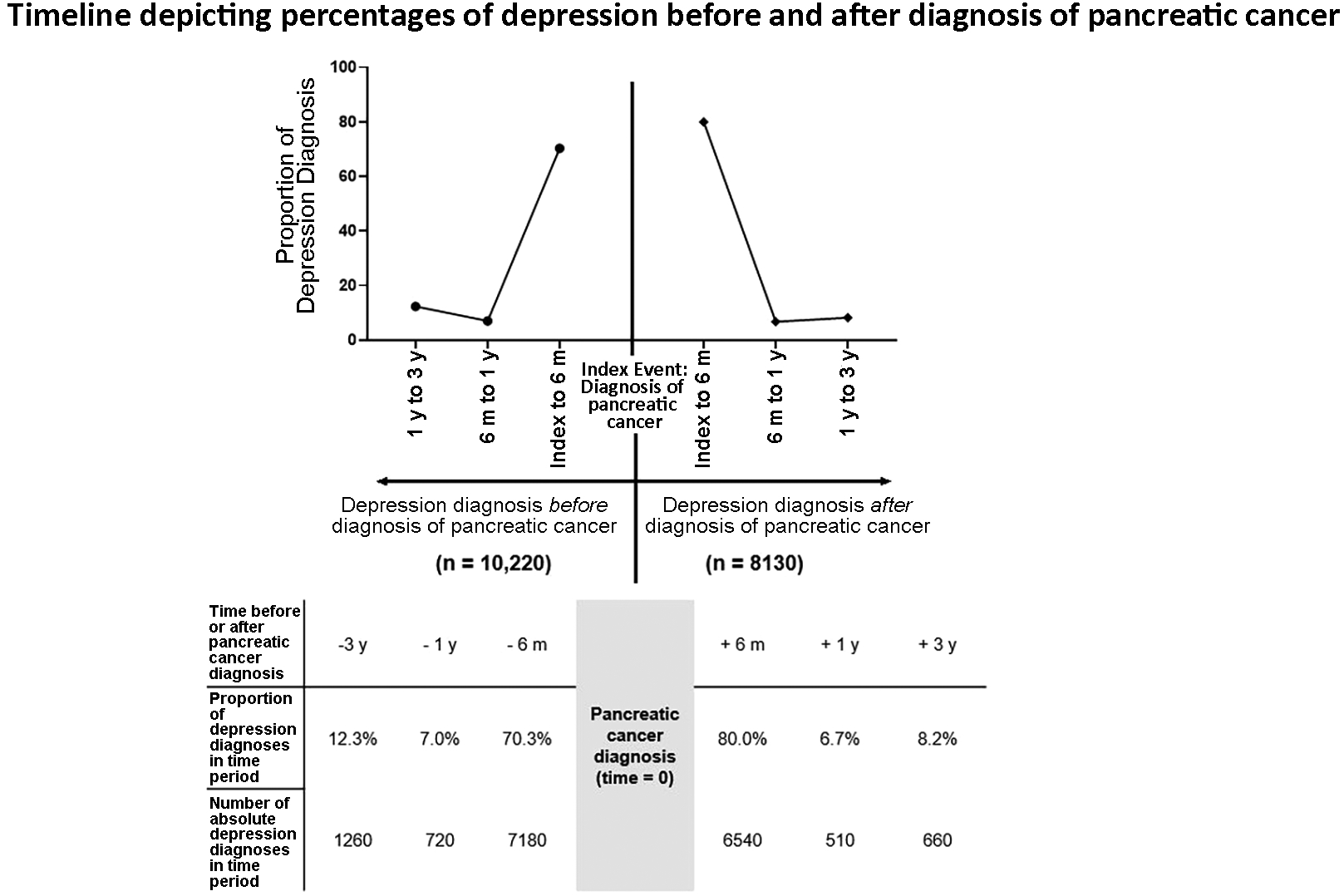
Timeline showing the proportion of depression diagnoses before and after a diagnosis of pancreatic cancer had been made.
The Role of Mental Health Providers
The impact of mental health providers and treatment with antidepressants in patients with PC was further evaluated (Table 3). During the study period, patients diagnosed with post-pancreatic cancer depression who were referred to a mental health professional had significantly lower all-cause mortality than patients who were not (36.9% vs 41.3%, P = 0.0006). Treatment of pancreatic cancer patients with depression via a combination of contact with a mental health professional and antidepressant therapy improved mortality as well (37.8% vs 41.3%; P < 0.0001). Interestingly, patients treated with only a mental health referral had similar all-cause mortality rate compared to patients treated with both a mental health referral and antidepressants (36.9% vs 37.8%, respectively; P = 0.5912).
TABLE 3.
Impact of Mental Health Providers and Treatment of Depression in Pancreatic Cancer Patients on Mortality
| A. PC With Subsequent Depression Diagnosis N = 8130 |
B. PC With Subsequent Depression Diagnosis and MHR N = 1790 |
C. PC With Subsequent Depression Diagnosis and Treatment With AD N= 6900 |
D. PC With Subsequent Depression Diagnosis and MHR and Treatment With AD N = 1560 |
P* | P† | |
|---|---|---|---|---|---|---|
| Sex, n (%) | ||||||
| Male | 3490 (42.9) | 770 (43.0) | 2770 (40.1) | 660 (42.3) | 0.9383 | 0.6829 |
| Female | 4630 (56.9) | 1020 (57.0) | 4120 (59.7) | 900 (57.7) | 0.9384 | 0.6829 |
| Race, n (%) | ||||||
| White | 6730 (82.8) | 1430 (79.9) | 5950 (86.2) | 1250 (80.1) | 0.0036 | 0.8853 |
| African American | 900 (11.1) | 320 (17.9) | 740 (10.7) | 270 (17.3) | <0.0001 | 0.6494 |
| Hispanic | 90 (1.1) | 10 (0.55) | 70 (1.0) | 10 (0.64) | 0.0554 | 0.7321 |
| Age, n (%) | ||||||
| 18–65 | 2860 (35.2) | 840 (46.9) | 2440 (35.4) | 740 (47.4) | <0.0001 | 0.7725 |
| >65 | 5250 (64.6) | 940 (52.5) | 4450 (64.5) | 820 (52.6) | <0.0001 | 0.9539 |
| All-cause mortality, n (%) | 3360 (41.3) | 660 (36.9) | 2700 (39.1) | 590 (37.8) | 0.0006 | 0.5912 |
P value comparing cohort (A) vs. (B).
P value comparing cohort (B) vs (D).
AD indicates antidepressants; MHR, mental health referral; PC, pancreatic cancer.
DISCUSSION
To our knowledge, this is the largest study conducted in the US that evaluates rates of depression both before and after a diagnosis of pancreatic cancer. Although it is well-established that there is a significant risk for cancer patients to develop depression after their diagnosis or during the course of disease, mental health disorders in cancer patients of all types continue to be underdiagnosed and are often left untreated.14,15 Several studies have investigated the occurrence of common mental disorders in cancer patients, but few to date have honed in on the relationship between depression and pancreatic cancer.6,16,17 We found that rates of depression diagnosis following a cancer diagnosis are highest in pancreatic cancer compared to other cancer types, with the rate of depression diagnosis peaking within 6 months before or after a pancreatic cancer diagnosis. Importantly, although depression significantly increases mortality in pancreatic cancer, our findings suggest that the implementation of a mental health professional into the care team of a pancreatic cancer patient can significantly improve mortality.
Our study reported depression in as many as 21% of pancreatic cancer patients prior to their cancer diagnosis. Our findings support a longstanding hypothesis that depression is a potential antecedent to pancreatic cancer, with studies as far back as 1931 describing anxiety and depression as early manifestations of the disease. Consistent with our findings and others, a recent literature review showed that as many as 45% of pancreatic cancer patients developed depressive symptoms before their cancer diagnosis.8 Another study showed that 16% of patients reported depressive symptoms up to a year before their pancreatic cancer diagnosis.19 Although these observations lend support to the view that clinical depression could be an early sign of pancreatic cancer, more data is needed to characterize this relationship.
This was the first study to show that the integration of a mental health professional into the treatment plan of pancreatic cancer patients significantly decreased all-cause mortality rates compared to patients who were not treated by a mental health professional. We also found that the majority of these patients received a clinical depression diagnosis within a year either before or after receiving a pancreatic cancer diagnosis. We hypothesize this is likely a synergistic effect of the diagnostic work up process as well as the decreased quality of life with the onset of nonspecific, syndromic symptoms that occur with a developing pancreatic cancer.
In patients with other conditions such as chronic pain, implementing mental health professionals as part of a multidisciplinary approach has been shown to improve the prognosis of somatic and psychiatric symptoms.20 However, there is little evidence to support that involving mental health professionals in the care of pancreatic cancer patients benefits overall survival. A study conducted by Boyd et al. noted that integrating mental health specialists into patient care once depressive symptoms have been identified could meaningfully enhance quality of life; however, it was concluded that this therapy is unlikely to significantly improve overall survival.9 An older review by Passik et al described the potential role a psycho-oncologist can play in the treatment of pancreatic cancer patients but it does not report the impact or effectiveness of integrating mental health providers into care.21 The present study, however, further validates the multidisciplinary approach, showing that the cohort of patients referred to mental health professionals with comparable mortality to pancreatic cancer patients without depression. Interestingly, pharmacological treatment of pancreatic cancer patients with depression did not have a significant impact on all-cause mortality. Therefore, it is possible that integrating a mental health professional into the care of pancreatic cancer patients has a greater impact on mortality and quality of life than any other depression treatment.
Ultimately, in spite of the disappointing survival rates in pancreatic cancer, optimizing care for pancreatic cancer patients can significantly enhance their quality of life.22 Our study showed that in the past 5 years, the integration of a mental health professional in the treatment plan of pancreatic cancer patients with associated depression significantly decreased all-cause mortality rates compared to patients who were not treated by a mental health professional, the first study to report this finding. Interestingly, in that same time period, patients with post pancreatic cancer and depression who were referred to mental health professionals showed a comparable mortality to pancreatic cancer patients without depression. Furthermore, pharmacological treatment of pancreatic cancer patients with depression did not seem to have a large effect on all-cause mortality and suggests that treating these patients by integrating a mental health provider has the most impact on mortality and quality of life.
There are several limitations to this study that should be addressed. Explorys is unable to present complete records for patients, which prevents multivariable analysis, such as understanding the etiology of depression, assessing severity of depression, assessing changes to patient lab values, and assessing survival as a function of time. Moreover, the diagnosis of depression and pancreatic cancer is based on SNOMED-CT diagnosis rather than chart review and diagnosis could not be validated because patient information is de-identified. The lack of chart review and access to patient-level data prevented our study from assessing factors such as quality of life, geographical location, socioeconomic status, histology, and effect of treatment of depression on mortality. Explorys relies on physician-reported data for search criteria, which can introduce additional biases. Moreover, Explorys incorporates hundreds of hospital systems, each of which uniquely denotes interventions, treatments, medications, presentations, procedures, in their EHRs. This may have caused discrepancies and misclassifications in some of the data presented in this study. Despite these limitations, most of these potential biases are mitigated by the large sample size and patient population. As the database collects data from all four United States census locations, generalizability to different geographical areas and patient populations is valid. A number of recent studies in various fields such as gastroenterology, hematology, and gynecology have been successfully conducted and published using Explorys, helping to validate its platform for population-level analyses.23–25
In conclusion, a diagnosis of depression is a common occurrence both before and after a diagnosis of pancreatic cancer. These findings suggest that depression is potentially a symptom of pancreatic cancer. Clinicians therefore should have a heightened awareness of signs and symptoms of a mental health disorder during diagnostic workup and disease management. Further, the results of this study suggest that involvement of a mental health professional in the treatment of pancreatic cancer patients with depression can improve all-cause mortality and is an important facet of a multidisciplinary approach to care.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the Explorys Database and IBM for providing the data.
Funding: This study was supported by the National Institutes of Health grant T32GM008208 to NC.
Footnotes
Competing Interests: All authors have nothing to disclose and have no conflicts of interest.
REFERENCES
- 1.Burke MA RC, Miller AH. Depression in cancer: pathophysiology at the mind-body interface In: Cleeland CS FM, Dunn AJ, ed. Cancer Symptom Science: Measurement, Mechanisms, and Management. Cambridge, UK: Cambridge University Press; 2010:70–80. [Google Scholar]
- 2.Brody DJ, Pratt LA, Hughes JP. Prevalence of depression among adults aged 20 and over: United States, 2013–2016. NCHS Data Brief. 2018:1–8. [PubMed] [Google Scholar]
- 3.Awsare NS, Green JS, Aldwinckle B, et al. The measurement of psychological distress in men being investigated for the presence of prostate cancer. Prostate Cancer Prostatic Dis. 2008;11:384–389. [DOI] [PubMed] [Google Scholar]
- 4.Brett J, Bankhead C, Henderson B, et al. The psychological impact of mammographic screening. A systematic review. Psychooncology. 2005;14:917–938. [DOI] [PubMed] [Google Scholar]
- 5.Kenner BJ. Early detection of pancreatic cancer: the role of depression and anxiety as a precursor for disease. Pancreas. 2018;47:363–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lu D, Andersson TM, Fall K, et al. Clinical diagnosis of mental disorders immediately before and after cancer diagnosis: a nationwide matched cohort study in Sweden. JAMA Oncol. 2016;2:1188–1196. [DOI] [PubMed] [Google Scholar]
- 7.Anguiano L, Mayer DK, Piven ML, et al. A literature review of suicide in cancer patients. Cancer Nurs. 2012;35:E14–26. [DOI] [PubMed] [Google Scholar]
- 8.Cosci F, Fava GA, Sonino N. Mood and anxiety disorders as early manifestations of medical illness: a systematic review. Psychother Psychosom. 2015;84:22–29. [DOI] [PubMed] [Google Scholar]
- 9.Boyd CA, Benarroch-Gampel J, Sheffield KM, H et al. The effect of depression on stage at diagnosis, treatment, and survival in pancreatic adenocarcinoma. Surgery. 2012;152:403–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tempero MA. NCCN guidelines updates: pancreatic cancer. J Natl Compr Canc Netw. 2019;17:603–605. [DOI] [PubMed] [Google Scholar]
- 11.Rao B, Syed A, Singh S, et al. Performance of a multidisciplinary pancreatic cancer conference in predicting and managing resectable pancreatic cancer. Pancreas. 2019;48:80–84. [DOI] [PubMed] [Google Scholar]
- 12.Olfson M, Wang S, Wall M, et al. Trends in serious psychological distress and outpatient mental health care of US adults. JAMA Psychiatry. 2019;76:152–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olfson M, Druss BG, Marcus SC. Trends in mental health care among children and adolescents. N Engl J Med. 2015;372:2029–2038. [DOI] [PubMed] [Google Scholar]
- 14.Mayr M, Schmid RM. Pancreatic cancer and depression: myth and truth. BMC Cancer. 2010;10:569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dauchy S, Dolbeault S, Reich M. Depression in cancer patients. EJC Suppl. 2013;11:205–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12:160–174. [DOI] [PubMed] [Google Scholar]
- 17.Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004:57–71. [DOI] [PubMed] [Google Scholar]
- 18.Yaskin JC. Nervous Symptoms As earliest manifestations of carcinoma of the pancreas. JAMA. Oncol 1931;96:1664–1668. [Google Scholar]
- 19.Olson SH, Xu Y, Herzog K, et al. Weight loss, diabetes, fatigue, and depression preceding pancreatic cancer. Pancreas. 2016;45:986–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dobscha SK, Corson K, Perrin NA, et al. Collaborative care for chronic pain in primary care: a cluster randomized trial. JAMA. 2009;301:1242–1252. [DOI] [PubMed] [Google Scholar]
- 21.Passik SD. Supportive care of the patient with pancreatic cancer: role of the psycho-oncologist. Oncology (Williston Park). 1996;10:33–34. [PubMed] [Google Scholar]
- 22.Barnes AF, Yeo TP, Leiby B, et al. Pancreatic cancer-associated depression: a case report and review of the literature. Pancreas. 2018;47:1065–1077. [DOI] [PubMed] [Google Scholar]
- 23.Yurteri-Kaplan LA, Mete MM, St Clair C, et al. Practice patterns of general gynecologic surgeons versus gynecologic subspecialists for concomitant apical suspension during vaginal hysterectomy for uterovaginal prolapse. South Med J. 2015;108:17–22. [DOI] [PubMed] [Google Scholar]
- 24.Syed A, Maradey-Romero C, Fass R. The relationship between eosinophilic esophagitis and esophageal cancer. Dis Esophagus. 2017;30:1–5. [DOI] [PubMed] [Google Scholar]
- 25.Kaelber DC, Foster W, Gilder J, et al. Patient characteristics associated with venous thromboembolic events: a cohort study using pooled electronic health record data. J Am Med Inform Assoc. 2012;19:965–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


