Abstract
Introduction
Shoulder arthroplasty rates are increasing in the UK. No data have been published from a UK centre on predictors of length of inpatient stay following shoulder arthroplasty. This study analyses the length of inpatient stay following shoulder arthroplasty in a high-volume UK centre and identifies predictors of prolonged inpatient stay.
Materials and methods
All shoulder arthroplasty cases performed between 2012 and 2018 were identified. A review of case notes and electronic patient records was completed to identify demographic data, Charlson comorbidity score, length of inpatient stay and factors associated with length of stay. Multiple linear regression analysis was conducted to determine which factors were independently associated with length of inpatient stay.
Results
A total of 640 shoulder arthroplasty cases were performed in 566 patients. Median length of stay was two days. Length of stay was predicted by age, sex, chronic kidney disease, congestive cardiac failure, previous myocardial infarction, intraoperative complication and postoperative transfusion.
Discussion
Increasing age, female sex, chronic kidney disease, congestive cardiac failure, previous myocardial infarction, intraoperative complication and transfusion were independent predictors of increased length of stay. Strategies to reduce perioperative complication and transfusion, and to optimise renal and cardiac comorbidities may reduce overall length of stay for shoulder arthroplasty patients.
Keywords: Arthroplasties, shoulder replacement; Treatment outcome; Length of stay
Introduction
Rates of primary shoulder arthroplasty have consistently risen year on year over the last decade. In the UK, the National Joint Registry (NJR) for England and Wales began recording shoulder arthroplasty cases in April 2012 and Northern Ireland and the Isle of Man joined in February 2013 and July 2015, respectively.1 Some 6,526 cases were performed in 2017, which represents a 5.6-fold increase in annual rates of shoulder arthroplasty over the past 20 years.1,2
While it is positive that an increasing number of patients have access to the beneficial shoulder specific and overall lifestyle effects of arthroplasty for end-stage glenohumeral arthropathies,3–5 the rise in demand confers a significant increase in the burden on healthcare resources. In the UK, the NHS has recently experienced a period of unprecedented rising demand with below inflation funding leading to a provider sector deficit of £960 million in 2017/18.6 This has led to increased scrutiny on resource allocation, with elective orthopaedic procedures commonly targeted for healthcare cost savings. In addition to this funding shortfall, seasonal peaks in demand have consistently led to bed shortages and cancellation of elective surgery over the winter months.7 It is therefore vital for any unit offering shoulder arthroplasty to understand the implications of providing shoulder arthroplasty on the use of inpatient beds.
The increased use of shoulder arthroplasty has led to increased scrutiny of the outcomes of these procedures, Craig et al reported higher than previously estimated rates of lifetime revision, particularly in young men, and serious adverse events within 90 days of surgery in a study of 58,054 shoulder arthroplasty procedures performed between 1998 and 2017.2 In the United States, several papers have evaluated the length of stay following shoulder arthroplasty and identified predictors of increased length of stay. Dunn et al analysed 2,004 patients undergoing primary elective total shoulder arthroplasty reporting a mean length of stay of 2.2 days and identifying age, female sex, renal insufficiency and American Society of Anesthesiologists (ASA) grade of 3 or above as predictive of increased length of stay.8 In a further study, Menendez et al analysed 40,869 patients who underwent elective total shoulder arthroplasty, they also identified age, female sex and renal failure as associated with increased length of stay. In addition, they reported that chronic obstructive pulmonary disease, preoperative anaemia and low-volume centres were associated with prolonged inpatient stay.9
To date, there has been no study of patient and surgical factors associated with increased length of inpatient stay following shoulder arthroplasty in the UK. This study aims to address this evidence gap by reporting the length of inpatient stay following shoulder arthroplasty in a high-volume UK centre and identify factors associated with greater increasing length of stay.
Materials and methods
A consecutive series of shoulder arthroplasties was identified, performed at the host institution, a tertiary referral upper limb unit, between January 2012 and January 2018. Patients were included if they underwent any form of shoulder arthroplasty, including anatomical total shoulder replacement, reverse total shoulder replacement, hemiarthroplasty and revision procedures for all indications. Patients were excluded if they did not receive a shoulder arthroplasty procedure, no cases were excluded for incomplete data. A review of case notes, electronic patient record, operation notes, anaesthetic charts and discharge summaries was conducted to collect patient demographic data, comorbidities, details of inpatient stay and date of death. Length of stay was defined as the number of nights spent in an acute inpatient bed. The Charlson Comorbidity Index, a validated scoring system used to predict mortality based on a patient’s comorbidities was calculated for each patient.10
This study was performed under the jurisdiction of the Health Research Authority and their decision-making tool indicates that ethical approval is not required for the current study or study design.
Statistical methods
Descriptive statistical analysis was carried out using Microsoft Excel. Multiple linear regression analysis was performed using GraphPad InStat and Prism. Significance was determined when the p-value is less than 0.05.
In the multiple linear regression model, independent variables included were age, sex, ASA grade (1–2, 3–4), Charlson Comorbidity Index, comorbidities (diabetes, liver failure, malignancy, chronic kidney disease, congestive cardiac failure, myocardial infarction, chronic obstructive pulmonary disease (COPD), peripheral vascular disease, cerebrovascular accident, connective tissue disorder and peptic ulcer), trauma or elective surgery, primary or revision surgery, indication for primary surgery (osteoarthritis, cuff-tear arthropathy, other), year of surgery (2011–14, 2015–17), type of shoulder arthroplasty (hemiarthroplasty, anatomical total shoulder replacement, reverse geometry shoulder replacement), side of operation, hand dominance, anaesthesia (general or general plus regional block), operating surgeon grade (consultant or training grade), previous surgery (arthroscopic surgery, arthroplasty surgery, open reduction internal fixation), fixation of humeral component (cemented or uncemented), intraoperative complication and postoperative transfusion. Comorbidities of AIDS, dementia and hemiplegia were excluded as there were no cases. Multicollinearity was assessed and addressed where it was a problem (R2 > 0.75); it was addressed either by grouping variables as described above (eg ASA grade and year of surgery) or removal of variables from the model (eg day of the week of surgery) until it was no longer a problem (R2 < 0.75 for all variables).
Results
During the study period, 640 shoulder arthroplasty cases were performed in 566 patients. The mean age at the time of surgery was 72 years (standard deviation, SD, ± 10), 451 cases (70%) were performed in female patients. The most common procedure was primary reverse total shoulder replacement (287 cases; 45%) followed by primary anatomical total shoulder replacement (262 cases; 41%) and hemiarthroplasty (36 cases; 6%), 55 revision procedures were undertaken. Of the cases performed 569 (89%) were elective cases, with 71 (11%) due to trauma. The most common indication was osteoarthritis (289 cases, 45%), followed by rotator cuff arthropathy (160 cases; 25%). Demographic details broken down by length of stay for all patients included are provided in Table 1 for illustration of trends
Table 1.
Patient demographic data.
| Demographic | All patients | Length of stay | ||
|---|---|---|---|---|
| < 3 days | 3–7 days | > 7 days | ||
| Patients (n) | 640 | 348 | 210 | 82 |
| Age (years): | ||||
| Mean (SD) | 72 (± 10) | 70 (± 10) | 73 (± 9) | 77 (± 9) |
| Minimum | 24 | 24 | 31 | 42 |
| Maximum | 95 | 89 | 95 | 93 |
| Sex (n): | ||||
| Male | 189 | 129 | 45 | 15 |
| Female | 451 | 219 | 165 | 67 |
| ASA grade: | ||||
| 1 | 52 | 40 | 12 | 0 |
| 2 | 314 | 197 | 95 | 22 |
| 3 | 265 | 109 | 101 | 55 |
| 4 | 9 | 2 | 2 | 5 |
| Median Charlson Comorbidity Index (IQR) | 3 (2–4) | 3 (2–4) | 4 (3–5) | 4 (4–5) |
| Procedure: | ||||
| Anatomical | 262 | 178 | 72 | 12 |
| Reverse | 287 | 125 | 108 | 54 |
| Hemi | 36 | 20 | 10 | 6 |
| Revision | 55 | 25 | 20 | 10 |
| Indication: | ||||
| Osteoarthritis | 297 | 193 | 86 | 18 |
| Rheumatoid arthritis | 36 | 23 | 9 | 4 |
| Cuff arthropathy | 160 | 69 | 64 | 27 |
| Avascular necrosis | 18 | 11 | 5 | 2 |
| Trauma | 22 | 7 | 8 | 7 |
| Trauma sequelae | 49 | 20 | 17 | 12 |
| Revision | 55 | 25 | 20 | 10 |
| Infection | 3 | 0 | 1 | 2 |
| Elective vs trauma: | ||||
| Elective | 569 | 321 | 185 | 63 |
| Trauma | 71 | 27 | 25 | 19 |
| Side: | ||||
| Right | 351 | 173 | 132 | 46 |
| Left | 289 | 175 | 78 | 36 |
| Previous surgery: | ||||
| Yes | 95 | 48 | 35 | 12 |
| No | 545 | 300 | 175 | 70 |
ASA, American Society of Anesthesiologists; IQR, interquartile range.
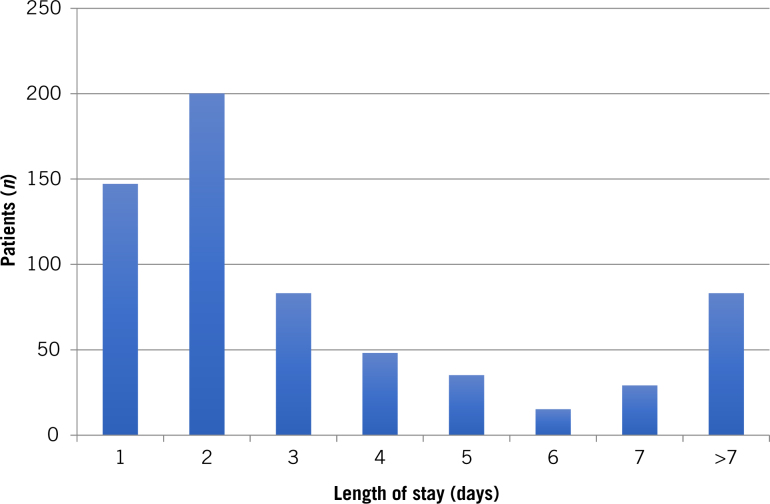
The median length of stay and a breakdown of median length of stay by patient and surgical factors is shown in Table 2, the mean and standard deviation is also included to allow comparison to published data. The median length of inpatient stay was two days (interquartile range, IQR, 2–4 days) and the mean was four days (SD ± 6), 348 patients stayed for one or two days, 210 patients stayed between three and seven days and 82 patients had an inpatient stay of greater than seven days (see Fig 1).
Table 2.
Length of Inpatient Stay by Indicative Patient and Surgical Factors
| All patients | Length of stay (days) |
|---|---|
| Median (IQR) | 2 (2–4) |
| Mean (SD) | 4 (± 6) |
| Range | 0–71 |
| Median length of stay (IQR) | |
| Age (years): | |
| < 60 | 2 (1–3) |
| 60–69 | 2 (1–3) |
| 70–79 | 2 (2–4) |
| > 79 | 4 (2–8) |
| Sex: | |
| Male | 2 (1–3) |
| Female | 3 (2–5) |
| American Society of Anesthesiologists grade: | |
| 1 | 2 (1–2) |
| 2 | 2 (1–4) |
| 3 | 3 (2–7) |
| 4 | 8 (3–23) |
| Charlson Comorbidity Index score: | |
| 0–3 | 2 (1–3) |
| 3–6 | 4 (2–7) |
| 6–9 | 8 (4–15) |
| Procedure: | |
| Anatomical | 2 (1–3) |
| Reverse | 3 (2–7) |
| Hemi | 2 (2–6) |
| Revision | 3 (2–5) |
| Indication: | |
| Elective | 2 (2–4) |
| Trauma | 3 (2–8) |
| Previous surgery: | |
| Yes | 2 (2–4) |
| No | 2 (2–5) |
IQR, interquartile range.
Figure 1.
Number of patients who stayed for each time period
Univariate comparisons suggested that patients who required inpatient stays of greater than the median were older (mean age 74 years vs 70 years), more likely to be female (80% vs 63%), had a higher Charlson Comorbidity Index (4 vs 3) and were more likely to have undergone surgery for trauma (19% vs 8%). Analysis of length of stay by patient and surgical factors demonstrated patients over 79 years had double the length of stay of younger patients (4 days vs 2 days), female patients had a median length of stay of three days compared with two days for males and that a Charlson Comorbidity Index of 6–9 was associated with a four-times longer inpatient stay when compared with patients with a score of 0–3 (8 days vs 2 days).
The analysis of variance indicated that the multiple regression model did significantly predict length of stay (p < 0.0001; Table 3). The length of stay was predicted by the following variables in the model (Table 1): age (p = 0.033), sex (p = 0.021), chronic kidney disease (p = 0.0008), congestive cardiac failure (p = 0.035), previous myocardial infarction (p = 0.030), intraoperative complication (p = 0.014) and postoperative transfusion (p = 0.0006). None of the other variables independently predicted length of stay.
Table 3.
Multiple regression model investigating factors that significantly predict increasing length of inpatient stay following shoulder arthroplasty
| Variable | Multiple regression model estimate | 95% confidence interval | t value | p–value |
|---|---|---|---|---|
| Age | 0.137 | 0.011 to 0.263 | 2.141 | 0.0327 |
| Sex | 1.091 | 0.165 to 2.018 | 2.314 | 0.0210 |
| ASA 1–2 or 3–4 | –0.861 | –1.820 to 0.098 | 1.763 | 0.0784 |
| Charlson Comorbidity Index score | –0.340 | –1.549 to 0.870 | 0.5519 | 0.5812 |
| Diabetes | 0.566 | –1.226 to 2.358 | 0.6207 | 0.5350 |
| Liver failure | –3.815 | –14.220 to 6.589 | 0.7201 | 0.4717 |
| Malignancy | 1.299 | –0.306 to 2.905 | 1.589 | 0.1125 |
| Chronic kidney disease | 3.727 | 1.565 to 5.889 | 3.386 | 0.0008 |
| Congestive cardiac failure | 2.581 | 0.186 to 4.977 | 2.116 | 0.0348 |
| Myocardial infarction | 2.672 | 0.265 to 5.078 | 2.180 | 0.0296 |
| COPD | 0.843 | –1.097 to 2.782 | 0.8533 | 0.3938 |
| Peripheral vascular disease | 2.621 | –2.131 to 7.372 | 1.083 | 0.2792 |
| Cerebrovascular accident | –0.560 | –3.140 to 2.020 | 0.4265 | 0.6699 |
| Connective tissue | 0.836 | –1.051 to 2.722 | 0.8700 | 0.3846 |
| Peptic ulcer | 0.738 | –2.155 to 3.632 | 0.5012 | 0.6164 |
| Trauma or elective | 1.341 | –0.566 to 3.247 | 1.381 | 0.1678 |
| Primary or revision | –0.281 | –0.642 to 0.084 | < 0.001 | > 0.9999 |
| Indication: osteoarthritis | –0.872 | –2.531 to 0.787 | 1.032 | 0.3025 |
| Indication: cuff tear arthropathy | –0.098 | –1.841 to 1.646 | 0.110 | 0.9123 |
| Year 2011–14 or 2015–17 | –0.473 | –1.365 to 0.419 | 1.042 | 0.2980 |
| Hemiarthroplasty | –0.069 | –0.711 to 0.573 | < 0.001 | > 0.9999 |
| Anatomical TSR | –2.399 | –8.721 to 4.021 | < 0.001 | > 0.9999 |
| Reverse TSR | –2.871 | –9.121 to 3.379 | < 0.001 | > 0.9999 |
| Side | –0.150 | –0.984 to 0.684 | 0.352 | 0.7247 |
| Hand dominance | 1.585 | –0.220 to 3.390 | 1.724 | 0.0852 |
| Anaesthetic (GA vs GA + block) | –0.551 | –1.859 to 0.756 | 0.828 | 0.4081 |
| Operating surgeon grade | 0.088 | –0.867 to 1.042 | 0.180 | 0.8572 |
| Previous arthroscopy | 0.315 | –1.366 to 1.997 | 0.368 | 0.7129 |
| Previous ORIF | –1.619 | –5.139 to 1.901 | 0.903 | 0.3667 |
| Previous arthroplasty | –2.739 | –5.626 to 0.148 | 1.863 | 0.0630 |
| Humeral fixation | –0.364 | –1.604 to 0.878 | 0.575 | 0.5654 |
| Intraoperative complication | 1.903 | 0.393 to 3.412 | 2.476 | 0.0136 |
| Postoperative transfusion | 3.888 | 1.671 to 6.106 | 3.444 | 0.0006 |
COPD, chronic obstructive pulmonary disease; GA, general anaesthetic; ORIF, open reduction and internal fixation; TSR, total shoulder replacement.
Discussion
This is the first study to determine factors associated with length of inpatient stay following shoulder arthroplasty in a UK population. We found a median inpatient stay of two days (IQR 2–4). 348 (54%) patients achieved discharge in two days or less with 83 (13%) patients requiring an inpatient stay of greater than seven days. The length of stay was predicted by age (p = 0.033), sex (p = 0.021), chronic kidney disease (p = 0.0008), congestive cardiac failure (p = 0.035), previous myocardial infarction (p = 0.030), intraoperative complication (p = 0.014) and postoperative transfusion (p = 0.0006) on multivariate analysis.
The two-day median length of stay reported here is less than the three-day (IQR 2–5) median length of stay reported by Craig et al in their study of 51,585 shoulder replacement carried out in the UK between 1998–2017.2 The 4 day mean length of stay is longer than the figure reported by Dunn et al who reported a 2.2-day mean length of inpatient stay in 2,004 primary elective total shoulder arthroplasties, with 91% of patients achieving discharge from hospital in three days or less, compared with 67% in this study.8 Padegimas et al reported a length of stay of 1.3 days in an orthopaedic specialist hospital, and 1.9 days in a tertiary referral centre when examining two groups of 136 patients, matched by baseline characteristics, who underwent primary total shoulder arthroplasty.11 These figures may not be entirely comparable though as these cases were all primary procedures, performed electively, and it is common practice in the United States for elective orthopaedic patients to be discharged to a rehabilitation facility prior to going home. Length of stay is also influenced in our institution by day case procedures being prioritised for early positioning on the operating list, with arthroplasty often undertaken later in the day.
In a study of 40,869 patients who underwent elective primary total shoulder arthroplasty, Menendez et al identified increasing age, female sex, renal failure, congestive heart failure, COPD and anaemia as factors associated with prolonged length of inpatient stay.9 Dunn et al also identified increasing age, female sex, chronic renal disease and higher comorbidity scores as predictive of prolonged length of stay in his cohort of 2,004 patients.8 The associations identified in this study between prolonged inpatient stay and increasing age, female sex, chronic renal failure and congestive cardiac failure are consistent with these previous findings. Previous myocardial infarction, intraoperative complication and postoperative transfusion independently predicting prolonged length of stay have not been reported previously.
Kim et al examined the use of the Charlson Comorbidity Index and the Elixhauser Comorbidity Measure in 90,491 patients who underwent primary elective total shoulder arthroplasty between 2002 and 2014 in Cleveland, Ohio.12 They reported both measures to be good predictors of postoperative complication, prolonged inpatient stay, discharge to a rehabilitation facility and death.12 While the Charlson Comorbidity Index was higher in patients with prolonged inpatient stay in this study, the Charlson score was not significantly associated with prolonged inpatient stay on multivariate analysis, so our findings do not support this Kim et al’s finding. However, the Charlson Comorbidity Index is made up of individual scores for comorbidities, some of which were found to be independent predictors of prolonged length of stay, so our data suggest the effect on length of stay appears to arise from the individual comorbidities rather than the overall Charlson Comorbidity Index.
The limitations of this paper are that this was a retrospective study based on a casenote and medical record review and the numbers may have been too small to detect all significant associations on multivariate analysis. The strengths of this paper are that it is a large, comprehensive, consecutive series of shoulder arthroplasty cases from a single UK centre with no cases excluded. It is a strength that this is the first work examining length of inpatient stay in a UK shoulder arthroplasty population and the factors associated with prolonged inpatient stay from a comprehensive consideration of potentially relevant factors. The methods used are robust and account for confounding and the interaction of effects from multiple variables. It must be stated however that the numbers are relatively small when compared with large national population level studies from the United States. The limitations are that this was a retrospective study based on case note and medical record review and the numbers may have been too small to detect all significant associations on multivariate analysis. These cases were performed in a high-volume UK centre so may not be generalisable to all UK centres performing shoulder arthroplasty. The study here is designed to demonstrate an association between considered variables and outcomes, but is not able to definitively prove causation.
Conclusion
This study reports the first data on length of stay following shoulder arthroplasty in a UK centre and the factors associated with prolonged inpatient stay. The findings are consistent with previously published work that increasing age, female sex, chronic renal failure and congestive cardiac failure are all associated with prolonged inpatient stay following total shoulder arthroplasty. Previous myocardial infarction, intraoperative complication and postoperative transfusion were also identified and predictors of prolonged inpatient stay. This study provides useful single-centre data in a UK population, and could be used in planning resource allocation for centres undertaking shoulder arthroplasty. This study also highlights the need for a larger in depth population level study of the length of inpatient stay and the factors associated with prolonged inpatient stay among patients undergoing shoulder arthroplasty in the UK.
References
- 1.National Joint Registry for England, Wales, Northern Ireland and the Isle of Man 16th Annual Report 2019: Surgical data to 31 December 2018. Hemel Hempstead: NJR Service Centre; 2019. http://www.njrcentre.org.uk/njrcentre/Reports-Publications-and-Minutes/Annual-reports (cited March 2020). [Google Scholar]
- 2.Craig RS, Lane JCE, Carr AJ et al. Serious adverse events and lifetime risk of reoperation after elective shoulder replacement: population based cohort study using hospital episode statistics for England. BMJ 2019; : l298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fevang B-TS, Lygre SHL, Bertelsen G et al. Good function after shoulder arthroplasty. Acta Orthop 2012; : 467–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fevang B-TS, Lygre SHL, Bertelsen G et al. Pain and function in eight hundred and fifty nine patients comparing shoulder hemiprostheses, resurfacing prostheses, reversed total and conventional total prostheses. Int Orthop 2013; : 59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boorman RS, Kopjar B, Fehringer E et al. The effect of total shoulder arthroplasty on self-assessed health status is comparable to that of total hip arthroplasty and coronary artery bypass grafting. J Shoulder Elbow Surg 2003; : 158–163. [DOI] [PubMed] [Google Scholar]
- 6.Anandaciva S, Jabbal J, Maguire D et al. How is the NHS Performing? London: King’s Fund; 2018. [Google Scholar]
- 7.Iacobucci G. NHS cancels planned surgery and outpatient appointments in response to winter crisis. BMJ 2018; : k19. [DOI] [PubMed] [Google Scholar]
- 8.Dunn JC, Lanzi J, Kusnezov N et al. Predictors of length of stay after elective total shoulder arthroplasty in the United States. J Shoulder Elbow Surg 2015; : 754–759. [DOI] [PubMed] [Google Scholar]
- 9.Menendez ME, Baker DK, Fryberger CT, Ponce BA. Predictors of extended length of stay after elective shoulder arthroplasty. J Shoulder Elbow Surg 2015; : 1527–1533. [DOI] [PubMed] [Google Scholar]
- 10.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; : 373–383. [DOI] [PubMed] [Google Scholar]
- 11.Padegimas EM, Zmistowski BM, Clyde CT et al. Length of stay after shoulder arthroplasty-the effect of an orthopedic specialty hospital. J Shoulder Elbow Surg 2016; : 1404–1411. [DOI] [PubMed] [Google Scholar]
- 12.Kim C-Y, Sivasundaram L, LaBelle MW et al. Predicting adverse events, length of stay, and discharge disposition following shoulder arthroplasty: a comparison of the Elixhauser Comorbidity Measure and Charlson Comorbidity Index. J Shoulder Elbow Surg 2018; : 1748–1755. [DOI] [PubMed] [Google Scholar]