Abstract
African American (AA) men continue to experience worse health outcomes compared to men of other races/ethnicities. Community-based interventions are known to be effective in health promotion and disease prevention. The program objectives were to (a) increase knowledge and risk awareness of targeted conditions, (b) change health-care-seeking attitudes toward regular primary care among AA men, and (c) improve their lifestyle-related health behaviors by leveraging the influence of women in their lives. The community-engaged educational intervention targeted both men and women and included eight 90-min sessions per cohort. Topics included prostate cancer, cardiovascular disease, diabetes, mental health, health-care access, and healthy lifestyle. Sessions were both didactic and interactive. A pre-/post-intervention questionnaire assessed knowledge. Interviews were conducted with male participants and a focus group discussion (FGD) with women to assess program impact. Interview and FGD transcripts were analyzed for themes and recommendations. Major themes were—increased knowledge/awareness of risk associated with chronic conditions, change in health-care-seeking attitudes, increased self-efficacy to engage the health-care system, and lifestyle changes. Other impacts reported were building community/social support, a safe and enabling learning environment, and enhanced community health status overall. Recommendations included having extended, more in-depth sessions, targeting the younger generation, smaller cohort sizes, and more community-based health programming. Community-engaged health promotion using a cohort model as well as including women can be effective in increasing knowledge, enhancing self-efficacy, and providing the much-needed social support. These can influence health-related behaviors and thus contribute to improving health outcomes for AA men.
Keywords: Prostate cancer, oncology/cancer, diabetes, physiological and endocrine disorders, cardiovascular disease, health inequality/disparity, health-care issues, African American
African American (AA) men are arguably the most vulnerable population regarding health disparities in the United States. Looking at all-cause mortality, AA men have the shortest life expectancy of all segments of the U.S. population (Azar et al., 2017). AA men in the United States bear a substantially higher burden of risk factors associated with chronic diseases including prostate cancer, cardiovascular disease (CVD), diabetes, and mental health conditions.
Prostate cancer is the most common cancer in men and ranks second among the leading causes of cancer mortality in men in the United States (American Cancer Society. Cancer Facts & Figures 2019, 2019; CDC D of CP and C, 2019). The risk of developing prostate cancer is 1.6 times higher for AA men than for White men, and AA men are also more likely to have prostate cancer at an earlier age, be diagnosed at a late stage of the disease, and have poorer outcomes (Smith et al., 2017). The rate of late-stage diagnosis of prostate cancer in AA men has been linked to a lack of primary care (Reynolds, 2008). Additionally, there are no genetic factors conclusively linked to prostate cancer disparities (Cuevas et al., 2019); however, many social determinants (e.g., insurance, education level, geography) are associated with patient diagnosis and outcomes (Hastert et al., 2015; Taitt, 2018).
Similarly, CVD including hypertension, stroke, end-stage renal disease, and type 2 diabetes (T2D) are more prevalent among AA men compared to men of other races/ethnicities (Hasson et al., 2015; Howard et al., 2017). For example, compared to White men, rates of CVD complications such as stroke and renal disease are two and five times higher, respectively, in AA men (Lackland, 2014). Additionally, AA men diagnosed with T2D have less glycemic control as well as greater risk of diabetes-associated complications such as retinopathy, nephropathy, and amputations (CDC, 2016), all of which have a significant impact on the life expectancy of AA men (Howard et al., 2018).
Disparities also exist for the mental health of AA men. The often concomitant burden of socioeconomic disadvantage combined with the psychosocial aspects of being Black in America has compounding effects that appear to affect the mental health of AA men. While mental health issues among AA men tend to be reported 30% more often than those of non-Hispanic White men, AA men are still less likely to receive adequate care from a mental health professional (American Psychiatric Assoc., 2017). The possible causes for the persistence of mental health disorders are a combination of financial and cultural barriers to accessing treatment, which make it difficult to adhere to many forms of psychotherapy (Bailey et al., 2011; Valenstein et al., 2004).
Health-Care-Seeking Behaviors: Barriers and Facilitators
For the aforementioned chronic conditions, regular primary care is critical to prevention, early diagnosis, and effective management. Compared to their White counterparts, AA men are less likely to utilize primary health-care services as their usual source of care (Arnett et al., 2016). While access-related factors are major barriers (Brown et al., n.d.; Satcher, 2003), underutilization is still high even among AA men with insurance coverage (Dunlop et al., 2002; Forrester-Anderson, 2005). A review of literature by Cheatham et al. identified several barriers to health-care-seeking behavior among AA men including masculinity, lack of awareness of the need for care, racism, distrust of the medical establishment, religion and spirituality, and criminal background (Cheatham et al., 2008). Several of the studies reviewed also identified kinship social networks as a facilitator of favorable health-care-seeking behavior, and female relatives in particular as motivators for AA men to seek care (Blocker et al., 2006; Plowden & Young, 2003; Rose et al., 2000).
Culturally, women have been known to have a strong influence in the AA family structure. Facilitating health-care utilization for male family members and supporting health-related decisions are components of the caregiving role that many AA women already play within their families (Jones et al., 2009, 2010). Previous research identified several roles for women in the effort to reduce health disparities affecting AA men and existing barriers to their health care (Okoro et al., 2018). These roles included being an education/information resource, providing support and encouragement, instituting a “culture” of regular primary care, modeling health-care-seeking behavior, surveillance and monitoring, motivation, and influencing diet. However, lack of knowledge was reported as a key limitation of their involvement in these roles. Therefore, the current study targeted women, in addition to men, for health education and promotion.
The objectives of the intervention were to (a) increase knowledge and awareness of risk factors associated with select chronic health conditions (prostate cancer, CVD, diabetes, mental health) and (b) change health-care-seeking attitudes toward regular primary care among AA men. The long-term goal was to improve health-related behaviors (diet, exercise, primary care utilization) among AA men.
Following this pilot intervention, a program impact evaluation was conducted to determine the immediate benefits of the program and receive participant feedback on how to improve program delivery and effectiveness. The specific aim of this article is to describe the pilot intervention and report on the findings from the program impact evaluation.
Methods
Using a community-engaged participatory approach, the intervention was conducted in partnership with the local chapter of the National Association for the Advancement of Colored People (NAACP). Two community members who are NAACP members (one male, one female) were recruited as research personnel. Both received training in “Research Ethics and Compliance” for social science research through the Collaborative Institutional Training Initiative (CITI). The training was done through the University of Minnesota.
Study Area and Recruitment
Male participants were recruited in response to fliers distributed at community meetings (NAACP, the AA men’s group, the Family Freedom Center) and community outreach programs in the Twin Ports area of Minnesota.. This area has a population of approximately 112,000 people. Within the small metropolitan area, 2.3% of the population identify as Black/AA, with 68% living below the poverty line (U.S. Census Bureau, 2018). At the time of the study, there were no barbershops and the two “Black churches” had very few AA men in attendance. To be in the study, participants had to be 18 years old and above, male, and self-identify as AA.
For female participants, each male participant was asked to recruit two women in their family and/or social network. Actual recruitment was not required for inclusion in the study. For further recruitment, the community research personnel reached out to other women in the community using fliers and word of mouth. Participants had to be 18 years and older, female, and related to any AA man (significant other, mother, daughter, etc.).
Informed Consent
The consenting process was conducted during the introductory sessions with potential participants prior to any intervention. Informed consent was administered following detailed description of the study including expectation of participants. Prior to each session, participants were reminded that prior consent was not binding and that withdrawal was an option at any time. The intervention was implemented for cohorts of male and female participants. Each consenting participant retained a duplicate copy of all signed forms.
Intervention
Educational Sessions
There were eight sessions per cohort. Three sessions were on prostate cancer based on strong interest from the community when conceptualizing the project. Other sessions included CVD, diabetes, mental health, access to health care, and healthy lifestyle (see Table 1). For the disease-focused sessions, the invited expert gave a presentation and thereafter facilitated discussion with an opportunity for participants to ask questions. For the session on access to health care, a public health nurse shared information on health-care-related resources in the area and how to access them. The session on lifestyle was a panel discussion. The invited experts constituted a discussion panel and educated participants on well-being (mental, physical, and emotional), physical activity, and dietary recommendations.
Table 1.
Summary of Health Education Sessions.
| Topical Area | Content of session | |
|---|---|---|
| Session 1 | Prostate Cancer—Part I | How common is prostate cancer? What is prostate cancer? |
| Session 2 | Prostate Cancer—Part II | What causes prostate cancer? What are the risk factors? Can prostate cancer be prevented? |
| Session 3 | Prostate Cancer—Part III | Available test to detect it early What can you do today? Resources |
| Session 4 | Cardiovascular Disease | Why is this important? What is heart disease? What are the treatments and advancements? How do you know if you are at risk? How can your doctor help you? (Questions to ask your doctor) |
| Session 5 | Diabetes | Why should you care? What is diabetes and how is it treated? How do I know I have diabetes? What happens if not treated? What can you do? (prevention) How can your doctor help you? (Questions to ask your doctor) |
| Session 6 | Mental Health | Why does mental health matter? What are common mental health conditions among AAs? What factors are associated with the development of mental health conditions? What are the AA community’s concerns about mental health? What are the challenges for the AA community receiving services? Ways to prevent mental illness Community resources |
| Session 7 | Healthcare Access | Where to go to for healthcare if you do not
have health insurance How to get healthcare insurance Government-assisted insurance and what it covers |
| Session 8 | Healthy Lifestyle | Topics: Physical Activity; Diet; Sleep; Mental
and Emotional Health; and Social
Support Importance and benefits Recommendations from experts and relevant professional bodies How to achieve the recommended goals |
Facilitators
The sessions for prostate cancer were facilitated by a cancer cell biologist/researcher. The sessions on CVD and diabetes were facilitated by a physician—a specialist in internal medicine. For mental health, the facilitator was a clinical therapist. All three facilitators were male (two Black/AA, one White) and all active members of the AA community in the region.
For Men
Based on availability of the majority, sessions were scheduled mostly on Sunday evenings with makeup sessions afterward for those unable to make it to the initial sessions. For six of the eight sessions, the respective invited expert gave a presentation on the scheduled health-related topic (prostate cancer, CVD, diabetes, or mental health) and thereafter facilitated discussion with an opportunity for participants to ask questions (see Table 2). Some meetings (for both male and female cohorts) incorporated two sessions per participants’ preference. Each session lasted for 90 min. A meal was served at each meeting (for both cohorts) with efforts to model healthy dietary recommendations. Meetings (including makeup sessions) were held in the VIP lounge of a local bar between January and April 2018. After each session, participants received printed materials for further reading and information on other relevant resources.
Table 2.
Demographic data of Study Participants.
| Demographic Characteristics | Men (n = 29) | Women (n = 46) |
|---|---|---|
| Frequency (percentage) | ||
| Race/ethnicity | ||
| AA | 29 (100) | 40 (87.0) |
| Other | – | 6 (13.0) |
| Marital status | ||
| Single, never married | 16 (55.2) | 26 (56.5) |
| Married | 8 (27.6) | 7 (15.2) |
| Divorced | 3 (10.3) | 4 (8.9) |
| Separated | 1 (3.4) | – |
| Widowed | – | 7 (15.2) |
| No response | 1 (3.4) | 2 (4.3) |
| Employment | ||
| Full-time | 11 (37.9) | 9 (34.6) |
| Part-time | 5 (17.2) | 9 (34.6) |
| Self-employed | 6 (20.7) | 1 (2.2) |
| Unemployed | 5 (17.2) | 12 (26.1) |
| Other | 2 (6.9) | 14 (30.4) |
| No response | 1 (2.2) | |
| Education | ||
| Graduate studies | 3 (10.3) | 4 (8.9) |
| College (some) | 21 (72.4) | 19 (41.3) |
| High school | 4 (13.8) | 20 (43.5) |
| <High school/none | 1 (3.4) | 3 (6.5) |
| Insurance type | ||
| Employment based | 6 (20.7) | 5 (10.9) |
| Government assisted | 12 (41.4) | 26 (56.5) |
| Other type/>one type | 4 (13.8) | 8 (17.4) |
| Privately purchased | 1 (3.4) | – |
| None | 6 (20.7) | 7 (15.2) |
| Age (years) | Mean | 45.1 Range | 27–74 |
Mean | 49.5 Range | 18–86 |
| Completed all sessions | 11 (37.9) | 33 (71.7) |
For Women
Sessions (including makeup sessions) were offered on Monday or Tuesday evenings after work hours, based on majority preference. Sessions commenced after the intervention for men was completed and were facilitated by the same invited experts as for the men. Meetings were held in the conference facility of a community center between April and June 2018.
Evaluation
Knowledge Questionnaire
On completion of all the sessions, participants in both cohorts filled out a pre-/post-knowledge questionnaire assessing knowledge of prostate cancer (29 items), CVD (10 items), diabetes (10 items), and mental health (15 items). The questionnaire was not a validated instrument. The questions were formulated by the investigators and facilitators based on the content covered in the sessions and materials provided. Participants were required to indicate prior knowledge (retrospective pretest) and current knowledge for each item. Only participants who completed the study filled out the pre/post questionnaire. A retrospective pretest design was used to minimize guessing since the response categories were “True,” “False,” and “I don’t know.” Eleven men and 33 women who completed the study filled out the pre-/post-knowledge questionnaire immediately after the sessions for each cohort, respectively. Participants received a debit card on enrolment and were compensated with $20 loaded on the card for each session they attended.
Interviews
Six months after the sessions, male participants who completed the sessions were invited to participate in one-on-one interviews. The interviews were conducted by one of the investigators. The purpose of the interviews was to obtain feedback from the participants on the value of the intervention and recommendations for improvement. The 6-month interval allowed for completion of the intervention for women and opportunity for the men to implement information from the sessions in their daily lives. Eight of the 11 men who completed the study participated in the interviews, which lasted an average of 18 min (range: 8–31 min). We also reached out to the men who did not complete the study for insight into the deterrents.
Focus Group Discussion
Immediately following the study, all the women participants were invited to a focus group discussion (FGD). Five women participated in the FGD. The FGD was conducted by the same investigator who conducted the interviews with the men, using questions adapted from the interview guide for the men. The questions were open ended and generated by the investigators with the aim of eliciting feedback and recommendations. The FGD lasted for 62 min.
Overall Program Impact Evaluation
Following the intervention, interviews were conducted with 7 of the 11 male participants who completed all eight sessions and a focus group discussion (FGD) with five women to assess program impact. All the interviews and FGD were conducted by the same researcher. These were audio-recorded and transcribed verbatim.
Data Analysis
Data from the knowledge questionnaire were analyzed using frequencies, percentages, and t tests. One question item was excluded from analysis due to a printing error that was not corrected before administering the survey. Therefore, only 28 items are used in the analysis of the knowledge questionnaire. For the qualitative data, three transcripts were coded independently by two researchers who then met to reconcile the codes. The codes adopted by agreement were used to code all the transcripts. The codes were put in categories based on relatedness. Themes emerged from more conceptual analysis of the categories. Recommendations were also identified and extracted from the data. These are the findings reported here.
Results
Demographics
There were 29 men and 46 women enrolled in the study, with a completion rate of 37.9% (n = 11) for men and 71.7% (n = 33) for women (see Table 2). Approximately a quarter (n = 8; 27.6%) of the men were married at the time of enrollment and almost all (n = 24; 82.7%) had more than a high school education. One fifth (n = 6; 20.7%) of the men had no insurance coverage at the time of enrolment (see Table 2). Six of the female enrollees were not AA and approximately half had more than a high school education (see Table 2).
Knowledge
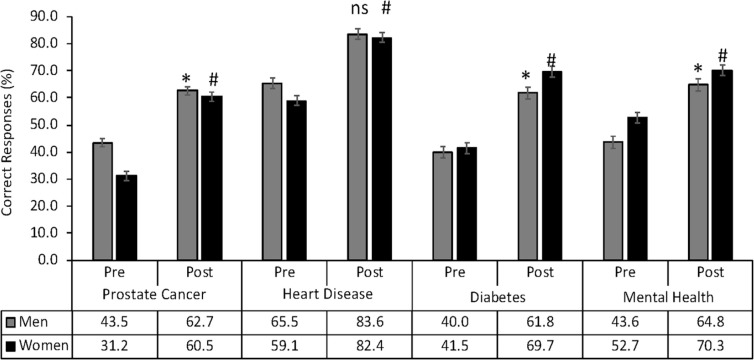
Only the participants who attended all the sessions on the four chronic conditions were assessed for knowledge. There was significant increase in knowledge for each chronic condition (Figure 1).
Figure 1.
Knowledge assessment response rate by male and female study participants. Values are expressed as means ± standard error of the means of each group. * indicates significant difference between men’s pre- and post-assessment scores (p < .05) using Student’s t test. # indicates significant difference between women’s pre- and post-assessment scores (p < .05) using Student’s t test. ns indicates no statistically significant difference (p > .05).
Program Impact
Major themes emerging from the feedback received from interviews with male participants and the FGD with female participants were regarding the impact of the program on the individual as well as collectively. These included the following:
(i). Increased knowledge/awareness of risk
(ii). Change in health-care-seeking attitudes
(iii). Increased self-efficacy to engage the health-care system
(iv). Lifestyle changes
(v). Sense of community/social support
(vi). Creating a safe and enabling learning environment
(vii). Enhancing community health status overall
Increased Knowledge/Awareness of Risk
Participants repeatedly acknowledged that through the program, they became more aware of the risk factors associated with chronic conditions and gained a lot of knowledge regarding the etiology, pathophysiology, and treatment of these conditions. The female participants also acknowledged that having gained knowledge, they shared it with males in their family and social networks including those who may not have participated in the study.
A lot of things about diabetes that I didn’t know. I’ve been fortunate enough not to have it, but I know more about it. I know a lot of people with it, but I didn’t know it was that serious. . [Male participant #2]
I learned a lot, so this program helped me realize the different types, ——- and it was able to help me tell a lot more of my male friends. I have a lot of male friends. I tell ’em you need to get checked, and how critical it can be. [Female participant]
The pre-/post-intervention assessment showed a statistically significant increase in mean scores for each targeted condition for both male and female participants (see Figure 1). Base knowledge for prostate cancer was significantly higher among men than among women (mean scores of 11.7 and 8.3, respectively) but similar for CVD, diabetes, and mental health. Levels of knowledge after the intervention were similar among men and women (see Figure 1).
Change in Health-Care-Seeking Attitudes
During the sessions, there was an emphasis on the benefits of preventive care and how critical early detection is to the effective management and treatment outcomes of the chronic conditions addressed. Participants generally acknowledged that AA men were often unlikely to seek regular medical care until they had a situation that impeded their daily function or was life-threatening. Some of the participants said they had thereafter resolved to be more proactive in getting regular care. The women reported that they were encouraging men in their families to seek primary and preventive care.
I’m going to be able to move forward with—since I’m just now turning 40, I’ll be able to start scheduling my doctor’s appointments, at least a yearly check up on all the aspects that we covered. I’ll be doing that soon. I haven’t done it yet, but I will. I plan on doing it. [Male participant #5]
I didn’t know nothin’ about it. That was enlightening. I told my son, but I don’t know. He might get it checked. He might not. I don’t know, but I did tell him, ———— We tell him he should go to the doctor. [Female participant]
I asked my husband did he have a prostate cancer check. I thought he did, but I really wasn’t for sure, but he did, and he had a colonoscopy, so that was all cool. [Female participant]
Increased Self-Efficacy to Engage the Health-Care System
Another key focus through the sessions was the education of participants on patient’s rights and role in health-care encounters. This elicited a lot of discussion as participants were mostly unaware of how they could initiate processes in the health-care system or advocate for themselves regarding their health-care needs. Male participants reported that one way the intervention impacted them was in empowering them to take on a more active role in their health care—requesting appointments/tests and asking the provider clarifying questions during clinic visits.
It helped me to focus more on what’s going on with me. You have a tendency to overlook and take for granted and listen to what the doctor says and that was my experience in the past where I listened, but I think they over assured me that they knew what they were doing with me, so I went along with them. . .what I’ve learned from this is to ask more questions. . . I’m sitting down asking anything and I get that number and I’ll call if I have a thought process, if I’m processing. That’s how it helped me. [Male participant #3]
Lifestyle Changes
That one’s lifestyle was a major factor (protective or adverse) in one’s health was undeniably a key message reinforced throughout the intervention. With the knowledge gained and practical tips/tools provided, most male participants had resolved to change poor habits and embrace a healthier lifestyle. The men interviewed talked about what they had started doing following the intervention. These included changes to dietary habits and increase in physical activity. They also reported feeling healthier as a result of these changes. The men also acknowledged the role women played in keeping them accountable to a healthier lifestyle.
Before that I was eating fruits, but not as much vegetables. I’m not eating fried, greasy foods. Well, other than that, I’ve lost 25lbs in what? A month and a half. I went down two pant sizes. Cause when we did the height, the weight (BMI), I was way over-weight. —- I climb hills, just walk. .. 10 miles. I bike. .. Got 10 more pounds to lose. I was at, last year in March, I was 316 pounds. It’s been down to 260. Yeah. [Male participant #4]
I’m drinking a lot more water. I used to drink water on a regular basis and, right now, it’s increased substantially. That’s been very helpful. The issue I had was the intake of Coca-Cola. That has been a stumbling block for me, but I’ve gone cold turkey. I don’t drink Coke products. Yes. I had become addicted to that and I stopped cold turkey, cold turkey. That’s what’s changed in my life and those— [Male participant #1]
I know there are a couple of females in my life that are a part of the study ——— They’re checking on me ——- Yes. I’m serious. They’re checking. One said, I’m gonna be knocking on your door on a regular basis just to check in to make sure ——— [Male participant #3]
Sense of Community and Social Support
The male participants repeatedly talked about the opportunity it afforded them to meet other AA men and come together in a way that was not commonplace in their years of residency in the area. There was an appreciation for the sense of community experienced and support garnered from each other during the sessions. Participants expressed interest in maintaining the connections made and nurturing the relationships built even after the sessions ended. According to some of the participants, these group sessions were like being in a support group and it was reportedly therapeutic and beneficial for their mental health.
We were really trying to communicate not only in terms of learnin’ for ourselves but create an opportunity for us to interact with each other. This community is disconnected, it’s a transit community and so many people don’t know each other. I think it’s been able to create a support system that we can fellowship and encourage each other. I mean, ‘cause I had an opportunity to get on one-on-one with people and get to know more about them. To share my story and to listen to their story was very important to me. [Male participant #7]
I saw more guys of color in there and I’ve been here three and one-half years that I’ve never seen before. It’s also a place where we could build some relationships. It’s also a place where we can network. It’s also a place where we can find out about people who might be struggling and how we can help them. [Male participant #6]
Most impactful was probably just being in a group of black men and talkin’ about some real actual issues. Things that really affect us. I think that was probably the most impactful because it said to me that, “Hey, I’m not alone, and I can actually talk about real stuff.”. . .‘cause you could just sit and say what’s on your mind, you could get some feedback and you could let it off your chest. . . talkin’ about it in a group, that’s positive. That can really help you out. It helped me out. [Male participant #8]
Unique and Enabling Learning Environment
The male participants described the sessions as unique in the sense that there were not just didactic but interactive and included visual aids. They also talked about how enabling and empowering it was for them to be able to share their thoughts and have conversations about their health with other AA men. According to their reports, also germane to their experience was having respective health-care experts on hand to answer their questions and address concerns. Other elements unique to their learning experience that they commented on included knowing that others faced similar challenges and hearing from older men who shared their health-related experiences.
We keep most things inside, to ourselves. It’s helpful to get outside of yourself and discuss it with other men who are in your same situation or you might be in their situation one day. A lot of information from the older men that were in their 60s and 70s having experienced those things personally leads you to see that you might not want to experience those, and if you do you see that there’s light at the end of the tunnel, for those. . .if you do have problem. [Male participant #5]
…being able to ask him questions, that was interesting. That doesn’t usually happen. Usually, you’re asking questions of a doctor when you’re in the clinic or in the hospital. You know what I mean? That’s different. [Male participant #8]
Enhancing Community Health Status Overall
There was some conversation around how the benefits from the intervention contributed to enhancing the health of others in the community, as participants used the knowledge gained to educate others. Some participants talked about the potential for further promoting awareness of health risks going forward. Participants generally agreed that continuing community-based health education would be helpful for the community as a whole and AA men in particular. Women acknowledged that including them guaranteed a wider reach even beyond their own families.
It’s not only helpful to me but helpful to my family and hopefully even future generations of descendants, for my descendants. I just spent a lot of time talkin’ to my family about this. They hate it. They hate for me to come ‘cause I’m lecturin’ them and always tryin’ to make sure because I know they don’ read stuff. [Male participant #7]
When we know, and when we are—and particularly women, because we carry the load. We carry the weight of everything, mothers, grandmothers, and we’ve got so many grandmothers raising kids and stuff like that, that we need to be so aware of things and stuff. The other thing that we have—we have a lot of kids comin’ to our homes, so we’ll be able to share. I know we all have—if you got a grandchild, you got other grandkids. Somebody just stepped out of my house today and said, “Bye, grandma!”, I looked around and it wasn’t one—and so all of the kids, all the young men that come in—the boys that come in my house— [Female participant]
Recommendations
There were some recommendations on how the intervention could be improved on, for more effectiveness. These included the following:
Have extended and more in-depth sessions on various health conditions. Both men and women reported that time was often not enough at the sessions.
Target the younger generation of men. One of the men suggested that this would help men develop a healthy lifestyle and adopt a preventive approach to health from an early age. This sentiment was echoed by the women.
Select smaller cohort sizes to facilitate effective engagement and social support for the men.
Use venue(s) that is/are more reflective of learning (e.g., classroom or conference room versus the space used for the men) to help participants more readily get into a learning mode.
Include more community-based health programming (e.g., screenings, health fairs).
Feedback From Non-Completers
The men who did not complete the study indicated the following as barriers: (a) conflict with schedule for work (some had jobs with changing shifts or jobs that took them out of town), (b) conflict with schedule for other community-related engagements, (c) lack of transportation, and (d) lack of childcare.
Discussion
The current study was a community-engaged health promotion intervention whose aim was to enhance the health of AA men in a geographical area that lacks the social institutions commonly associated with the Black/AA community such as Black churches and barbershops. The study aimed to increase knowledge and awareness of risk factors associated with select chronic health conditions, change health-care-seeking attitudes, and in the long term, improve health-related behaviors among AA men. Educational sessions for men were replicated for women who are believed to also play a critical role in the health of AA men. Following the intervention, participants completed a retrospective pre-/post-knowledge test and interviews. Findings from the evaluation for immediate impact demonstrate the value of a cohort-style, community-based health educational intervention as shown by the increase in knowledge and perceived benefits reported by participants.
Demographics
Among male participants enrolled in the study, government-assisted insurance was the most common type of insurance and less than half of the men (37.9%) had full-time employment. This is in contrast with the level of educational attainment as most of the men (82.7%) had more than a high school education. This reflects the low socioeconomic status prevalent in the AA population as well as the disparities in employment opportunities that adversely affect them (Williams & Wilson, 2019). Income level and employment are known social determinants of health (Singh et al., 2017).
Increase in Knowledge and Awareness
Along with the perception of increased knowledge emphasized by participants in exit interviews and the focus group, the post-assessment data indicated measurable gains in knowledge by participants related to each targeted disease. However, the overall magnitude of increase in knowledge was not always large, but this was expected, given the window of exposure to the information. Aside from prostate cancer which had three sessions, each of the other conditions was covered in a single 90-min session. However, the modest gain in this pilot provides the impetus to implement a larger scale intervention with longer and more in-depth educational sessions as recommended by the participants. Similar to this study, several studies have demonstrated the effectiveness of community-engaged health education in increasing knowledge of CVD (Brewer et al., 2017; Daniels et al., 2012), mental health (Ann Hall et al., 2011; Fuller et al., 2012), diabetes (Bertera, 2014; Embry et al., 2013; Peña-Purcell et al., 2015), and prostate cancer (Boehm et al., 1995; Linnan et al., 2014; Sandiford & D’Errico, 2016) among African Americans. A critical element is the utilization of existing social institutions and structures in the AA community to implement these health promotion programs.
Of note, the pre-/post knowledge levels of CVD and diabetes were lower when compared to those of prostate cancer and mental health. This may be attributable to several factors including the complexity of CVD and diabetes, difficulty in delivering the content, differences in learning styles of participants, or congruency between the cultural background of the facilitator and the audience (facilitators for prostate cancer and mental health were both males of African heritage). It is also plausible that these topic areas (prostate cancer and mental health) were of more interest to the participants. There is a substantial body of literature detailing the fears and misconceptions of Black men related to prostate cancer (O & A, 2018; Pedersen et al., 2012). Mental health as well is often a taboo subject among AA men for a variety of reasons, chief among which is the associated stigma (Primm et al., 2010). Yet, AA men are especially vulnerable to mental health problems and illnesses because of the persistent socioeconomic and structural inequities (Bryant et al., 2003). During these specific education sessions, there was consistent dialogue between the facilitator and the participants, demonstrating a high level of engagement among both male and female cohorts. Therefore, we surmise that the sessions related to prostate cancer and mental health provided a safe space for the men and women to discuss their own knowledge, experiences, and misunderstandings with knowledgeable facilitators.
Though lower than that of men, baseline knowledge of prostate cancer among women participants was appreciable, considering the male specificity of the disease. From discussions, many of the women reported that they have had experience with loved ones affected by prostate cancer. Near equivalence in post-intervention knowledge level for both men and women supports the premise of our approach—that women are as interested in men’s health or even more so than men. Further, the women who participated in this study may have played a role in fortifying the men’s knowledge, as women reported sharing the information they received with men in their family and social networks. Again, this supports the premise of the approach in this intervention that women can be a health information resource for men if they are adequately educated. Although we are interested in measuring the effect of women’s influence on knowledge retention in the male cohort, testing that influence directly is beyond the scope of the pilot. Findings from the current study are largely in agreement and build on those of previous studies demonstrating the interest and involvement of women in the health and health care of AA communities (Allen et al., 2018, 2013; Eley et al., 2019; Jones et al., 2010; Plowden & Young, 2003).
Change in Health-Care-Seeking Attitudes and Increased Self-Efficacy
The information provided during the sessions was helpful in linking poor health-care-seeking behavior to poor health outcomes and emphasized the importance of preventive care. The resolve by participants to seek timely care was demonstrated in the responses of the men during the 6-month post-intervention interviews. While distrust of the health-care system may still be a deterrent to seeking care, getting an accurate sense of disease morbidity and mortality, especially from the graphics in the presentations appeared to have contributed to changing attitudes and motivating better health-seeking and preventive behaviors. This is in alignment with the theoretical underpinnings of the health belief model (Becker, 1974; Plowden & Miller, 2000; see Figure 1). The self-reported change in behavior is therefore likely due to participants’ (a) perceptions of benefits (vs. barriers to) of seeking regular care, (b) perceptions of threats to their well-being and long-term health (based on seriousness and susceptibility of AA men to these conditions as demonstrated by data), (c) increased self-efficacy facilitated by information shared on patient advocacy and rights, and (d) receipt of practical tips offered by facilitators during the sessions. There is widespread recognition that health communication influences health-related attitudes and behaviors and thus contributes to eliminating health disparities (Freimuth & Quinn, 2004). However, cultural responsiveness is critical to the effectiveness of health communication (Thomas et al., 2004). In a study by Griffith et al. (2012), they found that family members were the most reliable source of health information among AA men. They also found that having a health issue and having social support were motivating factors for the translation of information to health-related behaviors (Griffith et al., 2012).
Lifestyle Changes
Health educational interventions are not only effective in increasing knowledge and awareness, but several studies have also demonstrated change in disease-specific measures and outcomes following educational interventions (Ghisi et al., 2014). While often critical in informing change, general knowledge alone is not enough to drive behavior change if the education does not build relevant skills and enhance self-efficacy to engage in the targeted health behavior (Arlinghaus & Johnston, 2018). In the current study, participants were educated on “what to do” but also on “how to do it” to achieve the desired results. In addition to these skills, the study also employed the benefits of social networks. This is a well-tested approach to assuring behavior change (Hunter et al., 2019; Latkin & Knowlton, 2015; Valente et al., 2015, 2007). By leveraging the distributive attributes and influences of social networks, and targeting influential individuals within these networks, health behaviors can be more effectively promoted in populations. The current study took advantage of the tight and pervasive kin networks within the AA population by targeting women (as influencers) in education aimed at promoting health behavior change among AA men.
Community Impact
The sense of community and perceived social support among the male participants was a welcomed outcome of the intervention. Compared to AA women, AA men are more likely to experience social isolation (Taylor et al., 2019). Social isolation has been significantly associated with poorer physical and mental health (Chatters et al., 2018). Social connectedness of AA men with other AA men has been shown to promote health as established by several studies that have used barbershops in health interventions for AA men (Brawner et al., 2013; Luque et al., 2014). Barbershops constitute social forums for AA men, providing a space where they can relish their historical and social identities and bond with each other (Shabazz, 2016). The current study highlights the importance of this social element in interventions to promote health among AA men.
Like the barbershop experience, being in a community space with other AA men gave the participants a sense of safety. Unburdening themselves to others they considered to have a shared experience with (of being a black male in a predominantly white population) served as a great mental health boost. This enabled learning from facilitators as well as fellow participants.
The community-based approach of the intervention and particularly the inclusion of women served to enhance health not just for the men as targeted by the study but reportedly for others in the community through diffusion of the knowledge gained. This outcome is supported by the social network theory. Some community members who did not participate in the study have since reached out to the investigators indicating their interest in participating in any future project.
Limitations
This was a pilot study with a small number of participants in a unique environment that may not mirror the areas where AAs are typically found in large numbers. While findings may not be generalizable to the latter, it does provide an alternative approach to health interventions targeting AA men’s health in areas where there are no culturally specific gathering places (e.g., barbershops). In addition, the innovation of including women who may or may not be significant others is applicable to the AA population in general, given the culturally specific social networks typical of AA communities.
Given the scale of the study, we were unable to conduct long-term follow-up to monitor sustained health behavior changes. For the same reason, the findings regarding changes in attitudes to health seeking and self-efficacy to engage with the health-care system and providers are by self-report and not measured objectively. Therefore, the validity of these claims cannot be established, necessitating further research. Another assessment-related limitation of the study is that the knowledge questionnaire used in the study was not a validated instrument. However, questions were generated by the facilitators in alignment with the objectives of the sessions.
This was a convenience sample. Participants may be more health conscious, hence their interest in participating in the study. There was considerable attrition in the men’s cohort due to conflicting work schedules, travel out of town for work, lack of transportation during the winter months, and a return to prison for two of the enrollees. Makeup sessions were offered to enable some of the participants to finish the study. In subsequent interventions, transportation will be provided and alternate times for each session scheduled a priori to enable participants to plan accordingly.
There may be some missed perspectives due to the low response rate for the women’s focus group. Attending the FGD required coming for an additional session for which no compensation was provided. In subsequent programming efforts, adequate compensation will be taken into account in the budgetary considerations.
Conclusions
The disparities in health that affect AA men are often more pronounced in areas where the Black/AA population is sparse due to the lack of a cohesive community. The current study offers an innovative approach to addressing the health disparities that affect AA men who live in such areas where the population is predominantly White and there are no spaces where the Black/AA community congregate and find social support. These preliminary findings suggest that leveraging the social networks characteristic of the AA culture and involving women within those networks, whether or not they are significant others, is an approach with potential to enhance the health of AA men and the community at large. The use of a cohort model that can serve as a support group presents an alternative approach in places where the commonly used social institutions (barbershops and faith-based institutions like Black churches) shown to be effective in health interventions are not present. Further research is needed to establish the efficacy of this strategy.
The community-based strategy where health education and promotion are done in the community space versus the health-care setting may provide a more enabling environment for learning and engagement for community members. With this public health approach, providers may be able to address health-related concerns from a broader perspective and equip community members with practical skills to actuate healthier behaviors. This also creates opportunity for health-care providers to reach exponentially many more people and make more impact on population health than they would providing patient care only in the clinic.
Supplemental Material
Supplemental material, Supplementary_File for Culturally Responsive Health Promotion to Address Health Disparities in African American Men: A Program Impact Evaluation by Olihe N. Okoro, Chantele S. Nelson, Stephan P. Witherspoon, Salaam F. Witherspoon and Glenn E. Simmons in American Journal of Men’s Health
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research conducted by the authors was supported by the Center for Healthy African American Men through Partnerships (CHAAMPS); CHAAMPS is made possible through NIH grant U54MD008620. The administrative home of the collaborative is at the University of Minnesota, with physical locations on both the University of Minnesota (UMN) and University of Alabama at Birmingham (UAB) campuses.
ORCID iDs: Chantele S. Nelson  https://orcid.org/0000-0003-4899-5185
https://orcid.org/0000-0003-4899-5185
Glenn E. Simmons  https://orcid.org/0000-0003-2081-5672
https://orcid.org/0000-0003-2081-5672
References
- Allen J. D., Akinyemi I. C., Reich A., Fleary S., Tendulkar S., Lamour N. (2018). African American women’s involvement in promoting informed decision-making for prostate cancer screening among their partners/spouses. American Journal of Men’s Health, 12(4), 884–893. 10.1177/1557988317742257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen J. O., Griffith D. M., Gaines H. C. (2013). “She looks out for the meals, period”: African American men’s perceptions of how their wives influence their eating behavior and dietary health. Health Psychology, 32(4), 447–455. 10.1037/a0028361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Cancer Society. Cancer Facts & Figures 2019. (2019). Retrieved January 15, 2019, from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf
- American Psychiatric Assoc. Mental Health Disparities: African Americans. https://www.psychiatry.org/File%20Library/Psychiatrists/Cultural-Competency/Mental-Health-Disparities/Mental-Health-Facts-for-African-Americans.pdf
- Ann Hall M. K., Johnson-Turbes A., Fuller F. T., Niles P., Cantey-McDonald S. (2011). Development and implementation of a culturally tailored, community-based intervention to raise awareness of brain health among African Americans. http://digitalscholarship.unlv.edu/jhdrp/http://digitalscholarship.unlv.edu/jhdrp/
- Arlinghaus K. R., Johnston C. A. (2018). Advocating for behavior change with education. American Journal of Lifestyle Medicine, 12(2), 113–116. doi: 10.1177/1559827617745479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnett M. J., Thorpe R. J., Gaskin D. J., Bowie J. V., LaVeist T. A. (2016). Race, medical mistrust, and segregation in primary care as usual source of care: Findings from the exploring health disparities in integrated communities study. Journal of Urban Health, 93(3), 456–467. doi: 10.1007/s11524-016-0054-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azar A. M., Redfield R. R., Rothwell C. J., Director M. B. A. (2017). Health, united states, 2017, with special feature on mortality. https://www.cdc.gov/nchs/data/hus/hus17.pdf
- Bailey R. K., Patel M., Barker N. C., Ali S., Jabeen S. (2011). Major depressive disorder in the African American population. Journal of the National Medical Association, 103(7), 548–557. doi: 10.1016/s0027-9684(15)30380-1. [DOI] [PubMed] [Google Scholar]
- Becker M. H. (1974). The health belief model and sick role behavior. Health Education Monographs, 2(4), 409–419. doi: 10.1177/109019817400200407. [DOI] [Google Scholar]
- Bertera E. M. (2014). Storytelling slide shows to improve diabetes and high blood pressure knowledge and self-efficacy: Three-year results among community dwelling older African Americans. Educational Gerontology, 40(11), 785–800. 10.1080/03601277.2014.894381 [DOI] [Google Scholar]
- Blocker D. E., Romocki L. S., Thomas K. B., Jones B. L., Jackson E. J., Reid L., Campbell M. K. (2006). Knowledge, beliefs and barriers associated with prostate cancer prevention and screening behaviors among African-American men. Journal of the National Medical Association, 98(8), 1286–1295. http://www.ncbi.nlm.nih.gov/pubmed/16916126. Accessed September 9, 2019. [PMC free article] [PubMed] [Google Scholar]
- Boehm S., Coleman-Burns P., Schlenk E. A., Funnell M. M., Parzuchowski J., Powell I. J. (1995). Prostate cancer in African American men: Increasing knowledge and self-efficacy. Journal of Community Health Nursing, 12(3), 161–169. 10.1207/s15327655jchn1203_4 [DOI] [PubMed] [Google Scholar]
- Brawner B. M., Baker J. L., Stewart J., Davis Z. M., Cederbaum J., Jemmott L. S. (2013). The Black Man’s Country Club”: Assessing the feasibility of an HIV risk-reduction program for young heterosexual African American men in barbershops. Family & Community Health, 36(2), 109–118. doi: 10.1097/FCH.0b013e318282b2b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer L. C., Balls-Berry J. E., Dean P., Lackore K., Jenkins S., Hayes S. N. (2017). Fostering african-american improvement in total health (FAITH!): An application of the american heart association’s life’s simple 7TM among midwestern African-Americans. Journal of Racial and Ethnic Health Disparities, 4(2), 269–281. 10.1007/s40615-016-0226-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown E. R., Ojeda V. D., Wyn R., Levan R. Racial and ethnic disparities in access to health insurance and health care. The Henry J. Kaiser Family Foundation; Retrieved September 22, 2019, from https://www.kff.org/disparities-policy/fact-sheet/racial-and-ethnic-disparities-in-access-to/ [Google Scholar]
- Bryant T., Ro M., Rowe R. (2003). The mental health of African American men factsheet. Community Voices, 4. [Google Scholar]
- CDC. (2016). National diabetes surveillance system. Incidence of end-stage renal disease related to diabetes per 100,000 diabetic population (2008). https://gis.cdc.gov/grasp/diabetes/DiabetesAtlas.html.
- CDC D of CP and C. (2019, September 22). Who is at risk for prostate cancer? CDC. https://www.cdc.gov/cancer/prostate/basic_info/risk_factors.htm.
- Chatters L., Taylor H., Nicklett E., Taylor R. (2018). Correlates of objective social isolation from family and friends among older adults. Healthcare, 6(1), 24. doi: 10.3390/healthcare6010024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheatham C. T., Barksdale D. J., Rodgers S. G. (2008). Barriers to health care and health-seeking behaviors faced by Black men. Journal of the American Association of Nurse Practitioners, 20(11), 555–562. doi: 10.1111/j.1745-7599.2008.00359.x. [DOI] [PubMed] [Google Scholar]
- Cuevas A. G., Trudel-Fitzgerald C., Cofie L., Zaitsu M., Allen J., Williams D. R. (2019). Placing prostate cancer disparities within a psychosocial context: Challenges and opportunities for future research. 10.1007/s10552-019-01159-1 [DOI] [PMC free article] [PubMed]
- Daniels E. C., Powe B. D., Metoyer T., McCray G., Baltrus P., Rust G. S. (2012). Increasing knowledge of cardiovascular risk factors among African Americans by use of community health workers: The ABCD community intervention pilot project. Journal of the National Medical Association, 104(3–4), 179–185. 10.1016/s0027-9684(15)30139-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlop D. D., Manheim L. M., Song J., Chang R. W. (2002). Gender and ethnic/racial disparities in health care utilization among older adults.The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 57(4), S221–S233. doi: 10.1093/geronb/57.4.S221. [DOI] [PubMed] [Google Scholar]
- Eley N. T., Namey E., McKenna K., Johnson A. C., Guest G. (2019). Beyond the individual: Social and cultural influences on the health-seeking behaviors of African American Men. American Journal of Men’s Health, 13(1). 10.1177/1557988319829953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Embry M. J., Ellison S. A., & -Committee Chair Jennifer Boyd M. (2013). Diabetes is a community issue: Evidence-based diabetes education outreach programs in the African American population EVIDENCE-BASED DIABETES PROGRAMS 2 acknowledgments. Public health program. http://corescholar.libraries.wright.edu/mph
- Forrester-Anderson I. T. (2005). Prostate cancer screening perceptions, knowledge and behaviors among African American men: Focus group findings. Journal of Health Care for the Poor and Underserved, 16(4 Suppl A), 22–30. doi: 10.1353/hpu.2005.0122. [DOI] [PubMed] [Google Scholar]
- Freimuth V. S., Quinn S. C. (2004). The contributions of health communication to eliminating health disparities. American Journal of Public Health. American Public Health Association Inc. 10.2105/AJPH.94.12.2053 [DOI] [PMC free article] [PubMed]
- Fuller F. T., Johnson-Turbes A., Hall M. A. K., Osuji T. A. (2012). Promoting brain health for African Americans: Evaluating the healthy brain initiative, a community-level demonstration project. Journal of Health Care for the Poor and Underserved, 23(1), 99–113. 10.1353/hpu.2012.0012 [DOI] [PubMed] [Google Scholar]
- Ghisi G. L., Abdallah F., Grace S. L., Thomas S., Oh P. (2014). A systematic review of patient education in cardiac patients: Do they increase knowledge and promote health behavior change? Patient Education and Counseling, 95(2), 160–174. doi: 10.1016/j.pec.2014.01.012. [DOI] [PubMed] [Google Scholar]
- Griffith D. M., Ellis K. R., Allen J. O. (2012). How does health information influence African American men’s health behavior? American Journal of Men’s Health, 6(2), 156–163. 10.1177/1557988311426910 [DOI] [PubMed] [Google Scholar]
- Hasson B. R., Apovian C., Istfan N. (2015). Racial/ethnic differences in insulin resistance and beta cell function: Relationship to racial disparities in type 2 diabetes among African Americans versus Caucasians. Current Obesity Reports, 4(2), 241–249. doi: 10.1007/s13679-015-0150-2. [DOI] [PubMed] [Google Scholar]
- Hastert T. A., Beresford S. A. A., Sheppard L., White E. (2015). Disparities in cancer incidence and mortality by area-level socioeconomic status: A multilevel analysis. Journal of Epidemiology and Community Health, 69(2), 168–176. doi: 10.1136/jech-2014-204417. [DOI] [PubMed] [Google Scholar]
- Howard G., Cushman M., Moy C. S., Oparil S., Muntner P., Lackland D. T., Manly J. J., Flaherty M. L., Judd S. E., Wadley V. G., Long D. L., Howard V. J. (2018). Association of clinical and social factors with excess hypertension risk in black compared with white US adults. Journal of the American Medical Association, 320(13), 1338–1348. doi: 10.1001/jama.2018.13467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard G., Safford M. M., Moy C. S., Howard V. J., Kleindorfer D. O., Unverzagt F. W., Soliman E. Z., Flaherty M. L., McClure L. A., Lackland D. T., Wadley V. G. (2017). Racial differences in the incidence of cardiovascular risk factors in older black and white adults. Journal of the American Geriatrics Society, 65(1), 83–90. 10.1111/jgs.14472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter R. F., De La Haye K., Murray J. M., Badham J., Valente T. W., Clarke M., Kee F. (2019). Social network interventions for health behaviours and outcomes: a systematic review and meta-analysis. PLoS Medicine, 16(9), e1002890. doi: 10.1371/journal.pmed.1002890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones R. A., Steeves R., Williams I. (2010). Family and friend interactions among African-American men deciding whether or not to have a prostate cancer screening. Urologic Nursing, 30(3), 189–193, 166. http://www.ncbi.nlm.nih.gov/pubmed/20648856. Accessed September 19, 2018. [PMC free article] [PubMed] [Google Scholar]
- Jones R. A., Steeves R., Williams I. (2009). Strategies for recruiting African American men into prostate cancer screening studies. Nursing Research, 58(6), 452–456. doi: 10.1097/NNR.0b013e3181b4bade. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lackland D. T. (2014). Racial differences in hypertension: Implications for high blood pressure management. American Journal of Medical Sciences, 348(2), 135–138. doi: 10.1097/MAJ.0000000000000308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin C. A., Knowlton A. R. (2015). Social network assessments and interventions for health behavior change: A critical review. Behavioral Medicine, 41(3), 90–97. doi: 10.1080/08964289.2015.1034645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linnan L. A., D’Angelo H., Harrington C. B. (2014). A literature synthesis of health promotion research in salons and barbershops. American Journal of Preventive Medicine, 47(1), 77–85. 10.1016/j.amepre.2014.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luque J. S., Ross L., Gwede C. K. (2014). Qualitative systematic review of barber-administered health education, promotion, screening and outreach programs in african-american communities. Journal of Community Health, 39(1), 181–190. doi: 10.1007/s10900-013-9744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O A., A W. (2018). An integrative review exploring black men of African and Caribbean backgrounds, their fears of prostate cancer and their attitudes towards screening. Health Education Research, 33(2). 10.1093/HER/CYY001 [DOI] [PubMed] [Google Scholar]
- Okoro O. N., Rutherford C. A., Witherspoon S. F. (2018). Leveraging the family influence of women in prostate cancer efforts targeting African American men. Journal of Racial and Ethnic Health Disparities, 5(4), 820–830. doi: 10.1007/s40615-017-0427-0. [DOI] [PubMed] [Google Scholar]
- Pedersen V. H., Armes J., Ream E. (2012, May). Perceptions of prostate cancer in Black African and Black Caribbean men: A systematic review of the literature. Psycho-Oncology. Psychooncology. 10.1002/pon.2043 [DOI] [PubMed]
- Peña-Purcell N. C., Jiang L., Ory M. G., Hollingsworth R. (2015). Translating an evidence-based diabetes education approach into rural African-American communities: The “wisdom, power, control” program. Diabetes Spectrum, 28(2), 106–115. 10.2337/diaspect.28.2.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plowden K. O., Miller J. L. (2000). Motivators of health seeking behavior in urban African-American men: An exploration of triggers and barriers. Journal of National Black Nurses’ Association: JNBNA, 11(1), 15–20. http://www.ncbi.nlm.nih.gov/pubmed/11854947 [PubMed] [Google Scholar]
- Plowden K. O., Young A. E. (2003). Sociostructural factors influencing health behaviors of urban African-American men. Journal of National Black Nurses’ Association, 14(1), 45–51. http://www.ncbi.nlm.nih.gov/pubmed/15259998. Accessed September 9, 2019. [PubMed] [Google Scholar]
- Primm A. B., Vasquez M. J. T., Mays R. A., Sammons-Posey D., McKnight-Eily L. R., Presley-Cantrell L. R., McGuire L. C., Chapman D. P., Perry G. S. (2010). The role of public health in addressing racial and ethnic disparities in mental health and mental illness. Preventing Chronic Disease, 7(1), A20. http://www.ncbi.nlm.nih.gov/pubmed/20040235 [PMC free article] [PubMed] [Google Scholar]
- Reynolds D. (2008). Prostate cancer screening in African American men: Barriers and methods for improvement. American Journal of Men’s Health, 2(2), 172–177. doi: 10.1177/1557988307312784. [DOI] [PubMed] [Google Scholar]
- Rose L. E., Kim M. T., Dennison C. R., Hill M. N. (2000). The contexts of adherence for African Americans with high blood pressure. Journal of Advanced Nursing, 32(3), 587–594. doi: 10.1046/j.1365-2648.2000.01538.x. [DOI] [PubMed] [Google Scholar]
- Sandiford L., D’Errico E. M. (2016). Facilitating shared decision making about prostate cancer screening among African American men. Oncology Nursing Forum, 43(1), 86–92. 10.1188/16.ONF.86-92 [DOI] [PubMed] [Google Scholar]
- Satcher D. (2003). Overlooked and underserved: improving the health of men of color. American Journal of Public Health, 93(5), 707–709. doi: 10.2105/AJPH.93.5.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shabazz D. L. (2016). Barbershops as cultural forums for African American males. Journal of Black Studies, 47(4), 295–312. doi: 10.1177/0021934716629337. [DOI] [Google Scholar]
- Singh G. K., Daus G. P., Allender M., Ramey C. T., Martin E. K., Perry C., Reyes A. A. D. L., Vedamuthu I. P. (2017). Social determinants of health in the United States: Addressing major health inequality trends for the nation, 1935–2016. International Journal of Maternal and Child Health and AIDS, 6(2), 139–164. doi: 10.21106/ijma.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith Z. L., Eggener S. E., Murphy A. B. (2017). African-American prostate cancer disparities. Current Urology Reports, 18(10), 81. doi: 10.1007/s11934-017-0724-5. [DOI] [PubMed] [Google Scholar]
- Taitt H. E. (2018, November 1). Global Trends and Prostate Cancer: A Review of Incidence, Detection, and Mortality as Influenced by Race, Ethnicity, and Geographic Location. American Journal of Men’s Health. SAGE Publications Inc; 10.1177/1557988318798279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor R. J., Chatters L. M., Taylor H. O., Carr D. (2019). Race and objective social isolation: Older African Americans, black caribbeans, and non-hispanic whites. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 74(8), 1429–1440. doi: 10.1093/geronb/gby114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas S. B., Fine M. J., Ibrahim S. A. (2004). Health disparities: The importance of culture and health communication. American Journal of Public Health. American Public Health Association Inc; 10.2105/AJPH.94.12.2050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Census Bureau. (2018). Narrative profiles 2014—2018 ACS 5-year narrative profile Duluth city, Minnesota. https://www.census.gov/acs/www/data/data-tables-and-tools/narrative-profiles/2018/report.php?geotype=place&state=27&place=17000
- Valenstein M., Blow F. C., Copeland L. A. (2004). Poor antipsychotic adherence among patients with schizophrenia: Medication and patient factors. Schizophrenia Bulletin, 30(2), 255–264. doi: 10.1093/oxfordjournals.schbul.a007076. [DOI] [PubMed] [Google Scholar]
- Valente T. W., Palinkas L. A., Czaja S., Chu K.-H., Brown C. H. (2015). Social network analysis for program implementation. PLoS One, 10(6), e0131712. doi: 10.1371/journal.pone.0131712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valente T. W., Ritt-Olson A., Stacy A., Unger J. B., Okamoto J., Sussman S. (2007). Peer acceleration: Effects of a social network tailored substance abuse prevention program among high-risk adolescents. Addiction, 102(11), 1804–1815. doi: 10.1111/j.1360-0443.2007.01992.x. [DOI] [PubMed] [Google Scholar]
- Williams J., Wilson V. (2019, December 2). Black workers endure persistent racial disparities in employment outcomes. Economic Policy Institute. https://www.epi.org/publication/labor-day-2019-racial-disparities-in-employment/. Published 2019
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_File for Culturally Responsive Health Promotion to Address Health Disparities in African American Men: A Program Impact Evaluation by Olihe N. Okoro, Chantele S. Nelson, Stephan P. Witherspoon, Salaam F. Witherspoon and Glenn E. Simmons in American Journal of Men’s Health