Clinicians involved in previous pandemics encountered mental health problems, and their experience predicts that clinicians working in the current COVID-19 pandemic will face similar issues. This article reviews what we know about how to prevent these problems and manage them as they develop.
Abstract
Previous pandemics have seen high psychiatric morbidity among health care workers. Protecting clinician mental health in the aftermath of coronavirus disease 2019 (COVID-19) requires an evidence-based approach to developing and deploying comprehensive clinician mental health support. In a narrative review of 96 articles addressing clinician mental health in COVID-19 and prior pandemics, 7 themes emerged: 1) the need for resilience and stress reduction training; 2) providing for clinicians' basic needs (food, drink, adequate rest, quarantine-appropriate housing, transportation, child care, personal protective equipment); 3) the importance of specialized training for pandemic-induced changes in job roles; 4) recognition and clear communication from leadership; 5) acknowledgment of and strategies for addressing moral injury; 6) the need for peer and social support interventions; and 7) normalization and provision of mental health support programs. In addition to the literature review, in collaboration with the Collaborative for Healing and Renewal in Medicine (CHARM) network, the authors gathered practice guidelines and resources from health care organizations and professional societies worldwide to synthesize a list of resources deemed high-yield by well-being leaders. Studies of previous pandemics demonstrate heightened distress in health care workers years after the event. The COVID-19 pandemic presents unique challenges that surpass those of previous pandemics, suggesting a significant mental health toll on clinicians. Long-term, proactive individual, organizational, and societal infrastructures for clinician mental health support are needed to mitigate the psychological costs of providing care during the COVID-19 pandemic.
Key SummaryPoints
The COVID-19 pandemic presents unprecedented psychological threats to clinician well-being; evidence from previous epidemics and disasters underscore clinicians' high risk for long-term mental health issues and emphasize the need for comprehensive mental health support during the COVID-19 recovery phase.
Addressing clinician wellness requires proactive support, because this population is known for not seeking support and for putting others' needs before their own.
Developing institutional and societal infrastructure that ensures clinicians' basic needs are met and arms them with psychological and social support tools is necessary to mitigate the known psychological costs of providing care during a pandemic.
The coronavirus disease 2019 (COVID-19) pandemic has exacerbated preexisting burnout and moral injury in health care professionals. Clinicians are dying not only of physical manifestations of COVID-19, but also of the emotional and mental health repercussions of caring for persons who are suffering without loved ones by their side (1–3). Concerns about adequate personal protective equipment (PPE), reliable testing, absence of specific treatments, risk for infection to self and family, lack of access to up-to-date information among ever-changing guidelines, and uncertainty about containment of disease also threaten clinician well-being (4, 5).
Many health organizations have already committed resources to clinician well-being, including chief wellness officer positions and well-being programs (6). These institutions must adapt their existing well-being infrastructure to meet evolving needs. Other organizations have yet to establish such programs and will benefit from a blueprint for a coordinated, systemic approach. Evidence from previous epidemics and disasters underscore clinicians' high risk for long-term mental health issues and emphasize the need for continued support during and after the pandemic (7–10).
The COVID-19 pandemic has necessitated rapid development and deployment of innovative solutions in medicine, including well-being resources for clinicians. As we look to an uncertain future, a conceptual framework for how to develop and deploy these resources will facilitate well-being endeavors and provide a foundation for addressing long-term needs. We performed a literature review and compiled a comprehensive guide to clinician mental health and well-being resources compiled by well-being leaders. We provide a conceptual map for allocation of these resources at the individual, organizational, and societal levels, focusing on addressing clinician well-being needs in the postpandemic phase.
Methods
This narrative review targeted the existing literature on clinician mental health and wellness needs in response to both COVID-19 and previous pandemics. PsycInfo, PubMed, SCOPUS, and Web of Science were searched by using the keywords “covid* OR corona*” “mental health”, “trauma”, “resilienc*”, “coping”, “anxiety”, “burnout”, “wellness OR wellbeing”, “occupational stress” “frontline OR medical OR hospital OR health care workers OR medical students OR physician OR nurse” “pandemic OR outbreak OR surge”. Articles were included if they provided evidence on 1) prevalence of mental health symptoms during or after the pandemic and 2) individual, organizational-level, or societal-level responses to or assessment of mental health in health care workers. The dates of the literature search were July 2004 (to capture the first severe acute respiratory syndrome [SARS] outbreak) through May 2020. Ongoing updates to the initial search were conducted through the end of May 2020 to capture additional in-press articles. Each author was responsible for searching 1 database, and included articles were reviewed by all 4 authors to determine their relevance. This peer-review process yielded 96 articles included in the narrative review.
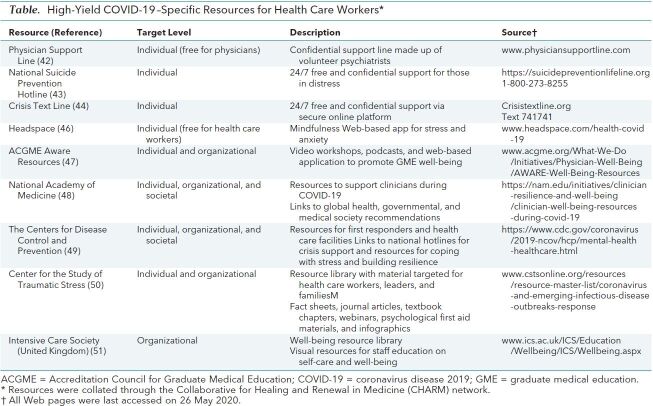
In addition to the comprehensive literature search described, we peer-reviewed well-being resources gathered by the Collaborative for Healing and Renewal in Medicine (CHARM) network. The CHARM network is a group of medical educators, leaders in academic medicine, experts in burnout research and interventions, and trainees working together to promote well-being among trainees and practicing physicians (11). This action-oriented group, through regular teleconferences and electronic communication, focused on creating deliverables for widespread dissemination during the COVID-19 pandemic to support the well-being of health care workers and their organizations. We reviewed practice guidelines and resources from numerous health care organizations and professional societies worldwide across various specialties (Table). Through the CHARM network, we gathered and then reviewed and annotated various media, including Web site resources, podcasts, popular media articles, Web-based applications, and any resource deemed high-yield by well-being leaders.
Table. High-Yield COVID-19–Specific Resources for Health Care Workers*.
Results of the Literature Search
Intervention Levels
Clinician well-being efforts fall into 3 interrelated categories: individual (for example, emotional awareness and self-care), organizational (for example, mental health support programs, engaged leadership), and societal (for example, supportive culture in medicine, national policies that enhance well-being) (12) (Figure).
Figure. Proposed framework of clinician well-being resources.
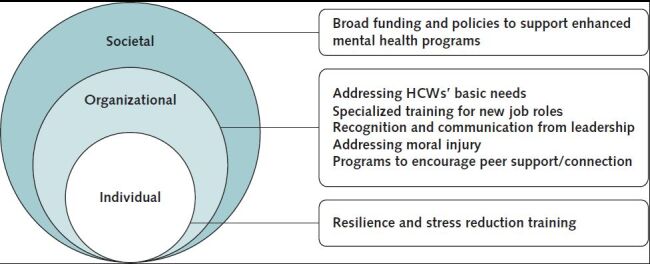
HCW = health care worker.
This review yielded insight in 2 areas: the prevalence of clinician mental health needs during and after a pandemic, and postpandemic strategies for comprehensive clinician mental health support.
Prevalence of Clinician Mental Health Needs During and After Pandemics
Previous Pandemics
The mental health toll of past pandemics on health care workers has been well documented. Chong and colleagues (8) estimated 75% psychiatric morbidity among health care workers in a tertiary hospital in China during the recovery phase of the SARS epidemic. Goulia and colleagues (13) found that 56.7% of health care worker participants reported moderately high anxiety during the A/H1N1 pandemic in Greece, noting that degree of worry was an independent correlate of anxiety. Maunder and colleagues (14) reported significantly higher levels of distress, burnout, and posttraumatic stress in health care workers who treated patients with SARS compared with their colleagues who did not have direct contact with patients with SARS. Health fear, social isolation, and job stress were mediating factors. Two months into the SARS pandemic, Chan and Huak (15) found that about 20% of health care workers in a hospital in Singapore reported symptoms indicative of posttraumatic stress. After the SARS outbreak in Taiwan, Bai and colleagues (16) reported a range of stress-related responses, such as acute stress disorder, feelings of stigmatization and rejection, and reluctance to go to work.
The COVID-19 Pandemic
There has been growing evidence of distress and mental health issues among health care workers treating patients with COVID-19. Dzau and colleagues (6) noted moral distress, anxiety, and suicide as negative effects of the COVID-19 pandemic and caution about possible increases in burnout. Depression, anxiety, insomnia, and distress have been reported among health care workers in China during this pandemic (17). A systematic review of COVID-19–related studies reported stress, anxiety, depression, and insomnia among health care workers (18). Excessive work hours, inadequate PPE, infection rate among medical staff, feeling a lack of support, and extensive media coverage were noted as factors associated with adverse psychological outcomes. In trying to understand anxiety associated with COVID-19, Maben and Bridges (19) outlined possible mental health–related issues in nurses in the United Kingdom, such as moral distress and fatigue, discomfort, and difficulties in communication due to wearing masks and full PPE. Stigma among the larger community and being perceived as a threat to safety of others were other issues that they outlined.
Kisely and colleagues (10) conducted a systematic analysis of studies documenting the mental health effects of pandemics, such as COVID-19, SARS, Middle East respiratory syndrome, H1N1, H7N9, and Ebola. They reported that staff in direct contact with patients had higher levels of posttraumatic stress and psychological distress. Women, younger clinicians, and parents with dependent children were demographic factors associated with greater psychological distress. Shanafelt and colleagues (4) found that 8 themes emerged in discussions with health care workers: inadequate PPE, exposure to self and carrying of infection to family members, lack of rapid testing availability in the face of symptom development, exposing others at work, access to child care resources, support for other personal and family needs, uncertainty about organizational support, lack of up-to-date information and communication, and feelings of inadequacy if deployed to new areas. A qualitative study with general surgery residents in 2 Boston centers found that the health of their family, risk for being infected by patients, risk for carrying infection to family members, anticipatory overwork due to patients with COVID-19, and risk for infecting patients were common concerns (20). In a survey of surgical residents, more than one half of respondents reported psychological strain as a result of the pandemic (21).
Unique Challenges of COVID-19 Compared With Previous Pandemics
Environments that combine high levels of anxiety with prolonged uncertainty and reduced agency place clinicians at high risk for developing persistent stress exposure syndromes and burnout (22). The COVID-19 pandemic presents unprecedented challenges due to prolonged uncertainty and heightened anxiety, immediate threat to personal and family safety, social isolation, witnessing physical suffering and death, and evolving professional demands. These individual stressors combine to induce hyperarousal, hypervigilance, sleep disturbance, intrusive thoughts, depression, and grief (23). Schreiber and colleagues (24) reported that when first responders experienced 6 or more cumulative stress factors or 3 specific factors (performing duties outside their perceived skill set; witnessing a coworker become sick or injured, or die; and feeling that their own life is in danger), they were at higher risk for developing posttraumatic stress disorder 3 months later.
Narrative Themes
Seven themes, and associated interventions, emerged from the literature (Figure): 1) the need for resilience and stress reduction training; 2) providing for clinicians' basic needs (food, drink, adequate rest, quarantine-appropriate housing, transportation, child care, PPE); 3) the importance of specialized training for pandemic-induced changes in job roles; 4) recognition and clear communication from leadership; 5) acknowledgment of and strategies for addressing moral injury; 6) the need for peer and social support interventions and; 7) normalization and provision of mental health support programs.
Theme 1: The Need for Resilience and Stress Reduction Training
Across studies, there was an emphasis on implementing training programs that target clinician self-care, normalize anticipated psychological response to crisis, and promote adaptive response and self-efficacy (22, 24–27). Schreiber and colleagues' (24) anticipate, plan, and deter (APD) model incorporates pre-event training (“anticipate”), explaining the nature of cumulative responder stressors and anticipated stress reactions; development of a personal resilience plan (“plan”) to identify and document anticipated challenges and positive coping strategies; and trains participants on self-monitoring stress exposure to know when to implement personal resilience plans (“deter”). Albott and colleagues (22) developed a psychological resilience intervention that focused on self-care, self-efficacy, and social connection while providing rapid ongoing access to mental health support. Blake and colleagues (26) developed and disseminated a digital e-package with evidence-based guidance for psychological well-being. The content focused on self-care strategies at work and home, managing emotions, and encouraging help-seeking behavior. Fessell and Cherniss (25) identified actionable “micropractices” for physicians to implement during the workday, such as wellness self-checks and naming emotions.
Practice implications.
Given the demonstrated value of stress reduction and resiliency training, integrating these practices as a key part of clinician training may reduce distress.
Theme 2: Providing for Clinicians' Basic Needs
Strategies for addressing clinicians' basic needs during the COVID-19 pandemic ranged from covering basic meals and transportation needs to establishing a “well-being area” within the hospital in which staff and volunteers could rest (28) and providing living quarters, complete with food and living supplies, so that clinicians to safely quarantine from family (4, 29–31). One Chinese hospital helped clinicians create videos of their work routines to share with family to assuage concerns (29). Institutions in urban settings, where most rely on public transit, chose to subsidize clinicians' transportation, exploring bicycle and car rental options (30). Child care coverage and PPE are other essential needs (4, 31, 32). Some cities provided centers for children of health care workers, whereas other institutions developed volunteer programs connecting nonessential employees with frontline clinicians (30).
Practice implications.
Ensuring that clinicians' basic needs (food, adequate rest, shelter, transportation, child care, and PPE) are met is essential for their psychological well-being. Although not mentioned in the reviewed articles, the unfolding financial impact of the COVID-19 pandemic is another stressor whose effect has yet to be measured.
Theme 3: The Importance of Specialized Training for New Job Roles
Delivering care during a pandemic requires operating in a high-anxiety environment and, in many cases, being prepared to assume new professional roles to meet evolving needs. Training clinicians on infection control was shown to alleviate stress (33), because it arms them with protective tools. Formalized training on how to identify and respond to patients' psychological distress was requested as another strategy for clinician support (29). Finally, redeployment to a new clinical role in the case of a patient surge was a core source of anxiety that could be addressed through assessment of clinician skill sets before redeployment, targeted training, and improved information about redeployment plans (27, 34).
Practice implications.
Hospitals should consider adopting specialized skills assessment and training programs and use clear communication practices around redeployment to prepare for future needs.
Theme 4: Recognition and Clear Communication From Leadership
Many articles spoke to the importance of clinicians receiving recognition from leadership and the effect this had on well-being. Receiving recognition from hospital and government leaders was a motivational factor that supported COVID-19 clinicians' ability to continue delivering care (5). Transparent, bidirectional communication empowers clinical teams and improves morale (31, 32). Delivering current, reliable, and reassuring messaging improves transmission of critical information to clinical teams (30). Effective strategies include synthesizing information into a daily digest that links to a comprehensive resource page and providing weekly virtual town halls to disseminate critical information (30).
Practice implications.
Leadership can leverage communication strategies to provide clinicians with up-to-date information and reassurance.
Theme 5: Acknowledgment of and Strategies for Addressing Moral Injury
The ethical, social, and professional obligations toward their profession are frequently reported as the core motivator for clinicians' decision to provide care while putting themselves at risk (5, 35). This commitment to serving others, even at the cost of their own well-being, makes clinicians a uniquely vulnerable population. Moral injury is defined as psychological distress caused by a betrayal of what is right by someone in authority in a high-stakes situation (36), or witnessing, perpetrating, or failing to prevent acts that transgress core moral beliefs (37). The COVID-19 pandemic presents multiple potential sources of moral injury for clinicians, such as determining which patients will not receive life support owing to inadequate resources or bearing witness to (and having to enforce) policies that lead to patients dying alone (31). Williamson and colleagues (38) identified a set of strategies for addressing moral injury in frontline COVID-19 clinicians. They recommend making clinicians aware of the possibility of moral injury and associated symptoms. Encourage clinicians to seek informal support from colleagues, managers, or chaplains and provide rapid access to professional help; however, it is known that those suffering from moral injury often fail to discuss it owing to shame and guilt. As a result, leadership must proactively and routinely monitor the psychological well-being of their teams.
Practice implications.
Clinicians are unlikely to disclose moral injury. Psychological well-being should proactively be assessed, and both informal and professional support should be readily available to clinicians.
Theme 6: The Need for Peer and Social Support Interventions
Depriving humans of social connection comes at a high psychological cost (33), and the COVID-19 pandemic interferes with the ability to connect with colleagues and even one's own family owing to mandatory infection control precautions. Social support is associated with decreased stress and anxiety and increased self-efficacy and sleep quality (39). To sustain clinician well-being, heightened attention must be paid to fulfilling their social support needs. Whereas peer support occurs on an individual level, institutional programs provide a structured approach to building peer support and connection. One innovative strategy by Albott and colleagues (22) involved implementing a “battle buddy” model borrowed from the military that paired individuals on the basis of clinical area of practice, career stage, and life circumstance. Each partner in the team engages in daily conversation and looks out for the other's well-being. If distress is observed, mental health support is proactively deployed. Walton and colleagues (31) provide a comprehensive description of the physical, behavioral, emotional, and cognitive indicators of acute stress reactions; training clinicians to be aware of these reactions, in themselves and others, may allow for better peer support and intervention. Other proposed solutions include routinely holding Schwartz rounds, an interprofessional forum for health care professionals to discuss the emotional, social, and ethical challenges of work, during changing shift periods (40).
Practice implications.
Providing routine opportunities for social connection can improve clinician well-being.
Theme 7: Normalization and Provision of Mental Health Support Programs
The provision of clinician mental health support is not currently standard practice in the United States. Self-report questionnaires and observations of frontline clinicians during the COVID-19 pandemic demonstrated that they are unlikely to seek out psychological support resources (5, 29, 38), despite the availability of these resources. Leadership can normalize mental health support by modeling self-care and help-seeking behaviors (31), ensuring that available mental health resources are well-publicized, and developing a culture of caring with frequent check-ins with colleagues to assess psychological well-being and a protocol for professional referrals as needed. Establishing opportunities for clinicians to anonymously share concerns allows them to safely advocate for themselves and their patients (6). On a societal level, it is necessary to establish new infrastructure that will sustain and supplement existing clinician support programs. Dzau and colleagues (6) recommend allocation of federal funding to care for clinicians who have been impacted by their COVID-19 service and establishing a national epidemiologic tracking program to track clinician well-being and the effect of wellness interventions. Developing multidisciplinary mental health teams at the regional and national levels can allow clinicians greater access to needed resources (18, 41).
Practice implications.
Routine provision of mental health education and support needs to be delivered proactively to protect long-term clinician well-being. Federal funding for clinician well-being is needed to track clinician wellness and establish the resources necessary to care for those negatively affected by their COVID-19 service.
High-Yield COVID-19–Specific Resources for Health Care Workers
Crisis and virtual mental health services must be easily accessible for health care workers. The Table provides details on the resources discussed in this section.
The Physician Support line (42) is a national, free, and confidential support line service made up of volunteer psychiatrists, joined together to provide peer support for their physician colleagues. For those in crisis, additional resources include the National Suicide Prevention Hotline (43) and Crisis Text Line (44) which operate 24/7.
Mindfulness resources for emotional regulation have been shown to decrease physician burnout (45). Headspace (46), a popular mindfulness Web-based application, is offering free membership to U.S.-based health care professionals to help cope with stress and anxiety with resources for sleep, meditation, and movement exercises. The Accreditation Council for Graduate Medical Education (ACGME) AWARE Well-Being resources (47) include video workshops, podcasts, and a Web-based application designed to promote well-being in the graduate medical education community. The Well-Being in the Time of COVID-19 podcast by Stuart Slavin, MD, (ACGME's Senior Scholar for Well-being) provides well-being strategies for residents, fellows, and other clinicians from resources that include psychology and psychiatry, peer support programming, the military and Veterans Affairs, and literature for support of first responders to mass casualty events.
The National Academy of Medicine (48) Web site is a clearinghouse of resources to support the health and well-being of clinicians that includes links to numerous global health, governmental, and medical society recommendations. The Centers for Disease Control and Prevention (49) collated a comprehensive list of factors to consider during COVID-19 related to coping and stress, including considerations for first responders, and also serves as a resource for communities, families, and people at higher risk for serious illness. The Center for the Study of Traumatic Stress (50) is a high-yield, well-edited resource library with material targeted for health care workers, leaders, and families, including fact sheets, journal articles, textbook chapters, webinars, and infographics within the public domain. The United Kingdom's Intensive Care Society (51) offers a well-being resource library includes visual resources that can be displayed to educate staff on self-care, sustaining staff well-being during COVID-19, and specific critical care workplace interventions to improve local environments.
Identifying Health Care Workers at Highest Risk for Posttraumatic Stress and Mood Disorders in Response to the Pandemic
Across studies, frontline workers are at highest risk for developing acute stress, depression, anxiety, and insomnia (17, 33, 52). Approximately 45% of 1153 Italian COVID-19 frontline clinicians experienced at least 1 physical symptom of burnout in the previous 4 weeks. Increased irritability, change in food habits, difficulty falling asleep, and muscle tension were frequently experienced by the majority of respondents (53). One COVID-19 study showed twice the rates of anxiety and depression in frontline providers compared with nonclinical staff (54), whereas a SARS study showed psychiatric morbidity in hospital workers to be 3 times higher than the general population (8). Nurses may be more likely than other clinicians to show symptoms of posttraumatic stress (33). Loss of professional control—for example, due to changes in work assignment or work security—is associated with high levels of distress (33). A perception of inadequate institutional support, as reflected by feedback from frontline staff not reaching hospital administrators, in adequate health care insurance or compensation, or insufficient psychological support from employers, were all risk factors for poor mental health (33).
Tools for routine assessment of mental health status, such as Zung's self-rating depression scale and self-rating anxiety scale for self-monitoring (55–57); training health care workers to identify physical, behavioral, emotional, and cognitive indices of distress in themselves and colleagues; and regular visits from mental health clinicians to assess the well-being of frontline providers are needed (18, 31, 58).
Studies of previous pandemics demonstrate heightened distress in health care workers more than 2 years after the event (7). However, COVID-19 presents challenges not seen in previous pandemics, including a protracted timeline, severe financial implications, and a global scale. As a result, its effects on the mental health of health care workers can be expected to exceed those observed in previous pandemics. Proactive mental health support for health care providers is essential for protecting their long-term mental health (59).
In conclusion, clinicians require proactive psychological protection specifically because they are a population known for putting others' needs before their own. To mitigate the known psychological costs of providing care during a pandemic and recovering from associated experiences, comprehensive institutional and societal infrastructure for clinician well-being is needed, especially as we enter this unprecedented, global postpandemic era. This support should target resilience and stress reduction training, ensure that clinicians' basic needs are met, provide routine opportunities for social connection, and proactively normalize and deliver mental health care to clinicians.
Footnotes
This article was published at Annals.org on 21 August 2020.
References
- 1. Watkins A, Rothfeld M, Rashbaum WK, Rosenthal BM. Top E.R. doctor who treated virus patients dies by suicide. New York Times. 27 April 2020. Accessed at www.nytimes.com/2020/04/27/nyregion/new-york-city-doctor-suicide-coronavirus.html on 26 May 2020.
- 2. Edelman S, Moore T, Narizhnaya K, Balsamini D. EMT John Mondello kills himself after less than three months on the job. New York Post. 25 April 2020. Accessed at https://nypost.com/2020/04/25/nyc-emt-commits-suicide-with-gun-belonging-to-his-dad/ on 26 May 2020.
- 3. Jun J, Tucker S, Melnyk BM. Clinician mental health and well-being during global healthcare crises: evidence learned from prior epidemics for COVID-19 pandemic [Editorial]. Worldviews Evid Based Nurs. 2020;17:182-184. [PMID: 32246793] doi:10.1111/wvn.12439 [DOI] [PubMed]
- 4. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020. [PMID: 32259193] doi:10.1001/jama.2020.5893 [DOI] [PubMed]
- 5. Cai H, Tu B, Ma J, et al. Psychological impact and coping strategies of frontline medical staff in hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China. Med Sci Monit. 2020;26:e924171. [PMID: 32291383] doi:10.12659/MSM.924171 [DOI] [PMC free article] [PubMed]
- 6. Dzau VJ, Kirch D, Nasca T. Preventing a parallel pandemic—a national strategy to protect clinicians' well-being. N Engl J Med. 2020;383:513-515. [PMID: 32402153] doi:10.1056/NEJMp2011027 [DOI] [PubMed]
- 7. Maunder RG, Lancee WJ, Balderson KE, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12:1924-32. [PMID: 17326946] [DOI] [PMC free article] [PubMed]
- 8. Chong MY, Wang WC, Hsieh WC, et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry. 2004;185:127-33. [PMID: 15286063] [DOI] [PubMed]
- 9. Smith EC, Holmes L, Burkle FM. The physical and mental health challenges experienced by 9/11 first responders and recovery workers: a review of the literature. Prehosp Disaster Med. 2019;34:625-631. [PMID: 31625489] doi:10.1017/S1049023X19004989 [DOI] [PubMed]
- 10. Kisely S, Warren N, McMahon L, et al. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. [PMID: 32371466] doi:10.1136/bmj.m1642 [DOI] [PMC free article] [PubMed]
- 11. Alliance for Academic Internal Medicine. Wellness and resiliency: CHARM. Accessed at www.im.org/resources/wellness-resiliency/charm on 26 May 2020.
- 12. Thomas LR, Ripp JA, West CP. Charter on physician well-being. JAMA. 2018;319:1541-1542. [PMID: 29596592] doi:10.1001/jama.2018.1331 [DOI] [PubMed]
- 13. Goulia P, Mantas C, Dimitroula D, et al. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect Dis. 2010;10:322. [PMID: 21062471] doi:10.1186/1471-2334-10-322 [DOI] [PMC free article] [PubMed]
- 14. Maunder RG, Lancee WJ, Rourke S, et al. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom Med. 2004 Nov-Dec;66:938-42. [PMID: 15564361] [DOI] [PubMed]
- 15. Chan AO, Huak CY. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med (Lond). 2004;54:190-6. [PMID: 15133143] [DOI] [PMC free article] [PubMed]
- 16. Bai Y, Lin CC, Lin CY, et al. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. 2004;55:1055-7. [PMID: 15345768] [DOI] [PubMed]
- 17. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. [PMID: 32202646] doi:10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed]
- 18. Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic—a review [Letter]. Asian J Psychiatr. 2020;51:102119. [PMID: 32339895] doi:10.1016/j.ajp.2020.102119 [DOI] [PMC free article] [PubMed]
- 19. Maben J, Bridges J. Covid-19: Supporting nurses' psychological and mental health [Editorial]. J Clin Nurs. 2020;29:2742-2750. [PMID: 32320509] doi:10.1111/jocn.15307 [DOI] [PMC free article] [PubMed]
- 20. He K, Stolarski A, Whang E, et al. Addressing general surgery residents' concerns in the early phase of the COVID-19 pandemic. J Surg Educ. 2020 Jul - Aug;77:735-738. [PMID: 32354684] doi:10.1016/j.jsurg.2020.04.003 [DOI] [PMC free article] [PubMed]
- 21. Kapila AK, Farid Y, Kapila V, et al. The perspective of surgical residents on current and future training in light of the COVID-19 pandemic [Letter]. Br J Surg. 2020. [PMID: 32567688] doi:10.1002/bjs.11761 [DOI] [PMC free article] [PubMed]
- 22. Albott CS, Wozniak JR, McGlinch BP, et al. Battle buddies: rapid deployment of a psychological resilience intervention for health care workers during the COVID-19 pandemic. Anesth Analg. 2020;131:43-54. [PMID: 32345861] doi:10.1213/ANE.0000000000004912 [DOI] [PMC free article] [PubMed]
- 23. Palm KM, Polusny MA, Follette VM. Vicarious traumatization: potential hazards and interventions for disaster and trauma workers. Prehosp Disaster Med. 2004 Jan-Mar;19:73-8. [PMID: 15453162] [DOI] [PubMed]
- 24. Schreiber M, Cates DS, Formanski S, et al. Maximizing the resilience of healthcare workers in multi-hazard events: lessons from the 2014-2015 ebola response in Africa. Mil Med. 2019;184:114-120. [PMID: 30901435] doi:10.1093/milmed/usy400 [DOI] [PubMed]
- 25. Fessell D, Cherniss C. Coronavirus disease 2019 (COVID-19) and beyond: micropractices for burnout prevention and emotional wellness. J Am Coll Radiol. 2020;17:746-748. [PMID: 32208139] doi:10.1016/j.jacr.2020.03.013 [DOI] [PMC free article] [PubMed]
- 26. Blake H, Bermingham F, Johnson G, et al. Mitigating the psychological impact of COVID-19 on healthcare workers: a digital learning package. Int J Environ Res Public Health. 2020;17. [PMID: 32357424] doi:10.3390/ijerph17092997 [DOI] [PMC free article] [PubMed]
- 27. Aiello A, Khayeri MY, Raja S, et al. Resilience training for hospital workers in anticipation of an influenza pandemic. J Contin Educ Health Prof. 2011;31:15-20. [PMID: 21425355] doi:10.1002/chp.20096 [DOI] [PubMed]
- 28. Rimmer A. Covid-19: staff at Nightingale Hospital in London get wellbeing area courtesy of John Lewis. BMJ. 2020;369:m1451. [PMID: 32273262] doi:10.1136/bmj.m1451 [DOI] [PubMed]
- 29. Chen Q, Liang M, Li Y, et al. Mental health care for medical staff in China during the COVID-19 outbreak [Letter]. Lancet Psychiatry. 2020;7:e15-e16. [PMID: 32085839] doi:10.1016/S2215-0366(20)30078-X [DOI] [PMC free article] [PubMed]
- 30. Ripp J, Peccoralo L, Charney D. Attending to the emotional well-being of the health care workforce in a New York City health system during the COVID-19 pandemic. Acad Med. 2020;95:1136-1139. [PMID: 32282344] doi:10.1097/ACM.0000000000003414 [DOI] [PMC free article] [PubMed]
- 31. Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care. 2020;9:241-247. [PMID: 32342698] doi:10.1177/2048872620922795 [DOI] [PMC free article] [PubMed]
- 32. Vinson AE. Nurturing morale. Anesth Analg. 2020;131:395-397. [PMID: 32398426] doi:10.1213/ANE.0000000000004965 [DOI] [PubMed]
- 33. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912-920. [PMID: 32112714] doi:10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed]
- 34. Farid Y, Kapila AK, Schettino M, et al. Assessing the skillset of surgeons facing the COVID-19 pandemic [Letter]. Br J Surg. 2020. [PMID: 32497244] doi:10.1002/bjs.11723 [DOI] [PMC free article] [PubMed]
- 35. Khalid I, Khalid TJ, Qabajah MR, et al. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin Med Res. 2016;14:7-14. [PMID: 26847480] doi:10.3121/cmr.2016.1303 [DOI] [PMC free article] [PubMed]
- 36. Shay J. Casualties. Daedalus. 2011;140:179-88. [PMID: 21898967] [DOI] [PubMed]
- 37. Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29:695-706. [PMID: 19683376] doi:10.1016/j.cpr.2009.07.003 [DOI] [PubMed]
- 38. Williamson V, Murphy D, Greenberg N. COVID-19 and experiences of moral injury in front-line key workers [Editorial]. Occup Med (Lond). 2020;70:317-319. [PMID: 32239155] doi:10.1093/occmed/kqaa052 [DOI] [PMC free article] [PubMed]
- 39. Xiao H, Zhang Y, Kong D, et al. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26:e923549. [PMID: 32132521] doi:10.12659/MSM.923549 [DOI] [PMC free article] [PubMed]
- 40. Saniasiaya J, Ramasamy K. Schwartz rounds for healthcare personnel in coping with COVID-19 pandemic [Letter]. Postgrad Med J. 2020;96:425. [PMID: 32345755] doi:10.1136/postgradmedj-2020-137806 [DOI] [PMC free article] [PubMed]
- 41. Bao Y, Sun Y, Meng S, et al. 2019-nCoV epidemic: address mental health care to empower society [Letter]. Lancet. 2020;395:e37-e38. [PMID: 32043982] doi:10.1016/S0140-6736(20)30309-3 [DOI] [PMC free article] [PubMed]
- 42.Physician Support Line. Accessed at www.physiciansupportline.com on 26 May 2020.
- 43.National Suicide Prevention Lifeline. Accessed at https://suicidepreventionlifeline.org on 26 May 2020.
- 44.Crisis Text Line. Accessed at www.crisistextline.org on 26 May 2020.
- 45. Goodman MJ, Schorling JB. A mindfulness course decreases burnout and improves well-being among healthcare providers. Int J Psychiatry Med. 2012;43:119-28. [PMID: 22849035] [DOI] [PubMed]
- 46.Headspace. Accessed at www.headspace.com/health-covid-19 on 26 May 2020.
- 47.AWARE well-being resources. Accreditation Council for Graduate Medical Education. Accessed at www.acgme.org/What-We-Do/Initiatives/Physician-Well-Being/AWARE-Well-Being-Resources on 26 May 2020.
- 48. National Academy of Medicine. National Academy of Medicine resources to support the health and well-being of clinicians during the COVID-19 outbreak. Accessed at https://nam.edu/initiatives/clinician-resilience-and-well-being/clinician-well-being-resources-during-covid-19 on 26 May 2020.
- 49. Centers for Disease Control and Prevention. Coronavirus (COVID-19). Accessed at www.cdc.gov/coronavirus/2019-ncov/index.html on 26 May 2020.
- 50. Center for the Study of Traumatic Stress. COVID-19 pandemic response resources. Accessed at www.cstsonline.org/resources/resource-master-list/coronavirus-and-emerging-infectious-disease-outbreaks-response on 26 May 2020.
- 51. Intensive Care Society. Wellbeing and psychological resource library. Accessed at www.ics.ac.uk/ICS/Education/Wellbeing/ICS/Wellbeing.aspx? on 26 May 2020.
- 52. Lee SM, Kang WS, Cho AR, et al. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018;87:123-127. [PMID: 30343247] doi:10.1016/j.comppsych.2018.10.003 [DOI] [PMC free article] [PubMed]
- 53. Barello S, Palamenghi L, Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020;290:113129. [PMID: 32485487] doi:10.1016/j.psychres.2020.113129 [DOI] [PMC free article] [PubMed]
- 54. Lu W, Wang H, Lin Y, et al. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:112936. [PMID: 32276196] doi:10.1016/j.psychres.2020.112936 [DOI] [PMC free article] [PubMed]
- 55. Liang Y, Chen M, Zheng X, et al. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19 [Letter]. J Psychosom Res. 2020;133:110102. [PMID: 32224344] doi:10.1016/j.jpsychores.2020.110102 [DOI] [PMC free article] [PubMed]
- 56. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971 Nov-Dec;12:371-9. [PMID: 5172928] [DOI] [PubMed]
- 57. Zung WW. From art to science. The diagnosis and treatment of depression. Arch Gen Psychiatry. 1973;29:328-37. [PMID: 4724142] [DOI] [PubMed]
- 58. Chen Y, Zhou H, Zhou Y, et al. Prevalence of self-reported depression and anxiety among pediatric medical staff members during the COVID-19 outbreak in Guiyang, China [Letter]. Psychiatry Res. 2020;288:113005. [PMID: 32315886] doi:10.1016/j.psychres.2020.113005 [DOI] [PMC free article] [PubMed]
- 59. Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11-17. [PMID: 32240764] doi:10.1016/j.bbi.2020.03.028 [DOI] [PMC free article] [PubMed]