Abstract
Background
Resident participation in quality improvement and patient safety (QIPS) programs is an essential training experience and Accreditation Council for Graduate Medical Education requirement. However, the most effective approach to achieve this is unclear.
Objective
We developed an experiential Quality Improvement and Patient Safety Curriculum and Resident Experience (QIPS CURE) program, which provides internal medicine (IM) residents with foundational QIPS knowledge, and evaluated its effectiveness.
Methods
After reviewing IM residency QIPS curricula and obtaining input from institutional stakeholders in 2013–2014, we launched a longitudinal QIPS curriculum for all 66 postgraduate year 1–3 IM residents in July 2014. The QIPS CURE included 2 major elements: didactics, delivered through a variety of sources, including online modules and workshops, and hands-on projects. We delivered this curriculum annually from 2014 to 2018. We used project completion and an attitude survey of participants to evaluate it.
Results
Six projects were completed in 2014–2015, and 10 projects completed yearly for the next 3 academic years. Residents presented all projects at regional meetings. Surveyed residents reported improvement in understanding (M = 5.71, SD = 1.07 pre- to M = 6.38, SD = 0.49 post-curriculum, P = .013) and competence (M = 3.31, SD = 1.18 pre- to M = 6.08, SD = 0.77, post-curriculum, P < .001) when comparing graduates of the curriculum with incoming interns. Qualitative analysis revealed perceived acquisition of skills needed to carry out successful QIPS projects.
Conclusions
This QIPS program was sustainable over 4 years and generally well-received by residents, with many projects completed each year.
What was known and gap
Resident participation in quality improvement and patient safety (QIPS) programs is an essential training experience and an Accreditation Council for Graduate Medical Education requirement. However, the optimal way to meet these expectations is not clear.
What is new
A longitudinal, experiential Quality Improvement and Patient Safety Curriculum and Resident Experience (QIPS CURE) program that provides internal medicine residents with foundational QIPS knowledge.
Limitations
Single specialty and single institution limits generalizability; evaluation survey was not tested for validity.
Bottom line
A longitudinal QIPS curriculum in a GME program was sustained over multiple years and was well-received by residents.
Introduction
Development of quality improvement and patient safety (QIPS) skills has become a key competency in medical education since the Institute of Medicine underscored the prevalence of medical errors and the need to improve the quality of care in the US health care system.1–4 To achieve this goal, the Accreditation Council for Graduate Medical Education (ACGME) outlines expectations of programs and trainees.5 Trainees are expected to actively participate in patient safety systems and advocate for system improvement, recognize and report system errors, analyze and improve the quality of their practice, and participate in interprofessional QI activities.5–7
However, the optimal way to meet these expectations is not clear. Recently, QI leaders have identified that most resident QIPS projects are not aligned with clinical sites' priorities and fail to utilize an interprofessional team.8 Barriers include lack of dedicated time, lack of faculty expertise, and challenges to promoting interprofessional activities.9–11
In response to these barriers, we developed the Quality Improvement and Patient Safety Curriculum and Resident Experience (QIPS CURE) program, a longitudinal QIPS curriculum combining foundational QIPS knowledge with project-based experiences. We evaluated this program via resident surveys and completion of projects.
Methods
Setting and Participants
The University of Missouri-Kansas City (UMKC) internal medicine (IM) residency program is a university-based program affiliated with an urban safety net hospital and a tertiary referral center. The program has a total of 57 categorical and 9 preliminary residents.
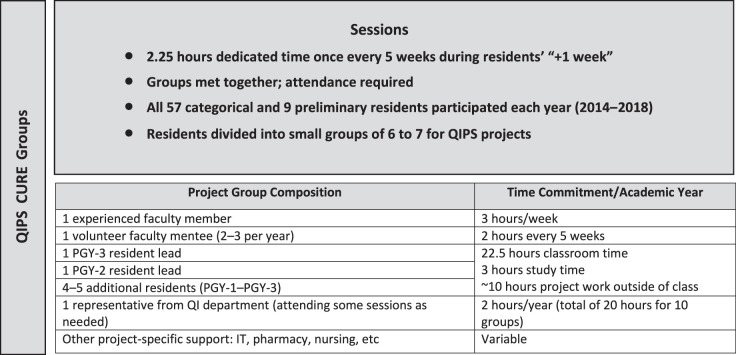
We introduced this curriculum to coincide with the launch of an ambulatory block scheduling system, in which residents are divided into 5 cohorts. Each cohort rotates through a staggered 4-week cycle followed by a 1-week outpatient block (4+1). We protected a 2.25-hour block of time during each cohort's outpatient (+1) week for the QIPS CURE. An overview of the composition of these groups, along with faculty and resident time commitments, can be found in the Figure.
Figure.
Quality Improvement and Patient Safety Curriculum and Resident Experience (QIPS CURE) Group Composition
Intervention
In 2013–2014, prior to launching the QIPS CURE at UMKC, the IM residency program director and the program's QI curriculum director, hereafter referred to as “lead faculty,” solicited support from multiple stakeholders—the designated institutional official; leadership from the hospitals' quality, safety, and information technology (IT) departments; residency leadership; residents; potential faculty mentors; and the chair of the department. We also sought insight and direction by reviewing the status of QIPS curricula in other ACGME IM residency programs in the United States. Results of the review are provided as online supplemental material. We launched our required longitudinal QIPS curriculum for all 66 postgraduate year (PGY) 1–3 IM residents in July 2014, and delivered it annually. We are reporting the results of the first 4 years (2014–2018), though the program is still ongoing.
QIPS CURE Curriculum
Didactic Component:
To give residents the practical skillset and basic QIPS knowledge needed to engage in projects, we used a variety of didactic methods. We employed a flipped classroom model, with residents completing Institute for Healthcare Improvement (IHI) Open School modules11 prior to meeting as a group. In-person time also included discussion of the modules and project development. Residents completed all modules necessary to earn the IHI's Basic Certificate in Quality and Safety. We invited members of the hospital's patient safety team to facilitate in-person sessions, including a simulated root cause analysis and a revamped monthly morbidity and mortality conference. The team members also demonstrated how to log a patient safety event. Each resident showed competency by logging an event themselves. Additional resources were employed to help with specific QIPS topics. An outline of the curriculum structure and specific sessions can be found in Table 1. Finally, residents reviewed and reflected on their own personal outpatient and inpatient quality metrics. An overview of our curricular goals and specifics of how they were achieved within the curriculum is provided as online supplemental material. We also reviewed the advantages and challenges of our approach.
Table 1.
Didactic Content of Quality Improvement and Patient Safety Curriculum and Resident Experience (QIPS CURE)
| Session | Outline of Session | IHI Modules | Guests/Stakeholders |
| July session | Didactics session
|
None | Invite IT representative (speak to feasibility) |
| Session 1 | Didactics session: Intro to QI
|
PGY-1 QI 101 & 102 PGY-2 L 101 | Invite IT representative (speak to feasibility) |
| Session 2 | Didactics session: QI tools
|
PGY-1 PS 104 PGY-2 QI 105 | Invite members of hospital QI team to help coach Note: (very busy session, allow extra time if possible) |
| Session 3 | Didactics session: defining metrics
|
PGY-1 QI 103 PGY-2 PS 103 | Optional: Invite members of hospital QI Team to help coach Note: Helpful to review IHI QI essentials toolkit |
| Session 4 | Didactics session: PDSA cycles
|
PGY-1 PS 101 PGY-2 TA 101 | None |
| Session 5 | Didactics session: reviewing data
|
PGY-1 PS 102 PGY-2 PS 105 | Optional: Invite members of hospital QI team to help coach |
| Session 6 | Didactics session: patient safetya
|
PGY-1 QI 104 PGY-2 No module assigned | Invite members of hospital patient safety team |
| Session 7 | Didactics: patient safety
|
PGY-1 PFC 101 PGY-2 No module assigned | Invite members of hospital patient safety team |
| Session 8 | Didactics: aim statements
|
No modules assigned | |
| Session 9 | Didactics: feedback
|
No modules assigned |
Abbreviations: IHI, Institute for Healthcare Improvement; QI, quality improvement; IT, information technology; CITI, Collaborative Institutional Training Initiative; PGY, postgraduate year; IRB, Institutional Review Board; PDSA, plan-do-study-act.
In March/April faculty meet with QI leaders/stakeholders to identify priorities and potential projects for upcoming year; review individual quality metrics with residents.
Leadership Roles:
To maintain momentum between sessions, residents took detailed minutes during each meeting and posted them to a shared project folder. PGY-2 and PGY-3 leads were appointed for each group and assigned tasks to members with clear deadlines. Additionally, we required resident leads to send email updates during the weeks between sessions. Categorical residents completed 3 separate projects over the course of their residency with increasing levels of responsibility each year.
Project Selection:
To promote buy-in, residents designed their own projects. Each group discussed all proposals and agreed on one project based on feasibility, alignment with institutional priorities, and the availability of specific, measurable, attainable, realistic, and timely outcome data. Each resident group then formalized a proposal using the Model for Improvement as a framework,12 with assistance from members of the hospital's quality resources department. A performance improvement project proposal worksheet (provided as online supplemental material) was completed and published on the hospital website. This process assisted coordination with hospital-wide initiatives, avoided duplication of effort, and facilitated collaboration with other involved departments. Each project was submitted to the Institutional Review Board (IRB) for review to ensure it did not meet the definition of human subjects research. All projects were completed within a 9-month time frame, culminating in submission for presentation at the UMKC School of Medicine's annual Quality and Patient Safety Day.
Faculty Support:
In addition to support from the department of quality resources, 2 faculty members worked with each cohort—one had prior QIPS experience. While some faculty attend only on designated weeks to mentor a specific project, at least 1 faculty member must attend consistently to provide curricular oversight and avoid duplication in projects. Like many programs, we have limited faculty with QIPS experience.12 Therefore, we utilized a co-learning environment as described by Wong et al13 and designed QIPS CURE to allow faculty to learn alongside residents with varying levels of commitment (mentor versus co-mentor, multiple projects versus one project).14 Two to 3 faculty mentees voluntarily participated each year, expanding our pool of faculty with a QIPS skillset by more than 10 since 2014. Through participation in QIPS, faculty also earned credit toward maintenance of specialty certification.
Outcomes
We evaluated QIPS CURE at different intervals from 2014 through 2018 with a semistructured anonymous survey of residents, similar to the one used by the University of Pennsylvania (provided as supplemental online material). The survey was administered to incoming interns before exposure to QIPS CURE (July 2017) and to graduating PGY-3 residents after participation in QIPS CURE (June 2017 and June 2018).
The survey included 3 demographic questions, 11 questions on a 7-point Likert scale (strongly disagree to strongly agree), and 5 open-ended questions, including reporting the number of patient safety events logged over the past year. The number of completed projects was tracked each year.
This study was deemed exempt from review by the UMKC IRB.
Analysis
We performed a t test to compare residents' survey responses before and after participating in QIPS CURE. We also evaluated responses on our annual ACGME Resident/Fellow Survey.
We performed conventional content data analysis using a data coding system that corresponds to the data collection, because the goal of our study was descriptive, and there is little existing theory to guide our analysis.15 We used a deductive coding process for the open-ended questions on the survey. Responses to open-ended questions were compiled and then read in their entirety. One author (K.G.) completed all data coding independently, then 2 other authors (R.M. and D.W.) reviewed the coding and confirmed the findings. Disagreement was resolved by discussion among the 3 investigators. After reading through the responses, codes were derived that captured key concepts from reading the data word for word.16 We started our analysis with codes already in mind, based on work published by Weigel et al17; however, we modified the codes iteratively as we completed the qualitative content analysis.10
To ensure rigor and trustworthiness, we enhanced credibility through several strategies. Peer debriefing was used in the form of ongoing discussions with members of the QIPS faculty, which allowed for testing of new ideas and insights throughout the curriculum evaluation process. We provided a written synthesis of the overall results with resident representatives and asked them to comment on the accuracy of the findings. Finally, we included representative quotes from participants.18
Results
Group Projects and QIPS Participation
Project completion and ACGME survey results are summarized in Table 2, and details of the QIPS projects from 2014 to 2018 are provided as online supplemental material. Prior to curriculum implementation in 2014, no residents submitted QIPS posters to regional or national scientific meetings. Since then, each project was presented at a minimum of one regional meeting: between 2014 and 2018, 8 were recognized with awards as one of the top 2 abstract submissions (invited for oral presentation) or top poster presentation.
Table 2.
QIPS Project Completion/ACGME Survey Results
| Year | No. of Projects Completed | No. (%) of Residents Reporting QI Participation on Annual ACGME Survey |
| 2013–2014a | 0 | 34 (57)b |
| 2014–2015 | 6 | 57 (93)c |
| 2015–2016 | 10 | 60 (100) |
| 2016–2017 | 10 | 60 (100) |
| 2017–2018 | 10 | 62 (100) |
Abbreviations: QIPS, Quality Improvement and Patient Safety; ACGME, Accreditation Council for Graduate Medical Education.
Pre-QIPS CURE implementation.
N = 60.
N = 61.
Curriculum Evaluation
We surveyed incoming residents before their exposure to the QIPS curriculum in 2017 (response rate: 14 of 26 [54%]), as well as graduating residents after QIPS participation in 2017 and 2018 (response rates: 20 of 20 [100%] and 12 of 19 [63%], respectively). Table 3 summarizes the results, showing residents perceived they improved in a wide variety of QIPS skills, and by graduation, most believed they would be able to independently lead a QIPS project. When graduating residents were asked how many patient safety events they logged in the past year, 58% (11 of 19) reported at least one, and 42% (8 of 19) responded “zero” or did not respond to the question. Before launching QIPS CURE, only one resident reported ever completing a PS report.
Table 3.
Residents' Survey Responses Before and After Participating in QIPS CURE
| Survey Question | Strongly Agree/ Agree, n (%) | Somewhat Agree/ Undecided/ Somewhat Disagree, n (%) | Disagree/Strongly Disagree, n (%) | Mean (SD) | P Value | ||||
| After QIPS CURE | Before QIPS CURE | After QIPS CURE | Before QIPS CURE | After QIPS CURE | Before QIPS CURE | After QIPS CURE | Before QIPS CURE | ||
| I understand the basic approach to quality improvement/patient safety as it applies to problems in health care. | 32 (100) | 8 (57) | 0 (0) | 6 (43) | 0 (0) | 0 (0) | 6.38 (0.49) | 5.71 (1.07) | .013 |
| I am able to identify key stakeholders in a process that requires improvement. | 30 (94) | 3 (21) | 2 (6) | 11 (79) | 0 (0) | 0 (0) | 6.32 (0.54) | 4.79 (1.12) | < .001 |
| I am able to create a fishbone diagram to understand the root causes of a quality or safety problems. | 28 (88) | 1 (7) | 4 (12) | 11 (79) | 0 (0) | 2 (14) | 6.15 (0.67) | 3.64 (1.22) | < .001 |
| I am able to create a SMART aim (goal) statement. | 28 (88) | 3 (21) | 3 (9) | 7 (50) | 0 (0) | 4 (29) | 6.03 (0.75) | 3.79 (1.63) | < .001 |
| I am able to design a plan-do-study-act cycle. | 30 (94) | 2 (14) | 2 (6) | 10 (71) | 0 (0) | 2 (14) | 6.25 (0.57) | 4.07 (1.44) | < .001 |
| I am able to identify if a change led to improvement. | 29 (91) | 5 (36) | 2 (6) | 9 (64) | 0 (0) | 0 (0) | 6.34 (0.48) | 5.21 (1.05) | < .001 |
| I am able to identify meaningful quality metrics for QI work. | 24 (75) | 1 (7) | 8 (25) | 13 (93) | 0 (0) | 0 (0) | 6.11 (0.63) | 4.36 (0.74) | < .001 |
| I feel comfortable leading a QI project. | 29 (91) | 1 (7) | 3 (9) | 8 (57) | 0 (0) | 5 (36) | 6.08 (0.77) | 3.31 (1.18) | < .001 |
| I am able to identify quality gaps within my own practice. | 28 (88) | 5 (36) | 4 (12) | 9 (64) | 0 (0) | 0 (0) | 6.33 (0.61) | 5.07 (0.83) | < .001 |
| I am able to log a patient safety event in the hospital's incident reporting system. | 30 (94) | 3 (21) | 2 (6) | 8 (57) | 0 (0) | 3 (21) | 6.47 (0.72) | 4.07 (1.44) | < .001 |
| I believe that the QIPS curriculum was a valuable learning experience. | 26 (81) | a | 6 (19) | a | 0 (0) | a | 6.16 (1.05) | a | a |
Abbreviation: QIPS CURE, Quality Improvement and Patient Safety Curriculum and Resident Experience.
Note: Each question's responses on a 7-point Likert scale (strongly agree, agree, somewhat agree, undecided, somewhat disagree, disagree, strongly disagree).
Question only asked after participation in QIPS CURE.
Table 4 summarizes themes that emerged from the qualitative analysis of residents' survey comments (full comments provided as online supplemental material). Review of the data demonstrated understanding of skills critical to project development, including systems-based thinking, QI principles, teamwork, and challenges of QI work.
Table 4.
Selected Results of the Qualitative Analysis of Resident Comments
| Themes | Examples of Resident Comments |
| What Part of the Curriculum Experience Was the Most Useful? | |
| Teamwork | “Ability to see QI on a grand scale and interact with people outside of the immediate residency program.” |
| Systems-based learning and systems thinking | “Improved patient care involves changes in the system and not mere individuals.” “How to identify issues within our system and create a project to address these issues.” “Learned to identify system inadequacies and create a safe plan to address them through implementing safe alternatives.” “The other stakeholders [and] other clinical staff are as important in-patient care.” |
| QI principles and knowledge | “Basics behind the QI project, why we do it, how it is different from research.” “A practical education of quality improvement was valuable to me. The QI curriculum taught residents not only the theoretic aspects of QI, but a hands-on education on how one may go about a QI project.” |
| Mentorship | “Presence of faculty mentors at every meeting to add critical thinking and valuable input at important decision-making points.” |
| Firsthand experience | “Organizing and completing a project, including IRB approval, etc.” “Running the project and doing hands-on work.” |
| What Would You Change About the Curriculum? What Challenges Did You Identify While Working on Your QI Project? | |
| Team management | “I feel we have too many projects going on at same time. It gets confusing for the other non-participating staff members to comply to all the changes within the short period of time.” |
| Curriculum implementation | “Didactic vs time on projects needs to be worked on without increasing the time outside of the QI sessions.” “Getting early feedback regarding the feasibility of projects.” “Working on QI in between sessions due to busy rotations.” |
| Stakeholder engagement | “More clearly identify and involve the administrative staff/stakeholders that we generally have no communication with/knowledge of. I think their involvement really helped to strengthen some of the projects.” |
Abbreviations: QI, quality improvement; IRB, Institutional Review Board.
The main resources required for curricular implementation were faculty expertise and faculty and resident time, summarized in the Figure. The QIPS CURE lead faculty was a core faculty member in the residency program, with QI education as the chief non-clinical responsibility. One residency program coordinator was responsible for room scheduling and spent approximately 15 minutes per week tracking resident completion of IHI modules. Materials costs were minimal, and access to the IHI modules was free.
Discussion
This longitudinal didactic and experiential QIPS curriculum for IM residents—QIPS CURE—was sustained over 4 years and appeared highly acceptable to residents who perceived increases in QIPS knowledge and skills. Many projects were completed each year of the program.
This work contributes to the emerging body of evidence across graduate medical education (GME) specialties supporting the effectiveness of curricula pairing didactic and experiential learning with an interdepartmental approach.8,19,20 Several other programs reported increases in QIPS participation and scholarly activity by embedding protected time into an ambulatory block curriculum.9,10 Lack of appropriate mentors is a commonly reported barrier, and our curriculum appears to facilitate capacity building among faculty with limited QIPS expertise. An alternative to reduce the need for faculty hours may be utilization of chief residents for mentorship.9 An approach different from our curriculum that has been reported is a QIPS curriculum that pools resources across departments and is inclusive of multiple GME specialties. This demonstrated an increase in knowledge scores and adverse event reporting by residents, but the overall curriculum appears more limited in scope than QIPS CURE and lacks a project component.20 While some studies report results of their curricular experience after just 1 year, this study is notable for demonstrating 4 years of sustainability.10,19
Throughout curricular implementation, we addressed several challenges. Multi-stakeholder involvement was a key element to the success of the residents' experience. However, many resident groups underestimated the time needed by the IT department to make changes. To minimize this barrier, we incorporated IT staff in the planning stages of our sessions to help ensure timeline feasibility.
Programs not utilizing an ambulatory block schedule may have challenges in finding alternative ways to dedicate protected time for group meetings. However, the importance of these topics and the limited opportunities for QIPS learning in other arenas might justify displacement of traditional learning time, such as passive lectures. Finding available faculty may be a commonly identified barrier to implementing QIPS curricula.14,21 Including faculty as co-mentors is an innovative way to overcome barriers for faculty participation and build capacity in this area among faculty, many of whom have not had any formal training or education in QIPS.
This was a single program and a single site study, which could limit generalizability. Implementation required significant commitment of residency and hospital leadership, resources for coordination, and faculty expertise and development. Prioritization as a centerpiece of the overall residency curriculum may be necessary for success. Without institutional support, the time and resources committed to this curriculum may not be feasible for all programs. Aligning with institutional priorities can leverage requests for support. The survey was not tested for validity evidence prior to use, and we recognize the potential for a social desirability bias that may have influenced residents' survey responses.
Next steps include external analysis of residents' acquisition of QIPS skills, as well as formal evaluation of the faculty experience. We will also evaluate long-term outcomes of our curriculum on practice patterns of graduates, namely quantifying their participation in QIPS projects.
Conclusions
Implementation of a longitudinal QIPS curriculum into a GME program was sustained over 4 years. It was well-received by residents, who perceived improvement in QIPS knowledge and skills. The curriculum resulted in completion of multiple QIPS projects each year.
Supplementary Material
Footnotes
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
The authors would like to thank Dr. Julie Banderas for her input and support of the QIPS CURE curriculum, Kristy Steigerwalt for her assistance with designing and running the literature searches that informed this work and publication, and Dr. Jennifer Myers for guidance on the survey and for providing a copy of the survey used as part of the curriculum at the University of Pennsylvania.
References
- 1.Kohn LT, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Washington, DC: National Academies Press;; 2000. [PubMed] [Google Scholar]
- 2.Institute of Medicine Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press;; 2001. [Google Scholar]
- 3.Mangione-Smith R, DeCristofaro AH, Setodji CM, Keesey J, Klein DJ, Adams JL, et al. The quality of ambulatory care delivered to children in the United States. N Engl J Med. 2007;357(15):1515–1523. doi: 10.1056/NEJMsa064637. [DOI] [PubMed] [Google Scholar]
- 4.Berwick DM. Continuous improvement as an ideal in health care. N Engl J Med. 1989;320(1):53–56. doi: 10.1056/NEJM198901053200110. [DOI] [PubMed] [Google Scholar]
- 5.Accreditation Council for Graduate Medical Education. Common Program Requirements. 2020 http://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirements Accessed June 22.
- 6.Accreditation Council for Graduate Medical Education. Milestones. 2020 http://www.acgme.org/What-We-Do/Accreditation/Milestones/Overview Accessed June 22.
- 7.Accreditation Council for Graduate Medical Education. Clinical Learning Environment Review (CLER) 2020 http://www.acgme.org/What-We-Do/Initiatives/Clinical-Learning-Environment-Review-CLER Accessed June 22.
- 8.Bodenheimer T, Dickinson WP, Kong M. Quality improvement models in residency programs. J Grad Med Educ. 2019;11(1):15–17. doi: 10.4300/JGME-D-18-00556.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tentler A, Feurdean M, Keller S, Kothari N. Integrating a resident-driven longitudinal quality improvement curriculum within an ambulatory block schedule. J Grad Med Educ. 2016;8(3):405–409. doi: 10.4300/JGME-D-15-00371.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnson KM, Fiordellisi W, Kuperman E, Wickersham A, Kuehn C, Kamath A, et al. X + Y = time for qi: meaningful engagement of residents in quality improvement during the ambulatory block. J Grad Med Educ. 2018;10(3):316–324. doi: 10.4300/JGME-D-17-00761.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baxter K, Petz C, Middleton JL, Chan M. Re-thinking how we teach quality improvement: adding meaning to an ACGME requirement. J Gen Intern Med. 2019;34(8):1662–1667. doi: 10.1007/s11606-019-05059-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Byrne JM, Hall S, Baz S, Kessler T, Roman M, Patuszynski M, et al. Quality and safety training in primary care: making an impact. J Grad Med Educ. 2012;4(4):510–515. doi: 10.4300/JGME-D-11-00322.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong BM, Levinson W, Shojania KG. Quality improvement in medical education: current state and future directions. Med Educ. 2012;46(1):107–119. doi: 10.1111/j.1365-2923.2011.04154.x. [DOI] [PubMed] [Google Scholar]
- 14.Wong BM, Goguen J, Shojania KG. Building capacity for quality: a pilot co-learning curriculum in quality improvement for faculty and resident learners. J Grad Med Educ. 2013;5(4):689–693. doi: 10.4300/JGME-D-13-00051.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 16.Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. New York, NY: Sage Publications;; 1994. [Google Scholar]
- 17.Weigel C, Suen W, Gupte G. Using lean methodology to teach quality improvement to internal medicine residents at a safety net hospital. Am J Med Qual. 2013;28(5):392–399. doi: 10.1177/1062860612474062. [DOI] [PubMed] [Google Scholar]
- 18.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–112. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Reardon CL, Ogrinc G, Walaszek A. A didactic and experiential quality improvement curriculum for psychiatry residents. J Grad Med Educ. 2011;3(4):562–565. doi: 10.4300/JGME-D-11-0008.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miller ME, Patel A, Schindler N, Hirsch K, Ming M, Weber S, et al. Bridging the gap: interdepartmental quality improvement and patient safety curriculum created by hospital leaders, faculty, and trainees. J Grad Med Educ. 2018;10(5):566–572. doi: 10.4300/JGME-D-18-00060.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myers JS, Jaeger J. Faculty development in quality improvement: crossing the educational chasm. Am J Med Qual. 2012;27(2):96–97. doi: 10.1177/1062860611433640. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.