Abstract
Background
Because residents are often on the frontlines of patient care and are likely to witness adverse events firsthand, it is critical they report patient safety events. They may, however, be underreporting.
Objective
We examined the current literature to identify strategies to increase patient safety event reporting by residents.
Methods
We used CINAHL (EBSCO Information Services, Ipswich, MA), EMBASE (Elsevier, Amsterdam, the Netherlands), PsycINFO (APA Publishing, Washington, DC), and PubMed (National Center for Biotechnology Information, Bethesda, MD) databases. The search was limited to English-language articles published in peer-reviewed journals through March 2020. Key terms included “residents, trainees, fellows, interns, graduate medical education, house staff, event reporting, patient safety reporting, incident reporting, adverse event, and medical error.” To organize findings, we adapted a published framework of strategies for encouraging self-protective behavior.
Results
We identified 68 articles that described strategies used to increase event reporting. The most sustainable interventions used a combination of 3 of the 5 strategies: behavior modeling, surveys and messaging, and required limited financial support. The survey creates awareness; the behavior modeling is critical for educational purposes, and the reminders help to reinforce the new behavior and embed it into routine patient care activities. We noted a dearth of studies involving trainees in root cause analysis following submission of event reports.
Conclusions
The most successful sustainable interventions were those that combined strategies that minimized time for busy physicians, incorporated accessible event reporting in already existing medical records, and became part of a normal workflow in patient care.
Introduction
The culture of safety over the past 2 decades has shifted from one of individual patient care responsibility to one of shared responsibility and teamwork.1 The concept of “just culture” has replaced individual blame and punishment for errors. The focus of safety is no longer remediation of the individual, but identification of system changes and standardization that will reduce the likelihood of an error.2 It is paramount that residents engage in event reporting to identify system gaps, standardize processes, and improve patient care.
Despite the clear importance of safety event reporting by graduate medical education trainees, there is ample literature describing barriers that currently exist and that must be addressed to improve event reporting.3 First, many residents do not know what should be reported and how to report it. Often, trainees rotate through multiple hospitals, each with a different event reporting system, and need to be educated on how to enter an event at each location. Many event reporting systems are cumbersome and time consuming, which may cause busy trainees to resist entering an event. Lack of feedback or change after reporting an event has also been cited as a reason why trainees do not report safety events.3 As residents are early in their careers, they may be less confident in their knowledge and uncomfortable admitting signs of vulnerability.4,5 For these reasons, residents may refrain from calling attention to an error and prefer to hide or ignore it. Lastly, as residents are often new to an institution and dependent on faculty supervisors to support them in finding a future job or fellowship, they may have concerns about repercussions such as ruined reputations, inability to find a job, or punishment for an error.6
Residents are often on the frontlines of patient care and are likely to witness adverse events firsthand, making it imperative that they report events. Therefore, the goal of this narrative review was to examine current literature to identify strategies to increase patient safety event reporting by resident physicians.
Methods
We searched the CINAHL (EBSCO Information Services, Ipswich, MA), EMBASE (Elsevier, Amsterdam, the Netherlands), PsycINFO (APA Publishing, Washington, DC), and PubMed (National Center for Biotechnology Information, Bethesda, MD) databases to inform our narrative review. The search was limited to English-language articles published in peer-reviewed journals. No limitations were placed on publication time range. Through consultation with a librarian, we focused on graduate medical education trainees only as our population of interest. As a result, we conducted title and abstract searches using the following key terms for participants: residents, trainees, fellows, interns, graduate medical education, house staff, and the following key terms to identify interventions of interest: event reporting, patient safety reporting, incident reporting, adverse event, medical error. Eligibility criteria were articles in which participants included residents/fellows and interventions/outcomes related to increasing patient safety event reporting. Articles were excluded when the term “residents” referred to occupants of nursing care homes. Database searches were conducted by one author (U.L.); title, abstract, and full-text screenings by 2 authors (M.A. and U.L.); and analysis and write up by all authors.
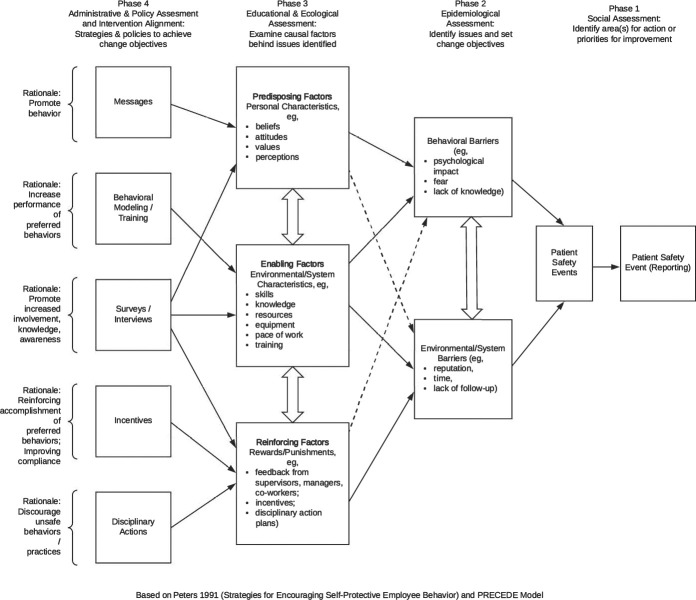
We adapted the Peters7 5 Strategies for Encouraging Self-Protective Behavior framework as a way to organize and interpret which articles addressed which barriers to patient safety event reporting. The Peters7 model was developed to obtain diagnostic information about self-protective behaviors that can be translated into effective accident prevention strategies in workplace environments. The organization of elements in the model is based on the PRECEDE (predisposing, reinforcing, and enabling causes in educational diagnosis and evaluation) model developed as a framework for planning health education programs.8 The 5 strategies in the Peters7 model were chosen because they have undergone a significant amount of empirical research and appear to be widely used in studies of workplace self-protective behaviors. Given the importance of safety event reporting in promoting a culture of safety in health care environments, we felt this model provided an excellent way to categorize patient safety event-reporting education interventions.
Our framework provides a way to organize strategies to address barriers and improve patient safety event reporting (Figure 1). The framework begins by identifying the event for action or improvement (phase 1); then, we identify the behavioral and environmental barriers related to patient safety event reporting (phase 2), which is followed by the predisposing, enabling, and reinforcing of factors that could improve event reporting (phase 3), and finally, strategies are sought that could be used to overcome identified barriers (phase 4). Given that the goal of our qualitative synthesis process was to identify the most commonly used strategies to increase event reporting among residents and fellows and the characteristics of interventions that reported sustainability over time, we used the framework to develop our data extraction form. To help organize our findings, we reported results according to the 5 strategies of our guiding framework: behavioral modeling and training, disciplinary actions, incentives, messages, surveys, and interviews.
Figure 1.
Adaptation of the Peters7 5 Strategies for Encouraging Self-Protective Behavior Framework
The Emory University Institutional Review Board determined that this study was exempt from review.
Results
We identified 68 articles that described strategies used to increase event reporting among residents and fellows (Figure 2). The Table provided as online supplemental material lists the 68 articles and indicates which strategies were used to increase patient safety event reporting in each article and the factors addressed by the selected strategies. Several articles described interventions that used multiple strategies. Across the 68 articles, the most common strategy used to increase event reporting was surveys and interviews (n = 45, 66%),9–46 followed by behavioral modeling and training (n = 42, 62%),* messages (n = 11, 16%),† incentives (n = 4, 6%),18,57,67,71 and disciplinary actions (n = 1, 1%).73 Most articles did not report sustainability of interventions; however, for those articles that reported sustainability of interventions (n = 14, 21%),‡ sustainability ranged from 5 months to 2 years. Articles reporting sustainability of interventions involved the use of 3 primary strategies: behavioral modeling and training (13 of 14, 93%),§ reminder messaging (5 of 14, 36%),6,18,57,62,71 and incentives (4 of 14, 29%).18,57,67,71 In the following sections, examples are used to highlight different aspects of each of the 5 strategies.
Figure 2.
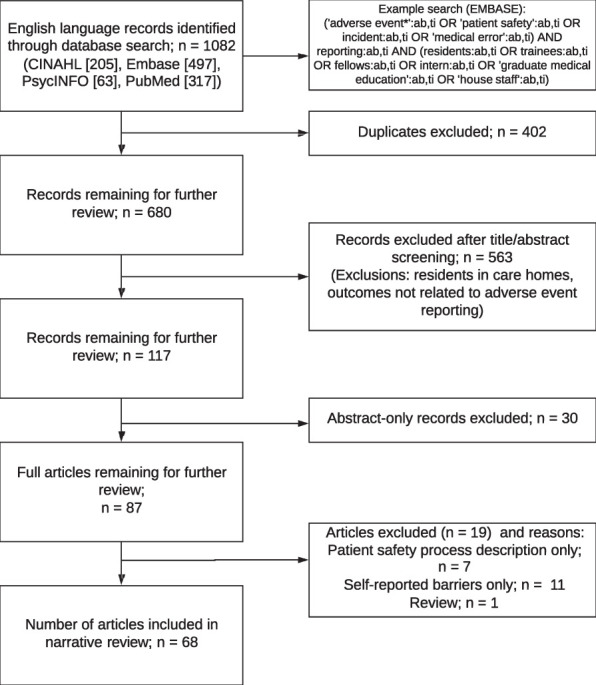
Narrative Review Flow Diagram
Surveys and Interviews
Surveys and interviews were used to promote increased involvement, knowledge, and awareness of patient safety event reporting. Across the 45 articles (of 68 total, 66%) using surveys and interviews, 38 (84%) used surveys‖ and 7 (16%) used interviews.13,17,25,32,44–46 In 42 articles (62%),# surveys and interviews were used to address enabling factors (eg, skills, knowledge, or resources). For example, Martowirono and colleagues13 used interviews to explore barriers that residents experience (eg, negative attitudes, unsupportive culture, lack of perceived ability) and obtain proposed solutions from residents (eg, provide feedback, simplify reporting process, promote incident reporting culture). In 34 articles (50%),** surveys and interviews were used to identify predisposing factors (eg, beliefs, attitudes, values, or perceptions); for example, Louis and colleagues12 surveyed residents and faculty using the Healthcare Provider's Perceptions of Safety Events Questionnaire, a tool based on 9 core domains, which contains 60 items focused on variables that either facilitate or impede patient safety event reporting.
In 21 articles (31%),†† surveys and interviews were used to identify reinforcing factors (eg, feedback from supervisors or coworkers, incentives, or disciplinary action). For example, Heard et al75 mailed a survey to anesthesiology residents to determine attitudinal and emotional factors influencing reporting of an unspecified adverse event caused by error.
Behavioral Modeling and Training
Behavioral modeling or training was used to increase performance of preferred behaviors. The primary modes of providing modeling and training were through educational programming (33 articles, 49%)‡‡ and new or updated technology (9 articles, 13%).§§ This strategy was primarily used to address deficits related to patient safety event reporting knowledge and resources (ie, enabling factors).
Most educational programs were led by a team of faculty and residents; however, 2 articles (3%) described resident-led curricula.59,63 Tevis and colleagues,64 for example, developed an annual patient safety orientation of first-year students. The 4-hour event was developed by a multidisciplinary team, including faculty, residents, and experts in quality improvement and patient safety. including the vice president of quality and safety and the medical director of patient safety. This event consisted of large group discussions about event reporting and small group sessions where residents worked with a facilitator to complete a root cause analysis (RCA). Discussions covered topics such as just culture, definitions of adverse events and near misses, the importance of reporting, instructions about how to submit event reports, and a summary of how reports are processed and how institutional processes are changed based on reports.64 Smith et al63 described how pediatric residents developed a curriculum and led a monthly conference during which they reviewed adverse event reports, identified system vulnerabilities, and designed solutions to address those vulnerabilities. As part of educational programming, morbidity and mortality conferences were used to increase trainee awareness about adverse events and the importance of reporting31,34,53,57,63,74,76–79; however, although there were calls for increased trainee participation in RCA),19 only Murphy and colleagues60 described an intervention using a mock RCA to increase trainee adverse event reporting, and only the study by Dunbar and colleagues52 reported increased resident physician involvement in RCA as a result of their intervention.
New or updated technology, including mobile technology and computer software, was primarily introduced to reduce the burden of submitting an adverse event report. Bent and colleagues47 described how personal digital assistants were introduced to help anesthesiology residents complete a collection of logbook data, procedural performance data, and critical incident reports. Thoms et al65 described how they introduced a trigger list to suggest suitable types of incidents to report and trained faculty and residents to use the electronic reporting system that contained the list.
Forty-one of 42 articles (98%) related to behavioral training or modeling addressed enabling factors (ie, knowledge and resources).‖‖ For example, Macht et al59 described the development of a resident-led patient safety curriculum conducted quarterly during academic conferences. That curriculum involved a review of topics such as what to report, how to report, and methods for analysis of an adverse event. The curriculum also involved reviewing aggregated resident-filed events and conducting a detailed mini RCA.59 With regard to reinforcing factors, 22 of those 42 articles (52%)## addressed how programs used feedback or incentives to promote patient safety event reporting. Steen and colleagues19 developed an educational session on event reporting and followed up by providing feedback every 2 months on events reported and actions taken. Finally, 18 of the 42 articles (43%)*** discussed the use of behavioral modeling or training to address attitudes and beliefs; for example, Boike and colleagues21 used 1-hour training conferences to educate residents on the types of events that qualify for adverse event reporting.
Messages
Messages, in the form of emails, documents (eg, manuals), and meetings were used to promote patient safety event reporting behaviors. This strategy was used to primarily address enabling factors and reinforcing factors. In an example of an enabling factor, Jericho et al44 developed a resident education manual that included references to resources, such as the National Quality Forum Serious Reportable Adverse Events in Healthcare, and included a reporting quick reference guide. That manual was distributed to residents as part of an educational program.44 Desbiens51 described how their setting used an event reporting records audit process coupled with program director meetings with residents as an example of reinforcing adverse event reporting behavior. Finally, in an attempt to address resident concerns around repercussions of reporting patient safety events (ie, predisposing factors), Fleming and colleagues70 proposed a set of 14 recommendations to improve protection for residents in raising patient safety concerns. These recommendations include calls for educating physicians on their professional duty and responsibility to report adverse events and developing open and positive workplace cultures where patient safety events can be discussed and resident input is welcomed.70
Incentives
Incentives, while rare, were used to reinforce accomplishment of preferred patient safety event reporting behaviors and improve compliance. For example, Herzer and colleagues57 described how they developed a “Good Catch” award to recognize an individual or group who identified and reported an adverse event and participated in efforts to analyze the hazard and implement a plan to address it. To improve compliance, Scott et al18 described how they used a retirement savings benefit to improve resident participation in adverse event reporting. In particular, they set a goal of having residents report 5% or more of all adverse events for a period within the academic year and the economic incentive consisted of a retirement savings benefit in the amount of 1.5% of residents' annual salaries.18
Disciplinary Actions
Disciplinary action was the least used strategy. The only article that discussed disciplinary actions related to patient safety event reporting used a survey to ask participants which responses to protocol lapses (eg, public reporting or penalties, fine, suspension, or firing) they would endorse for different adverse event scenarios.73 Driver and colleagues73 noted that, although participants endorsed the use of penalties, implementation of such a system would go against developing positive workplace cultures where adverse events can be discussed without fear of repercussions.
Largest Strategy Combination
One publication included 4 of the 5 strategies that resulted in sustained event reporting for at least a year.18 That team used a multifaceted intervention that incorporated a comprehensive educational campaign, email notifications, one-on-one discussions, a survey asking for the resident's principal motivations for completing an adverse event report (87% cited patient wellness as a motivation for reporting, 64% cited the financial retirement incentive, and 17% cited educational opportunity), and a financial incentive of retirement matching. This combination of strategies resulted in an increase in the average number of adverse events reported by residents from 1.6% to 9% of the institution's overall event reports, representing a 5.6-fold increase during the 1-year initiative.18
Discussion
This narrative review provides a comprehensive examination of the most commonly used strategies to increase patient safety event reporting among residents and fellows and the interventions that reported sustainability over time.
The most common strategy—surveys and interviews—was instrumental in assessing current barriers to reporting and/or the trainees' understanding of patient safety and for increasing awareness of event reporting. Behavior modeling and training was also essential for educational purposes, addressing deficits in knowledge and/or specific hospital systems used for event reporting. Lastly, frequent messaging was needed to reinforce behaviors that are often not part of routine patient care. Busy trainees are focused on providing appropriate patient care, completing administrative tasks, documenting in the electronic medical record, meeting work hour requirements, all while maintaining their own personal health. Patient safety is often a low priority, resulting in trainees who do not wish to take additional time, do not recognize the importance, or do not remember to log patient safety events, particularly at the end of a long shift.
Our review demonstrates that no single strategy solves the many challenges that exist, but a combination of strategies seems to have a cumulative, sustainable effect on resident physician reporting by supporting a culture that fosters reporting. While many successful interventions reviewed in this study incorporated a combination of strategies, some were expensive18 or time consuming to the leadership and trainees. However, the combination of surveys, behavior modeling and training, and messages required fewer resources and resulted in positive behavior modification in patient safety event reporting.
While a combination of all the strategies may best sustain results, resources (particularly time and money) are often limited. For many institutions, particularly large institutions with multiple participating sites, it is not practical to implement and sustain all these strategies. Articles highlighting sustained improvements6,11,18 used a combination of behavior modeling, coupled with surveys and messaging, and required limited financial support, but some time and dedication by leaders and educators. The survey creates awareness, the behavior modeling is critical for educational purposes, and the reminders help to reinforce the new behavior and embed it into routine patient care activities.
One limitation of our review, or potentially a limitation in the state of patient safety education, was the dearth of studies discussing involvement of trainees in RCA following submission of event reports. The National Collaborative for Improving the Clinical Learning Environment suggests that, by using facilitated, interprofessional, systems-based approaches to analyze patient safety events (ie, RCA) and by understanding how these events translate into improvements, residents will be more likely to recognize and report patient safety events.80
One additional component that is critical to the success of event reporting is leadership. While our review did not specifically address the role of leadership, it appears to be a vital element for engaging residents in event reporting. Mitchell and colleagues81 noted, “If the healthcare industry wants to learn from its mistakes, miss or near miss events, it will need to take incident reporting as seriously as the health budget.” Organizational leaders, patient safety leaders, and education leaders must all be invested in creating a culture in which everyone believes that patient safety is a top priority. Engaged leaders will prioritize patient safety so that event reporting is part of the routine culture of patient care and, therefore, encouraged and expected.
Patient safety event reporting is a complex issue that requires a multifaceted approach. The future of engaging residents in incident reporting lies in creating awareness of the issues, targeted behavior modifications, effective messaging and training, robust analysis of the incident reports, and meaningful engagement of physicians. The Accreditation Council for Graduate Medical Education has already begun this process by promoting a culture of safety (ie, supportive culture, emotional support for those involved in patient safety events, and a culture of safety survey), patient safety education, reporting of safety events, and encouraging participation in RCA and disclosure of medical errors. Ultimately, creating a hospital system that effortlessly and continuously collects safety data will solve the challenge of event reporting among physicians.
Conclusions
Based on our study results, the most successful sustainable interventions are those that use a combination of behavior modeling, coupled with surveys and messaging, and that minimize the time required for busy residents by incorporating accessible event reporting in already existing medical records.
Supplementary Material
Footnotes
References
- 1.Kohn L, Corrigan J, Donaldson M, for Committee on Quality of Health Care in America To Err Is Human: Building a Safer Health System. 2000. Washington, DC: Institute of Medicine, National Academies Press; [PubMed]
- 2.Wachter R. Understanding Patient Safety 2nd ed. New York, NY: McGraw-Hill Professional Publishing;; 2012. [Google Scholar]
- 3.Eng JA, Hatoun J, Liu C, Blum-Smith L, Shea S, Suen W. Resident attitudes, knowledge and behaviors regarding an electronic incident reporting system. J Gen Intern Med. 2013;28(1 suppl):88. doi: 10.1007/s11606-013-2436-y. [DOI] [Google Scholar]
- 4.Jagsi R, Kitch BT, Weinstein DF, Campbell EG, Hutter M, Weissman JS. Residents report on adverse events and their causes. Arch Intern Med. 2005;165(22):2607–2613. doi: 10.1001/archinte.165.22.2607. [DOI] [PubMed] [Google Scholar]
- 5.Varkey P, Karlapudi S, Rose S, Swensen S. A patient safety curriculum for graduate medical education: results from a needs assessment of educators and patient safety experts. Am J Med Qual. 2009;24(3):214–221. doi: 10.1177/1062860609332905. [DOI] [PubMed] [Google Scholar]
- 6.Stewart DA, Junn J, Adams MA, Spencer-Segal JL, Perdoncin E, Lopez K, et al. House staff participation in patient safety reporting: identification of predominant barriers and implementation of a pilot program. South Med J. 2016;109(7):395–400. doi: 10.14423/smj.0000000000000486. [DOI] [PubMed] [Google Scholar]
- 7.Peters RH. Strategies for encouraging self-protective employee behavior. J Safety Res. 1991;22(2):53–70. doi: 10.1016/0022-4375(91)90014-M. [DOI] [Google Scholar]
- 8.Porter CM. Revisiting precede-proceed: a leading model for ecological and ethical health promotion. Health Educ J. 2016;75(6):753–764. doi: 10.1177/0017896915619645. [DOI] [Google Scholar]
- 9.Ashar BH, Rice TN, Sisson SD. Physicians' understanding of the regulation of dietary supplements. Arch Intern Med. 2007;167(9):966–969. doi: 10.1001/archinte.167.9.966. [DOI] [PubMed] [Google Scholar]
- 10.Basu A, Gopinath D, Anjum N, Hotchkies S. Feedback in incident reporting—more needed. Clin Gov. 2009;14(1):38–41. doi: 10.1108/14777270910933451. [DOI] [Google Scholar]
- 11.Krouss M, Alshaikh J, Croft L, Morgan DJ. Improving incident reporting among physician trainees. J Patient Saf. 2019;15(4):308–310. doi: 10.1097/PTS.0000000000000325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Louis MY, Dhanraj DN, Khan BS, Jung SR, Quiles WR, Stephens LA, et al. Improving patient safety event reporting among residents and teaching faculty. Ochsner J. 2016;16(1):73–80. [PMC free article] [PubMed] [Google Scholar]
- 13.Martowirono K, Jansma JD, Van Luijk SJ, Wagner C, Bijnen AB. Possible solutions for barriers in incident reporting by residents. J Eval Clin Pract. 2012;18(1):76–81. doi: 10.1111/j.1365-2753.2010.01544.x. [DOI] [PubMed] [Google Scholar]
- 14.McCarthy SE, O'Boyle CA, O'Shaughnessy A, Walsh G. Online patient safety education programme for junior doctors: is it worthwhile? Ir J Med Sci. 2016;185(1):51–58. doi: 10.1007/s11845-014-1218-9. [DOI] [PubMed] [Google Scholar]
- 15.Nabors C, Peterson SJ, Aronow WS, Sule S, Mumtaz A, Shah T, et al. Mobile physician reporting of clinically significant events-a novel way to improve handoff communication and supervision of resident on call activities. J Patient Saf. 2014;10(4):211–217. doi: 10.1097/PTS.0b013e31829952ff. [DOI] [PubMed] [Google Scholar]
- 16.Nabors C, Peterson SJ, Aronow WS, Sule S, Mumtaz A, Jhingan R, et al. Physician reporting of clinically significant events through a computerized patient sign-out system. J Patient Saf. 2011;7(3):155–161. doi: 10.1097/PTS.0b013e31822d7a66. [DOI] [PubMed] [Google Scholar]
- 17.Rosenthal MM, Cornett PL, Sutcliffe KM, Lewton E. Beyond the medical record: other modes of error acknowledgment. J Gen Intern Med. 2005;20(5):404–409. doi: 10.1111/j.1525-1497.2005.0098.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scott DR, Weimer M, English C, Shaker L, Ward W, Choi D, et al. A novel approach to increase residents' involvement in reporting adverse events. Acad Med. 2011;86(6):742–746. doi: 10.1097/ACM.0b013e318217e12a. [DOI] [PubMed] [Google Scholar]
- 19.Steen S, Jaeger C, Price L, Griffen D. Increasing patient safety event reporting in an emergency medicine residency. BMJ Qual Improv Rep. 2017 doi: 10.1136/bmjquality.u223876.w5716. 6(1):u223876.w5716. [DOI] [PMC free article] [PubMed]
- 20.Vohra PD, Johnson JK, Daugherty CK, Wen M, Barach P. Housestaff and medical student attitudes toward medical errors and adverse events. Jt Comm J Qual Patient Saf. 2007;33(8):493–501. doi: 10.1016/S1553-7250(07)33053-5. [DOI] [PubMed] [Google Scholar]
- 21.Boike JR, Bortman JS, Radosta JM, Turner CL, Anderson-Shaw L, Centomani NM, et al. Patient safety event reporting expectation. J Patient Saf. 2013;9(2):59–67. doi: 10.1097/pts.0b013e3182676e53. [DOI] [PubMed] [Google Scholar]
- 22.Weingart SN, Callanan LD, Ship AN, Aronson MD. A physician-based voluntary reporting system for adverse events and medical errors. J Gen Intern Med. 2001;16(12):809–814. doi: 10.1046/j.1525-1497.2001.10231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wild D, Bradley EH. The gap between nurses and residents in a community hospital's error-reporting system. Jt Comm J Qual Patient Saf. 2005;31(1):13–20. doi: 10.1016/S1553-7250(05)31003-8. [DOI] [PubMed] [Google Scholar]
- 24.Valery J, Helmi H, Spaulding A, Che X, Prada G, Chamorro Pareja N, et al. Video intervention to improve incident reporting among medical trainees. BMJ Open Qual. 2019;8(4):e000706. doi: 10.1136/bmjoq-2019-000706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Szymusiak J, Walk TJ, Benson M, Hamm M, Zickmund S, Gonzaga AM, et al. Encouraging resident adverse event reporting. Pediatr Qual Saf. 2019;4(3):e167. doi: 10.1097/pq9.0000000000000167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Singal M, Zafar A, Tbakhi B, Jadhav N, Alweis R, Bhavsar H. Assessment of knowledge and attitudes towards safety events reporting among residents in a community health system. J Community Hosp Intern Med Perspect. 2018;8(5):253–259. doi: 10.1080/20009666.2018.1527670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller ME, Patel A, Schindler N, Hirsch K, Ming M, Weber S, et al. Bridging the gap: interdepartmental quality improvement and patient safety curriculum created by hospital leaders, faculty, and trainees. J Grad Med Educ. 2018;10(5):566–572. doi: 10.4300/JGME-D-18-00060.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krouss M, Alshaikh J, Croft L, Morgan DJ. Improving incident reporting among physician trainees. J Patient Saf. 2019;15(4):308–310. doi: 10.1097/PTS.0000000000000325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.González-Formoso C, Clavería A, Fernández-Domínguez MJ, Lago-Deibe FL, Hermida-Rial L, Rial A, et al. Effectiveness of an educational intervention to improve the safety culture in primary care: a randomized trial. BMC Fam Pract. 2019;20(1):1–10. doi: 10.1186/s12875-018-0901-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kusano AS, Nyflot MJ, Zeng J, Sponseller PA, Ermoian R, Jordan L, et al. Measurable improvement in patient safety culture: a departmental experience with incident learning. Pract Radiat Oncol. 2015;5(3):e229–e237. doi: 10.1016/j.prro.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 31.Appelbaum NP, Dow A, Mazmanian PE, Jundt DK, Appelbaum EN. The effects of power, leadership and psychological safety on resident event reporting. Med Educ. 2016;50(3):343–350. doi: 10.1111/medu.12947. [DOI] [PubMed] [Google Scholar]
- 32.Coffey M, Thomson K, Tallett S, Matlow A. Pediatric residents' decision-making around disclosing and reporting adverse events: the importance of social context. Acad Med. 2010;85(10):1619–1625. doi: 10.1097/acm.0b013e3181f046a6. [DOI] [PubMed] [Google Scholar]
- 33.Bump GM, Coots N, Liberi CA, Minnier TE, Phrampus PE, Gosman G, et al. Comparing trainee and staff perceptions of patient safety culture. Acad Med. 2017;92(1):116–122. doi: 10.1097/ACM.0000000000001255. [DOI] [PubMed] [Google Scholar]
- 34.Flynn-O'Brien KT, Mandell SP, Eaton E. Van, Schleyer AM, McIntyre LK. Surgery and medicine residents' perspectives of Morbidity and Mortality Conference: an interdisciplinary approach to improve ACGME core competency compliance. J Surg Educ. 2015;72(6):e258–e266. doi: 10.1016/j.jsurg.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 35.Friedman SM, Sowerby RJ, Guo R, Bandiera G. Perceptions of emergency medicine residents and fellows regarding competence, adverse events and reporting to supervisors: a national survey. CJEM. 2010;12(6):491–499. doi: 10.1017/S1481803500012719. [DOI] [PubMed] [Google Scholar]
- 36.Garbutt J, Brownstein DR, Klein EJ, Waterman A, Krauss MJ, Marcuse EK, et al. Reporting and disclosing medical errors. Arch Pediatr Adolesc Med. 2007;161(2):179. doi: 10.1001/archpedi.161.2.179. [DOI] [PubMed] [Google Scholar]
- 37.Harrison R, Lawton R, Stewart K. Doctors' experiences of adverse events in secondary care: the professional and personal impact. Clin Med (Lond) 2014;14(6):585–590. doi: 10.7861/clinmedicine.14-6-585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hatoun J, Suen W, Liu C, Shea S, Patts G, Weinberg J, et al. Elucidating reasons for resident underutilization of electronic adverse event reporting. Am J Med Qual. 2016;31(4):308–314. doi: 10.1177/1062860615574504. [DOI] [PubMed] [Google Scholar]
- 39.Logio LS, Ramanujam R. Medical trainees' formal and informal incident reporting across a five-hospital academic medical center. Jt Comm J Qual Patient Saf. 2010;36(1):36–42. doi: 10.1016/S1553-7250(10)36007-7. [DOI] [PubMed] [Google Scholar]
- 40.Poorolajal J, Rezaie S, Aghighi N. Barriers to medical error reporting. Int J Prev Med. 2015;6:97. doi: 10.4103/2008-7802.166680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Coyle YM, Mercer SQ, Murphy-Cullen CL, Schneider GW, Hynan LS. Effectiveness of a graduate medical education program for improving medical event reporting attitude and behavior. Qual Saf Heal Care. 2005;14(5):383–388. doi: 10.1136/qshc.2005.013979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gore DC, Powell JM, Baer JG, Sexton KH, Richardson CJ, Marshall DR, et al. Crew resource management improved perception of patient safety in the operating room. Am J Med Qual. 2010;25(1):60–63. doi: 10.1177/1062860609351236. [DOI] [PubMed] [Google Scholar]
- 43.Jansma JD, Wagner C. Ten Kate RW, Bijnen AB. Effects on incident reporting after educating residents in patient safety: a controlled study. BMC Health Serv Res. 2011;11(1):335. doi: 10.1186/1472-6963-11-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jericho BG, Tassone RF, Centomani NM, Clary J, Turner C, Sikora M, et al. An assessment of an educational intervention on resident physician attitudes, knowledge, and skills related to adverse event reporting. J Grad Med Educ. 2013;2(2):188–194. doi: 10.4300/jgme-d-10-00036.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jones DL. Residents' perspectives on patient safety in university and community teaching hospitals. J Grad Med Educ. 2014;6(3):603–607. doi: 10.4300/jgme-d-14-00350.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kroll L, Singleton A, Collier J. Rees Jones I. Learning not to take it seriously: junior doctors' accounts of error. Med Educ. 2008;42(10):982–990. doi: 10.1111/j.1365-2923.2008.03151.x. [DOI] [PubMed] [Google Scholar]
- 47.Bent PD, Bolsin SN, Creati BJ, Patrick AJ, Colson ME. Professional monitoring and critical incident reporting using personal digital assistants. Med J Aust. 2002;177(9):496–499. doi: 10.5694/j.1326-5377.2002.tb04918.x. [DOI] [PubMed] [Google Scholar]
- 48.Bussel II, Abrahamyan A, Staehle W, Loj J, Patton J. Attitudes of physicians in training regarding reporting of patient safety events. J Clin Outcomes Manag. 2015;22(11):508–511. [Google Scholar]
- 49.Cox LM, Logio LS. Patient safety stories: a project utilizing narratives in resident training. Acad Med. 2011;86(11):1473–1478. doi: 10.1097/ACM.0b013e318230efaa. [DOI] [PubMed] [Google Scholar]
- 50.DeSalvo DJ, Greenberg LW, Henderson CL, Cogen FR. A learner-centered diabetes management curriculum: reducing resident errors on an inpatient diabetes pathway. Diabetes Care. 2012;35(11):2188–2193. doi: 10.2337/dc12-0450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Desbiens NA. Use of a residency program incident reporting system as an educational tool. J Contin Educ Health Prof. 1999;19(3):163–169. [Google Scholar]
- 52.Dunbar AE, III, Cupit M, Vath RJ, Pontiff K, Evans N, Roy M, et al. An improvement approach to integrate teaching teams in the reporting of safety events. Pediatrics. 2017;139(2):e20153807. doi: 10.1542/peds.2015-3807. [DOI] [PubMed] [Google Scholar]
- 53.Falcone JL, Lee KKW, Billiar TR, Hamad GG. Practice-based learning and improvement: a two-year experience with the reporting of morbidity and mortality cases by general surgery residents. J Surg Educ. 2012;69(3):385–392. doi: 10.1016/j.jsurg.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 54.Fox MD, Bump GM, Butler GA, Chen L-W, Buchert AR. Making residents part of the safety culture: improving error reporting and reducing harms. 2020] doi: 10.1097/pts.0000000000000344. [published online ahead of print January 30, J Patient Saf. doi: [DOI] [PubMed]
- 55.Freestone L, Bolsin SN, Colson M, Patrick A, Creati B. Voluntary incident reporting by anaesthetic trainees in an Australian hospital. Int J Qual Health Care. 2006;18(6):452–457. doi: 10.1093/intqhc/mzl054. [DOI] [PubMed] [Google Scholar]
- 56.Gupta S, Naithani U, Brajesh SK, Pathania VS, Gupta A. Critical incident reporting in anaesthesia: a prospective internal audit. Indian J Anaesth. 2009;53(4):425–433. [PMC free article] [PubMed] [Google Scholar]
- 57.Herzer KR, Mirrer M, Xie Y, Steppan J, Li M, Jung C, et al. Patient safety reporting systems: Sustained quality improvement using a multidisciplinary team and “good catch” awards. Jt Comm J Qual Patient Saf. 2012;38(8):339–347. doi: 10.1016/s1553-7250(12)38044-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jansma JD, Wagner C, Bijnen AB. Residents' intentions and actions after patient safety education. BMC Health Serv Res. 2010;10(1):350. doi: 10.1186/1472-6963-10-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Macht R, Balen A, McAneny D, Hess D. A multifaceted intervention to increase surgery resident engagement in reporting adverse events. J Surg Educ. 2015;72(6):e117–e122. doi: 10.1016/j.jsurg.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 60.Murphy M, Duff J, Whitney J, Canales B, Markham M-J, Close J. Implementation of a mock root cause analysis to provide simulated patient safety training. BMJ Open Qual. 2017;6(2):e000096. doi: 10.1136/bmjoq-2017-000096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Okafor N, Doshi P, Miller S, McCarthy JJ, Hoot NR, Darger BF, et al. Voluntary medical incident reporting tool to improve physician reporting of medical errors in an emergency department. West J Emerg Med. 2015;16(7):1073–1078. doi: 10.5811/westjem.2015.8.27390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Plews-Ogan ML, Nadkarni MM, Forren S, Leon D, White D, Marineau D, et al. Patient safety in the ambulatory setting. J Gen Intern Med. 2004;19(7):719–725. doi: 10.1111/j.1525-1497.2004.30386.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Smith A, Hatoun J, Moses J. Increasing trainee reporting of adverse events with monthly trainee-directed review of adverse events. Acad Pediatr. 2017;17(8):902–906. doi: 10.1016/j.acap.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 64.Tevis SE, Schmocker RK, Wetterneck TB. Adverse event reporting: harnessing residents to improve patient safety. J Patient Saf. 2017] doi: 10.1097/PTS.0000000000000333. [published online ahead of print October 13, [DOI] [PMC free article] [PubMed]
- 65.Thoms G, Ellis R, Afolabi G, Graham M. Improving clinical supervision through formal incident reporting. Med Educ. 2012;46(11):1116–1117. doi: 10.1111/medu.12002. [DOI] [PubMed] [Google Scholar]
- 66.Zwart DLM, Heddema WS, Vermeulen MI, Van Rensen ELJ, Verheij TJM, Kalkman CJ. Lessons learnt from incidents reported by postgraduate trainees in Dutch general practice. A prospective cohort study. BMJ Qual Saf. 2011;20(10):857–862. doi: 10.1136/bmjqs.2010.045484. [DOI] [PubMed] [Google Scholar]
- 67.Turner DA, Bae J, Cheely G, Milne J, Owens TA, Kuhn CM. Improving resident and fellow engagement in patient safety through a graduate medical education incentive program. J Grad Med Educ. 2018;10(6):671–675. doi: 10.4300/JGME-D-18-00281.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Keefer P, Helms L, Warrier K, Vredeveld J, Burrows H, Orringer K. SAFEST: use of a rubric to teach safety reporting to pediatric house officers. Pediatr Qual Saf. 2017;2(6):e045. doi: 10.1097/pq9.0000000000000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zwart DLM, Steerneman AHM, Van Rensen ELJ, Kalkman CJ, Verheij TJM. Feasibility of centre-based incident reporting in primary healthcare: the SPIEGEL study. BMJ Qual Saf. 2011;20(2):121–127. doi: 10.1136/bmjqs.2009.033472. [DOI] [PubMed] [Google Scholar]
- 70.Fleming CA, Humm G, Wild JR, Mohan HM, Hornby ST, Harries RL, et al. Supporting doctors as healthcare quality and safety advocates: recommendations from the Association of Surgeons in Training (ASiT) Int J Surg. 2018;52:349–354. doi: 10.1016/j.ijsu.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 71.Foster PN, Sidhu R, Gadhia DA, DeMusis M. Leveraging computerized sign-out to increase error reporting and addressing patient safety in graduate medical education. J Gen Intern Med. 2008;23(4):481–484. doi: 10.1007/s11606-007-0503-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Welsh CH, Pedot R, Anderson RJ. Use of morning report to enhance adverse event detection. J Gen Intern Med. 1996;11(8):454–460. doi: 10.1007/BF02599039. [DOI] [PubMed] [Google Scholar]
- 73.Driver TH, Katz PP, Trupin L, Wachter RM. Responding to clinicians who fail to follow patient safety practices: perceptions of physicians, nurses, trainees, and patients. J Hosp Med. 2014;9(2):99–105. doi: 10.1002/jhm.2136. [DOI] [PubMed] [Google Scholar]
- 74.Parikh RP, Snyder-Warwick A, Naidoo S, Skolnick GB, Patel KB. Impact of an event reporting system on resident complication reporting in plastic surgery training. Plast Reconstr Surg. 2017;140(5):e736–e745. doi: 10.1097/prs.0000000000003771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Heard GC, Sanderson PM, Thomas RD. Barriers to adverse event and error reporting in anesthesia. Anesth Analg. 2012;114(3):604–614. doi: 10.1213/ANE.0b013e31822649e8. [DOI] [PubMed] [Google Scholar]
- 76.Fischer MA, Mazor KM, Baril J, Alper E, DeMarco D, Pugnaire M. Learning from mistakes. Factors that influence how students and residents learn from medical errors. J Gen Intern Med. 2006;21(5):419–423. doi: 10.1111/j.1525-1497.2006.00420.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Saeed SA, Masroor I, Shafqat G. Learning from errors in radiology to improve patient safety. J Coll Physicians Surg Pakistan. 2013;23(10):691–694. doi: 10.2013/JCPSP.691694. [DOI] [PubMed] [Google Scholar]
- 78.Davies J, Chintapatla S, Miller G. Developing a weekly patient safety and quality meeting in a medium-sized GI surgical unit in the United Kingdom. Patient Saf Surg. 2014;8(1):1–4. doi: 10.1186/1754-9493-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Aaronson E, Wittels K, Nadel E, Schuur J. Morbidity and Mortality Conference in emergency medicine residencies and the culture of safety. West J Emerg Med. 2015;16(6):810–817. doi: 10.5811/westjem.2015.8.26559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Disch J, Kilo C, Passiment M, Wagner R, Weiss K. National Collaborative for Improving the Clinical Learning Environment; NCICLE. The role of clinical learning environments in preparing new clinicians to engage in patient safety. 2020 https://psnet.ahrq.gov/issue/role-clinical-learning-environments-preparing-new-clinicians-engage-patient-safety Accessed May 29.
- 81.Mitchell I, Schuster A, Smith K, Pronovost P, Wu A. Patient safety incident reporting: a qualitative study of thoughts and perceptions of experts 15 years after “To Err is Human.”. BMJ Qual Saf. 2016;25(2):92–99. doi: 10.1136/bmjqs-2015-004405. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.