Abstract
Lingual lymph nodes are an inconstant group of in-transit nodes, which are located on the route of lymph drainage from the tongue mucosa to the regional nodes in neck levels I and II. There is growing academic data on the metastatic spread of oral cancer, particularly regarding the spreading of oral tongue squamous cell carcinoma to lingual nodes. These nodes are not currently included in diagnostic and treatment protocols for oral tongue cancer. Combined information on surgical anatomy, clinical observations, means of detection, and prognostic value is presented. Anatomically obtained incidence of lingual nodes ranges from 8.6% to 30.2%. Incidence of lingual lymph node metastasis ranges from 1.3% to 17.1%. It is clear that lymph nodes that bear intervening tissues from the floor of the mouth should be removed to improve loco-regional control. Extended resection volume, which is required for the surgical treatment of lingual node metastasis, cannot be implied to every tongue cancer patient. As these lesions significantly influence prognosis, special efforts of their detection must be made. Reasonably, every tongue cancer patient must be investigated for the existence of lingual lymph node metastasis. Lymphographic tracing methods, which are currently implied for sentinel lymph node biopsies, may improve the detection of lingual lymph nodes.
Keywords: Lingual lymph node, Sublingual lymph node, Tongue cancer, Regional metastasis, Lymph drainage, Head neck region, En-bloc resection
Core tip: Lingual lymph nodes comprise an inconstant group of in-transit nodes, which are located on the route of lymph drainage from the tongue mucosa to the regional nodes in neck levels I and II. This group of lymph nodes may represent a site of tongue cancer metastasis or locoregional recurrence. These nodes are not currently included in diagnostic and treatment protocols for oral tongue cancer. The reported rate of anatomical existence, as well as metastatic lingual node involvement incidence, may not be considered low. As these lesions were shown to significantly influence survival prognosis, special efforts for their detection must be carried out.
INTRODUCTION
Oral cavity carcinoma is a common malignant neoplasm with over 400000 cases detected annually worldwide. Squamous cell carcinoma (SCC) is the most frequent form, accounting for around 90% of malignancies found in the oral cavity region. Among anatomical subsites of the oral cavity, the highest incidence of SCC affection was reported for oral tongue (35.3%)[1-3]. The prognosis for subjects with oral SCC relies of tumor- and host-related features, as well as treatment variations. N stage is deemed to be the most significant predictive factor, since the existence of a single metastatic node in the regional lymphatic basin at referral creates a 50% drop in 5-year survival[4]. SCC has a high potency for regional lymphogenic spread to the neck lymph nodes. Regional lymphatic drainage pathways are well recognized in the head and neck regions, and on this basis, several neck dissection modifications have been elaborated. For oral tongue SCC, the submental, submandibular, and jugulodigastric lymph nodes are known to be the first echelon of draining nodes.
In 1985, Ozeki et al[5] documented lingual lymph nodes (LLNs) as possible sites of metastatic spread for oral tongue SCC. Although anatomical descriptions have long been available in the literature, this paper had first drawn attention due to this inconstant group of lymph nodes in terms of tongue cancer progression. Up until now, considerable clinical data has accumulated on LLN metastasis. The purpose of this paper is to overview the anatomy, the current clinical experience in detection and treatment of metastasis to LLNs, and its influence on survival and prognosis.
Literature sources on LLN metastasis were searched in both PubMed and Google Scholar. As initial clinical descriptions of LLN metastasis were reported by Japanese authors, searches in the J-STAGE scientific database were employed. The heading and key words “lingual lymph node”, “sublingual lymph node”, “tongue cancer”, “regional metastasis”, and “lymph drainage” were used for exploration. The obtained articles were separated into two groups: One including case reports, and one including clinical series and trials related to LLNs. Subject details, tumor stage and characteristics, LLN involvement, treatment modes, and follow-up results were collected from the case report group. In the clinical series and trials group, the following information was acquired: Diagnostic and therapeutic recommendations, survival scores, and prognostic value for patients with LLN lesions.
The review included 27 evaluable papers on LLN metastasis from oral SCC in the form of case reports or clinical series and trials published between 1985 and 2020. The summarized data are presented in Tables 1 and 2.
Table 1.
Case reports of lingual lymph node lesions
| Year | Ref. | Clinical details | Treatment mode/s | Results |
| 1985 | Ozeki et al[5] | Reported 3 cases: (1) A 49-year-old male with SCC of the lateral tongue surface with invasion to the base of the tongue, T3N3M0. During surgery an enlarged median LLN was spotted and resected | Neoadjuvant chemotherapy, hemi-glossectomy with in-continuous bilateral RND | The patient died 9 mo after surgery due to regional recurrence |
| (2) A 54-year-old male with SCC of lateral lingual surface, T1N0M0. One lateral LLN with extracapsular spread encountered in the surgical specimen | Radium needles to the primary site, after 4 mo-unilateral RND with partial resection of the floor of the mouth | No loco-regional recurrence in 5 yr after surgery | ||
| (3) A 63-year-old male with SCC of the margin of the tongue, T2N1M0. One lateral LLN identified in the surgical specimen | Composite resection | The patient died of unrelated causes 10 yr after surgery with no loco-regional recurrence | ||
| 1986 | Honma et al[28] | A 77-year-old male with SCC of the inferior later tongue margin, T2N0M0. Two lateral LLN represented foci of loco-regional recurrence | Primary site treated with radium needles. At 1 mo post-treatment – submaxillary dissection with adjuvant neck radiotherapy | Deceased within 1 yr 4 mo after primary tumor treatment initiation |
| 1989 | Omura et al[29] | A 54-year-old male with SCC of lateral tongue, T2N0. One LLN at the greater cornu of the hyoid spotted during surgery | Primary site treated with radium needles. At 4 mo posttreatment–hemiglossectomy with wide upper neck resection | No loco-regional recurrence in 6 mo after surgery |
| 1999 | Kitada et al[30] | A 73-year-old male with SCC of the lateral lingual margin, T3N2bM0. One metastatic lateral LLN suspected during preoperative CT and MRI | Neoadjuvant radiotherapy, subtotal tongue with ipsilateral mouth floor resection combined with bilateral ND | Local recurrence 3 mo postoperatively, died in 5 mo after surgery |
| 2002 | Dutton et al[25] | A 73-year-old male with SCC of the lateral lingual margin, T2N2b. In the surgical specimen two positive LLN were identified | Partial glossectomy in-continuity with MRND, adjuvant radiotherapy | No loco-regional recurrence in more than 2 yr after surgery |
| 2002 | Ohiro et al[31] | A 28-year-old male with SCC of the later tongue margin, T2N1M0. One metastatic lateral LLN identified on preoperative CT and MRI | Neoadjuvant chemoradiation. Partial glossectomy combined via pull–thorough approach with RND, free flap reconstruction | Follow-up results not stated |
| 2008 | Han et al[32] | A 46-year-old male with SCC of the lateral lingual margin, cT2N0M0. Two LLN noted during surgery showed metastasis on frozen section analysis | Partial glossectomy en-bloc with lateral mouth floor and sublingual gland resection | No loco-regional recurrence in more than 2 yr after surgery |
| 2008 | Kawahara et al[33] | A 56-year-old male with SCC of the lateral tongue, cT3N0M0. One metastatic lateral LLN was detected intraoperatively by palpation | Composite resection of hemi-tongue with floor of the mouth and neck specimen with midline mandible split | No loco-regional recurrence in 2 yr 6 mo postoperatively |
| 2009 | Umeda et al[37] | Reported 2 cases: (1) A 62-year-old male with SCC of the anterior floor of the mouth, T3N2cM0. CT and MRI visualized an enlarged LLN | Resection of the tumor en-bloc with mylohyoid and anterior belly of digastric, bilateral FND, free flap reconstruction. | No loco-regional recurrence, deceased of pneumonia 10 mo after surgery |
| (2) A 62-year-old male with SCC of the median floor of the mouth, T2N2cM0. CT and MRI visualized an enlarged LLN | Resection of the tumor en-bloc with mylohyoid and anterior belly of digastric, bilateral FND, free flap reconstruction | No loco-regional recurrence, deceased of distant metastasis 16 mo after surgery | ||
| 2010 | Ando et al[39] | A 63-year-old male with mouth floor and root of the tongue SCC, three enlarged nodes shown on MRI. Three LLNs in close contact with sublingual gland and one at the root of lingual artery were encountered in the specimen | Subtotal tongue resection en-bloc with bilateral ND | No loco-regional recurrence in 10 mo after surgery |
| 2011 | Zhang et al[34] | Reported 2 cases: (1) A 47-year-old female with ventral lingual surface SCC cT1N0M0 received three operations. (a) 7 mo after first surgery PET-CT suspected LLN lesion; (b) second surgery and adjuvant 60 Gy radiotherapy were carried out; and (c) After 6 mo the third intervention was performed for extensive loco-regional recurrence | (a) Partial glossectomy and discontinuous supraomohyoid ND; (b) Wide local resection with contralateral RND; and (c) Wide local resection, subtotal thyroidectomy, internal carotid artery reconstruction | Patient died 3 mo after the third surgery due to multiple organ failure |
| (2) A 42-year-old man with ventral lingual surface SCC, T2N0MO. Surgical specimen contained one LLN metastasis with extracapsular spread | Partial tongue resection with mouth floor and in-continuity supra-omohyoid ND, free flap reconstruction, adjuvant 60 Gy radiotherapy | No local regional recurrence in 2 yr after surgery | ||
| 2012 | Saito et al[42] | А 81-year-old female with lateral margin of the tongue SCC, T2N0. CT lymphography revealed a metastatic lateral LLN | Partial tongue resection with the identified LLN resection | No loco-regional recurrence in 14 mo after surgery |
| 2014 | Saida et al[26] | A 57-year-old male with cT2N2bM0 SCC of the left lower gingiva | Radical neck dissection, marginal mandibulectomy | No evidence of disease was noted during more than 6 yr of follow-up |
| 2017 | Kaya et al[48] | A 57-year-old male with localized midline floor of the mouth SCC, T1N0M0. The primary site resection specimen contained one metastatic LLN | Primary tumor resection en-bloc with sublingual glands and bilateral discontinuous selective ND. Adjuvant radiotherapy | No loco-regional recurrence in 12 mo after surgery |
| 2017 | Nishio et al[41] | Lingual lymph node metastasis from an early tongue cancer detected by ultrasound exam during follow-up | The patient underwent complete surgical resection | No evidence of recurrence 5 yr later |
| 2019 | Eguchi et al[18] | A 55-year-old male with tongue border SCC, cT4aN0M0. (1) Firm medial LLN was detected in the lingual septum during initial surgery, after which the patient was staged pT4aN2b; (2) At 6 mo later due to contralateral regional recurrence second surgery undertaken; (3) At 14 mo after first treatment multiple distant lesions diagnosed | (a) Hemiglossectomy with partial genioglossus and geniohyoid resection, ipsilateral supraomohyoid ND, free flap reconstruction; (b) Contralateral MRND, adjuvant chemo-radiation; and (c) Palliative chemo-radiation | Died of distant disease 18 after initial surgery |
LLNs: Lingual lymph nodes; SCC: Squamous cell carcinoma; ND: Neck dissection; RND: Radical neck dissection; MRND: Modified radical neck dissection; MRI: Magnetic resonance imaging; CT: Computed tomography.
Table 2.
Clinical series related to lingual lymph nodes
| Year | Ref. | Clinical data | Recommendations |
| 1994 | Omura et al[36] | Reported 1 case of median LLN and 3 cases of lateral LLN among 311 patients (1.3%) with tongue SCC | Mandatory intraoperative palpation in the areas of potential LLNs location |
| 2009 | Ando et al[35] | Observed parahyoid nodes involvement in 6.3% of 248 patients with T1-2 oral tongue SCC | Intraoperative inspection of tissue along the course of lingual artery for possible firm LLN during ND |
| 2010 | Hoshina et al[16] | Positive in-transit LLNs visualized and proven metastatic in 16.3% of their 43 patients | Routine preoperative imaging and careful data interpretation for possible occult in-transit LLN metastasis |
| 2011 | Calabrese et al[38] | Designed a modification of in-continuous resection. 143 patients with previously untreated tongue SCC. In 5 years, loco-regional control was 83.5% (24.4% improvement on standard surgery); overall survival of 70.7% (27.3% improvement) | Advocated en-bloc resection of a hemi-tongue compartment that includes the underlying mouth floor tissues, the stylohyoid and mylohyoid muscles |
| 2016 | Suzuki et al[14] | Reported incidence of 8% of LLNs metastasis in a series of 100 tongue SCC | Proposed recommendations for choosing surgical access to different groups of LLNs |
| 2017 | Tomblinson et al[13] | 500 consecutive face-neck MRI-scans were reviewed for structures consistent with median LLNs | In the study group, 1 (0.95%) of 105 cases demonstrated a single median LLN metastasis from a lateral tongue tumor |
| 2018 | Jia et al[46] | Reported total incidence of LLN metastasis of 17.1% in 111 patients with T0-4, N0, N+ tongue cancer | The existence of LLN metastasis was found to significantly associate with the pathological grade of the tumor |
| 2019 | Fang et al[47] | Treated 231 patients with T2-4, N0, N+ tongue SCC, all underwent an in-continuity operation. The surgical specimen of the floor of the mouth was separated postoperatively and histologically studied for the presence of LLNs and LLNs metastasis | It was shown that LLN metastasis were significantly related with the following pathologic features: the lymphovascular and peritumoral invasion, tumor stage, regional metastasis and malignancy grade |
LLNs: Lingual lymph nodes; SCC: Squamous cell carcinoma; ND: Neck dissection; RND: Radical neck dissection; MRND: Modified radical neck dissection; FND: Functional neck dissection.
ANATOMY
LLN classification
One of the earliest references to LLNs are found in Kuttner’s work on tongue cancer spreading to regional lymph nodes, wherein he illustrated that up to three nodes localized near the sublingual salivary gland[6]. Traditional classification of LLNs, which is still generally applied today, was proposed by Rouviere[7] in 1938. In the classic tutorial Anatomy of the human lymphatic system, he grouped LLNs as rare median and more prominent lateral. In a study of embryos, Katayama found that the incidence of median LLNs is 15.1% and lateral LLNs is 30.2%[8]. In an anatomical study of 104 adult cadavers, LLNs were observed within the tongue musculature in 8.6%, and were outlined as regional draining lymph nodes of the tongue[9]. Later, the LLNs were termed as “interrupting nodules”, which are situated along the collecting lymphatic trunks of the tongue and the sublingual gland as an insertion on the lymphatic flow pathway to levels I and II[10]. Shelomentsev and Sushentsov (1975) documented the close connections of lingual lymphatic vessels to the sublingual salivary gland. Lingual lymphatics were shown to pass through the sublingual gland parenchyma and drain it. The authors discovered that the major lingual efferent lymphatic trunks are located along the lingual vein in the sublingual and upper neck regions[11]. Ananian et al[12] reported a 23.8% incidence of lateral LLNs, and further divided them into parahyoid and paraglandular nodes according to their position. No median LLNs were identified. Median LLNs were spotted as rare as 0.95% in a large imaging series[13]. Surgical-anatomical classification of LLNs was proposed by Suzuki et al[14], where LLNs were distributed into four subgroups: Median LLNs, anterolateral LLNs (located in proximity to the sublingual gland), parahyoid LLNs (located along the greater cornu of the hyoid bone), and posterolateral LLNs. This group consists of one or two small lymph nodes outside the sublingual and floor of the mouth regions. These nodes reside between the posterior edge of the mylohyoid and the inner surface of the submandibular gland. In a study by DiNardo et al[15], this lymph node was depicted in detail earlier and termed as the deep submandibular node. It was proposed that this node is located along the course of the lymph drainage route that is directed straight to level II from the tongue margin mucosa[16]. These works were based on clinical observations of metastatic spread. The precise affiliation of this node is debatable, since it topographically belongs to the submandibular space, which is outside the sublingual and floor of the mouth regions. On the other hand, relevant anatomical material was recently published by Eguchi et al[17]. During gross dissection, the authors managed to identify a thin fascial lamina located deep to the submandibular salivary gland that covered the hyoglossus muscle and the lingual and hypoglossal nerves. It was stated that this fascial layer is distinct from the superficial layer of the deep cervical fascia, which splits to envelope the superficial and deep surfaces of the submandibular gland. The authors assumed that the posterolateral LLN or deep submandibular node is also covered by that facial layer, which in turn extends to the sublingual region. These nodes therefore may be anatomically related to the LLN group[17]. Further micro- and macroscopic research of the floor of the mouth and submandibular triangle anatomy is needed to clarify this controversial issue.
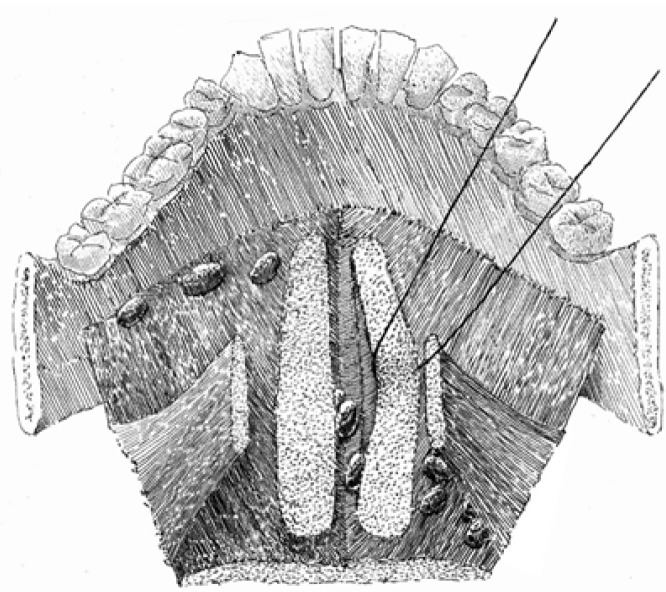
Spatial arrangement of the floor of the mouth
For a clear understanding of the LLN location, the presentation of the spatial arrangement of the mouth floor is valuable (Figure 1). The floor of the mouth region is composed of five intermuscular gaps; these include one unpaired median gap, and two paired later spaces, the floor for them all of which is constituted by the upper surface of mylohyoid muscles. The median or central space lies in between the inner surfaces of the genioglossal and geniohyoid muscles. Anteriorly, it is bounded by the medial aspect of the mandibular lingual cortical plate and anteromedially by tendinous muscular attachments to the mental spine. Posteriorly, the space is continuous with the fatty tissue of the root of the tongue. This space is enclosed by skeletal muscles and has no connections with both lateral spaces. Median LLNs may be contained in this space on each side of the lingual septum in a sagittal position of three-fourth of the distance from the mental spine[18]. Moving outwards, the intermediate lateral space is encountered. This lies surrounded by the lateral surfaces of the genioglossal and geniohyoid, and the medial surface of the hyoglossal muscle. Anteriorly, it is continuous with the lateral gap of the floor of the mouth, and posteriorly, the areolar tissue extends into the parapharyngeal space. The lingual artery travels along this anatomical space, and here the lateral parahyoid LLNs can be found at the great cornu of the hyoid bone. The third space is anteriorly and laterally limited by the lingual cortical plate of the mandible and the sublingual fossa of the mandible. Anteromedially, the space is bounded by the anterior division of the genioglossal and the geniohyoid muscles. Posteromedially, it opens into the intermediate lateral space of the mouth floor. Posterolaterally, it extends into the submandibular space via the aperture between the mylohyoid and hyoglossal muscles. This space harbors the following structures: Deep lingual vein, hypoglossal, lingual and mylohyoid nerves, deep lobe of the submandibular salivary gland, submandibular duct, and sublingual salivary gland[19,20]. The lateral paraglandular LLNs lie in this space adjacent to the sublingual salivary gland.
Figure 1.
Intermuscular spaces in the floor of the mouth. The median LLNs are situated in the central unpaired space, and the anterolateral (paraglandular) and posterolateral (parahyoid) nodes are located in the intermediate and outmost lateral spaces.
Lymphatic drainage pathways
The lymphatics from the anterior two thirds of the tongue (the oral portion) may be divided into two divisions: Marginal and central vessels[21,22]. The marginal vessels receive lymph from the outer one third of the upper surface of the tongue, the marginal surface, and tissues close to the sublingual region. The more anterior marginal vessels originate behind the tip of the tongue, pass laterally downward and through the mylohyoid muscle to finish in the submental nodes, or are addressed towards the submandibular nodes. The posterior marginal lymphatics direct downward and laterally pass the posterior border of the mylohyoid muscle to reach the deep cervical lymph nodes. The central group of vessels situated at the tip of the tongue proceed through the mylohyoid muscle to drain into the submental nodes (level IA). Less commonly, lymphatics may course caudally across the hyoid bone to join nodes of the deep cervical chain, which particularly include the jugulodigastric and rarely the jugulo-omohyoid nodes. The central route from the remainder of the upper surface of the tongue runs mainly between the genioglossus and geniohyoid muscles towards the submental, submandibular nodes, or avoiding these groups that connect directly to the upper deep cervical nodes. The mylohyoid muscle is penetrated by the lymphatic vessels that run to the regional lymphatic basin from the tongue and floor of the mouth in two locations, the anterior and posterior portions of the muscle, thus connecting oral mucosa lymphatics with levels I, II and III[15,23,24].
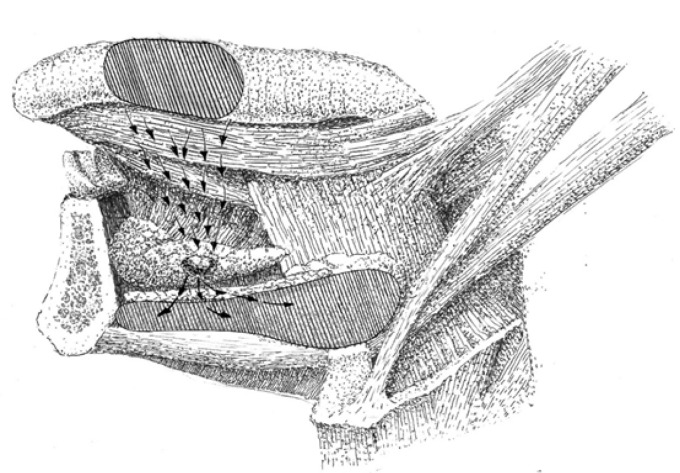
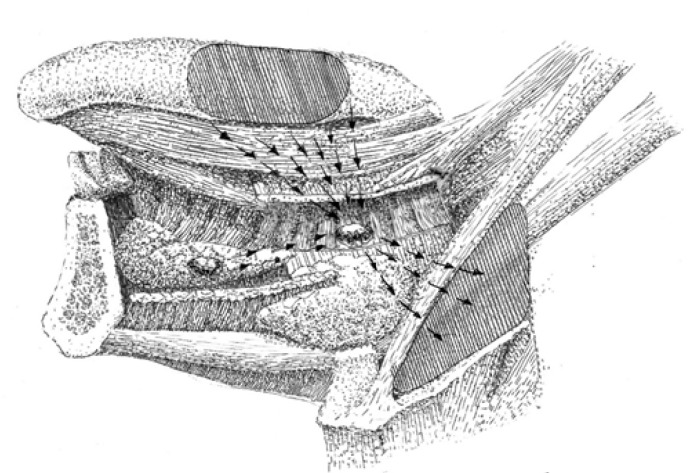
According to the interposition of LLNs on the lymphatic route from the primary site in the tongue to the regional nodes in levels I and II, they were termed as intervening[25,26], in-transit[16], and intercalated[27] in the literature. Generally, there are two main lateral directions of lymph transit from the oral tongue mucosa, which are anatomically delineated by the plane of the mylohyoid muscle. In the route of these two drainage pathways, lateral LLN may function as in-transit intermediary lymphatic elements[10]. The first pathway leads straight to level I through the mylohyoid muscle and further continues to levels II or III. The anterolateral or paraglandular LLNs may reside between the primary site in the anterior part of the tongue and level I (Figure 2). The second pathway is directed more horizontally and backward toward level II, specifically to the jugulodigastric node. This route runs along the upper surface of the mylohyoid (without penetrating it) towards the hyoglossus muscle and the greater cornu of the hyoid bone, and drains into level II nodes. It may in some instances incorporate a paraglandular LLN, but it is more probable to occur in the posterolateral or parahyoid LLN as well as the deep submandibular in-transit node, which were described by Hoshina et al[16] as located on the course to level II (Figure 3). The central drainage pathway courses along the midline and spreads bilaterally towards levels I and II, depending on the sagittal position of the primary site. If present, the median LLNs receive lymph before it transcends the mylohyoid muscle and drains into regional lymph nodes[15].
Figure 2.
Lymph drainage direction toward the paraglandular LLNs. The paraglandular LLN lies in an in-transit position of the lymph flow (arrows) from the oral tongue mucous membrane to regional level I.
Figure 3.
Lymph drainage direction toward the parahyoid LLNs. Parahyoid LLN lies in an in-transit position of the lymph flow (arrows) from the tongue mucous membrane to level II. If present, paraglandular LLN may drain into the parahyoid LLN.
CLINICAL EXPERIENCE
Case reports and series
The first three observations of tongue SCC with metastasis to the lateral and median LLN were described by Ozeki et al[5]. This was followed by case reports of LLN involvement detected in different clinical settings: As loco-regional recurrence[28], during surgery[29], and on preoperative CT and MRI[30,31]. Only two out of the six subjects with LLN lesions had survived recurrent-free during the stated follow-up period. Both of these patients received radium needle treatment for the primary tumor and an in-continuous surgery with wide floor of the mouth and upper neck resection. Dutton et al[25] suggested a local resection of the mouth floor in combination with partial glossectomy for oral tongue SCC with risk for LLN involvement as a potential substitute for an in-continuity surgical approach. The lateral anatomical space of floor of the mouth can be accessed intra-orally and dissected simultaneously to glossectomy. With such access, the sublingual gland is removed in en-bloc fashion with sublingual loose fatty tissue. Han et al[32], Kawahara et al[33], and Zhang et al[34] reported successful surgical treatment that incorporated hemi- or partial glossectomy combined with sublingual gland and floor of the mouth resection in 3 N0 patients with lateral LLN metastasis. Ando et al[35] was the first to distinguish the parahyoid group of LLNs. Located at the root of the lingual artery close to the cornu of the hyoid bone, these were observed to harbor tongue SCC metastasis in 6.3% of their 248 patients. This incidence was significantly higher than that reported in previous work, which ranged between 1.3%-2.1%[5,36]. It was suspected that small LLN size and their anatomical contiguity to the primary tumor precludes accurate in-time identification of LLN as a focus of metastasis or recurrence. This may also explain why there have only been two reported descriptions of LLN metastasis of SCC of the floor of the mouth[37]. Hoshina et al[16] observed lateral LLN metastasis in 16.3% of 43 patients with tongue SCC. Suzuki et al[14] reported an 8% incidence of LLN metastasis in a series of 100 tongue SCCs, and proposed recommendations for choosing surgical access to different LLN groups. The anterolateral paraglandular nodes are accessed intraorally, the posterolateral parahyoid node resection requires additional dissection of the tissue at the greater cornu of the hyoid close to the parapharyngeal space, and the deep submandibular node should be removed during neck dissection together with the submandibular salivary gland. It is evident that the lymph node bearing intervening tissues of the floor of the mouth should be removed to improve loco-regional control. A modification of an in-continuous approach, which is based on a principle of fascial tongue compartments, was designed by Calabrese et al[38]. The authors performed a wide resection of a tongue compartment that included the adjacent floor of the mouth, mylohyoid, and stylohyoid muscles. In a study of 143 subjects with cT2-4a, cN0, cN+, and M0 tongue SCC, they reported 16.8% improvement in local control, 24.4% improvement in loco-regional control, and a 27.3% improvement in overall survival compared to standard surgery. Median LLN metastasis was very rarely observed. Eguchi et al[18] summarized the details of seven published cases of median LLN metastasis secondary to tongue SCC, and presented one new case. It was concluded that median LLN lesions are strongly associated with bilateral metastatic spread.
LLN detection
Detection of LLN metastasis is a crucial but most often neglected part of diagnosis and surgical treatment planning, especially in otherwise cN0 patients. Reasonably, every patient with tongue cancer must be investigated for the presence of LLN lesions. Preoperative palpation may bring out a suspicion of firm LLNs: Median and anterolateral paraglandular LLN lesions are palpated intraorally along the median and lateral aspects of the sublingual region; posterolateral LLN lesions are bimanually accessed and palpated in the mandibular-lingual groove. Attentive palpation at the area of the greater cornu of the hyoid bone and along the lingual vessels course helps to intraoperatively detect LLN metastasis during neck dissection[29,35,36].
LLNs are an inconstant lymph node group with an extended surgical volume that is required for the surgical treatment of LLN metastasis, which cannot be implied for every tongue cancer patient. Anatomically-obtained incidences of LLN range from 8.6% to 30.2%[8,9,12]. This necessitates the performance of various preoperative imaging modes with consequent meticulous data analysis. CT and MRI were reported to be effective for LLN metastasis visualization in cN+ staged cases[30,31,37,39]. Several researchers outlined the benefits of combining preoperative contrast-enhanced CT and MRI (central necrosis and/or extracapsular spread are usual findings in LLN metastasis), and postoperative ultrasound monitoring (every month follow-up)[40,41]. Saito et al[42] spotted a metastatic lateral LLN in a patient with T2 tongue SCC using CT lymphography with peritumoral iopamidol injection, and stressed the possibility that LLNs may serve as sentinel lymph nodes. Sugiyama et al[43] used CT lymphography in 20 patients with cN0 oral tongue and floor of the mouth cancer. They noticed two LLNs, which were accepted as sentinel lymph nodes, and stated that LLN may be readily identified in 3D with this technique. This suggests that special lymphographic tracing techniques, which are used for sentinel lymph node mapping and biopsy, may be useful in the pre- or intraoperative identification of LLNs[44,45].
Prognosis
Few clinical studies are available in the literature that imply homogenous groups, treatment and/or investigation standardization, long-term follow up, and prognosis calculations. The initial statistical proof that LLN metastases are correlated with worsening of survival prognosis was presented by Hoshina et al[16]. They observed seven cases of lateral LLN and 3 cases of deep in-transit submandibular node metastases in 43 tongue SCC patients. The associated incidence of delayed regional metastasis development with the presence of LLN lesions was estimated to be 85.7%, with 100% demonstrating a presence of deep submandibular node metastatic involvement. Jia et al[46] documented a total incidence of LLN metastasis in 17.1% of 111 patients with T0-4, N0 , and N+ tongue cancer. The existence of LLN metastasis was found to be significantly associated with the pathological grade of the tumor. A large clinical study was carried out by Fang et al[47]. They treated 231 patients with T2-4, N0, and N+ tongue SCC, and all subjects underwent an in-continuity operation. The surgical specimen of the floor of the mouth was separated postoperatively, and then histologically examined for the presence of LLNs and LLN metastasis. LLNs were identified in 58 patients (23.1%), with a mean number of 1.3. Of these patients, 33 had metastatic deposits within the LLN, with a total LLN metastasis incidence of 14.3%. It was shown that LLN metastasis was significantly related with the following pathological features: Lymphovascular and peritumoral invasion, tumor stage, presence of regional metastasis, and malignancy grade. The loco-regional control rate was significantly related to the finding of LLN metastasis. For patients who exhibited LLN metastasis, the 5-year loco-regional control rate was estimated to be 45%, while this rate was estimated to be 65% in patients without LLN lesions. According to these new data, LLN metastasis should be considered as an adverse prognostic factor, as well as a strong sign of high primary tumor aggressiveness.
CONCLUSION
While summarizing the available literature on LLNs, it becomes obvious that rates of anatomical existence and metastatic LLN involvement incidence may in not be considered low. Surgical excision implies that adjacent sublingual glands and floor of the mouth subunits are included in the volume of resected tissues. This assures treatment radicality, although it cannot be applied to all tongue cancer patients. As these lesions were shown to significantly influence prognosis, special efforts for their detection must be made. Such measures as pre- or intraoperative palpatory inspection may uncover occult disease in the LLNs. Preoperative contrast-enhanced CT and MRI with postoperative ultrasound follow-up exams are diagnostically beneficial for cN0 patients. Special lymphographic tracing methods as used for sentinel lymph node mapping have the potential to improve LLN identification. In addition, more clinical studies on LLN metastasis diagnosis and treatment must be performed for the possible inclusion of these nodes in the TNM staging system.
ACKNOWLEDGEMENTS
The authors would like to thank Alexander Gaprindashvili for the artwork development.
Footnotes
Conflict-of-interest statement: The authors declare no conflict of interests for this article.
Manuscript source: Invited manuscript
Peer-review started: December 31, 2019
First decision: March 24, 2020
Article in press: May 5, 2020
Specialty type: Oncology
Country/Territory of origin: Russia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: de Melo FF, Sukocheva O S-Editor: Wang J L-Editor: Filipodia E-Editor: Liu MY
Contributor Information
Shalva R Gvetadze, Central Research Institute of Dentistry and Maxillofacial Surgery, Moscow 119991, Russia. shalvagvetadze@yandex.ru.
Konstantin D Ilkaev, Central Research Institute of Dentistry and Maxillofacial Surgery, Moscow 119991, Russia; Blokhin National Medical Research Center of Oncology, Moscow 115478, Russia.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 3.Weatherspoon DJ, Chattopadhyay A, Boroumand S, Garcia I. Oral cavity and oropharyngeal cancer incidence trends and disparities in the United States: 2000-2010. Cancer Epidemiol. 2015;39:497–504. doi: 10.1016/j.canep.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woolgar JA, Triantafyllou A, Lewis JS Jr, Hunt J, Williams MD, Takes RP, Thompson LD, Slootweg PJ, Devaney KO, Ferlito A. Prognostic biological features in neck dissection specimens. Eur Arch Otorhinolaryngol. 2013;270:1581–1592. doi: 10.1007/s00405-012-2170-9. [DOI] [PubMed] [Google Scholar]
- 5.Ozeki S, Tashiro H, Okamoto M, Matsushima T. Metastasis to the lingual lymph node in carcinoma of the tongue. J Maxillofac Surg. 1985;13:277–281. doi: 10.1016/s0301-0503(85)80064-3. [DOI] [PubMed] [Google Scholar]
- 6.Küttner H. Über die Lymphgefäße und Lymphdrüsen der Zunge mit Beziehung auf die Verbreitung des Zungencarcinoms. Beitr Klin Chir. 1898;21:732. [Google Scholar]
- 7.Rouviere H. Michigan, Ann Arbor: Edwards Brother, Inc; 1938. Anatomy of the human lymphatic system. [Google Scholar]
- 8.Katayama T. Anatomical study of the lymphatic system of the mouth. J Nippon Dent Assoc. 1943;30:647-677. [Google Scholar]
- 9.Mashkov OA. Anatomy and topography of lymphatic vessels and regional lymph nodes of adult human tongue. Moscow: I.M.Sechenov First Moscow State Medical University, 1968. [Google Scholar]
- 10.Feind CR, Haagensen CD. The head and neck. The Lymphatics in Cancer. Pennsylvania, Philadelphia: Saunders WB, 1972. [Google Scholar]
- 11.Shelomentsev IuA, Sushentsov AA. [Certain principles of prevention of recurrences after surgical treatment of tongue cancer] Vestn Khir Im I I Grek. 1975;114:71–74. [PubMed] [Google Scholar]
- 12.Ananian SG, Gvetadze SR, Ilkaev KD, Mochalnikova VV, Zayratiants GO, Mkhitarov VA, Yang X, Ciciashvili AM. Anatomic-histologic study of the floor of the mouth: the lingual lymph nodes. Jpn J Clin Oncol. 2015;45:547–554. doi: 10.1093/jjco/hyv029. [DOI] [PubMed] [Google Scholar]
- 13.Tomblinson CM, Nagel TH, Hu LS, Zarka MA, Hoxworth JM. Median Lingual Lymph Nodes: Prevalence on Imaging and Potential Implications for Oral Cavity Cancer Staging. J Comput Assist Tomogr. 2017;41:528–534. doi: 10.1097/RCT.0000000000000568. [DOI] [PubMed] [Google Scholar]
- 14.Suzuki M, Eguchi K, Ida S, Okada R, Kawada T, Kudo T. Lateral lingual lymph node metastasis in tongue cancer and the clinical classification of lingual lymph nodes. J Jpn Soc Head Neck Surg. 2016;26:71–78. [Google Scholar]
- 15.DiNardo LJ. Lymphatics of the submandibular space: an anatomic, clinical, and pathologic study with applications to floor-of-mouth carcinoma. Laryngoscope. 1998;108:206–214. doi: 10.1097/00005537-199802000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Hoshina Y, Hayashi T, Shingaki S, Saito C. Imaging features of in-transit lymph node metastases in patients with tongue carcinoma. J Jpn Soc Oral Oncol. 2010;22:25–36. [Google Scholar]
- 17.Eguchi K, Muro S, Miwa K, Yamaguchi K, Akita K. Deep cervical fascia as an anatomical landmark of lingual lymph nodes: An anatomic and histologic study. Auris Nasus Larynx. 2019;S0385-8146:30930–7. doi: 10.1016/j.anl.2019.11.007. [DOI] [PubMed] [Google Scholar]
- 18.Eguchi K, Kawai S, Mukai M, Nagashima H, Shirakura S, Sugimoto T, Asakage T. Medial lingual lymph node metastasis in carcinoma of the tongue. Auris Nasus Larynx. 2020;47:158–162. doi: 10.1016/j.anl.2019.03.003. [DOI] [PubMed] [Google Scholar]
- 19.Grodinsky M. RETROPHARYNGEAL AND LATERAL PHARYNGEAL ABSCESSES: AN ANATOMIC AND CLINICAL STUDY. Ann Surg. 1939;110:177–199. doi: 10.1097/00000658-193908000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lindner HH. The anatomy of the fasciae of the face and neck with particular reference to the spread and treatment of intraoral infections (Ludwig's) that have progressed into adjacent fascial spaces. Ann Surg. 1986;204:705–714. doi: 10.1097/00000658-198612000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hollinshead WH. Anatomy for surgeons. Head and neck. Pennsylvania, Philadelphia: Harper Row, 1982. [Google Scholar]
- 22.Werner JA, Dünne AA, Myers JN. Functional anatomy of the lymphatic drainage system of the upper aerodigestive tract and its role in metastasis of squamous cell carcinoma. Head Neck. 2003;25:322–332. doi: 10.1002/hed.10257. [DOI] [PubMed] [Google Scholar]
- 23.Abe M, Murakami G, Noguchi M, Yajima T, Kohama GI. Afferent and efferent lymph-collecting vessels of the submandibular nodes with special reference to the lymphatic route passing through the mylohyoid muscle. Head Neck. 2003;25:59–66. doi: 10.1002/hed.10188. [DOI] [PubMed] [Google Scholar]
- 24.Pan WR, Suami H, Taylor GI. Lymphatic drainage of the superficial tissues of the head and neck: anatomical study and clinical implications. Plast Reconstr Surg. 2008;121:1614–24; discussion 1625-6. doi: 10.1097/PRS.0b013e31816aa072. [DOI] [PubMed] [Google Scholar]
- 25.Dutton JM, Graham SM, Hoffman HT. Metastatic cancer to the floor of mouth: the lingual lymph nodes. Head Neck. 2002;24:401–405. doi: 10.1002/hed.10026. [DOI] [PubMed] [Google Scholar]
- 26.Saida K, Naganawa Y, Umemura M, Oto H, Iwai S, Sakuma H. A case of multiple metastases to the lateral lymph nodes from carcinoma of the lower gingiva. Jpn J Oral Maxillofac Surg. 2014;60:257–261. [Google Scholar]
- 27.Kimura Y, Hanazawa T, Okano T. Lingual lymph node metastases from carcinoma of the tongue and floor of the mouth suspected by image findings: clinical analysis and a review of the Japanese literature. Toukeibu Gan. 2010;36:488–497. [Google Scholar]
- 28.Honma Y, Kinoshita Y, Asano N, Mizutani N, Kakuta T, Hirai E, Shimura K. Metastasis to the lingual lymph node in carcinoma of the tongue: report of a case. Jpn J Oral Maxillofac Surg. 1986;32:1522–1524. [Google Scholar]
- 29.Omura K, Takemiya S, Shimada F, Hayashi N. Lingual node metastasis from tongue cancer: report of a case. Jpn J Oral Maxillofac Surg. 1989;35:996–1000. [Google Scholar]
- 30.Kitada H, Harada S, Ishikawa M, Notani K, Fukuda H, Shindoh M. A case of metastasis to the lateral lingual lymph nodes in a patient with carcinoma of the tongue detected preoperatively. Jpn J Oral Maxillofac Surg. 1999;45:620–622. [Google Scholar]
- 31.Ohiro Y, Tei K, Kashiwazaki H, Totsuka Y, Iizuka T, Minowa K. A case of metastasis to the lateral lingual lymph nodes in a patient with a preoperative diagnosis of carcinoma of the tongue. Jpn J Oral Maxillofac Surg. 2002;48:359–362. [Google Scholar]
- 32.Han W, Yang X, Huang X, Hu Q, Wang Z. Metastases to lingual lymph nodes from squamous cell carcinoma of the tongue. Br J Oral Maxillofac Surg. 2008;46:376–378. doi: 10.1016/j.bjoms.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 33.Kawahara K, Kamiya Y, Ozawa N, Yamada T, Watanabe H, Sano D. A case of metastasis to the lateral lingual lymph nodes in a patient with carcinoma of the tongue, confirmed by palpation during operation. J Jpn Soc Oral Oncol. 2008;20:131–136. [Google Scholar]
- 34.Zhang T, Ord RA, Wei WI, Zhao J. Sublingual lymph node metastasis of early tongue cancer: report of two cases and review of the literature. Int J Oral Maxillofac Surg. 2011;40:597–600. doi: 10.1016/j.ijom.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 35.Ando M, Asai M, Asakage T, Oyama W, Saikawa M, Yamazaki M, Miyazaki M, Ugumori T, Daiko H, Hayashi R. Metastatic neck disease beyond the limits of a neck dissection: attention to the 'para-hyoid' area in T1/2 oral tongue cancer. Jpn J Clin Oncol. 2009;39:231–236. doi: 10.1093/jjco/hyp001. [DOI] [PubMed] [Google Scholar]
- 36.Omura K, Takemiya S, Shimada F, Makino S, Katahashi T, Honda T, Hayashi N, Okamura H. Lingual lymph node metastasis from tongue cancer. Jpn J Head Neck Cancer. 1994;20:50–56. [Google Scholar]
- 37.Umeda M, Minamikawa T, Shigeta T, Oguni A, Kataoka T, Takahashi H, Shibuya Y, Komori T. Metastasis to the lingual lymph node in patients with squamous cell carcinoma of the floor of the mouth: a report of two cases. Kobe J Med Sci. 2010;55:E67–E72. [PubMed] [Google Scholar]
- 38.Calabrese L, Bruschini R, Giugliano G, Ostuni A, Maffini F, Massaro MA, Santoro L, Navach V, Preda L, Alterio D, Ansarin M, Chiesa F. Compartmental tongue surgery: Long term oncologic results in the treatment of tongue cancer. Oral Oncol. 2011;47:174–179. doi: 10.1016/j.oraloncology.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 39.Ando M, Asai M, Ono T, Nakanishi Y, Asakage T, Yamasoba T. Metastases to the lingual nodes in tongue cancer: a pitfall in a conventional neck dissection. Auris Nasus Larynx. 2010;37:386–389. doi: 10.1016/j.anl.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 40.Hayashi N, Okamura H, Tanaka H, Ogoh K, Hashiguchi M, Masui I, Honda T, Komoto K, Hayashi T, Omura K. Median lingual lymph node metastasis from tongue cancer. Report of a case. Jpn J Oral Maxillofac Surg. 1992;38:140–141. [Google Scholar]
- 41.Nishio N, Fujimoto Y, Hiramatsu M, Yamamoto Y, Sone M. Sonographic detection of a lingual node metastasis from early squamous cell cancer of the tongue. J Clin Ultrasound. 2018;46:69–72. doi: 10.1002/jcu.22486. [DOI] [PubMed] [Google Scholar]
- 42.Saito M, Nishiyama H, Oda Y, Shingaki S, Hayashi T. The lingual lymph node identified as a sentinel node on CT lymphography in a patient with cN0 squamous cell carcinoma of the tongue. Dentomaxillofac Radiol. 2012;41:254–258. doi: 10.1259/dmfr/61883763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sugiyama S, Iwai T, Izumi T, Ishiguro K, Baba J, Oguri S, Mitsudo K. CT lymphography for sentinel lymph node mapping of clinically N0 early oral cancer. Cancer Imaging. 2019;19:72. doi: 10.1186/s40644-019-0258-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yang Y, Zhou J, Shi X, Sha Y, Wu H. Long-term observation of indirect lymphography using gadolinium-loaded polyethylenimine-entrapped gold nanoparticles as a dual mode CT/MR contrast agent for rabbit lingual sentinel lymph node identification. Acta Otolaryngol. 2017;137:207–214. doi: 10.1080/00016489.2016.1222550. [DOI] [PubMed] [Google Scholar]
- 45.Wu WJ, Zheng L, Zhang JG. The use of carbon nanoparticles to track occult lingual lymph nodes in early-stage tongue squamous cell carcinoma. Int J Oral Maxillofac Surg. 2019;48:1153–1155. doi: 10.1016/j.ijom.2019.02.010. [DOI] [PubMed] [Google Scholar]
- 46.Jia J, Jia MQ, Zou HX. Lingual lymph nodes in patients with squamous cell carcinoma of the tongue and the floor of the mouth. Head Neck. 2018;40:2383–2388. doi: 10.1002/hed.25340. [DOI] [PubMed] [Google Scholar]
- 47.Fang Q, Li P, Qi J, Luo R, Chen D, Zhang X. Value of lingual lymph node metastasis in patients with squamous cell carcinoma of the tongue. Laryngoscope. 2019;129:2527–2530. doi: 10.1002/lary.27927. [DOI] [PubMed] [Google Scholar]
- 48.Kaya İ, Öztürk K, Turhal G. Sublingual Lymph Node Metastasis in Early-Stage Floor of the Mouth Carcinoma. Turk Arch Otorhinolaryngol. 2017;55:177–179. doi: 10.5152/tao.2017.2461. [DOI] [PMC free article] [PubMed] [Google Scholar]